Fatigue is a frequent symptom in patients with rheumatoid arthritis (RA). The Functional Assessment of Chronic illnesses Therapy-Fatigue (FACIT-F) is an instrument that assesses self-reported fatigue and was validated for measuring fatigue in RA.
ObjectiveThe aim of this study was to validate the FACIT-F for use in Spanish-speaking RA patients.
Materials and methodsCross-sectional, multicentre study. We included patients (n = 192) with RA diagnosis from two hospitals. Exploratory and confirmatory analyses were conducted. Construct validity and internal consistency were evaluated.
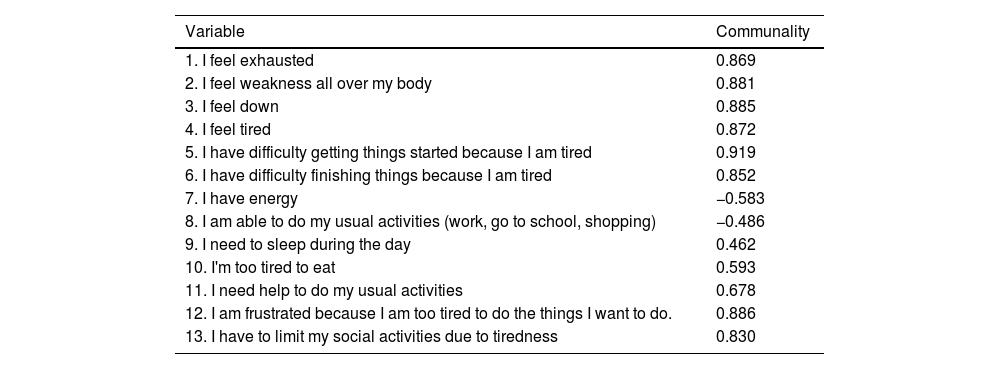
ResultsFACIT-F showed high internal consistency (Alpha = .87, Omega = .93). Analysis of the main components showed a single factor, which explained 62% of the variance. The confirmatory factor analysis showed a satisfactory fit of the model. We found a correlation between FACIT–F, VAS fatigue (−.72 p-value <,001), and BRAF-MDQ (−.81 p-value <.001).
ConclusionFACIT-F is a valid instrument with a high internal consistency for measuring fatigue in clinical practice and research in Spanish-speaking patients with RA.
La fatiga es un síntoma frecuente entre los pacientes con artritis reumatoide (AR). La Escala de Evaluación Funcional de Terapia de Enfermedades Crónicas-Fatiga (FACIT-F) es una herramienta usada para medir la fatiga.
ObjetivoEl objetivo de este estudio fue la validación de FACIT-F en una población hispanohablante con AR.
Materiales y métodosDiseño transversal multicéntrico. Se incluyeron pacientes con AR (n = 192). Se realizó un análisis factorial exploratorio y confirmatorio para la escala FACIT-F. Se evaluó la validez del constructo y la consistencia interna del cuestionario.
ResultadosFACIT-F presentó una alta consistencia interna (Alfa = 0,87, Omega = 0,93). El análisis de componentes principales mostró un solo factor, lo que explicó el 62% de la varianza total. El análisis factorial confirmatorio mostró un ajuste satisfactorio del modelo. Se observó una fuerte correlación significativamente estadística entre FACIT–F, EVA fatiga (-0,72 p-valor <0,001) y BRAF-MDQ (-0,81 p-valor <0,001).
ConclusiónFACIT-F es un instrumento válido y con alta consistencia interna para medir la fatiga en la práctica clínica y en la investigación dirigidas a la población hispanohablante con AR.