The activity and risk of relapse of Takayasu’s arteritis are low during pregnancy. Up to 40% of patients may have unfavorable obstetric outcomes, therefore it is important to know their clinical behavior. We describe the clinical characteristics and obstetric outcome of pregnant women with Takayasu arteritis treated in a hospital of high complexity.
Materials and methodsA retrospective evaluation of medical records of pregnant patients with Takayasu’s arteritis treated at Hospital Universitario San Vicente Fundación in Medellin, Colombia between 2011 and 2018.
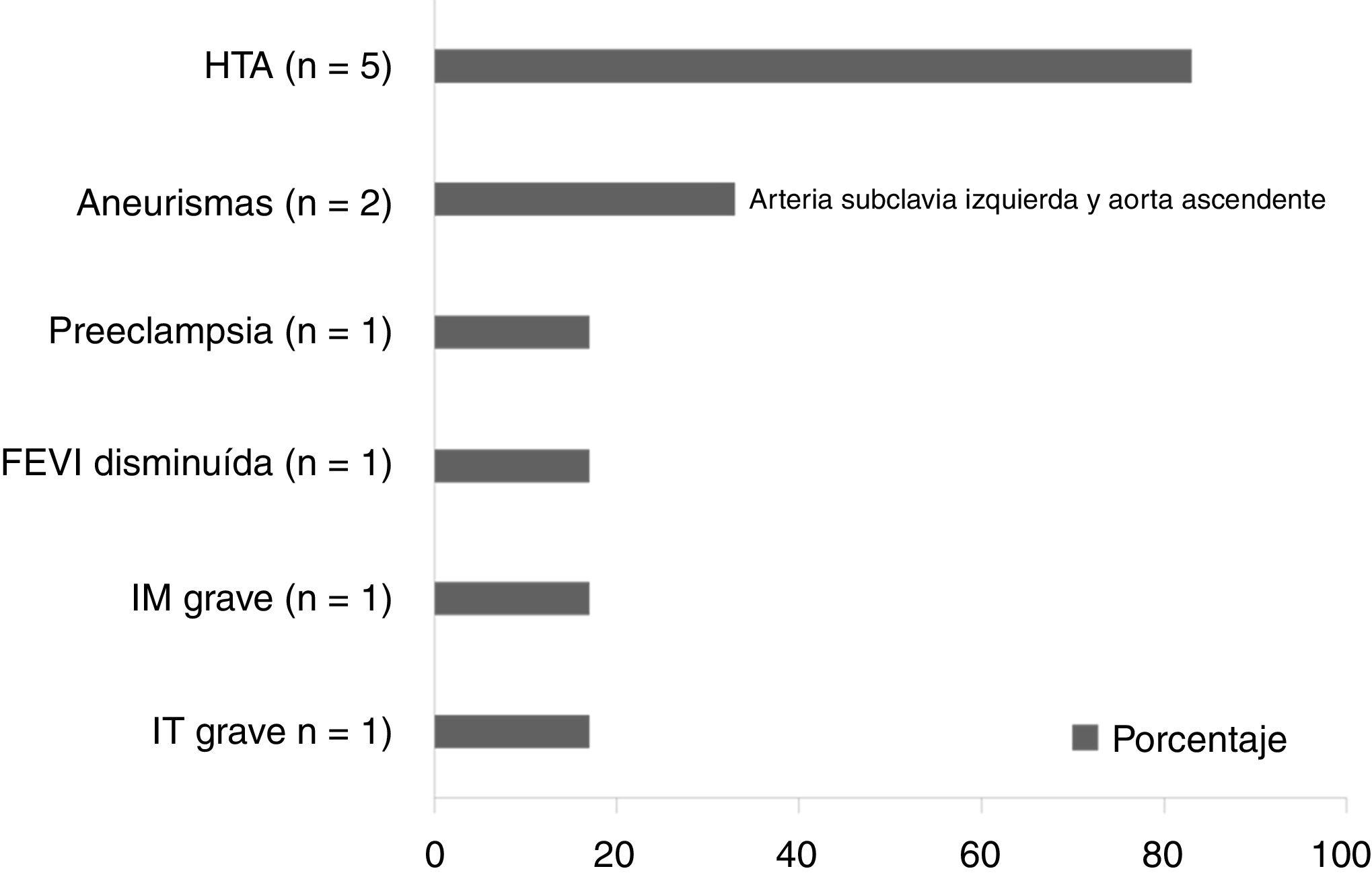
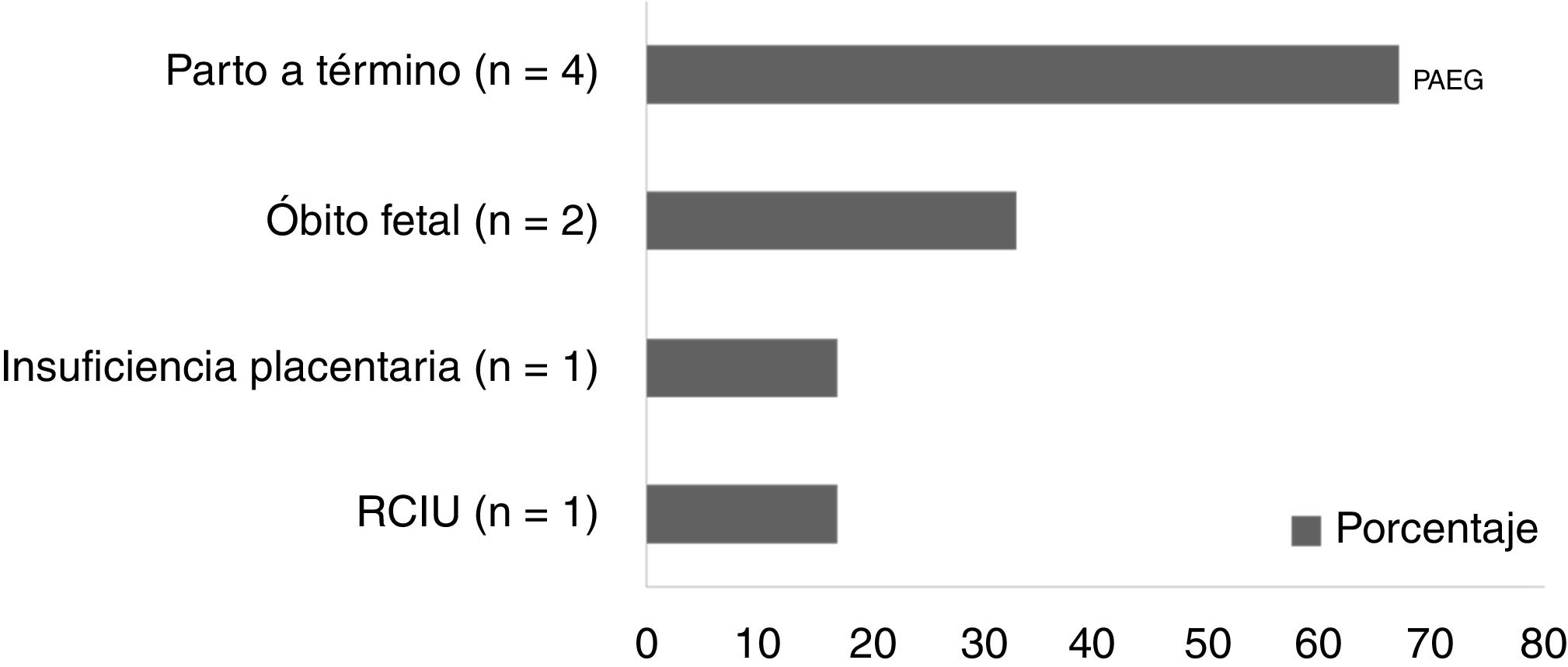
ResultsSix patients with a median age at diagnosis 17.5 years (IQR 9.25), at delivery 24 years (IQR 8.25), disease duration 5.5 years (IQR 10.5). Three patients had extensive aortic involvement; at delivery, three patients were active and required immunosuppressants, five had high blood pressure, one developed preeclampsia in the second trimester, one had severe mitral and tricuspid insufficiency with a decreased ejection fraction of the left ventricle; two had aneurysms (left subclavian artery and ascending aorta). No pregnancy resulted in abortion or preterm birth; there were two fetal deaths, one due to intrauterine growth restriction and placental insufficiency and another of unknown etiology; both patients with disease activity, extensive aortic condition, and arterial hypertension. Five deliveries were by cesarean section by maternal indication; there was no aortic dissection, aneurysmal rupture or cerebral hemorrhage.
ConclusionPatients with active disease and extensive aortic compromise presented unfavorable obstetric results, suggesting that inadequate control of vasculitis leads to greater maternal-fetal complications.
la actividad y riesgo de recaída de la arteritis de Takayasu son bajos durante la gestación. Hasta el 40% de pacientes puede tener desenlaces obstétricos desfavorables por lo que es importante conocer su comportamiento clínico. Describimos las características clínicas y el desenlace obstétrico de gestantes con arteritis de Takayasu atendidas en un hospital de alta complejidad.
Materiales y métodosevaluación retrospectiva de historias clínicas de gestantes con arteritis de Takayasu atendidas en el Hospital Universitario San Vicente Fundación de Medellín, Colombia, entre 2011 y 2018.
Resultadosseis pacientes con mediana de edad al diagnóstico 17,5 años (RI 9,25), al parto 24 años (RI 8,25), duración de la enfermedad 5,5 años (RI 10,5). Tres pacientes tenían compromiso aórtico extenso; al parto, tres pacientes estaban activas y requirieron inmunosupresores, cinco tenían hipertensión arterial, una desarrolló preeclampsia en el segundo trimestre, una tenía insuficiencia mitral y tricuspídea graves con disminución de la fracción de eyección del ventrículo izquierdo; dos tenían aneurismas (arteria subclavia izquierda y aorta ascendente). Ningún embarazo resultó en aborto ni parto pretérmino; hubo dos óbitos fetales, uno por restricción del crecimiento intrauterino e insuficiencia placentaria, y otro de etiología desconocida; ambas pacientes con actividad de la enfermedad, afección aórtica extensa e hipertensión arterial. Cinco partos fueron por cesárea por indicación materna; no hubo disección aórtica, ruptura aneurismática o hemorragia cerebral.
Conclusiónlas pacientes con enfermedad activa y afección aórtica extensa presentaron resultados obstétricos desfavorables, sugiriendo que el inadecuado control de la vasculitis genera mayores complicaciones materno-fetales.
Takayasu’s arteritis (TA) is a granulomatous vasculitis of large vessels that mainly affects the aorta and its proximal branches.1,2 It has historically been known as «pulseless disease» or «aortic arch syndrome», among other names. It was in 1990 when the American College of Rheumatology published the classification criteria and the disease took the name of TA.3 Its etiology is unknown, but it seems to be related to infectious triggers that amplify the inflammatory response through cellular mechanisms and cause damage to the vascular wall with subsequent thickening, fibrosis, stenosis, thrombus formation, and aneurysms.3 The lesions are usually asymptomatic and are discovered in late stages of the disease, when ischemic symptoms occur.4
TA occurs more frequently in women (80–90% of cases), usually between the second and third decades of life, that is, of childbearing age.5 Even though pregnancy has been associated with a polarization of cytokines towards the TH2 phenotype, both at the maternal-fetal interface and systemically, which decreases the frequency of the activity and reduces the risk of relapse of the vasculitis,6 unfavorable obstetric outcomes occur in up to 40% of the cases.7 Maternal complications can include preeclampsia, heart failure, aortic regurgitation, aneurysms in the aorta and in other arterial beds (which can undergo rupture), brain hemorrhage, pulmonary hypertension, renal failure and even death.8–10 Fetal complications include abortion, fetal death, intrauterine growth restriction (IUGR), preterm birth, low birth weight and neonatal maladaptation.5,8,11
It is fundamental for the rheumatologist and the obstetrician to know the clinical behavior of this disease during pregnancy and the possible maternal and fetal outcomes, since complications could be predicted and reduced with an adequate control. The objective of this study is to describe the clinical characteristics and the obstetric outcomes of pregnant patients with TA treated in a center of high complexity in the city.
Materials and methodsIt was conducted a retrospective cross-sectional descriptive study of case series, in which the medical records of the patients treated at the Hospital Universitario San Vicente Foundation in Medellin between August 2011 and May 2018 were reviewed. The inclusion criteria were: having the diagnosis of TA established by a rheumatologist, with or without disease activity according to the criteria of this expert, being pregnant during that period, having complete data from the records, including acute phase reactants, and knowing the outcome of the pregnancy.
For the data analysis, descriptive statistics were used through frequency, mean and median to know the central tendency, and interquartile range (IQR) for data dispersion. The analyses were carried out using SPSS 22. It is an observational, retrospective study, approved by the institutional ethics committee, without interventions or risk to the subjects, which does not contain personal information, photographs or images that allow to identify the patients, in which their confidentiality is guaranteed and the data were obtained from a secondary source (medical records).
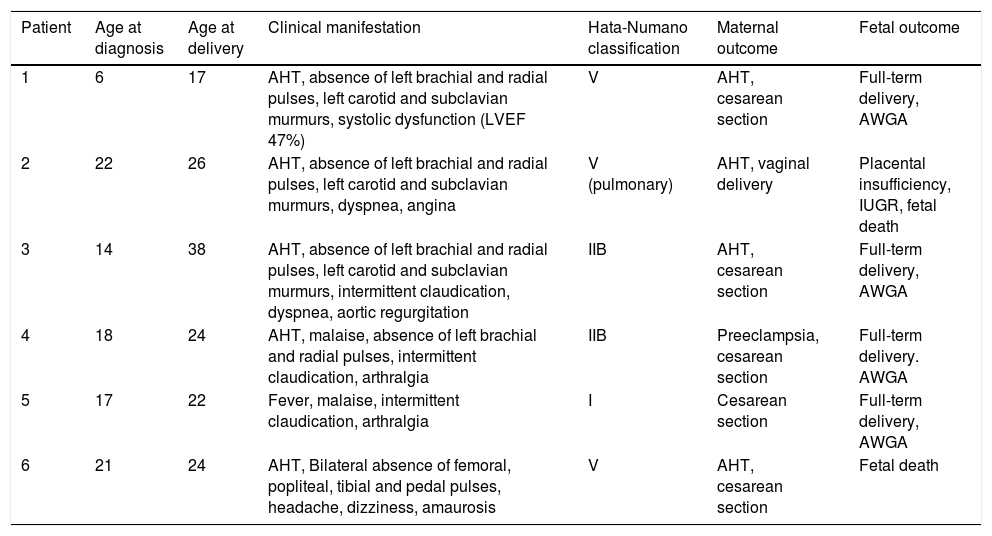
ResultsThe medical records of 8 pregnancies in 8 patients with TA were retrospectively evaluated, 2 of them were excluded because the data were incomplete and the obstetric outcomes were unknown. Of the 6 patients analyzed, 3 lived in the city of Medellin and the others came from a rural area, with a median age at diagnosis of 17.5 years (IQR 9.25), at the time of pregnancy of 24 years (IQR 8.25) and a disease duration of 5.5 years (IQR 10.5). Of them, 5 had a previous diagnosis of TA and in one it began during pregnancy.
The clinical findings were pulse deficit and AHT in 5 patients, intermittent claudication in 3, subclavian and carotid murmurs in 3, fever and malaise in 2, and arthralgia in 2. Other clinical manifestations were dyspnea, angina, headache, dizziness and amaurosis present in at least one of the patients (Table 1). Three patients were classified according to the extent of the disease as Numano type v, 2 as type iiB and one as type i. The averages of erythrocyte sedimentation rate and C-reactive protein were 101 ± 21 mm/h and 3.78 ± 3 mg/dl, respectively. Regarding the treatment, 2 patients received prednisolone, azathioprine and low doses of aspirin. At the time of delivery, the disease was active in 3 patients, so they required prednisolone (1 mg/kg/day) and starting methotrexate in the postpartum.
Demographic and clinical characteristics of the patients.
| Patient | Age at diagnosis | Age at delivery | Clinical manifestation | Hata-Numano classification | Maternal outcome | Fetal outcome |
|---|---|---|---|---|---|---|
| 1 | 6 | 17 | AHT, absence of left brachial and radial pulses, left carotid and subclavian murmurs, systolic dysfunction (LVEF 47%) | V | AHT, cesarean section | Full-term delivery, AWGA |
| 2 | 22 | 26 | AHT, absence of left brachial and radial pulses, left carotid and subclavian murmurs, dyspnea, angina | V (pulmonary) | AHT, vaginal delivery | Placental insufficiency, IUGR, fetal death |
| 3 | 14 | 38 | AHT, absence of left brachial and radial pulses, left carotid and subclavian murmurs, intermittent claudication, dyspnea, aortic regurgitation | IIB | AHT, cesarean section | Full-term delivery, AWGA |
| 4 | 18 | 24 | AHT, malaise, absence of left brachial and radial pulses, intermittent claudication, arthralgia | IIB | Preeclampsia, cesarean section | Full-term delivery. AWGA |
| 5 | 17 | 22 | Fever, malaise, intermittent claudication, arthralgia | I | Cesarean section | Full-term delivery, AWGA |
| 6 | 21 | 24 | AHT, Bilateral absence of femoral, popliteal, tibial and pedal pulses, headache, dizziness, amaurosis | V | AHT, cesarean section | Fetal death |
AHT: arterial hypertension; LVEF: left ventricular ejection fraction; AWGA: adequate weight for gestational age; IUGR: intrauterine growth restriction.
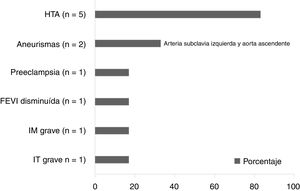
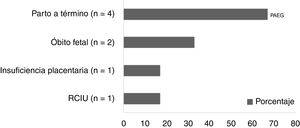
The obstetric outcomes are depicted in Figs. 1 and 2, respectively. No pregnancy resulted in abortion or preterm delivery. The median pregnancy length was 37 weeks (IQR 1.25). There were 2 fetal deaths, one related to IUGR and placental insufficiency, and the other of unclear etiology; both patients had disease activity during pregnancy, extensive aortic commitment (Numano V and pulmonary involvement) and AHT. Five deliveries were by cesarean section due to maternal indication (AHT, unawareness of the presence of aneurysms, fetal death of unknown duration) and no patient presented aortic dissection, aneurysmal rupture or brain hemorrhage.
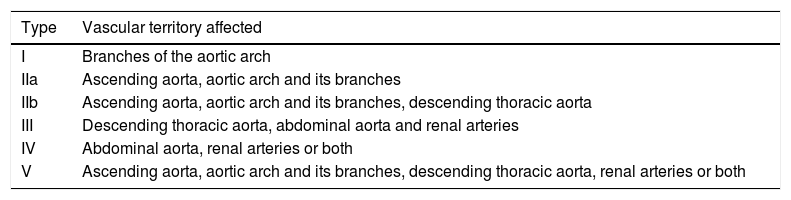
TA is a systemic vasculitis that mainly affects the large caliber-vessels, it usually occurs in women of reproductive age, and it does not affect fertility,12 its extension is classified depending on the affected arterial segments according to Hata-Numano (Table 2),13 and it is the most frequent primary systemic vasculitis in Colombia, according to the study conducted by Ochoa et al.14 The clinical data of this vasculitis during pregnancy known to date come from cohort studies, series and case reports: they include approximately 500 pregnancies in more than 300 patients,6,15 showing as fetal outcomes a proportion of live births of up to 85%, IUGR in 18%, preterm births in 15%, abortions in 10% and fetal deaths in 7%. Chronic AHT in up to 40% and preeclampsia in 20% are described as maternal outcomes.6,15
Hata-Numano classification of the extent of the disease.
| Type | Vascular territory affected |
|---|---|
| I | Branches of the aortic arch |
| IIa | Ascending aorta, aortic arch and its branches |
| IIb | Ascending aorta, aortic arch and its branches, descending thoracic aorta |
| III | Descending thoracic aorta, abdominal aorta and renal arteries |
| IV | Abdominal aorta, renal arteries or both |
| V | Ascending aorta, aortic arch and its branches, descending thoracic aorta, renal arteries or both |
The age of the patients at diagnosis and at pregnancy was lower than that reported in other studies.15 Regarding the disease activity, the evidence is controversial, because although in some studies it has been found that it does not worsen during pregnancy, as in what was reported by Assad et al.,6 Tanaka et al.8 and Hernández-Pacheco et al.,16 in our study half of the patients had active disease, similarly to that was observed by Zhang et al.9
The most frequent complications in our series were AHT, aneurysms, and fetal deaths. Unlike in other reports, cardiovascular events such as aneurysmal rupture, aortic dissection or intracerebral hemorrhage did not occur.15 Unfavorable obstetric outcomes were evident in patients with disease activity and extensive vascular involvement, which can be probably explained by a lower blood flow that can lead to IUGR, placental insufficiency and fetal death, similarly to what is reported in the literature.4,17
Due to the restriction of diagnostic imaging during pregnancy, the existence of aneurysms at the end of pregnancy was unknown in the majority of patients, which influenced the choice of the route of delivery. Even though there are not clear recommendations on the use of angioresonance or angiotomography in the follow-up of these patients due to the risk that the exposure to radiation and contrast media implies,18,19 these images could have a prognostic value, by evaluating the extent of the vascular involvement and the presence of complications such as aneurysms, in addition to playing an important role in the choice of the route of delivery in case that any of these findings is documented.
The limitations of this study are given mainly by the small number of patients, due to the low frequency of the disease, in addition to its retrospective nature by means of the review of medical records, which implied that information was missing in some medical histories and 2 patients had to be excluded from the study due to the absence of follow-up data.
ConclusionsTA is a vasculitis that mainly affects women of childbearing age, so it is possible to find pregnant patients with the disease. Patients with active disease during pregnancy and at the time of delivery, as well as with extensive aortic involvement, presented unfavorable obstetric outcomes, indicating that inadequate control of vasculitis leads to an increased risk of maternal-fetal complications, therefore, it is important that both the obstetrician and the rheumatologist become familiar with the disease and its possible outcomes.
Conflict of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Velásquez Giraldo I, Torres Saavedra FA, Muñoz Vahos CH, Jaramillo Arroyave D, Hernández Zapata J, Vásquez G, et al. Desenlaces obstétricos en pacientes con arteritis de Takayasu: serie de casos. Rev Colomb Reumatol. 2021;28:213–217.