Transient osteoporosis of pregnancy is a pathology of low prevalence and difficult diagnosis that mainly affects pregnant women in the third trimester of pregnancy. It is characterized by mechanical joint pain, more frequent in the lower limbs, radiological osteopenia, and bone oedema on magnetic resonance imaging (MRI). A series of 4 cases is presented in pregnant women between 26 weeks of gestation and the early puerperium with symptoms of coxalgia and/or knee pain. The treatment was based on conservative measures: analgesics that are allowed during pregnancy and non-weight bearing on the joints, and the possibility of corticosteroid infiltration into the joint. Bisphosphonates can be added in the puerperium. All cases resolved within a maximum of 9 months, without subsequent sequelae.
La osteoporosis transitoria del embarazo es una patología de baja prevalencia y difícil diagnóstico que afecta sobre todo a embarazadas en el tercer trimestre de gestación. Se caracteriza por dolor mecánico articular, más frecuente en miembros inferiores, osteopenia radiológica y edema óseo en resonancia magnética nuclear (RMN). Presentamos una serie de 4 casos en gestantes entre las 26 semanas de gestación y el puerperio precoz con clínica de coxalgia y/o gonalgia. El tratamiento se basó en medidas conservadoras: analgésicos permitidos durante la gestación y descarga articular, con la posibilidad de utilizar infiltración articular de corticoesteroides. En el puerperio se pueden añadir bifosfonatos. Todos los cuadros se resolvieron en un plazo máximo de 9 meses, sin secuelas posteriores.
Transient osteoporosis of pregnancy is a rare, generally underdiagnosed disease that presents as pain and functional impotence of the affected limb. It usually affects women in the last trimester of pregnancy and in the postpartum period.1
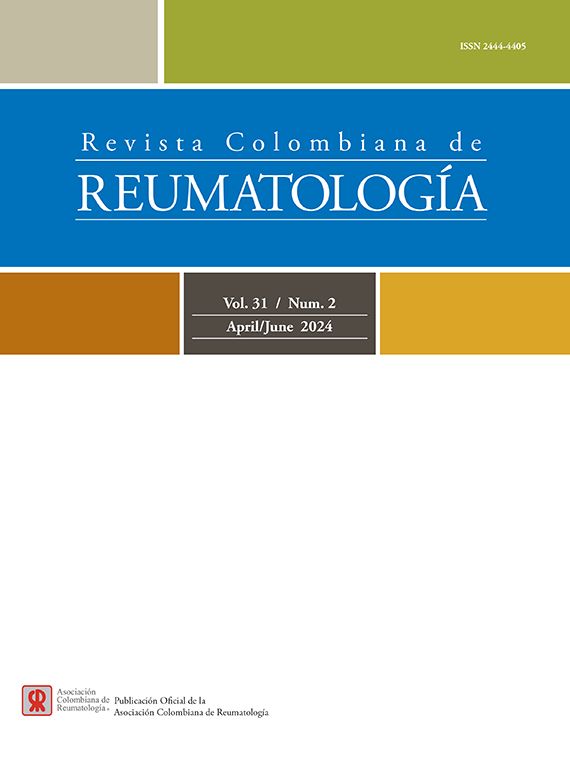
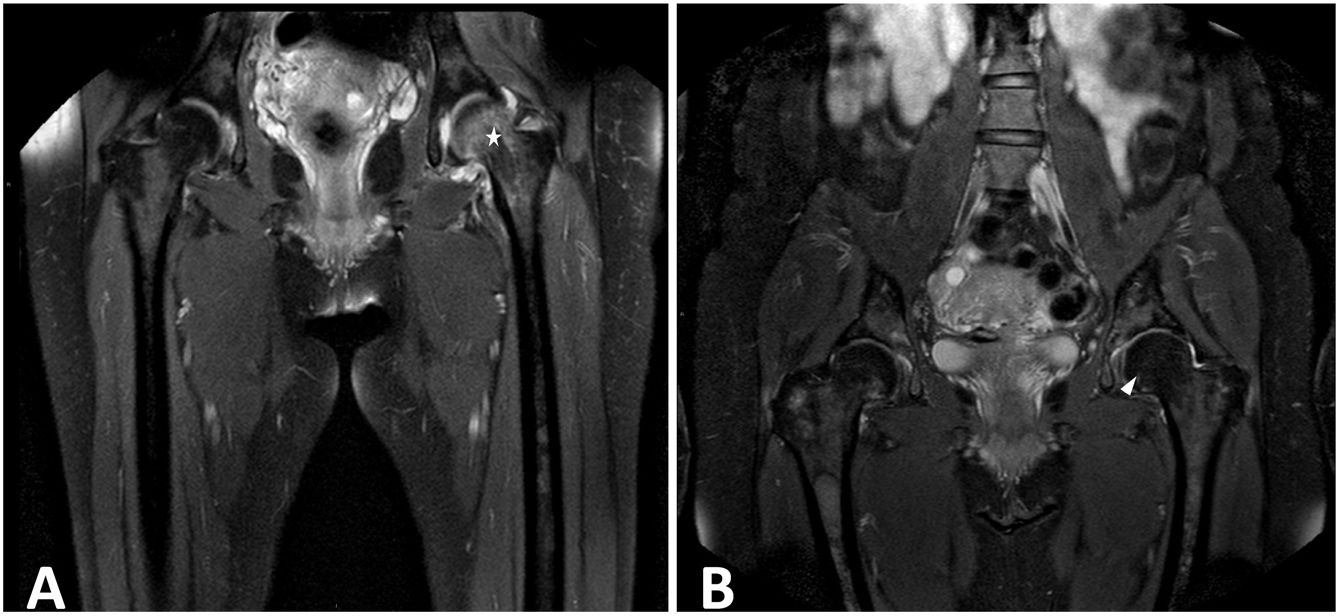
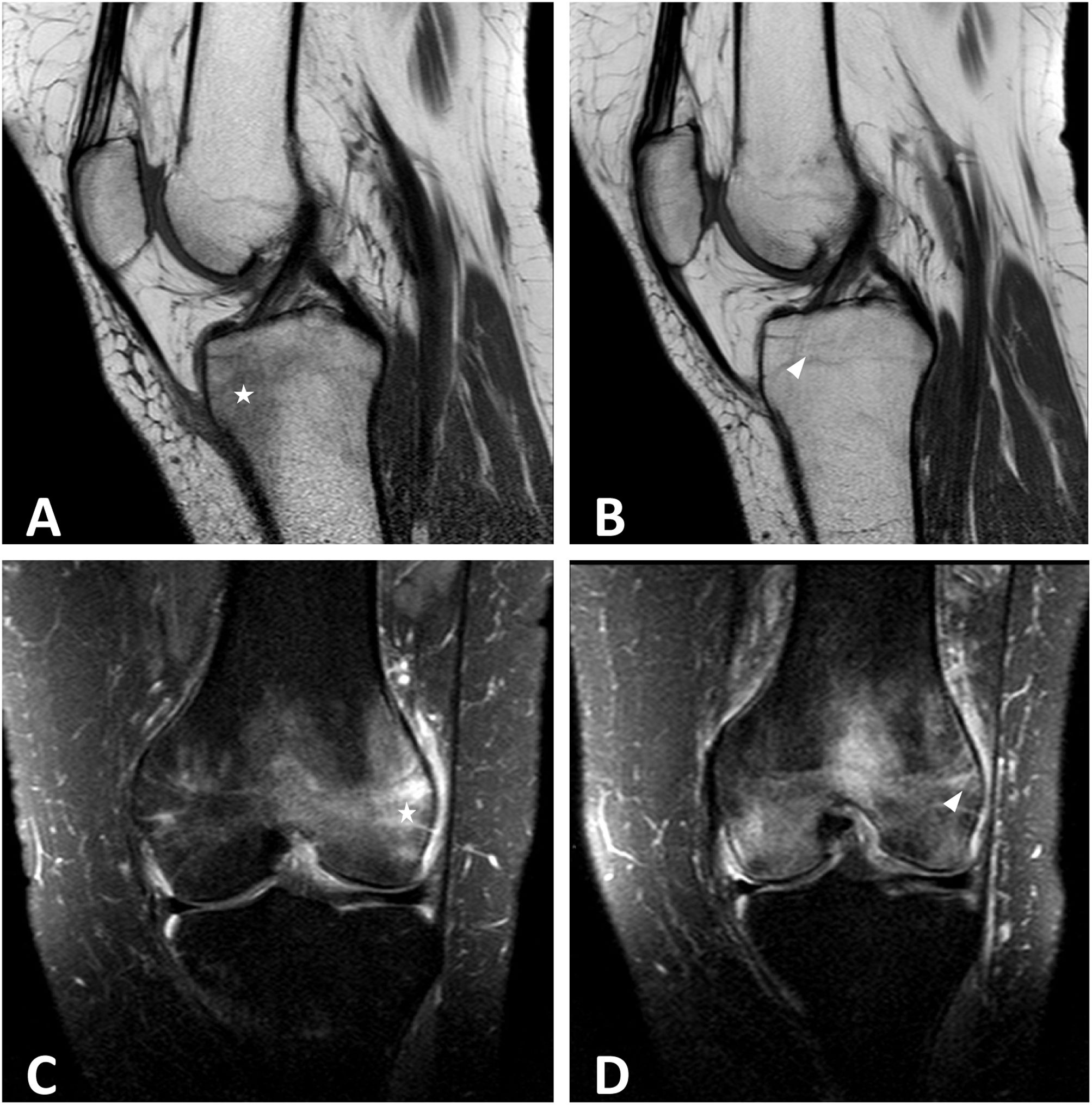
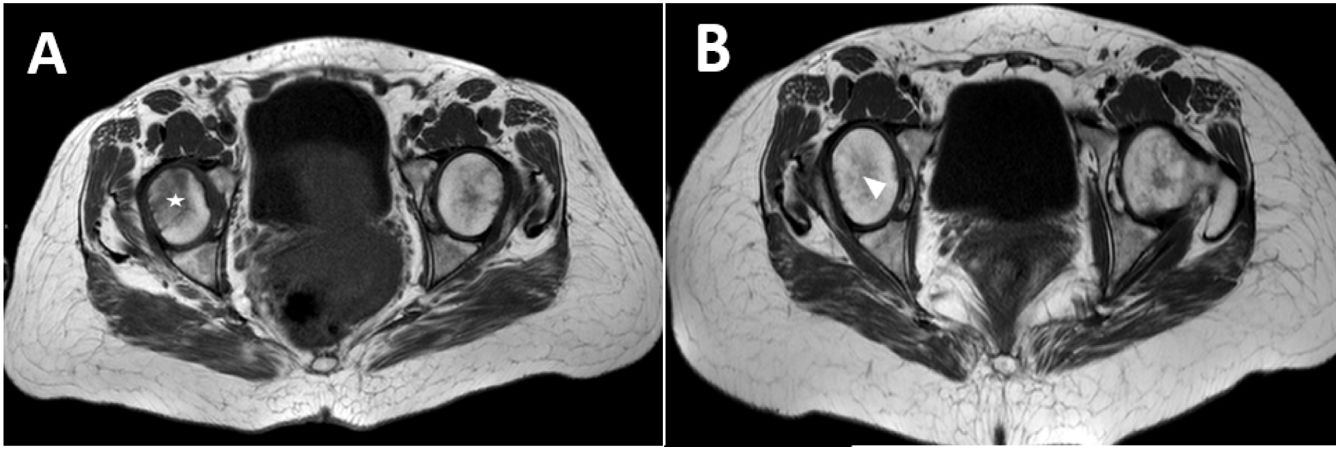
It is characterized by mechanical arthralgias, radiological osteopenia and spontaneous resolution of the condition after childbirth.2 The most affected joint is usually the hip, in up to 75% of cases,3,4 but it can affect the knees, ankles, elbows or wrists.5 Its pathophysiology is unknown, although it has been proposed that it could be secondary to microlesions due to mechanical overload and the displacement of the center of gravity that occurs during pregnancy,6 as the load-bearing joints are preferentially affected. The diagnosis can be made by plain radiography, which shows radiological osteopenia, or by magnetic resonance imaging (MRI), in which a pattern of bone marrow edema with increased signal intensity is observed in T2-weighted images. In addition, MRI allows us to make the differential diagnosis between osteoporosis and avascular osteonecrosis.7
Case seriesBelow we present 4 cases of transient osteoporosis in pregnant women diagnosed in our center (Hospital Universitario Nuestra Señora de Valme, Seville).
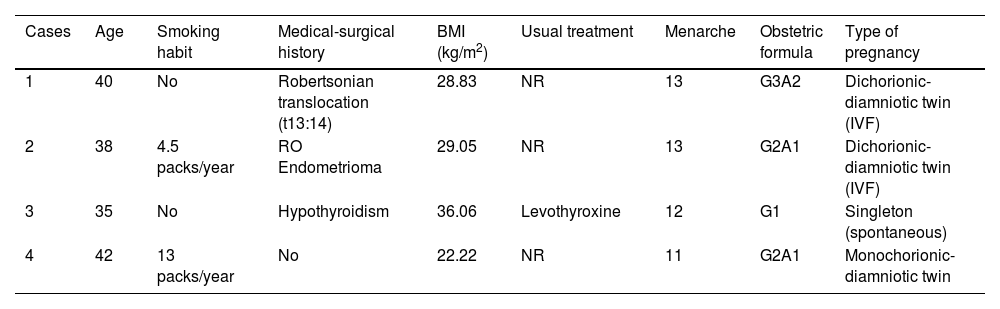
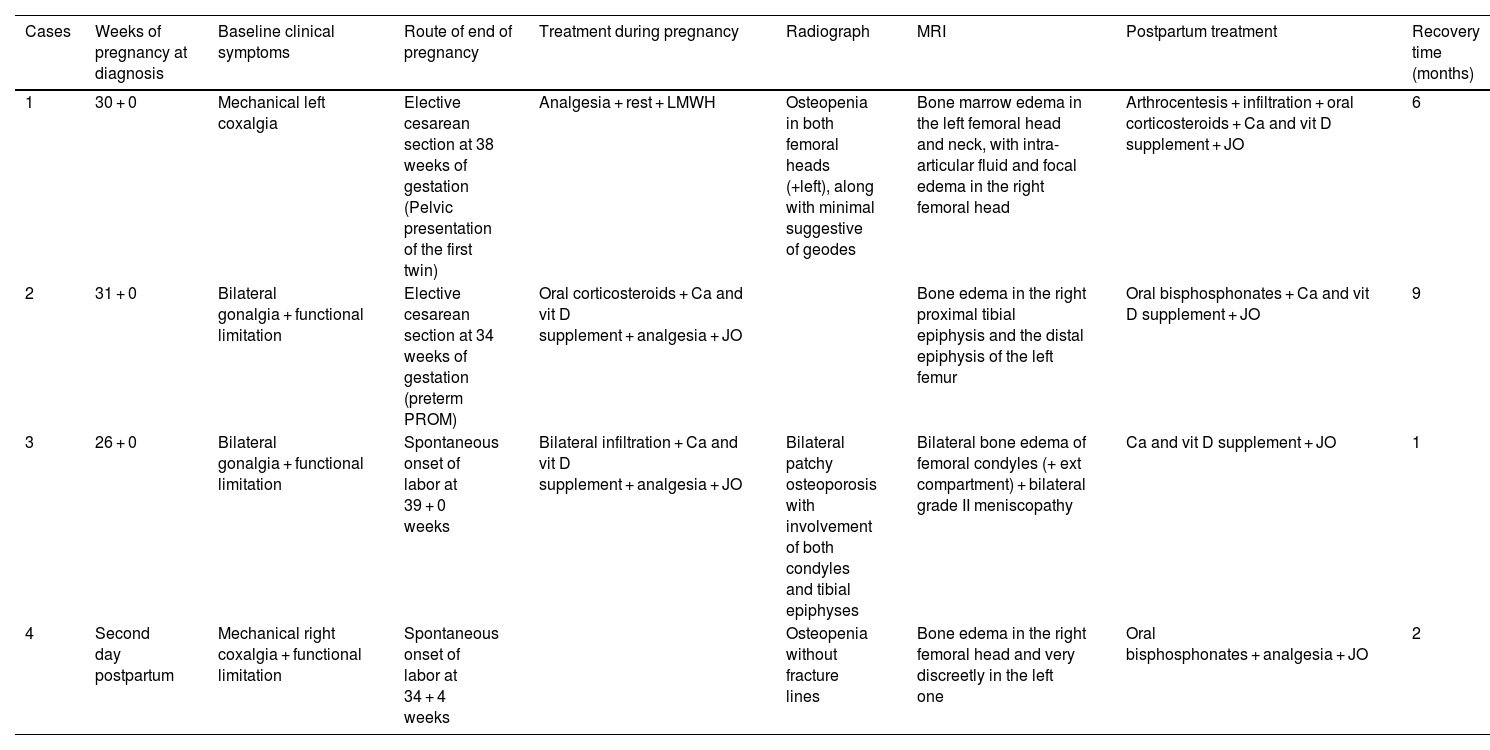
The mean age of the patients was 38.7 years (42–35); 2 of the 4 patients had a smoking habit, with a consumption of 4.5 and 13 packs per year. One of the patients had normal weight (body mass index of 22.22 kg/m2), while the rest had a weight above the normal range, one of them in the range of moderate obesity (36.06 kg/m2). Otherwise, they were healthy women, with no medical history relevant to the case. Regarding the gyneco-obstetric sphere, all patients were nulliparous, although 3 of them had a history of abortion; 3 of the 4 cases were twin pregnancies: 2 dichorionic-diamniotic and one monochorionic-diamniotic. The clinical manifestations were unilateral coxalgia (right) in 50% and bilateral gonalgia in the same percentage. With the exception of one case in which the clinical manifestations began on the second day postpartum, in the rest of the patients the onset of symptoms was at the end of the second trimester or at the beginning of the third trimester of pregnancy. In all cases, management was carried out with on-demand analgesia and unloading of the affected joint, with joint infiltration with corticosteroids and local anesthetic before delivery in one case and after delivery in another (in this case oral prednisone was required during pregnancy). In the postpartum, half of the patients received oral bisphosphonates, but all patients received calcium and cholecalciferol supplements and showed improvement in the following months, with complete recovery within the first 9 months. (Tables 1 and 2).
Personal history of case patients (H. Universitario Virgen de Valme).
| Cases | Age | Smoking habit | Medical-surgical history | BMI (kg/m2) | Usual treatment | Menarche | Obstetric formula | Type of pregnancy |
|---|---|---|---|---|---|---|---|---|
| 1 | 40 | No | Robertsonian translocation (t13:14) | 28.83 | NR | 13 | G3A2 | Dichorionic-diamniotic twin (IVF) |
| 2 | 38 | 4.5 packs/year | RO Endometrioma | 29.05 | NR | 13 | G2A1 | Dichorionic-diamniotic twin (IVF) |
| 3 | 35 | No | Hypothyroidism | 36.06 | Levothyroxine | 12 | G1 | Singleton (spontaneous) |
| 4 | 42 | 13 packs/year | No | 22.22 | NR | 11 | G2A1 | Monochorionic-diamniotic twin |
IVF: in vitro fertilization; BMI: body mass index; NR: not recorded in the medical history; RO: right ovary.
Clinical, diagnostic and therapeutic data of the case patients (H. Universitario Virgen de Valme).
| Cases | Weeks of pregnancy at diagnosis | Baseline clinical symptoms | Route of end of pregnancy | Treatment during pregnancy | Radiograph | MRI | Postpartum treatment | Recovery time (months) |
|---|---|---|---|---|---|---|---|---|
| 1 | 30 + 0 | Mechanical left coxalgia | Elective cesarean section at 38 weeks of gestation (Pelvic presentation of the first twin) | Analgesia + rest + LMWH | Osteopenia in both femoral heads (+left), along with minimal suggestive of geodes | Bone marrow edema in the left femoral head and neck, with intra-articular fluid and focal edema in the right femoral head | Arthrocentesis + infiltration + oral corticosteroids + Ca and vit D supplement + JO | 6 |
| 2 | 31 + 0 | Bilateral gonalgia + functional limitation | Elective cesarean section at 34 weeks of gestation (preterm PROM) | Oral corticosteroids + Ca and vit D supplement + analgesia + JO | Bone edema in the right proximal tibial epiphysis and the distal epiphysis of the left femur | Oral bisphosphonates + Ca and vit D supplement + JO | 9 | |
| 3 | 26 + 0 | Bilateral gonalgia + functional limitation | Spontaneous onset of labor at 39 + 0 weeks | Bilateral infiltration + Ca and vit D supplement + analgesia + JO | Bilateral patchy osteoporosis with involvement of both condyles and tibial epiphyses | Bilateral bone edema of femoral condyles (+ ext compartment) + bilateral grade II meniscopathy | Ca and vit D supplement + JO | 1 |
| 4 | Second day postpartum | Mechanical right coxalgia + functional limitation | Spontaneous onset of labor at 34 + 4 weeks | Osteopenia without fracture lines | Bone edema in the right femoral head and very discreetly in the left one | Oral bisphosphonates + analgesia + JO | 2 |
JO: joint unloading; LMWH: low molecular weight heparin; MRI: Magnetic Resonance Imaging; PROM: premature rupture of membranes; vit: vitamin.
Transient osteoporosis of pregnancy is a rare entity, often underdiagnosed, because it presents mechanical pain that is also characteristic of the adaptive changes in pregnancy. It is more frequent in previously healthy women during the third trimester of pregnancy.8,9 It can occur in 2 forms: systemic and regional. The systemic form mainly affects the trabecular bone and, in particular, the spine. Its prevalence is unknown, since some of its predominant clinical manifestations, such as low back pain, are typical in the course of a normal gestation, due to the mechanical overload inherent to pregnancy.10 The regional form, which predominates in our series of cases, usually settles on load-bearing joints, with the most frequent location in the hip, followed by the knee. Bilateral involvement is more exceptional. Nevertheless, in our case series 50% of the patients had bilateral gonalgia, 25% migratory coxalgia and another 25% postpartum right coxalgia (Figs. 1–4).
Its etiopathogenesis is unknown, but several theories have been proposed in the literature: compression of the pelvic nerve, vascular insufficiency with difficult venous return, complex regional pain secondary to repetitive microtrauma, due to weight gain during pregnancy, hormonal changes typical of pregnancy, insufficient intake of calcium and vitamin D before pregnancy, alteration in the regulation of PTH or PTH-related peptide (PTH-RP) or the presence of a previous disease that could favor the alteration of mineral homeostasis.5,6,8,11
It seems a must to open a section to mention a brief physiological reminder about calcium metabolism during pregnancy. It has been established that during pregnancy the maternal organism will transfer a total of 30 g of calcium to the fetus, since it constitutes the amount necessary to complete the fetal mineralization. Furthermore, 80% of that amount will be mobilized during the third trimester. These fetal demands will be satisfied by an increase in intestinal absorption of calcium, mediated by the increase in the circulating concentration of calcitriol, produced by the placenta, the decidua and the fetal and maternal kidneys. Total plasma calcium levels progressively decrease during pregnancy due to an increase in fetal consumption, hemodilution and hypoalbuminemia.12 Hence the importance of starting from adequate levels at the beginning of pregnancy. Unfortunately, in our case series the calcium and vitamin D levels of the patients prior to pregnancy were not available.
As for the role of PTH, there is a panorama that has yet to be defined; the initial hypothesis established that low calcium levels were a persistent inducer of a certain hyperparathyroidism, which increases bone resorption. Today, it is known that the decrease in total plasma calcium is secondary to a state of hypoalbuminemia, while the level of ionic calcium (the only reference for the adjustment of the level of circulating PTH) remains constant. On the other hand, histomorphometric studies have shown a predominance of bone resorption in the first half of pregnancy; however, in the second trimester, when the massive transfer of maternal calcium to the fetus takes place, resorption decreases and bone formation-mineralization increases.6
It has been postulated that gastrointestinal calcium absorption may not be sufficient to meet the demands required for the formation of the fetal skeleton and, therefore, the use of calcium supplements during pregnancy is proposed. In subjects with a low dietary intake of calcium, supplementation could reduce bone resorption and prevent the decrease in bone mineral density that we have observed. However, this issue remains in question, since current evidence indicates that the gastrointestinal tract cannot increase calcium absorption to provide all the requirements demanded by the fetus.13
The diagnosis is of exclusion, since there are various diseases that can simulate transient osteoporosis of pregnancy, such as reflex-sympathetic dystrophy or Südeck’s dystrophy, also known as complex regional pain syndrome, bone marrow edema syndrome and avascular necrosis.6 All of them present with mechanical rhythm pain and bone edema on MRI, so it is necessary to take them into account when making the differential diagnosis.2 In addition to these entities, infections (osteomyelitis, septic arthritis), pigmented villonodular synovitis, stress fractures and neoplasms (metastasis, multiple myeloma, lymphoma or primary bone tumor) should be considered.14
MRI is the imaging test indicated to demonstrate the characteristic edema of the bone marrow of the affected joint, as it is sensitive enough to detect it in the first 48 hours from the onset of symptoms.13 It shows increased signal intensity in fat-suppressed T2-weighted or STIR images and decreased signal intensity in T1-weighted images,6,8 as observed in the images presented in our case series.
The technique of choice for the general study of bone mineral density and osteoporosis is dual-energy X-ray absorptiometry (DEXA), more commonly known as bone densitometry. Its application in pregnant patients is limited by the use of ionizing radiation. A recently emerging technique is radiofrequency echographic multispectrometry (REMS), which could be an alternative to measure bone mass during pregnancy, with high sensitivity and specificity for the detection of healthy, osteopenic or osteoporotic patients, similar to DEXA.14 This novel technique has several advantages that will facilitate its future standardization, since it would not only have application in pregnant patients, but also in pediatrics, in patients at risk of secondary osteoporosis (diabetic, nephropathic, oncological patients), in patients immobilized due to fractures and in home follow-up.14,15
As for treatment, it is based on conservative measures, with unloading of the affected joint, analgesics allowed during pregnancy on demand, and rehabilitation.5,16 Paracetamol is the most commonly used analgesic during pregnancy, since it is generally considered safe, due to its widespread use and the scarcity of documented adverse effects.5 Nonsteroidal anti-inflammatory drugs have been associated with premature closure of the fetal ductus arteriosus and the consequent persistent pulmonary hypertension, fetal nephrotoxicity, and periventricular hemorrhage. As we have mentioned, the supplementation of calcium and vitamin D is in question,13 as well as the use of both intra-articular and systemic corticosteroids since, despite reducing the clinical symptoms, they can be risk factors for osteoporosis itself, so it is necessary to individualize it in each case.17 Prophylaxis of deep vein thrombosis with LMWH may also be considered on an individual basis because of the increased risk due to pregnancy itself and the rest for joint unloading.5
Despite the spontaneous resolution of the condition, the literature has described the use of antiresorptive treatment with bisphosphonates, which have been shown to be effective in the described cases of transient osteoporosis not related to pregnancy. They should not be used during pregnancy, as they are considered category C by the Food and Drug Administration (FDA) and can be associated with fetal loss, labor dystocia, visceral alterations (renal pelvis and ureters syndrome), low weight and alterations in fetal ossification.1,6,17 However, they can be incorporated into the treatment during the puerperium, since they present a low risk for breastfeeding.
Finally, there are no randomized clinical trials or large case series that support these therapeutic decisions,6,18 so we rely on expert opinions and on the experience in daily clinical practice. Generally, it is usually a self-limiting process after childbirth, with resolution of the clinical picture within a period of 2–12 months.9,18 In our case series, all patients had a favorable evolution towards complete resolution without sequelae within 2–9 months.
ConclusionTransient osteoporosis of pregnancy is a rare and underdiagnosed entity, which can lead to a significant functional limitation that hinders the basic activities of daily life of patients. Its presentation in the third trimester of pregnancy represents a diagnostic and therapeutic challenge for the clinician, since some complementary tests or drugs may not be recommended during pregnancy. Its etiology is unknown, although several theories have been proposed. Likewise, different treatments have been proposed, but the effects on the mother and fetus and the breastfeeding newborn must be considered. The first-line treatment consists of analgesics and unloading of the affected joint. In general, it usually presents a self-limited clinical picture with complete recovery in a period of 2–12 months.
Ethical considerationsGiven the descriptive nature of the cases and the bibliographic review on the subject, authorization from the Bioethics Committee has not been necessary, as no action was taken on the patients, in the same way that no external funding has been received. The images presented are part of the clinical study conducted by the Andalusian Health Service and for their use, as well as for all the clinical data reflected in this article, prior informed consent has been required from each of the patients.
Conflict of interestThe authors declare that they have no conflict of interest.