Point-of-care abdominal ultrasound (US) has emerged as a powerful tool for clinicians and is becoming a routine bedside tool to rapidly diagnose, manage hemodynamics, monitor fluid status, and guide procedures in emergency and critical care. Extended focused assessment with sonography for trauma (eFAST), is commonly used to detect free intraperitoneal blood in the trauma setting and may also be an option in non-trauma patients. However, it has significant limitations for detecting gastrointestinal or retroperitoneal bleeding. To date, there is no US protocol described for the diagnosis of occult bleeding in the retroperitoneal space. We describe a new US protocol called “Ultrasound For Occult Hemorrhage” (UFOH) for a fast diagnosis of occult hemorrhage. The UFOH protocol is a novel ultrasound-guided approach designed to detect occult bleeding in various clinical settings, including emergency department, intensive care and perioperative environment.
La ecografía abdominal como «point of care», en el punto de atención, ha surgido como una herramienta potente para los clínicos, habiéndose convertido en una herramienta rutinaria a pie de cama para diagnosticar, manejar la hemodinámica, supervisar el estado de los líquidos y guiar los procedimientos de urgencias y cuidados críticos. Se utiliza comúnmente Extended Focused Assessment with Sonography for Trauma para detectar sangre libre intra-peritoneal en el ámbito traumático, pudiendo ser también una opción en los pacientes no traumáticos. Sin embargo, tiene limitaciones significativas para la detección de la hemorragia gastrointestinal o retroperitoneal. Hasta la fecha, no existe ningún protocolo ecográfico des-crito para el diagnóstico de la hemorragia oculta en el espacio retroperitoneal. Describimos un nuevo protocolo ecográfico denominado Ultrasound For Occult Hemorrhage para el diagnóstico rápido de la hemorragia oculta. Dicho protocolo es un nuevo enfoque ecográfico diseñado para detectar el sangrado oculto en diversos ámbitos clínicos, incluyendo los servicios de urgencias, cuidados intensivos y el entorno perioperatorio.
Point-of-care ultrasonography (POCUS) is a validated clinical technique that is performed and interpreted in real-time by the attending physician at the bedside. It is used for screening and procedural guidance.1 Several medical associations have recommended ultrasound for diagnostic and procedural assessment.2 In a recently published multicentre, prospective cohort 1-day study at 142 ICUs in France, 1073 POCUS explorations were performed in 709 patients in one day, of which 10% were abdominal ultrasounds.3 In this cohort study, the diagnostic and therapeutic impact of diagnostic POCUS examinations were 84% and 69%, respectively.
Abdominal ultrasound examination to detect free intraperitoneal fluid in the trauma setting, known as focused assessment with sonography for trauma (FAST), was first described in an international consensus conference in 1996.4 This US evaluation technique focused on scanning trauma patients for free fluid in four areas: the right upper quadrant, left upper quadrant, pelvis, and pericardium. Its sensitivity ranged from 62% to 96% and specificity from 87% to 99%,5 with an associated significant reduction in CT needs, costs, and complication rates, as well as a substantial reduction in time to surgical intervention.6 However, the FAST examination is not a comprehensive evaluation of all the possible sources of bleeding in a critically ill patient. It does not include the pleural space (currently included in the E-FAST protocol6) or the gastrointestinal or retroperitoneal area, which are known to be the source of critical bleeding and haemorrhagic shock in the non-trauma setting.7
Retroperitoneal bleeding is an uncommon, life-threatening condition, and gastrointestinal bleeding is a frequent cause of ICU admission. Both origins of bleeding can produce clinically occult bleeding leading to haemorrhagic shock, which can have devastating consequences. Bleeding can occur in any part of the gastrointestinal system or retroperitoneal structures, such as the pancreas, duodenum, adrenal glands or kidneys. Survival of these patients depends on rapid and accurate diagnosis and prompt institution of resuscitative and therapeutic measures.8 US, which has already proven invaluable in other emergency and critical care situations, can be a valuable aid in this context.9
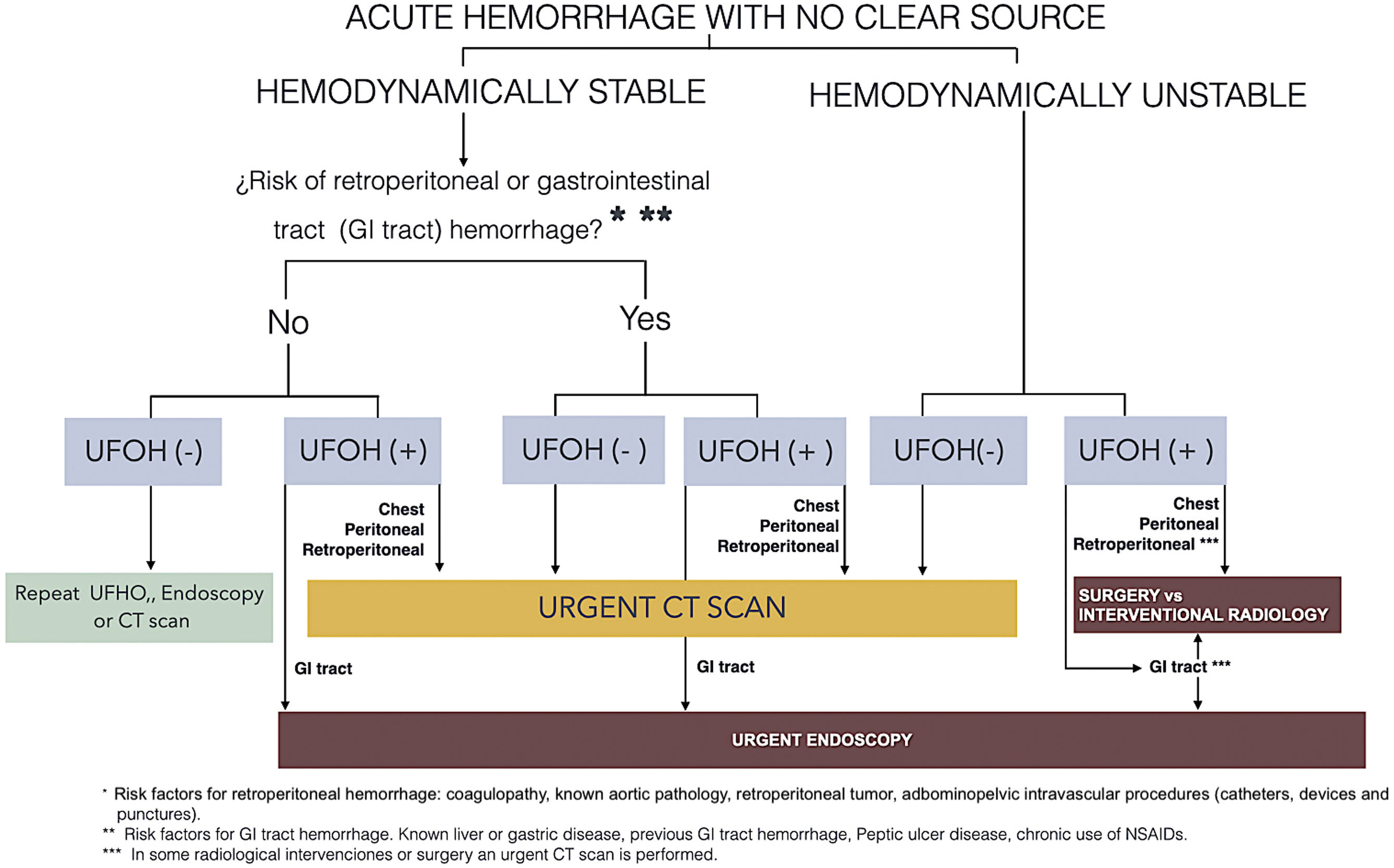
This article describes a new approach to comprehensive, systematic US evaluation of the origin of bleeding in an acute/emergency setting. This new protocol is called Ultrasound For Occult Hemorrhage (UFOH), and has been included in “the acute hemorrage with no clear source algorithm” (Fig. 1).
This protocol is effective in detecting occult bleeding in stable and unstable patients, considering haemorrhage risk factors. The algorithm outlines actions based on the bleeding site (UFOH (+)): thorax, peritoneum, retroperitoneum, or digestive tract. A negative result (UFOH (−)) in patients with risk factors (e.g., coagulopathy, intravascular procedures) requires urgent CT or endoscopy. Bleeding (UFOH +) is identified by imaging findings such as haematoma, clot, or abnormal free fluid in a structure that appears normal on POCUS.
We are aware that this protocol requires an advanced level of abdominal ultrasound skills. However, since it includes the same ultrasound techniques as those taught and used in POCUS, with the addition of a systematic visualisation of the retroperitoneum, we believe it can be performed by any trained specialist.
Description of the UFOH protocolIn the UFOH protocol, ultrasound scanning is performed with a 2.5–5 MHz convex or multiplane probe in the abdomen of a supine patient. The probe is held with the dominant hand rather like a dagger and moved from top to bottom (Fig. 2) as many times as necessary following a dynamic system of 3 extended zones with 3 well-defined stations (Figs. 3–5). The depth and gain of the image should allow the operator to visualise structures up to the posterior musculoskeletal muscles (spine, psoas muscles, and iliac bone). The pressure exerted on the abdominal wall should be sufficient to obtain the best image and displace the intestinal air that diminishes image quality. It is essential to visualise both psoas compartments to rule out psoas haemorrhagic pathology and its relationship with all retroperitoneal structures, especially vascular structures.
The photo shows the recommended way of holding the transducer (like a dagger) to scan the lateral zones of the UFOH protocol. The transducer is moved towards the pelvis along the path of the psoas muscles (see Stations 2 and 3).
To make this protocol easier to understand, we have decided to follow the method used by our ultrasound teaching group in our abdominal ultrasound workshops and divide it into 3 different stations.
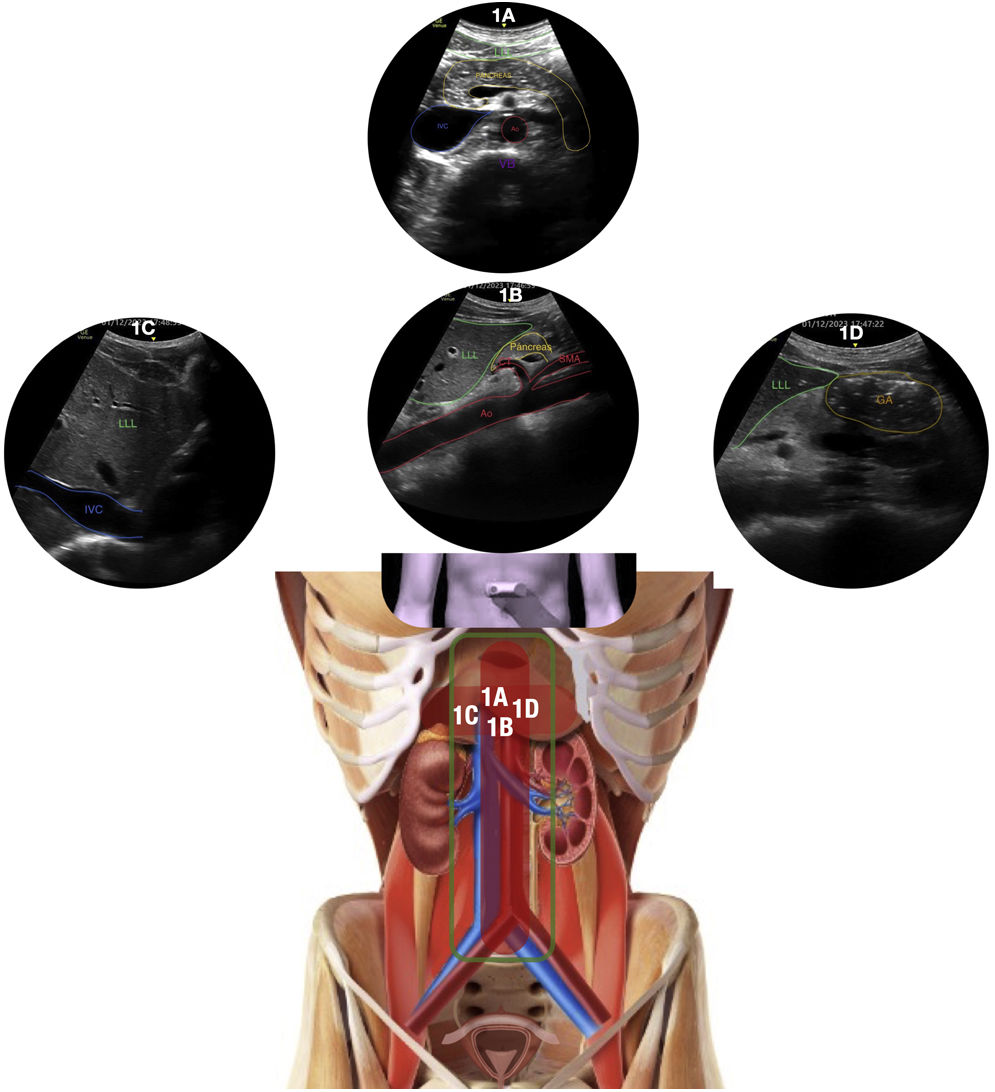
Station 1 (see Fig. 3 for summary)Station 1AThe UFOH examination protocol starts in the central zone (Zone 1) of the large vessels. The transducer is positioned transversally to visualise the abdomen, similar to a CT scan in the coronal view. After evaluating the heart through the standard subcostal view to initially determine the possible cause of shock, the transducer is placed in the 9 o’clock position in the epigastric area in a transverse or axial plane to visualise the large abdominal vessels, which include the aorta (Ao) and inferior vena cava (IVC) (Station 1A). Examination in the central zone is performed from the initial epigastric area down to the division of the aorta in its two iliac arteries. The probe should be moved smoothly and continuously, exerting pressure as described above. The aim of the examination in Station 1A is to identify heterogeneous or anechoic masses compatible with haematoma or bleeding related to aorta pathology (aneurysm or dissection rupture) and free fluid between bowel loops.
Station 1B, 1C and 1DFollowing our protocol, the next step is to move the probe back up to the epigastric region. The transducer is placed in the 12 o’clock position in a sagittal or longitudinal plane to obtain a longitudinal view of the aorta and identify aortic pathology (Station 1B). Slightly tilting or moving the probe to the right will show the longitudinal plane of the IVC (Station 1C). Slightly tilting or moving the probe to the left will show the gastric antrum below the left hepatic lobe in a sagittal or longitudinal view, appearing as a ring shape due to its wall and low fluid content (Station 1D). In this gastric antrum view, the operator should look for abnormal gastric content, either due to increased volume or atypical density characteristics, such as heterogeneous content suggesting blood.Station 1A
The aorta (Ao) and inferior vena cava (IVC) are shown in a transverse epigastric plane, in front of a lumbar vertebral body (VB) and behind the pancreas (Pancreas) below the left liver lobe (LLL) as part of the retroperitoneum. (See clip 1A in Supplementary material).
Station 1BThe image show the aorta (Ao) in a sagittal plane at the epigastric level, with its main branches (celiac trunk [CT] and superior mesenteric artery [SMA]), and below, the left liver lobe (LLL) and the head of the pancreas in the midline. (See clip 1B in Supplementary material)
Station 1CThe image shows the inferior vena cava (IVC) in an epigastric sagittal plane. This image is obtained by moving the transducer a few centimeters to the patient’s right from Station 1B. (See clip 1C in Supplementary material)
Station 1DThe image shows the gastric antrum (GA) in a short circular axis, very close to the left liver lobe (LLL) in a sagittal epigastric plane moving to the patient’s left from 1A station. (see clip 1D in Supplementary material)
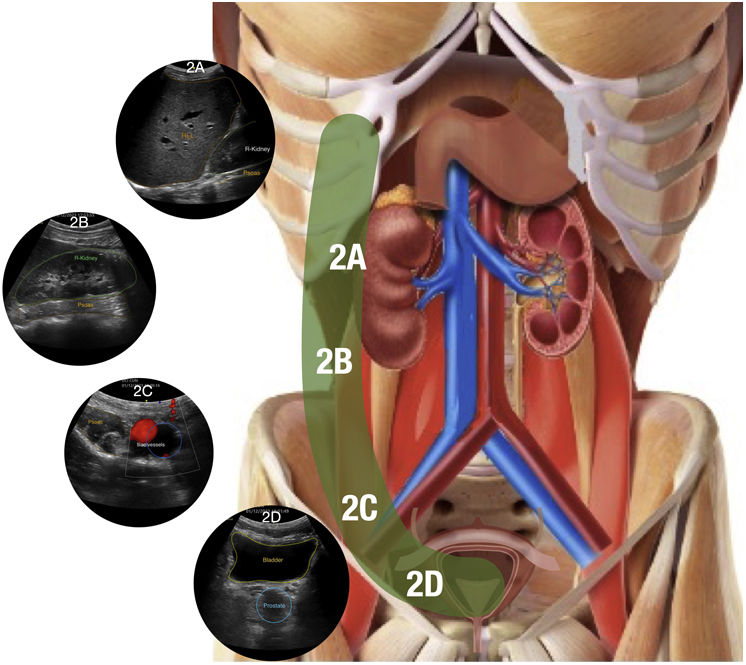
Station 2 (see Fig. 4 for summary)Zone 2 starts by placing the transducer in the 12 o'clock position on the right and slightly lateral to the hypochondrium to visualise the liver, diaphragm, and lower right chest, searching for signs of both abdominal and thoracic bleeding (Station 2A). The transducer is then moved approximately 4−5 cm down towards the axillary midline to visualise the right kidney on the proximal portion of the iliac-psoas muscle (Station 2B). From Station 2B, the transducer should be moved downward and slightly laterally following the colonic framework while exerting pressure to follow the iliopsoas muscle in the sagittal plane until the ilio-pelvic area is visualised in a transverse oblique plane (Station 2C). The probe should be at a depth of approximately 5−6 cm. It is then tilted to the right side to identify a posterior linear structure (iliac bone) related to the iliopsoas muscle and the iliac vessels are visualised in a transverse or axial plane. From Station 2C, the probe is moved medially, aiming to follow the bladder in a transverse or axial plane and its relationship with its diverticulum (Station 2D).Station 2A
The right diaphragm, right liver lobe (RLL), upper portion of the right kidney (R-Kidney) and ipsilateral psoas muscle are shown in a sagittal-oblique plane of the right hypochondrium. (see clip 2A in Supplementary material)
Station 2BThe lower portion of the right kidney (R-Kidney) resting on the medial region of the ipsilateral psoas muscle is shown in an oblique sagittal plane in the right flank area. (see clip 2B in Supplementary material)
Station 2CThe iliac vessels (red & blue) resting on the psoas-iliac muscle are shown in a transverse oblique plane in the right hypochondrium. The hyperechogenic line is the iliac bone. The image is optimized by pressing the transducer to displace and air in the cecum that may obstruct the view. (see clip 2C in Supplementary material)
Station 2DThe bladder and prostate are shown in a transverse plane in the hypogastrium. (see clip 2D in Supplementary material)
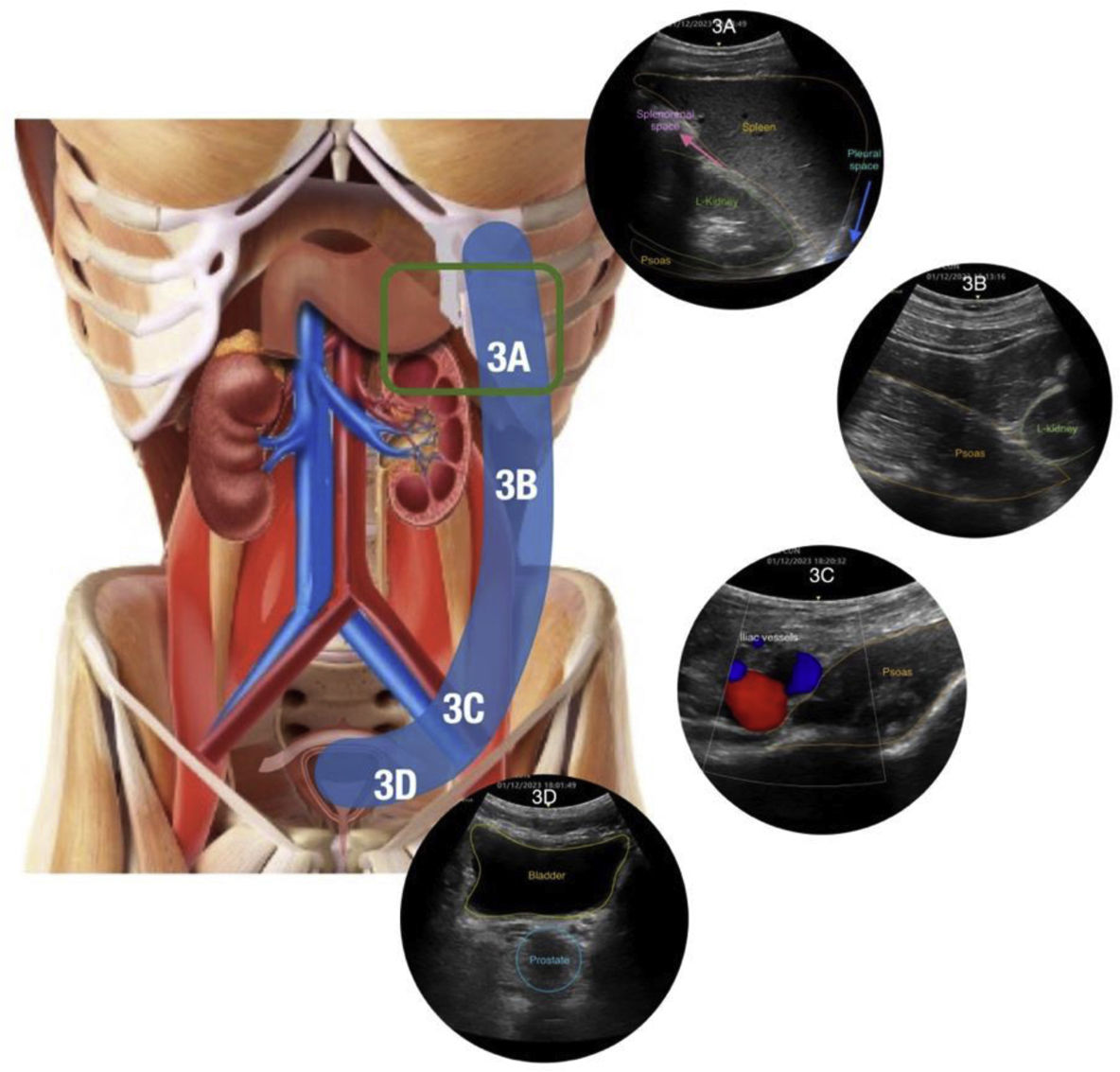
Station 3 (see Fig. 5 for summary)In Zone 3, the left flank is explored in a similar way to Zone 2 on the right side. Zone 3 exploration should be initiated with the transducer in the 12 o’clock position in the longitudinal or sagittal plane, slightly posterior to the left flank.
The spleen is more cephalic than the liver but closely related to the upper pole of the ipsilateral kidney. As it appears on the right side, the iliopsoas muscle is used as a reference due to its association with other structures. In the first view of Station 3 (3A), the presence of content in the gastric fundus may be observed by tilting the probe anteriorly and posteriorly. The gastric fundus is closely related to the diaphragm, spleen, and left kidney. The station where the diaphragm, spleen, left kidney, and gastric fundus are observed is called Station 3A extended (green square in Fig. 4). The transducer is then moved approximately 4−5 cm down towards the midaxillary line to visualise the left kidney on the proximal iliopsoas muscle (Station 3B). From Station 3B, the transducer is moved down laterally following the colonic framework while exerting pressure to follow the iliopsoas muscle sagittally or longitudinally until the ilio-pelvic area is visualised. The probe should be at a depth of approximately 5−6 cm. It is then tilted to the left to identify a posterior linear structure (iliac bone) concerning the iliopsoas muscle and the iliac vessels in a transverse or axial plane (Station 3C). From Station 3C, the probe is moved medially, aiming to visualise the bladder in a transverse or axial plane and its diverticulum (Station 3D).Station 3A
The left diaphragm, the spleen and the upper portion of the ipsilateral kidney (L-Kidney) are shown in a high coronal section; the proximal portion of the left psoas muscle may also be visualised. (see clip 3A in Supplementary material).
Station 3BThe lower pole of the L-Kidney and a large portion of the proximal psoas muscle on which it rests are visualised. (see clip 3B in Supplementary material).
Station 3CThe iliac vessels (red & blue) resting on the psoas-iliac muscle are visualised in a transverse oblique plane in the left hypochondrium area, similar to the contralateral Station (2C). The hyperechogenic line posterior to the muscle is the left iliac bone (see clip 3C).
Station 3DThe bladder and prostate are visualised in a transverse plane in the hypogastrium. (see clip 3D in Supplementary material).
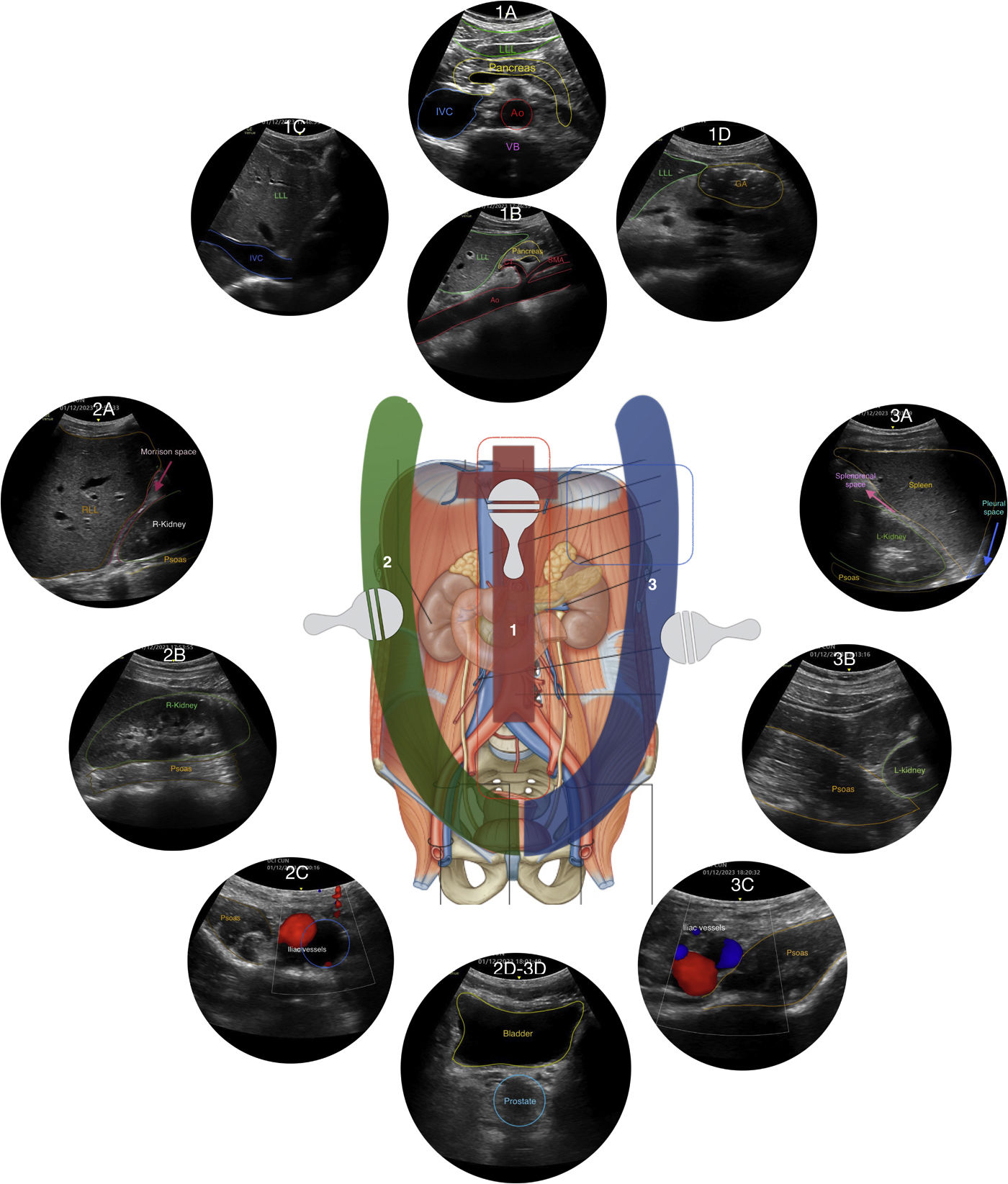
In summary, our protocol comprises: 1) an extended upper abdominal examination including: heart, IVC, stomach, pancreas, abdominal aorta and bilateral proximal psoas muscles. 2) an extended right flank examination including: thorax-lung-pleura, hepatorenal, psoas muscle, iliac vessels, pelvis and bladder. 3) an extended left flank examination including: thorax-lung-pleura, splenorenal recess, stomach (fundus), psoas muscle, iliac vessels, pelvis and bladder. An overview of all stations is shown in Fig. 6.
Overview of all stations of the Ultrasound For Occult Hemorrhage (UFOH) protocol (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.).
Abbreviations: Ao: aorta; SMA: mesenteric superior artery; LLL: left liver lobe; IVC: inferior vena cava; VB: vertebral body; RLL: right liver lobe; GA: gastric antrum; R-Kidney: right kidney; L-Kidney: left kidney; Red: iliac artery; Blue: iliac vein.
We use this protocol routinely in our intensive care unit to detect retroperitoneal bleeding with excellents results. Now, to recap and show the potential and usefulness of the UFOH protocol described in this article, we present 3 cases that illustrate the clinical utility of the UFOH protocol for the diagnosis of occult abdominal bleeding that cannot be detected with the eFAST protocol.
Case 1 (see Fig. 7 for summary)A 67-year-old woman was admitted to the ICU with mechanical circulatory support using central venoarterial extracorporeal membrane oxygenation (VA-ECMO) secondary to acute coronary syndrome complicated by cardiogenic shock refractory to standard therapy.
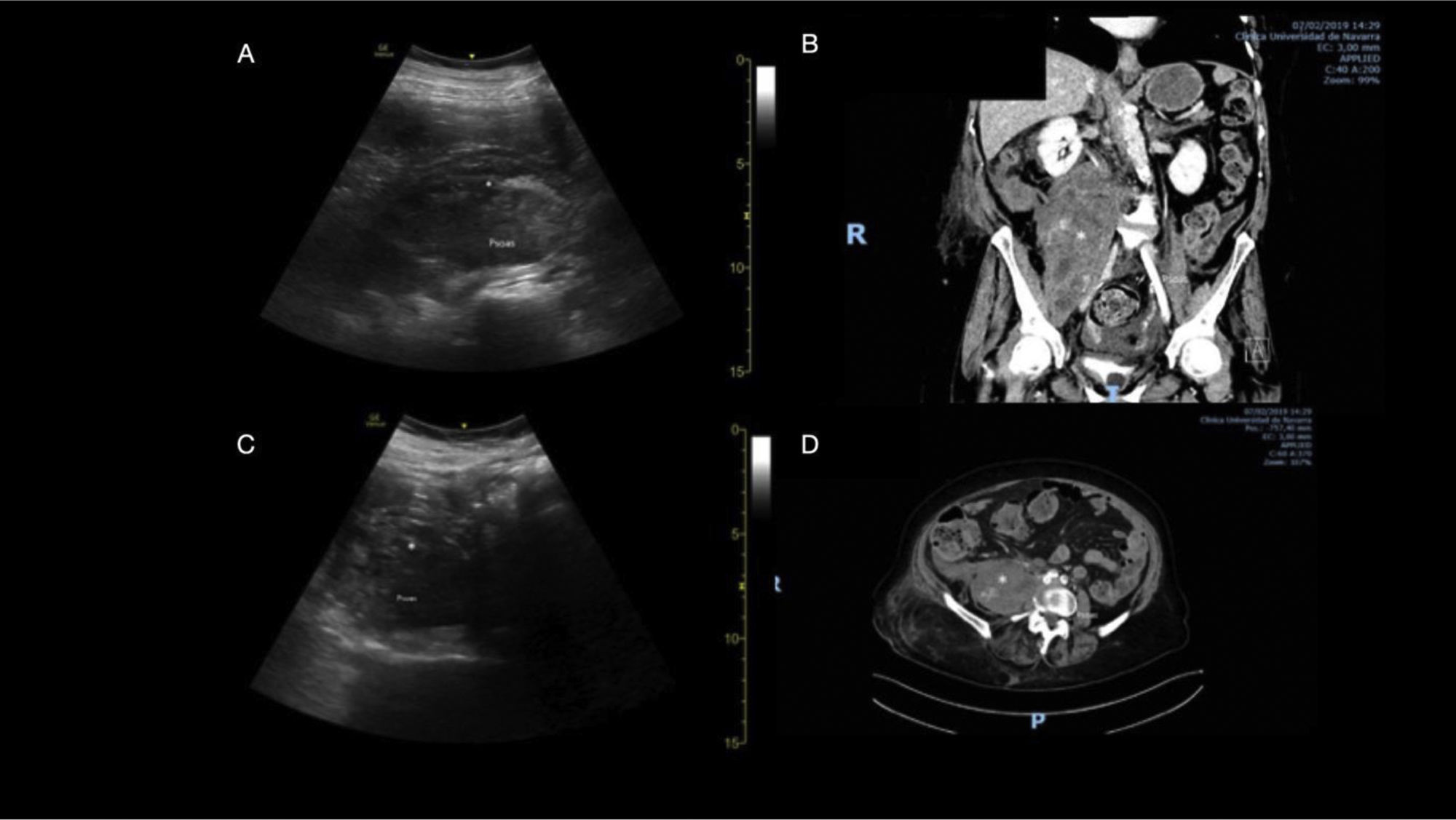
During her ICU stay, her haemoglobin slowly decreased, requiring blood transfusion. After 10 days, she presented an episode of severe haemodynamic instability due to hypovolaemia, requiring fluid resuscitation and blood transfusion. We performed a bedside US study following the UFOH protocol described in this article, which allowed us to identify a large haematoma on the right iliopsoas muscle as the cause of bleeding (Fig. 7A and C). After haemodynamic stabilization, the patient was transferred for a CT scan, which showed a large haematoma on the right iliopsoas muscle, confirming the UFOH findings (Fig. 7B and D). An urgent embolization was successfully performed.
US and CT scan showing a large haematoma on the right iliopsoas muscle.
A: Right zone 2 of the UFOH protocol Station 2B (sagittal plane) (see clip 4A in Supplementary material). A large haematoma on the right iliopsoas muscle is observed on ultrasound (US) following the UFOH protocol Station 2B. (*) Note the unstructured and heterogeneous image of the anterior portion of the psoas muscle.
B: A large haematoma on the right iliopsoas muscle, actively bleeding, is confirmed by CT angiography, coronal view (*).
C: Right zone 2 of the UFOH protocol Station 2B (transverse plane in the right flank area) (see clip 4B in Supplementary material). A large haematoma on the right iliopsoas muscle is observed on US.
D: The presence of a large haematoma on the right iliopsoas muscle is confirmed by CT angiography, transverse view.
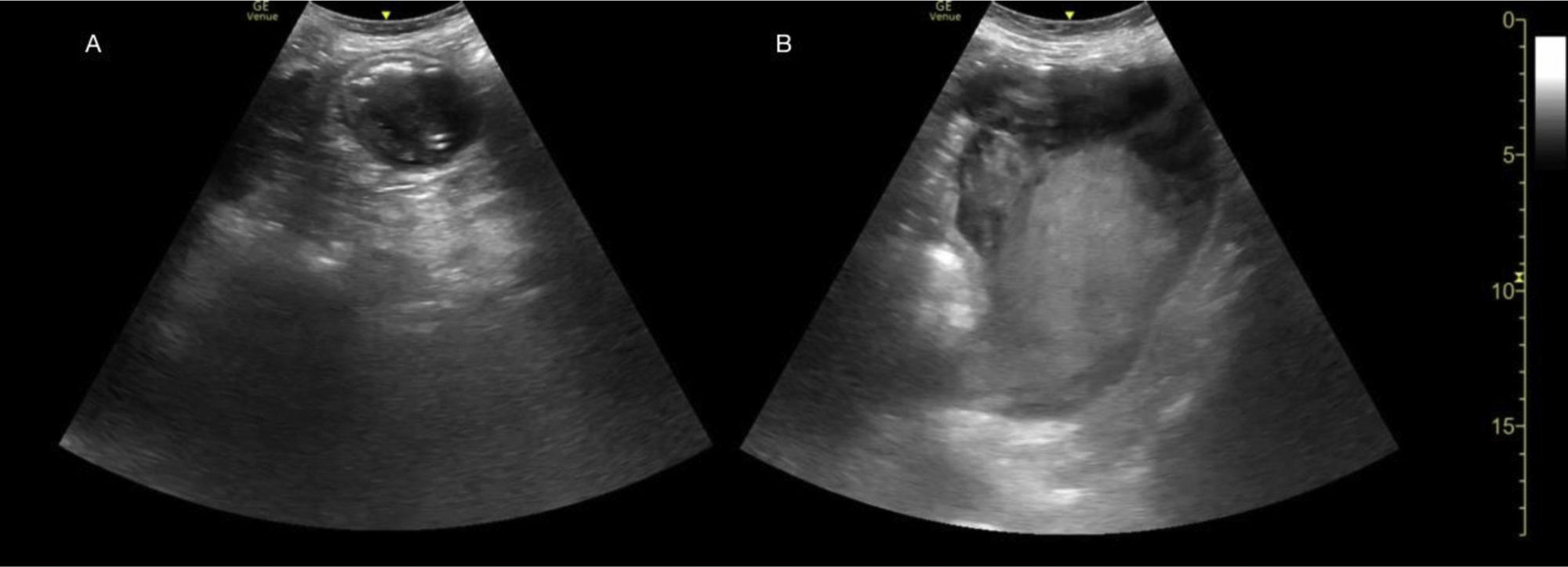
A 35-year-old woman was admitted to hospital due to severe upper abdominal pain. No significant findings were observed in the initial physical examination. Analgesics were prescribed, but produced no pain relief. The patient was later transferred to the ICU due to a syncopal episode associated with haemodynamic instability. We performed a US study following our UFOH protocol, which revealed heterogeneous content in the gastric antrum compatible with a large clot (Fig. 8A, B). An emergency upper endoscopy was performed, and a Forrest IIa peptic ulcer with an adherent clot suggesting signs of recent bleeding was observed, confirming the initial ultrasound findings. In this case, the UFOH protocol was able to diagnose gastrointestinal bleeding secondary to nonsteroidal anti-inflammatory drugs (NSAIDs).
Central zone 1, Station 1D (sagittal or longitudinal plane) of the UFOH protocol. Transducer placed at 11 o’clock. A: A heterogeneous content is observed in the view of the gastric antrum (*) (see clip 5A). This is compatible with blood or clot in a patient who developed gastrointestinal bleeding secondary to the use of nonsteroidal anti-inflammatory drugs (NSAIDs). LLL: left lobe of the liver. B: Blood or clots (*) are observed in the gastric fundus in an oblique subcostal view (see clip 5B).
A 17-year-old girl in the early postoperative period following orthotopic liver transplantation for fulminant hepatic failure secondary to toxic overdose developed a progressive increase in transaminase levels. US showed signs of hepatic artery stenosis requiring an endovascular procedure. The procedure was performed under local anaesthesia. After balloon dilatation was completed, two stents were inserted in the hepatic artery due to significant arterial tortuosity, with good results. Post-procedure management varies widely between centres, but generally includes a course of anticoagulation and/or antiplatelet therapy and imaging of the treated vessel for assessment of restenosis over the following 24 h. In our case, 3000 IU of heparin and 900 mg of i.v. lysine-aspirin solution (equivalent to 0.5 g acetylsalicylate acid) were given throughout the procedure.
Over the following 48 h, her red blood cell count fell sharply, despite no obvious source of bleeding. Our UFOH protocol was performed and revealed a right iliopsoas haematoma and findings suggestive of new-onset haemorrhagic ascites (Fig. 9A and C). Diagnostic paracentesis was performed, and a CT scan confirmed the findings observed on the UFOH examination (Fig. 9B and D). The patient made a good recovery with a conservative approach, including blood transfusion and withdrawing heparin treatment.
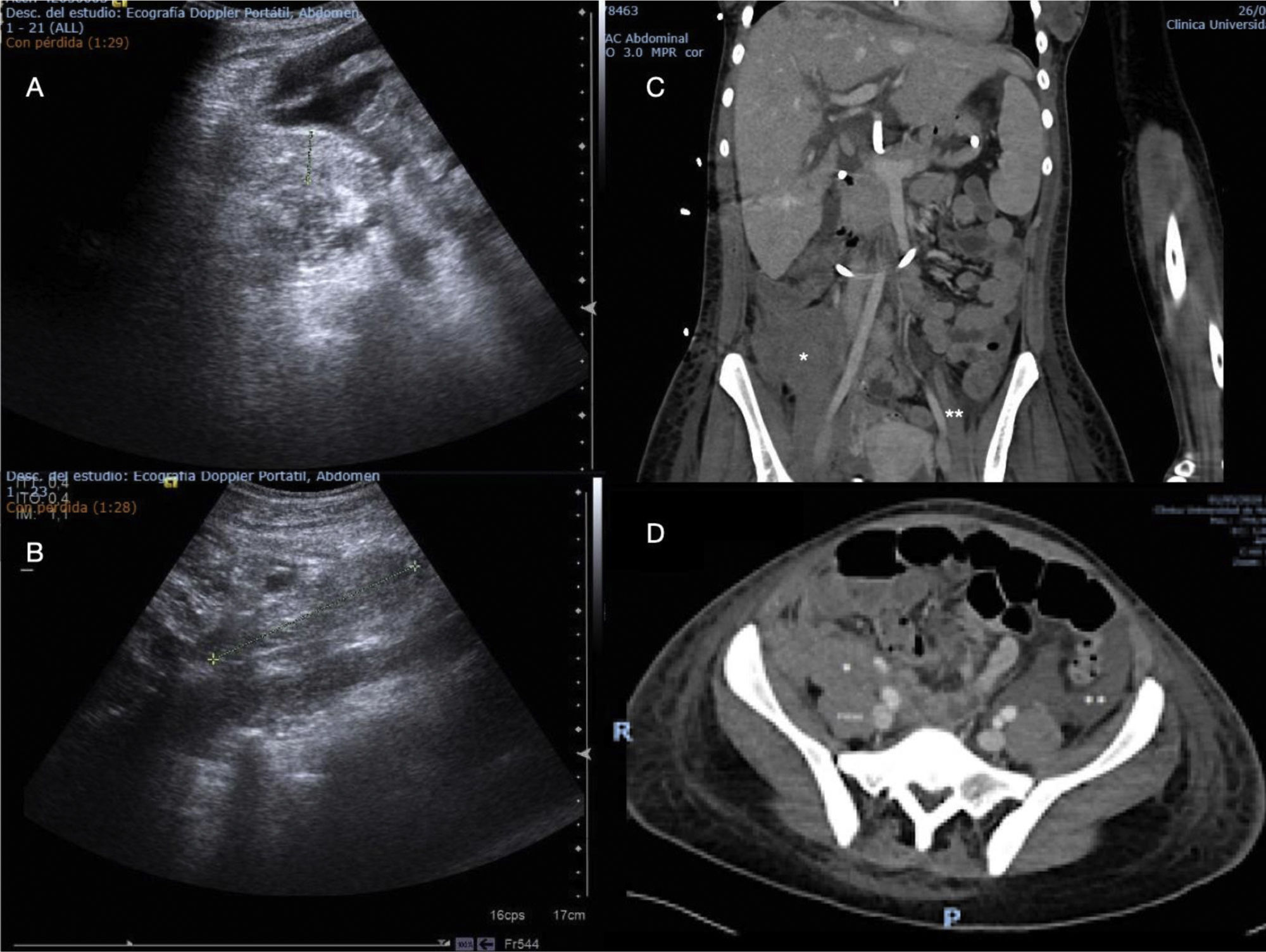
Right zone 2, Station 2B y 2C (sagittal and transverse plane) of the UFOH protocol and CT angiography showing a haematoma on the psoas muscle.
A. Right zone 2 (Station 2C) in a transverse oblique plane of the UFOH protocol. A haematoma measuring 18.2 mm anterior to the psoas muscle and haemorrhagic ascites were observed in a patient with a liver transplant.
B: Right zone 2 (Station 2B) of the UFOH protocol (sagittal plane). A psoas muscle haematoma is observed in a patient with liver transplant. Note the ovoid image measuring 93.6 mm in the anterior portion of the psoas muscle. (see clip 6 in Supplementary material).
C. The presence of a haematoma on the psoas muscle (*) compressing part of the right common iliac artery, in a coronal view, is confirmed by CT angiography.
D. The presence of a haematoma on the psoas muscle (*) and ascites (**) is confirmed by CT angiography.
Since the introduction of the FAST protocol which is performed at the bedside, there have been considerable advances in the understanding, teaching and certification of point-of-care ultrasound. Ultrasound has emerged as the most valuable aid for clinicians in all fields of medicine, but especially in anesthesiology, critical care and emergency medicine.
The new protocol described here was developed to meet the need for a systematic, comprehensive, easy-to-use US-focused examination in patients with bleeding with no obvious initial source—a common problem in intensive care. The technique has been useful in our clinical practice, as illustrated by our case series, and because it can be immediately and easily performed, ongoing resuscitation treatment does not need to be interrupted, thus saving time and optimizing the resources available for complex patients (case No. 1).
There is extensive experience with FAST and E-FAST protocols in trauma. However, the objective of the FAST protocol is to detect the presence of abdominal free fluid, but not to define the origin of this bleeding. The clinical context will define further diagnostic tests and therapeutics. In the critical care setting, the cause of haemodynamic instability or anaemia may be multifactorial. Patients in shock or with rapidly developing anaemia often show no obvious source of bleeding.10 Occult upper gastrointestinal haemorrhage and retroperitoneal bleeding may be the cause of shock or occult bleeding; however, they are not a target of existing point-of-care ultrasound techniques, despite evidence that both the retroperitoneal space and upper gastrointestinal bleeding can be visualised on ultrasound.11–15 Mechanical circulatory devices are increasingly being utilized for both acute and chronic heart failure, and retroperitoneal bleeding is a serious complication.
The UFHO protocol aims to combine the simplicity of the E-FAST protocol with a more comprehensive, standardized examination of the pleural space, abdominal cavity, and retroperitoneal space that extends the search for the origin of the bleeding. It adds a quick but full study of the infradiaphragmatic aorta up to the iliac arteries in order to identify perivessel bleeding suggestive of aneurysm/dissection. IVC visualisation may add a further element to the somewhat limited differential diagnosis of haemodynamic shock.6 To identify the source of occult bleeding, which is common in critically ill patients with coagulopathy, complex procedures, or instrumentation, abdominal ultrasound findings should be considered together with the findings of the physical examination of the stomach and retroperitoneal space and the results of blood tests.
The UFOH protocol is designed to be performed rapidy using 3 scanning trajectories to systematically visualise the great vessels (aorta, iliac arteries and inferior vena cava) and the mid-abdomen in search of free fluid in the following spaces: between intestinal loops, inferior pleural cavities and subdiaphragmatic spaces, the hepatorenal and splenorenal recesses, and the retroperitoneal space up to the pelvic fossa. It is a structured, systematic approach to identify free fluid as the origin of anaemia and haemodynamic instability, especially when bleeding is suspected or confirmed but has no obvious source.
Early clinical experience has been promising, but further evaluation is needed before the protocol can be widely introduced.
In our opinion, our protocol has several strengths. First, it includes ultrasound skills frequently taught and used (FAST, E-FAST, basic cardiac, vascular, and gastric ultrasound), adding the systematic approach to visualise the retroperitoneum. Abdominal and kidney ultrasound is becoming increasingly used, and like interfascial plane blocks it requires good knowledge of the anatomy of the abdominal and retroperitoneal space. Second, the technique includes only a few continuous movements, which simplifies ultrasound exploration of a large area. For teaching purposes, we have defined just a few stations with clear images to ensure that all the structures of interest are visualised. Third, this approach does not replace other imaging modalities or diagnostic tests, but provides clinicians with an additional diagnostic tool in a bleeding/shocked patient that may be performed concomitantly with other diagnostic and urgent therapeutic procedures. Fourth, we have developed an algorithm to help organize a structured approach to a bleeding patient with no obvious source of bleeding. Fifth, although designed for intensive care, the UFOH protocol can also detect occult bleeding in other scenarios, including post-invasive procedures such as peripheral extracorporeal membrane oxygenation (ECMO) implantation, especially in patients with coagulopathies or anticoagulant therapy.
Our protocol also has several limitations. First, while it relies on basic ultrasound skills, specific advanced abdominal ultrasound training will also be needed. Second, the UFHO protocol is limited to evaluating the potential cause of haemodynamic shock, which requires more advanced functional echocardiographic monitoring.14 Finally, and most importantly, more data, especially from other centres, are needed to assess its impact on decision-making and clinical outcomes. Accordingly, we plan to perform a multicentre prospective cohort study to determine the usefulness of the UFHO protocol in a real-world clinical setting.
ConclusionThe UFOH protocol is a novel ultrasound-guided approach to detect occult bleeding in various clinical settings, including emergency care, critical care, and perioperative environments. In patients with unexplained haemorrhagic shock, the UFOH protocol may play an important role in identifying unknown sources of abdominal bleeding, thereby facilitating prompt diagnosis, differential diagnosis, and management. By incorporating a point-of-care US examination of the retroperitoneal space, the UFOH protocol provides a comprehensive assessment and has the potential to become a valuable tool that will improve care quality in emergency and critical care settings.
M. Vivesj, J. Mercadall, A. Hernándezk, D. González-Delgadoj, P. Carmonam, X. Borratk, D. Nagoren, E. Sánchezo, M. Sernap, P. Cuestaq, U. Bengoetxear
j Department of Anesthesiology & Critical Care, Clínica Universidad de Navarra, University of Navarra, Navarra, Pamplona, España
k Department of Anesthesiology & Perioperative Medicine, Policlínica Ibiza Hospital, Ibiza, España
l Department of Anesthesiology & Critical Care, Hospital Clínic de Barcelona, University of Barcelona, Barcelona, España
m Department of Anesthesiology & Critical Care, Hospital Universitario La Fe, Valencia, España
n Department of Anesthesiology & Critical Care, Barts Heart Center, Barts Health NHS Trust, Londres, Reino Unido
o Department of Anesthesiology & Critical Care, Hospital Gregorio Marañón, Madrid, España
p Department of Anesthesiology & Critical Care, Hospital Universitario de Denia, Denia, Alicante, España
q Department of Anesthesiology & Critical Care, Hospital Universitario de Albacete, Albacete, España
r Department of Anesthesiology & Critical Care, Hospital de Urduliz, Urduliz, Vizcaya, España.