It may be necessary a consideration about the best approach to the acute concomitant problems that critical COVID-19 patients can develop. They require a rapid diagnosis and an early treatment by a multidisciplinary team. As a result, we would like to describe two clinical cases a patient with diagnosis of COVID-19 pneumonia with good respiratory evolution that, after extubation suffered an acalculous cholecystitis and a patient with COVID-19 pneumonia that suffered an overinfection with necrotising pneumonia that presented with haemoptysis and was finally treated with arterial embolisation by the interventional radiologist’s team.
Puede ser necesaria una reflexión sobre cuál es el mejor abordaje para las enfermedades agudas concomitantes que pueden desarrollar los pacientes críticos con COVID-19. Estos requieren una sospecha diagnóstica y un tratamiento precoz, basados en el trabajo de equipos multidisciplinares. Presentamos dos casos de enfermedades concomitantes en pacientes con COVID-19. Un paciente diagnosticado de COVID-19 con buena evolución respiratoria que tras extubación presentó una colecistitis acalculosa y un paciente con neumonía por COVID-19 que presentó una sobreinfección con neumonía necrotizante, cuyo primer síntoma fue hemoptisis y fue finalmente tratado con embolización arterial por radiología intervencionista.
The treatment of respiratory failure, inflammatory response and hypercoagulability are the main therapeutic challenges in patients with COVID-19 admitted to critical care units (CCU). The basic principles of critical care must be taken into consideration1 when deciding the best approach to the different acute and serious problems of patients with COVID-19. Due to its complexity and severity, it is not surprising that these patients may develop other concomitant diseases typical of CCU patients, such as thromboembolic events,2 acute kidney injury, or secondary infections such as necrotizing pneumonia or acalculous cholecystitis.3–5 The overall mortality rate of 31% described in Spanish series is higher in patients with these complications.3 We describe 2 cases of complications that occurred in critically ill patients admitted for COVID-19.
Case 1A 65-year-old man admitted to the hospital after 10 days of fever, cough, and dyspnoea. His medical history was significant for: allergy to aspirin and NSAIDs, former smoker, and high blood pressure under treatment with enalapril. The chest X-ray on admission showed bilateral interstitial infiltrates. After SARS-CoV-2 was detected by polymerase chain reaction (PCR), treatment with hydroxychloroquine, lopinavir/ritonavir, amoxicillin-clavulanate, and interferon beta was started. On the fourth day of admission, he presented clinical worsening with tachypnoea of up to 45 breaths per minute and SaO2 80% despite non-invasive mechanical ventilation (NIMV) with a high fraction of inspired oxygen. Orotracheal intubation was performed without complications in the CCU. Following this, and after recruitment manoeuvres, it was decided to ventilate in the prone position. Treatment with a single dose of tocilizumab and dexamethasone for 10 days was started in the CCU.
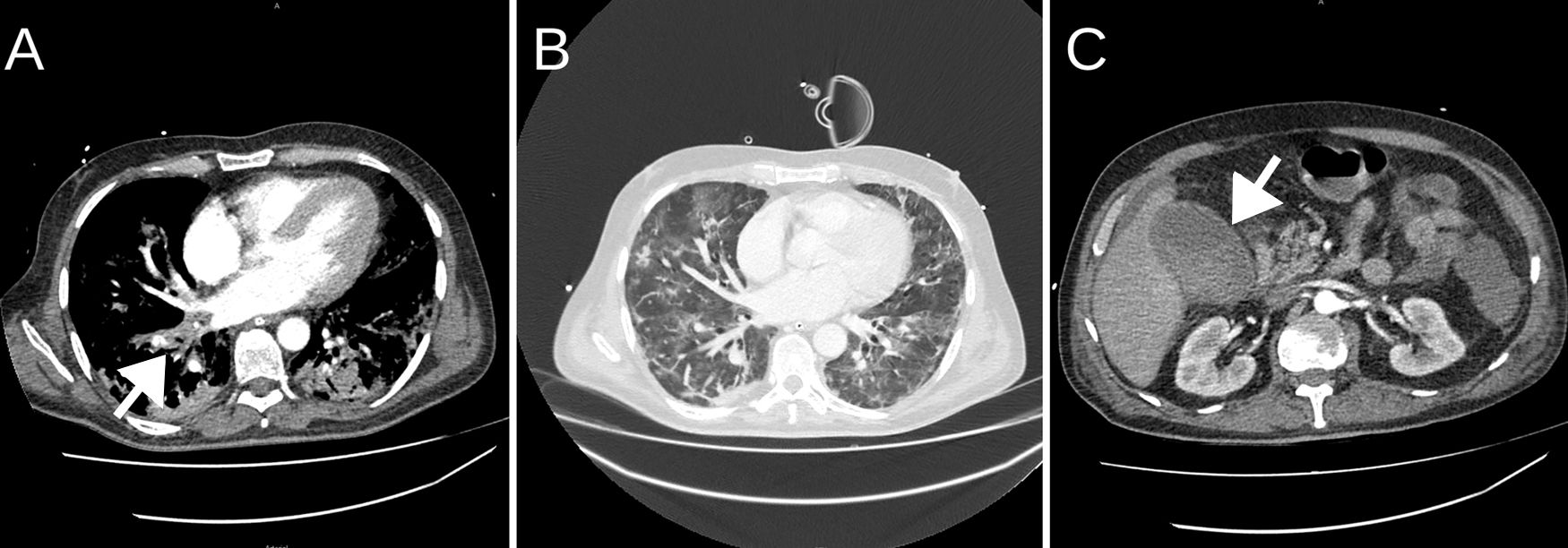
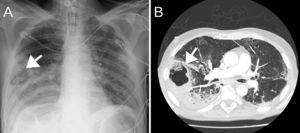
The patient improved after 24h in the prone position, and was extubated 5 days after admission. He was treated with high-flow nasal cannula (HFNC) until the seventh day, when he gradually developed tachypnoea together with intense abdominal pain with guarding in the right upper quadrant. He was re-intubated due to clinical and blood gas worsening with PaO2 65mmHg and PaCO2 30mmHg. Biliary pathology was suspected, so an urgent CT scan was performed, which showed acalculous cholecystitis (Fig. 1), massive bilateral PE and ischaemic colitis. The patient developed septic shock, probably of biliary origin, with growth of Enterobacter aerogenes in peripheral blood cultures, and required infusion of norepinephrine at 0.3mcg/kg/min. The infection was controlled by ultrasound-guided percutaneous cholecystostomy and ertapenem 1g/24h. He also received an anticoagulant (enoxaparin 1mg/kg/12h) for PE. Fourteen days after admission, and after improvement of inflammatory parameters and withdrawal of norepinephrine, he was extubated with PaO2/FiO2 >250; HFNC therapy was maintained. The patient had significant muscle weakness. On the 17th day of admission, he presented lower gastrointestinal bleeding in the form of haematochezia and haemodynamic instability, for which he was re-intubated and norepinephrine infusion 0.2mcg/kg/min was restarted. An urgent CT scan showed ischaemic colitis with no active bleeding or perforation. On the 19th day of admission a tracheotomy was performed. After weaning procedures, he was disconnected from mechanical ventilation on the 34th day of admission. The patient is still in the CCU, receiving conventional oxygen therapy through the tracheostomy and intensive physiotherapy sessions.
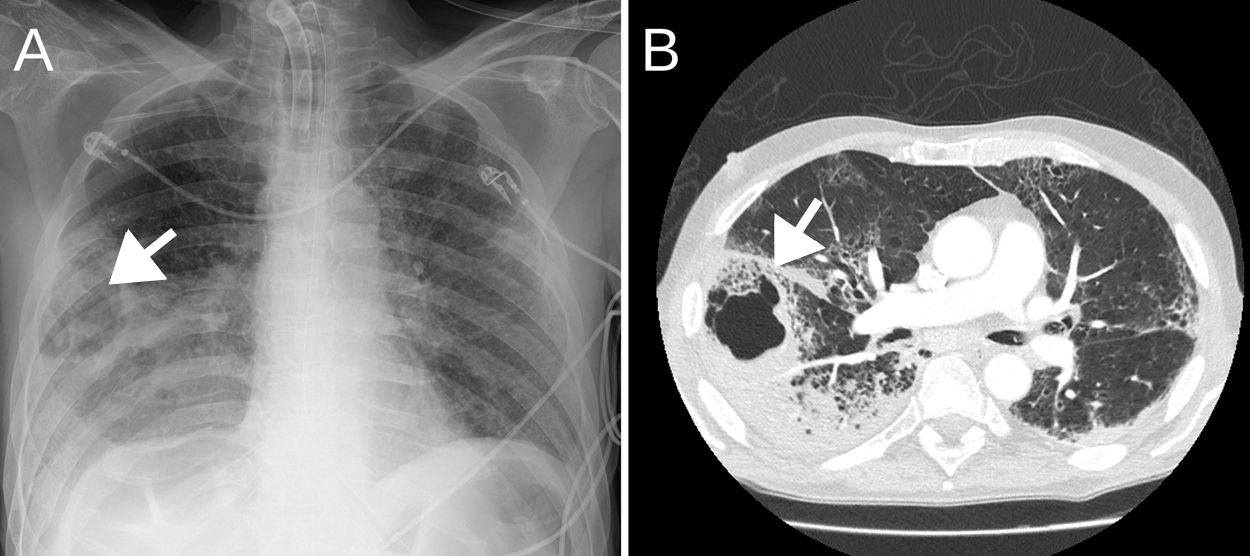
Case 2A 57-year-old man weighing 68kg with a history of active alcoholism, former smoker, laryngectomy in 2016 for supraglottic carcinoma with no evidence of disease, and treated for tuberculosis 15 years earlier. He came to our hospital 6 days after the onset of symptoms consisting of fever peaks and dyspnoea at rest. A chest X-ray performed on admission showed bilateral alveolar infiltrates. SARS-CoV-2 tests were positive, so treatment was started with hydroxychloroquine, lopinavir/ritonavir, amoxicillin-clavulanate, anti-inflammatory therapy with methylprednisolone for 3 days, tocilizumab (2 doses) and tacrolimus. On the ward, he presented delirium, possibly due to alcohol withdrawal. On the sixth day of admission, haemoptysis was observed in the tracheal aspirate, causing tachypnoea and desaturation, so piperacillin-tazobactam was started. Chest X-ray and CT angiography revealed possible right lower lobe (RLL) pulmonary cavitation and PE (Fig. 2).
On the seventh day, he was admitted to the CCU with hypotension and hypoxaemia. He was sedated with remifentanil and propofol in order to start mechanical ventilation, as well as norepinephrine at 0.25mcg/kg/min.
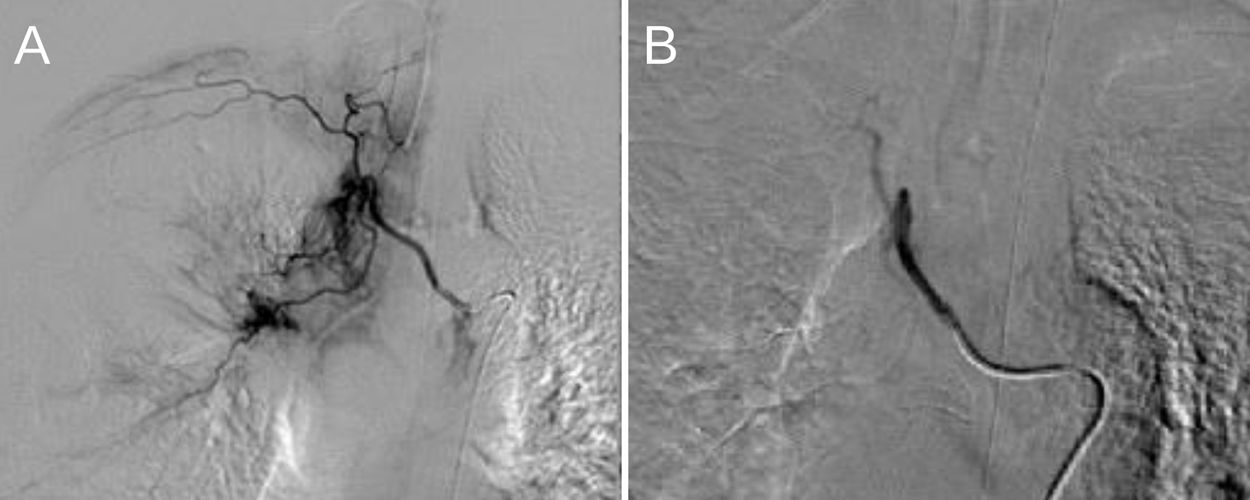
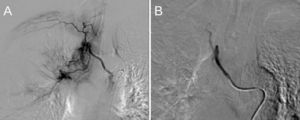
Treatment with enoxaparin 40mg every 12h was started after weighing up bleeding versus thrombotic risk due to PE. Bronchoalveolar aspirate (BAA) samples were taken for culture, being positive for Staphylococcus aureus and Proteus mirabilis, culture and auramine–rhodamine stain were negative for TB, and nasopharyngeal swab was negative for methicillin-resistant S. aureus (MRSA). Serum galactomannans were slightly positive, but fungal colonies were never isolated in respiratory specimen. Haemoptysis episodes persisted for 48h, so in consensus with the vascular and interventional radiologist diagnostic arteriography was performed.
The image showed hypertrophy of the bronchial arteries with pathological vascularization of the RLL (right intercostobronchial trunk and right branch of the bronchial trunk), so these were embolised without incident (Fig. 3). Haemoptysis improved and the patient was disconnected from mechanical ventilation 2 days later. He also developed acute kidney injury stage 2 with hypernatremia and hypokalaemia that progressively improved. Eight days after admission to the UCC, he was discharged to the Semicritical Pulmonology Care Unit.
DiscussionCritically ill patients with COVID-19 are likely to present various concomitant pathologies that need to be diagnosed and treated early.3
Acalculous cholecystitis is a typical complication of major surgery and trauma in critically ill patients.6,7 Prolonged fasting, arterial hypotension, and parenteral nutrition, which would predispose to an alteration of gallbladder motility and the formation of bile stasis have been described as risk factors. Mortality in these cases is up to 50%, and has a worse prognosis than calculous cholecystitis,7 mainly due to diagnostic difficulty and the population it usually affects. It requires a high diagnostic suspicion for which a specific diagnostic imaging test, either an ultrasound or an abdominal CT, is indicated. In the case described here, it was essential that the patient was conscious.
Necrotizing pneumonia, which was diagnosed in the second patient, is a rare form of adult pneumonia, with a prevalence of less than 1%. Among the risk factors described are alcoholism, diabetes mellitus, or corticosteroid therapy.8 Many pathogens have been described as causative agents, one of the most frequent being S. aureus. Other aetiological agents are anaerobic bacteria, mycobacteria or fungi, especially in immunosuppressed patients. In our case, haemoptysis, which can sometimes be massive, was the first symptom that helped guide the diagnosis and choose radiological and microbiological diagnostic tests. The usual treatment is empirical antibiotic therapy that is later directed according to the culture results, reserving surgery or bronchial artery embolization for severe cases that do not respond to medical treatment, or when anticoagulation is indicated, which was the case in our patient.8,9
COVID-19 patients are known to present a wide array of dysfunctions in various organs, such as the lungs, heart, liver, kidney, and as new research is showing, the vascular endothelium.10 The benefit of a multidisciplinary approach is shown in the 2 cases presented here.
ConclusionSeriously ill patients admitted for SARS-CoV-2 pneumonia may suffer other pathologies that require early diagnosis and treatment, and a multidisciplinary approach is highly beneficial.
FundingThe authors have not received any type of funding for this article.
Conflict of interestsThe authors of this article have no conflicts of interest to declare.
Please cite this article as: Puig G, Giménez-Milà M, Campistol E, Caño V, Valcarcel J, Colomina MJ. Desarrollo de enfermedades concomitantes en pacientes críticos con COVID-19. Rev Esp Anestesiol Reanim. 2021;68:37–40.