Paget's disease of bone (PDB) is a benign disorder characterized by focal areas of bone turnover. So far, only 17 cases have been described in Colombia. We present the case of a 68-year-old male who presented with otorrhea and deafness. The skull x-rays and computerized tomography findings were suggestive of malignancy. Consequently, an 18F-FDG PET/CT was performed and showed intense uptake in the skull and lumbar spine. The workup showed elevated alkaline phosphatase levels consistent with PDB and the biopsy ruled out other differential diagnoses. The patient received alendronate with symptomatic improvement and decreased alkaline phosphatase levels.
La enfermedad ósea de Paget (EOP) es un trastorno benigno, caracterizado por áreas focales de recambio óseo. Hasta el momento solo se han descrito 17 casos en Colombia. Se presenta el caso de un paciente masculino de 68 años que consultó por otorrea e hipoacusia. Los hallazgos en la radiografía y la tomografía computarizada fueron sugestivos de malignidad craneana, se realizó una 18F-FDG PET/CT que mostró hipercaptación en el cráneo y en la columna lumbar. Se encontraron niveles altos de fosfatasa alcalina consistente con EOP. La biopsia descartó otros diagnósticos diferenciales. El paciente recibió alendronato y experimentó una mejoría sintomática y disminución de la fosfatasa alcalina.
Paget’s disease of the bone (PDB), also known as deformans osteitis, described in 1877 by James Paget,1 is a benign disorder characterized by focal areas of increased bone turnover.2,3 Its etiology has not been completely clarified, it is believed that it involves genetic and environmental factors.3,4 Worldwide, the prevalence of the disease in people over 40 years of age varies between 3 and 4% and increases with age.1 It has a heterogeneous geographical distribution, mainly in Great Britain, Australia, New Zealand and the United States.5 In contrast, this disease is rare in Latin America; although it is more frequent in Argentina and Brazil, it is unusual in Colombia,5 with only 17 cases reported in the literature.5–9
This disease can be asymptomatic in up to 20% of cases and is incidentally diagnosed with alkaline phosphatase (AP) levels or images suggestive of PDB.1 The clinical presentation is variable and bone pain is its most common symptom.2 The most frequent locations are the skull, spine, pelvis, and proximal long bones.1 The diagnosis is mainly clinical-radiological and its extension can be evaluated by scintigraphy with technetium-99-m-methyl-disphosphonate (99mTc-MDP).10 In patients with diagnostic uncertainty or with the disease confirmed and poor response to treatment, tomography, magnetic resonance imaging (MRI), and [18F]Fluoro-2-deoxy-d-glucose positron emission tomography (18F-FDG PET/CT) can be used.10–12
We present the case of a male patient with a diagnosis of PDB, with involvement of the skull and vertebral spine, in which the importance of the use of 18F-FDG PET/CT for this diagnosis is demonstrated, as well as its advantages and disadvantages.
Clinical caseA 68-year-old male patient, non-native, from Montería, Colombia, of English and Lebanese descent, without family medical antecedents, who has a history of left tympanic rupture in childhood, due to trauma, as well as arterial hypertension, dyslipidemia, obesity, vitamin D deficiency, and squamous cell carcinoma on the face. The patient consulted to otorhinolaryngology for a clinical picture of 45 days of evolution of scant and intermitted right otorrhagia, with no other associated symptoms. In this evaluation, a polyp is detected in the external auditory canal, which is corrected by cauterization. The rest of the physical examination and vital signs are normal.
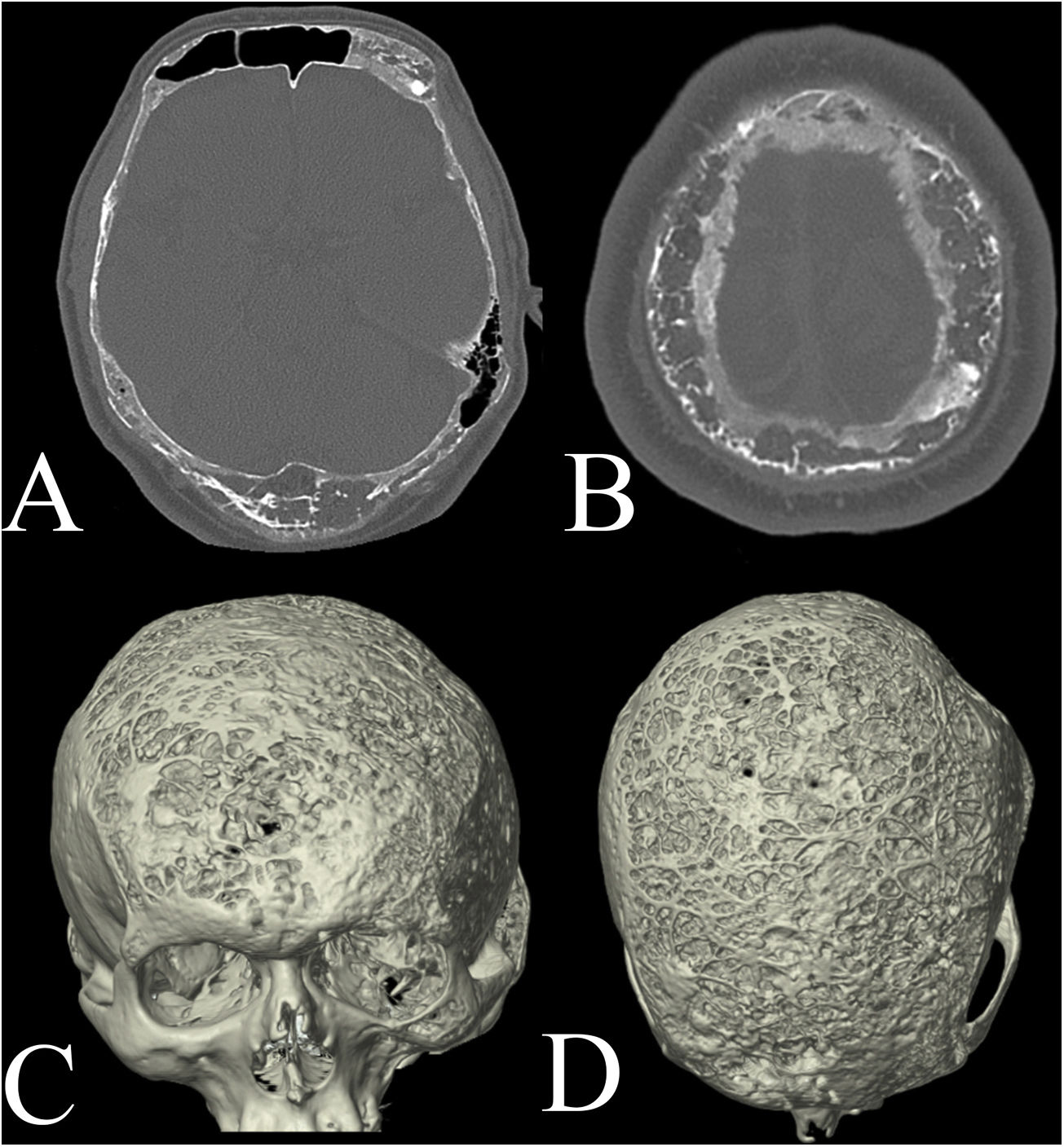
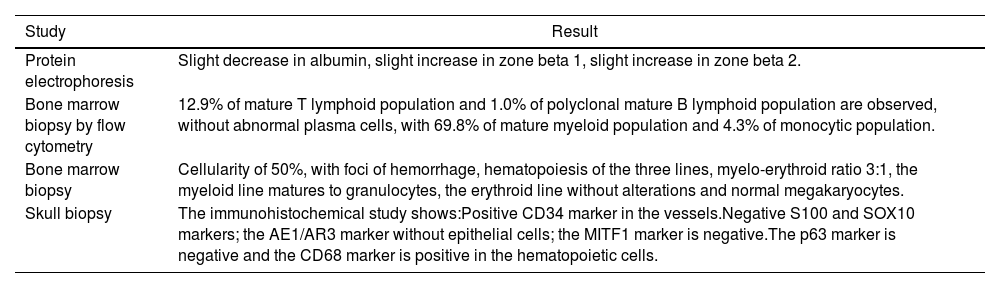
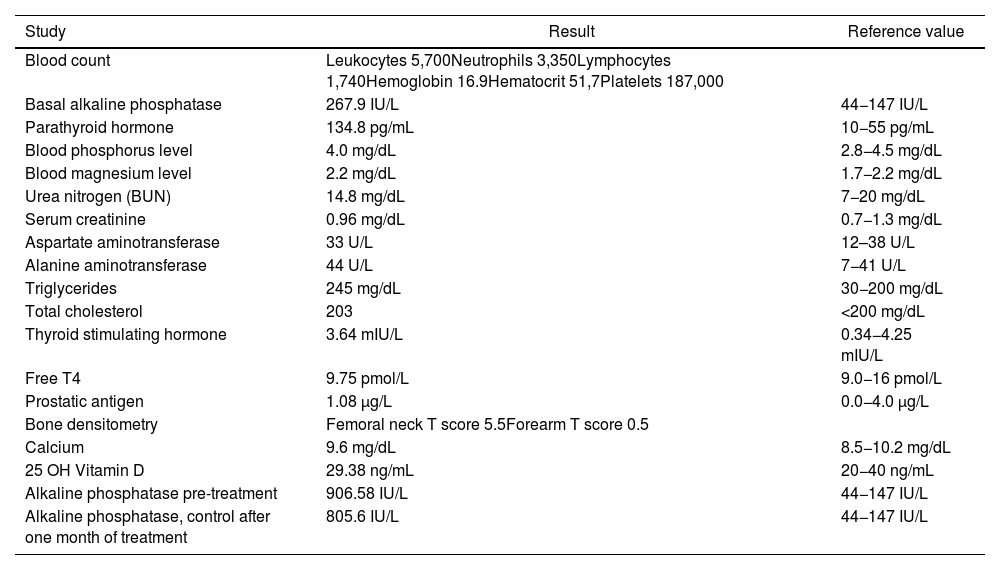
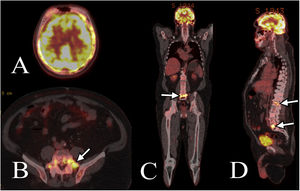
It is considered that the finding of the polyp is incidental and does not explain the symptoms, for which an audiometry is performed, which reveals a severe left conductive hearing loss, as well as a simple X-ray of the skull in which multiple non-specific nodular radiopaque images are visualized in the cranial vault; a simple skull tomography is also performed, in which multiple lytic lesions are observed with extensive and severe involvement of the entire cranial vault (Fig. 1). Due to this finding, the diagnosis of multiple myeloma (MM) is considered, for which a bone marrow biopsy is performed, with Bence-Jones protein and protein electrophoresis with kappa and lambda chains (Table 1), which are normal, so MM is ruled out. In addition extension paraclinical tests are performed (Table 2), which reveal elevated levels of AP, suggesting the biochemical diagnosis of PDB.
Simple skull tomography showing severe extensive involvement due to multiple lytic lesions in the cranial vault, including bilateral frontal, parietal, temporal and occipital involvement. (A, B) The axial sections in the bone window show lesions that compromise the outer table, the diploe and the inner table of the entire cranial vault. (C, D) The three-dimensional reconstruction of the tomography shows multiple lytic lesions that compromise the cranial vault in the outer table in its entire extension to the base of the skull.
Histopathological studies.
| Study | Result |
|---|---|
| Protein electrophoresis | Slight decrease in albumin, slight increase in zone beta 1, slight increase in zone beta 2. |
| Bone marrow biopsy by flow cytometry | 12.9% of mature T lymphoid population and 1.0% of polyclonal mature B lymphoid population are observed, without abnormal plasma cells, with 69.8% of mature myeloid population and 4.3% of monocytic population. |
| Bone marrow biopsy | Cellularity of 50%, with foci of hemorrhage, hematopoiesis of the three lines, myelo-erythroid ratio 3:1, the myeloid line matures to granulocytes, the erythroid line without alterations and normal megakaryocytes. |
| Skull biopsy | The immunohistochemical study shows:Positive CD34 marker in the vessels.Negative S100 and SOX10 markers; the AE1/AR3 marker without epithelial cells; the MITF1 marker is negative.The p63 marker is negative and the CD68 marker is positive in the hematopoietic cells. |
Biochemical tests.
| Study | Result | Reference value |
|---|---|---|
| Blood count | Leukocytes 5,700Neutrophils 3,350Lymphocytes 1,740Hemoglobin 16.9Hematocrit 51,7Platelets 187,000 | |
| Basal alkaline phosphatase | 267.9 IU/L | 44−147 IU/L |
| Parathyroid hormone | 134.8 pg/mL | 10−55 pg/mL |
| Blood phosphorus level | 4.0 mg/dL | 2.8−4.5 mg/dL |
| Blood magnesium level | 2.2 mg/dL | 1.7−2.2 mg/dL |
| Urea nitrogen (BUN) | 14.8 mg/dL | 7−20 mg/dL |
| Serum creatinine | 0.96 mg/dL | 0.7−1.3 mg/dL |
| Aspartate aminotransferase | 33 U/L | 12–38 U/L |
| Alanine aminotransferase | 44 U/L | 7−41 U/L |
| Triglycerides | 245 mg/dL | 30−200 mg/dL |
| Total cholesterol | 203 | <200 mg/dL |
| Thyroid stimulating hormone | 3.64 mIU/L | 0.34−4.25 mIU/L |
| Free T4 | 9.75 pmol/L | 9.0−16 pmol/L |
| Prostatic antigen | 1.08 μg/L | 0.0−4.0 μg/L |
| Bone densitometry | Femoral neck T score 5.5Forearm T score 0.5 | |
| Calcium | 9.6 mg/dL | 8.5−10.2 mg/dL |
| 25 OH Vitamin D | 29.38 ng/mL | 20−40 ng/mL |
| Alkaline phosphatase pre-treatment | 906.58 IU/L | 44−147 IU/L |
| Alkaline phosphatase, control after one month of treatment | 805.6 IU/L | 44−147 IU/L |
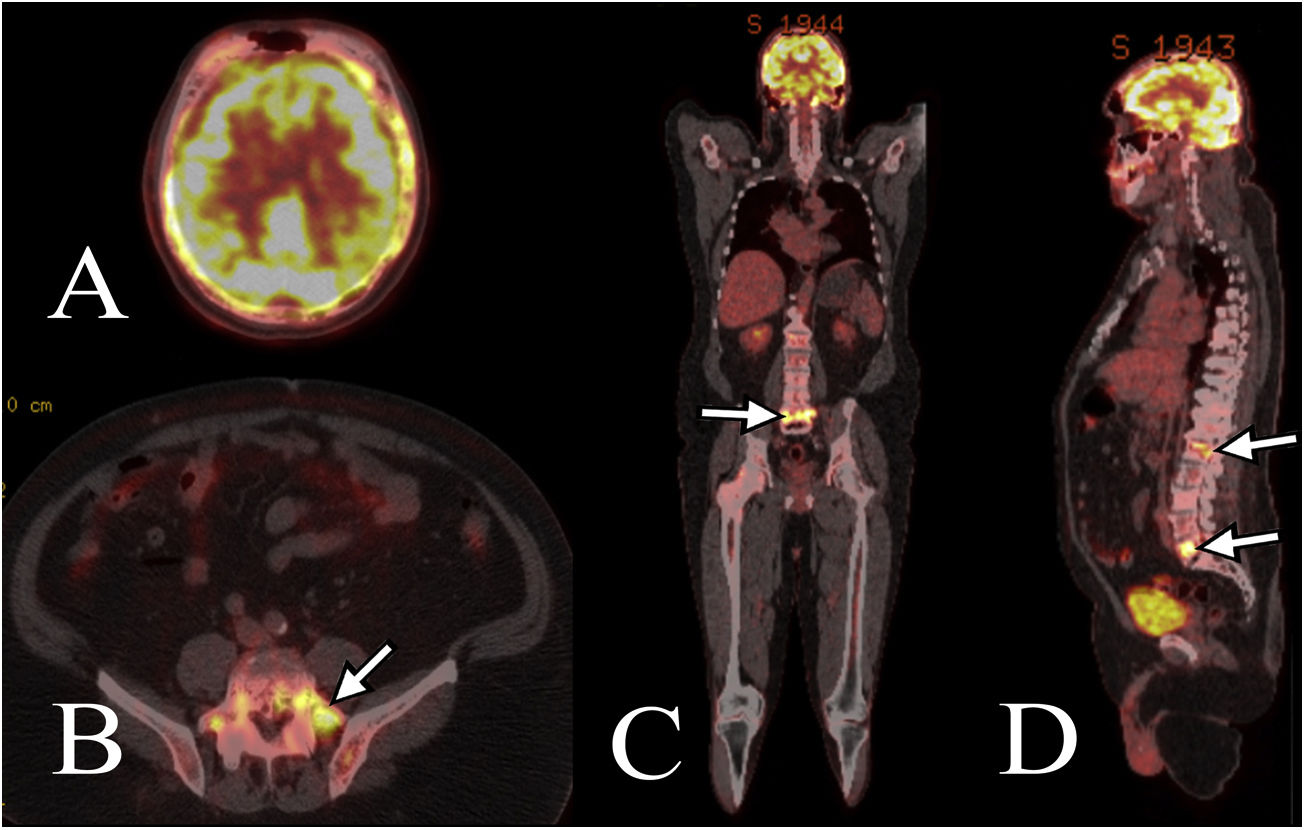
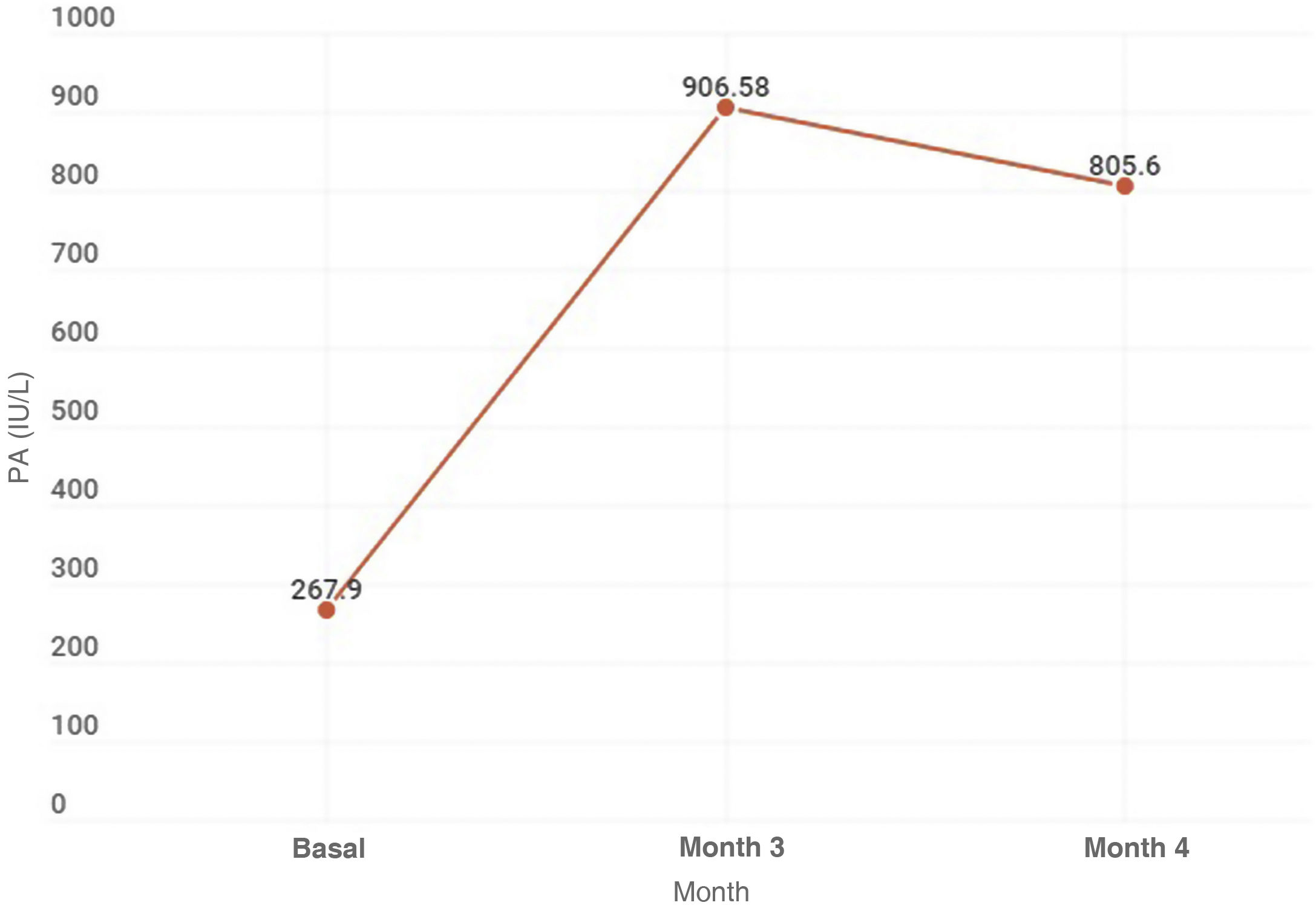
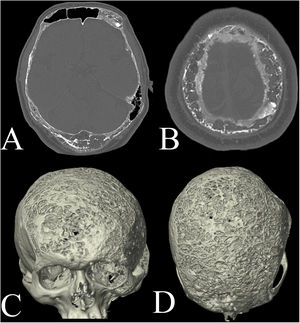
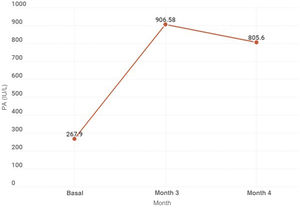
Without being able to rule out a possible neoplastic lesion and given the findings of severe involvement of the cranial vault, it was decided to perform an 18F-FDG PET/CT in order to clarify the diagnosis; the study finds an intense metabolic activity in the entire cranial vault and in the lumbar spine, with predominance in L1 and L4 (Fig. 2). Differential diagnoses at this point include: malignant neoplasms (lymphoma, sarcoma) with involvement of the skull and lumbar spine, PDB and systemic inflammatory process. The patient is evaluated by neurosurgery to define the possibility of performing a biopsy, which is performed due to the intense metabolic activity of the skull and its easy access. The histopathological and immunohistochemical results are consistent with PDB and rule out tumor pathology (Table 1). With this result, it is considered that the otorrhagia presented by the patient is the product of involvement by PDB in the base of the skull. Subsequently, the patient is managed with 70 mg of alendronate once per week, orally for three months and in the follow-up visit is observed an improvement in the levels of AP (Fig. 3), without other episodes of otorrhagia, or appearance of additional symptoms. After the control at three months, the patient did not continue his face-to-face or paraclinical follow-up due to limitations associated with the advent of the new coronavirus SARS-CoV-2 pandemic, however, in the telephone follow-up at three years of treatment he reports that he has not presented additional symptoms again.
The PET/CT images show hypermetabolism corresponding to the area of abnormal enhancement of the vertebrae and skull, with a maximum of 7.5 and 13.9 in L1, L5, and the cranial vault, respectively. (A) Both the skull and the brain show hypermetabolism. (B–D) The arrows show areas of hypermetabolism in the L1 and L5 vertebrae.
PDB is a benign disorder, characterized by focal areas of increased bone turnover in one or more skeletal sites.2,3 Its prevalence increases with age up to 10–11% in people over 80 years of age.1 it is associated with populations of Caucasian origin and areas with high rates of endogamy.5 PDB in Latin America is unusual, the largest number of reports being in Argentina and Brazil, probably because these countries have a higher rate of European ancestry.5 PDB is unusual in Colombia, for which its prevalence in our population is unknown, although an approximate frequency of 1:1,000,000 inhabitants is estimated.5 The first report of PDB in Colombia was published in 1980 and after this, five case series have been published, for a total of 17 reports of PDB in Colombians.5–9
The case of a male patient was presented, with demographic data consistent with that was reported in the literature,1 of Lebanese and English descent, not autochthonous.
This information is relevant, due to the high prevalence of PDB in Great Britain.1 It is noteworthy that, although extensive studies of the prevalence of PDB in Lebanon have not been described, one of the Colombian patients previously diagnosed with PDB also has Lebanese ancestry.9
20% of the patients with PDB are asymptomatic, while symptomatic cases may present pain, hyperemia, deformity, and decreased range of motion, among other symptoms.1 The most frequent locations are the skull (25–65%), the spine (30–75%), the pelvis (30–75%) and the proximal long bones (25–30%).1 The complications of PDB include deformity, fracture, arthritis, gait alterations, spinal cord compression, hypoacusia, and neoplastic transformations.1,2,4,13 The bone involvement of our patient was polyostotic, located in the cranial vault, the base of the skull and the lumbar spine, with a predominance in L1 and L4, findings consistent with what has been reported in the literature.1,5,9
The symptoms associated with the cranial affection are caused by the formation of new periosteal bones that affect the exit of the cranial nerves, for which hypoacusia (30–50%), vertigo (20%) an instability (20–25%) may occur, and less frequently visual, motor or sensory alterations.14 We consider that our patient could have presented otorrhagia due to a spontaneous fracture at the base of the skull, at the level of the temporal bone, secondary to its severe compromise; the finding of the polyp in the auditory canal is considered incidental and not related to the symptoms. It has been reported that in cases of PDB in the skull with malignant degeneration (mainly in osteosarcomas, giant cell tumors, and squamous cell carcinoma) involving the temporal bone or the infratemporal fossa, the most frequent symptoms are: pain, otorrhea, facial weakness, hypoacusia, tinnitus and trismus.15 However, this presentation is rare since malignant degeneration occurs in 1% of cases of PDB.1
The diagnosis of PDB is mainly clinical, radiological and biochemical, either as an incidental finding in images, or with high levels of AP.10 In the biochemical evaluation of our patient, elevated levels of AP were found, which is suggestive of PDB, as well as high levels of parathyroid hormone (PTH), which could be related to a history of vitamin D deficiency. The radiological appearance depends partially on the predominant phase of the disease: lytic, mixed or blastic.16 The scintigraphy with 99mTc-MDP is used to identify involvement in other locations, while other diagnostic images are only indicated in cases of diagnostic uncertainty or in patients with poor response to treatment.10
A radiograph was performed to our patient, with inconclusive findings; therefore, a simple skull tomography was carried out, in this occasion with findings suggestive of MM, which was ruled out by means of a bone marrow biopsy. Given the diagnostic doubt, an 18F-FDG PET/CT was indicated, which suggested PDB and was confirmed by skull biopsy to exclude the differential diagnoses of malignancy. Due to the differential diagnoses by the radiograph and the CT, the use of the 18F-FDG PET/CT was necessary; the most frequent findings of PDB in X-ray, scintigraphy, computed tomography, MRI, and 18F-FDG PET/CT images are described below.
On the radiograph, the lytic phase evidences osteolysis, which is seen as well-defined, radiolucent areas with circumscribed osteoporosis. In the skull, lytic areas are observed that involve the entire extension of the cranial vault, while in the long bones it is seen as a subchondral area that advances in a wedge shape, with a characteristic sharp radiolucent margin, without sclerosis, resembling a blade of grass. In the mixed phase, thickening and hardening of the trabecular pattern and cortex are observed, which are usually pathognomonic. In the blast phase, areas of extensive sclerosis are identified.1,16
In the scintigraphy with 99mTc-MDP, the image classically shows a greater uptake of radionuclides in the abnormal bone region in the three phases of the PDB, the area of distribution of increased uptake is elongated, which may differ from other diagnoses such as metastases and MM, which are usually circular. The advantages of this image are its high sensitivity and the ability to identify the extension in polyostotic PDB, and its main disadvantage is that it is usually normal in asymptomatic patients or in late stages of the disease.1
The findings of PDB on tomography and MRI can be found incidentally, since these tests are not routinely requested in the study of this disease. However, it is of great importance to know the typical appearance of the PDB in these images to avoid misdiagnosis, such as neoplastic diseases.1 The findings in tomography are similar to those of the radiography, in the lytic phase there is evidence of loss of normal trabeculae and lytic areas with circumscribed osteoporosis.1,16 The mixed phase shows cortical thickening and the blast phase show areas of sclerosis with fat attenuation.1,16
On the MRI, in the inactive mixed phase, the signal intensity of the bone marrow is maintained, regardless of the sequence; in the active mixed phase, the T1 images show decreased signal, similar to that of the muscle, with foci of intermixed, normal and maintained marrow, which helps to differentiate it from malignant lesions. In the late blast phase, the marrow space has a low signal intensity that represents sclerosis; regardless of the sequence, the increased blood flow causes the PDB to have a speckled pattern with the contrast medium.1,16
18F-FDG PET/CT in PDB has demonstrated to have a variable uptake in the compromised bones.11,17–19 In some cases, it has proven to be a useful tool to differentiate benign diseases such as PDB from primary or metastatic malignant lesions.10,20 However, it is not a routine study, due to its high cost and its possible false negatives or false positives. For example, either cases with findings suggestive of PDB that turned out to be malignant diseases,21 or findings suggestive of metastatic disease in patients with antecedents of malignancy that turned out to be PDB12,18,22–24 have been identified. These are the cases in which a confirmatory histopathological study would be indicated,25 as in the case presented here. Finally, there are studies that have demonstrated a role of the 18F-FDG PET/CT in the monitoring of the response to treatment with biphosphonates in patients with monostotic disease.11
ConclusionsThe case of a Colombian patient with PDB with atypical presentation is presented, in which it is demonstrated that 18F-FDG PET/CT is a complementary image that can guide the diagnosis of PDB in patients with a differential diagnosis of malignant, primary or metastatic disease, according to their antecedents and clinical history. In the same way, it serves to show the areas with the greatest activity to suggest the best biopsy site if required. However, given its high cost and possible false positives and negatives, it is not recommended to use it on a routine basis.
Ethical considerationsBeing a case report, it does not require approval by a research committee. However, our study had the informed consent from the patient for publishing the information and images in the article. The private information that could allow the identification of the patient was anonymized.
FundingThis work has not received any type of funding.
Conflict of interestThe authors declare they have no conflict of interest.