Around 60%–80% of the population suffers from back pain, making it one of the most common health complaints. Transforaminal percutaneous endoscopic discectomy (TPED) is an effective treatment for low back pain that can be performed using different anaesthesia techniques. Our primary objective was to test the hypothesis that bilateral Erector spinae plane block (ESP) plus sedation is equally effective as traditional local infiltration anaesthesia plus sedation in TPED.
Materials and methodsFifty-two patients undergoing TPED were randomly assigned to 2 groups: G1 – intravenous sedation with local infiltration anaesthesia; G2 – intravenous sedation with bilateral ESP. Primary outcome: volume of fentanyl and propofol administered during surgery. Secondary outcomes: adverse events during sedation reported using the World Society of Intravenous Anaesthesia (SIVA) adverse sedation event tool, level of postoperative sedation measured on the Richmond Agitation-Sedation Scale (RASS), intensity of postoperative pain on a visual analogue scale (VAS), mechanical pain threshold (MPT) measured with von Frey monofilaments on both lower extremities, patient satisfaction with analgesia on 5-point Likert scale.
ResultsVolume of fentanyl, propofol, and level of postoperative sedation was significantly lower in G2 (p < 0.001). There was no difference between groups in intensity of pain, patient satisfaction with analgesia, and mechanical pain threshold after surgery. There were no adverse events in G2, but in G1 2 patients presented minimal risk descriptors, 5 presented minor risk descriptors, and 1 presented sentinel risk descriptors that required additional medication or rescue ventilation.
ConclusionsThe ESP was equal to local infiltration anaesthesia in terms of intensity of pain, mechanical pain threshold after surgery, and patient satisfaction; however, ESP reduced the volume of intraoperative fentanyl and propofol, thereby reducing the adverse effects of sedation.
Low back pain is one of the most common health complaints.1,2 This pain, which is often severe, can significantly limit the patient's ability to work and can impact the patient both physical and economically.3,4
Low back pain treatment options range from therapeutic exercise and massage to transpedicular decompression and instrumented fusion of the spine. One of the latest, minimally invasive, effective treatments of low back pain is transforaminal percutaneous endoscopic discectomy (TPED), which can be performed on an outpatient basis under local anaesthesia with mild sedation.5 In this procedure, local anaesthesia is used to control sensitivity in the lower extremities in order to prevent damage to the spinal cord roots.6 For this reason, general anaesthesia with tracheal intubation is not always desirable as the patient will not be able to report discomfort in the limb. However, the prone position significantly limits the depth of anaesthesia due to the lack of adequate access to the patient's airway.
The rapid development of new regional anaesthesia techniques has led to a deeper understanding of their mechanisms of action.7–10 Numerous studies have described the erector spinae block as an effective component of intra- and postoperative analgesia in spinal surgery.11–14
The main aim of our study was to test the hypothesis that the erector spinae plane block (ESP) plus sedation is as effective as local infiltration anaesthesia with fentanyl and propofol plus sedation. The primary endpoint was the volume of fentanyl and propofol administered during surgery.
Materials and methodsThis study was conducted between January 2021 and January 2022 in the the Department of Anaesthesiology and Intensive Care of the public hospital Yuriy Semenyuk Rivne regional clinical hospital and the Rivne affiliate of the Department of Anaesthesiology and Intensive Care, Faculty of Postgraduate Education, Danylo Halytsky Lviv National Medical University. The study was approved by the Yuriy Semenyuk Rivne regional clinical hospital research ethics committee on 16 December 2020 (Chairperson V. Tkach, protocol No. 5-1B/1612).
All participants provided written informed consent to participate in the study.
The study was registered on ClinicalTrials.gov (identification number NCT05483647).
Study design: open, parallel, prospective, controlled, randomized, allocation ratio 1:1.
Inclusion criteria were: informed consent to participate in the study, intervertebral hernia requiring transforaminal percutaneous endoscopic discectomy, and no known allergies to local anaesthetics.
Exclusion criteria were: refusal to participate in the study, withdrawal from the study, ASA physical status III or greater, age over 50 years, body mass index (BMI) greater than 30 kg/m2.
Patients were randomly assigned to receive either intravenous sedation with local infiltration anaesthesia (G1) or intravenous sedation with bilateral ESP (G2), using the online randomisation program Random.org, https://www.random.org. Patients were randomised to G1 or G2 after being placed in the prone position, before skin incision. Regardless of the patient group, the mobile C-arm X-ray was used to identify the level of surgery. Patients were told that they would receive an injection for analgesia, but did not know whether they would receive local infiltration anaesthesia or bilateral ESP. In both cases, we used C-arm X-ray to guide needle placement. The treating anaesthesiologists were aware of group allocation, but both patients and researchers that collected and assessed the data were not.
Primary outcome: volume of fentanyl and propofol administered during surgery.
Secondary outcomes: adverse events during sedation reported using the World Society of Intravenous Anaesthesia (SIVA) adverse sedation event tool,15 level of postoperative sedation measured on the Richmond Agitation-Sedation Scale (RASS), intensity of postoperative pain on a visual analogue scale (VAS), mechanical pain threshold (MPT) measured with von Frey monofilaments on both lower extremities, patient satisfaction with analgesia on 5-point Likert scale.
In both groups, fentanyl was administered for intraoperative analgesia and propofol for sedation. In both groups, fentanyl (0.5 μg/kg) was administered if the patient complained of low back pain and/or heart rate and blood pressure increased by more than 20% from baseline. If the patient complained of sharp shooting pain in their leg, the surgeon repositioned the endoscope in order to avoid irritating the spinal cord root, and fentanyl was not administrated.
After performing administering local infiltration anaesthesia or performing ESP, propofol was administered using target-controlled infusion based on the propofol pharmacokinetic parameters reported by Eleveld 2.1.16 The initial propofol plasma concentration target was 1.0 μg/mL in both groups (we used iTIVA plus Anaesthesia software v5.2.3 to predict propofol concentrations). Subsequently, the infusion rate of propofol was changed in order maintain the modified observer's assessment of alertness/sedation scale (MOAA/S) score at between 2 and 3.
Adverse events during sedation were identified using the 5-step World SIVA adverse sedation event reporting tool. All 5 steps required by this tool were completed. Sedation-related adverse events were classified and recorded as minimal risk, minor risk, sentinel risk, and other according to SIVA definitions. Interventions that were performed to treat the adverse events and the outcomes of the adverse events were also recorded.
After the patient had been transferred from the operating room to the postoperative ward, the level of postoperative sedation was evaluated with RASS. Two hours after surgery, intensity of pain and the mechanical pain threshold were measured, and patients were asked to rate their satisfaction with the analgesia received using a 5-point Likert scale.
Von Frey monofilaments, consisting of 20 nylon filaments of different thicknesses in ascending order, were used to determine mechanical pain threshold after surgery. Patients were asked to lie supine, close their eyes, and report when they felt a clear point of contact with the skin. Monofilaments were pressed against the skin of the middle third of the palmar surface of the forearm at an angle of 90° until the filament bent for 2 s. Monofilaments were used in ascending order with an interval of 10 s.
All patients received paracetamol, dexketoprofen, ondansetron, dexamethasone, and tranexamic acid in the operating room. In the prone position, before the skin incision, patients in the G1 group received local infiltration anaesthesia at the level of incision. The skin, subcutaneous tissue and muscles up to the intervertebral foramen were anesthetized by the surgeon using 40 ml lidocaine 1% with dexamethasone 0.02% and epinephrine 0.00018%. Patients in the G2 group receiving bilateral ESP. In our study we used a C-arm X-ray (TCA 9″, No. 54-21-036-1155) system for spine and needle visualisation. X-ray guidance is commonly used to perform nerve, plexus or ganglion blocks to treat chronic pain.17–19 The C-arm was centred over the midlumbar region at an angle of 90°. A 22-gauge, 5-inch spinal needle was inserted through skin, subcutaneous tissues and the erector spinae muscles to reach the transverse processes. The direction of the needle was assessed and adjusted by obtaining repeat images every 1–1.5 cm of needle advancement. For ESP block, the needle was positioned over the posteromedial surface of the transversus processes, 3 cm lateral to the spinous process of the lumbar vertebral body. When the tip of the needle reached the bone, after negative aspiration for blood, 1% lidocaine with 0.02% dexamethasone and 0.00018% epinephrine were injected in small increments for a final dose of 40 ml. Bilateral ESP was administered 1 level above the intervertebral space where the surgery was performed due to the surgical cranial-caudal access to the foramen. Fluoroscopy time and anaesthetic dose was the same in both groups. For postoperative analgesia, patients in both groups received nonsteroidal anti-inflammatory drugs (paracetamol in combination with dexketoprofen) every 6 h. Thromboprophylaxis was administered based on the risk of thromboembolic complications. The patients were followed up until discharge home.
Sample size calculations for our hypothesis (ESP plus sedation is as effective as local infiltration anaesthesia plus sedation) resulted in 21 patients per group. We used a type 1 error of α = 0.05 and a power of 0.80 to calculate the sample size (G*Power version 3.3.9.4).
All data were tested for normality of distribution and expressed as mean ± SD. The significance of deviations in the mean values was assessed using the Student or Mann-Whitney tests. A p-value less than 0.05 was statistically significant.
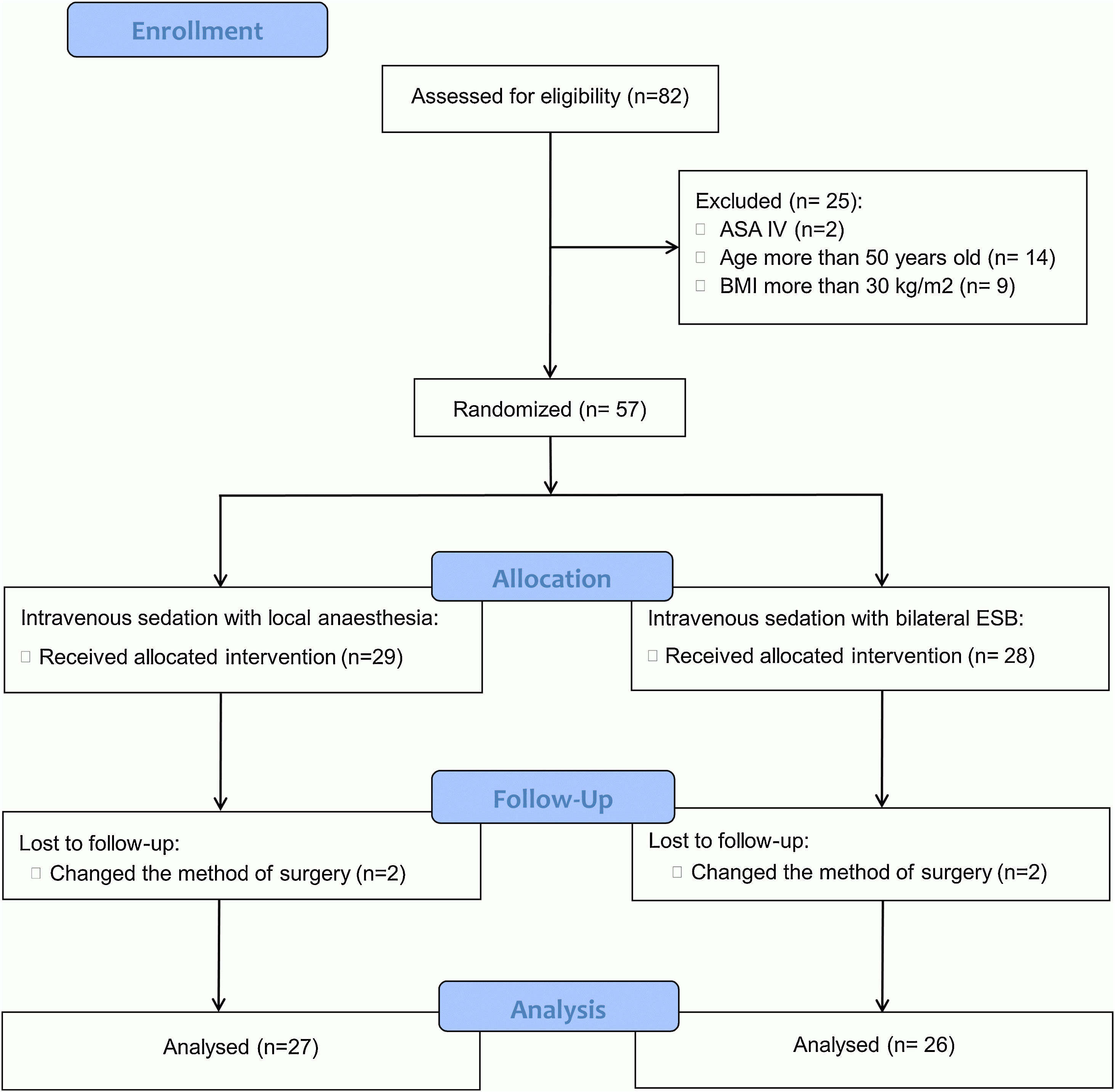
ResultsEighty-two patients were scheduled for transforaminal percutaneous endoscopic discectomy. Twenty-five fulfilled the exclusion criteria, so 57 patients were enrolled in the study. The CONSORT flow chart is shown in the Fig. 1.
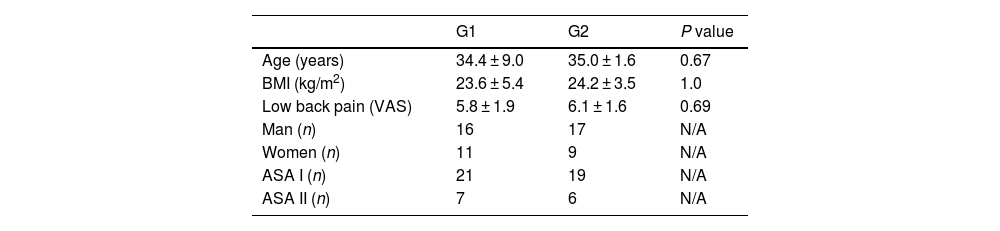
Two patients in each group dropped out due to changes in the surgery technique, leaving 53 to complete the study, with 27 in the local infiltration anaesthesia group (G1) and 26 in the bilateral ESB group (G2). The characteristics of the patients in both two groups are summarised in Table 1.
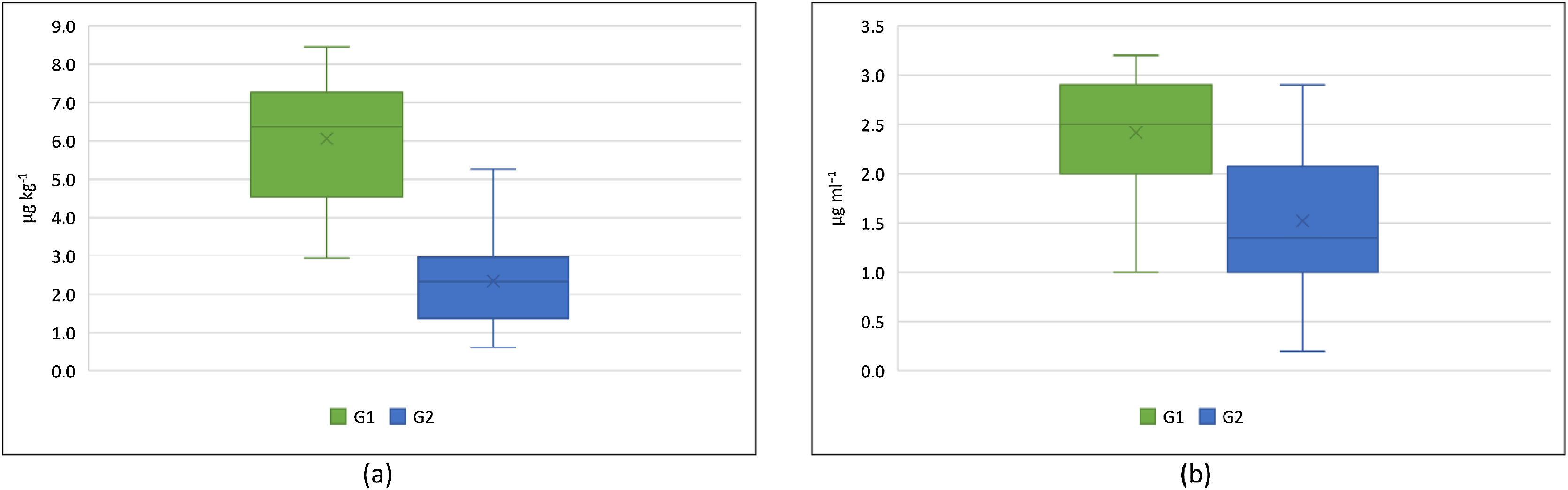
The mean volume of fentanyl in the local anaesthesia group (G1) was 6.06 ± 1.67 μg/kg versus 2.34 ± 1.13 μg/kg in ESP group (G2), p < 0.001. The volume of propofol administered intraoperatively was lower in G2 than G1 (1.5 ± 0.8 μg/mL vs. 2.4 ± 0.6 μg/mL, p < 0.001). A box plot of the volume of fentanyl and propofol administered in both groups is shown in Fig. 2.
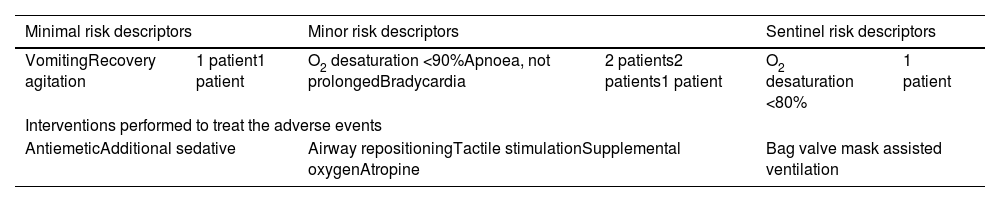
No adverse sedation events (SIVA reporting tool) were identified in G2, but in G1 two patients had minimal risk descriptors, and 1 patient had a sentinel risk descriptor that required additional medication or rescue ventilation. Adverse events in G1 identified using the World SIVA adverse sedation event reporting tool are shown in Table 2.
World SIVA adverse sedation event reporting tool in G1.
| Minimal risk descriptors | Minor risk descriptors | Sentinel risk descriptors | |||
|---|---|---|---|---|---|
| VomitingRecovery agitation | 1 patient1 patient | O2 desaturation <90%Apnoea, not prolongedBradycardia | 2 patients2 patients1 patient | O2 desaturation <80% | 1 patient |
| Interventions performed to treat the adverse events | |||||
| AntiemeticAdditional sedative | Airway repositioningTactile stimulationSupplemental oxygenAtropine | Bag valve mask assisted ventilation | |||
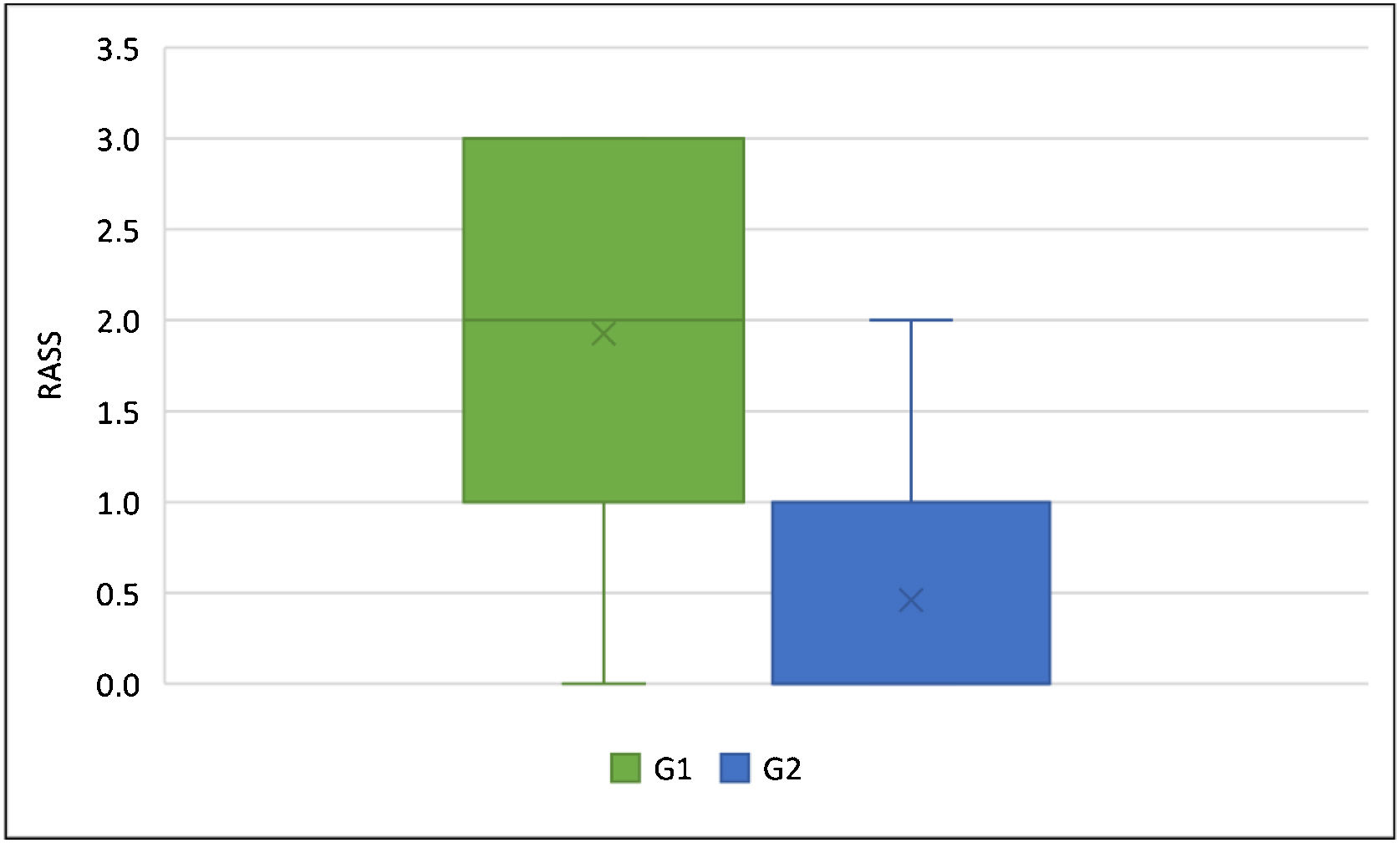
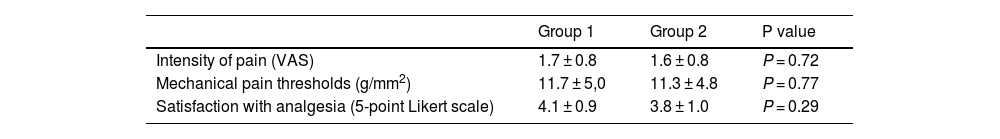
The level of postoperative sedation differed significantly between groups (RASS score in G1 – 1.9 ± 0.9 and in G2 – 0.5 ± 0.7, p < 0.001). A box plot of postoperative sedation in both groups is shown in Fig. 3. Intensity of pain, mechanical pain threshold, and patient satisfaction with analgesia did not differ significantly between groups, and are shown in Table 3.
Intensity of pain, mechanical pain thresholds and patient satisfaction with analgesia in both groups.
| Group 1 | Group 2 | P value | |
|---|---|---|---|
| Intensity of pain (VAS) | 1.7 ± 0.8 | 1.6 ± 0.8 | P = 0.72 |
| Mechanical pain thresholds (g/mm2) | 11.7 ± 5,0 | 11.3 ± 4.8 | P = 0.77 |
| Satisfaction with analgesia (5-point Likert scale) | 4.1 ± 0.9 | 3.8 ± 1.0 | P = 0.29 |
Despite the wide scope of modern local anaesthetics and the development of several different local infiltration anaesthesia techniques, they provide insufficient analgesia in some rare cases. Other problems include insufficient local anaesthetic infiltration of the surgical field requiring the administration of booster doses that can cause discomfort or even pain, and suboptimal local anaesthesia that causes the patient to move away from the source of pain and possibly dislodge the endoscopic device, thereby prolonging the surgery.
To overcome these difficulties, anaesthesiologists might increase the depth of sedation and analgesia, which can increase the risk of complications. Aware of the negative consequences of overly deep sedation in the prone position, we attempted to find a more effective method of anaesthetizing the operating field in transforaminal percutaneous endoscopic discectomy.
Numerous analgesia techniques have been developed for spinal surgery, included spinal and epidural anaesthesia. Spinal anaesthesia shortens anaesthesia and surgery time and the length of stay in the postanaesthetic care unit, reduces postoperative pain, and does not increase the risk of other complications.20 Even in high-risk cardiac patients, spinal anaesthesia is safe and provides good perioperative hemodynamic stability.21
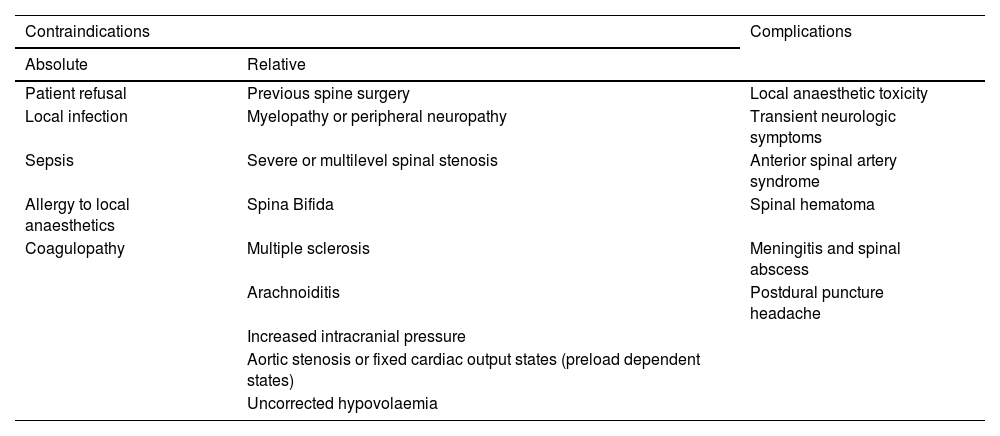
Epidural anaesthesia provides more effective pain control22 than general anaesthesia, but does not reduce the length of stay or the rate of readmission and complications, and does not lead to better outcomes in patients undergoing spinal surgery.23,24 Moreover, spinal and epidural anaesthesia are contraindicated in some patients, and can lead to complications, which are shown in Table 4.25–29
Contraindications and complications in spinal and epidural anaesthesia.
| Contraindications | Complications | |
|---|---|---|
| Absolute | Relative | |
| Patient refusal | Previous spine surgery | Local anaesthetic toxicity |
| Local infection | Myelopathy or peripheral neuropathy | Transient neurologic symptoms |
| Sepsis | Severe or multilevel spinal stenosis | Anterior spinal artery syndrome |
| Allergy to local anaesthetics | Spina Bifida | Spinal hematoma |
| Coagulopathy | Multiple sclerosis | Meningitis and spinal abscess |
| Arachnoiditis | Postdural puncture headache | |
| Increased intracranial pressure | ||
| Aortic stenosis or fixed cardiac output states (preload dependent states) | ||
| Uncorrected hypovolaemia | ||
The latest evidence-based guidelines in anaesthesiology recommend blocking peripheral nerves as close as possible to the lesion,30–33 so neuraxial anaesthesia is not required in a procedure that requires only a centimetre long incision in an area measuring 2−3 cm in diameter.
The posterior elements of the vertebral column are innervated by the dorsal branches of the spinal nerves, while the intervertebral discs and related ligaments are innervated by the ventral branches and sympathetic nervous system.34 In transforaminal percutaneous endoscopic discectomy, therefore, it is sufficient to block only the dorsal and ventral branches of the spinal cord.
In 2016, Mauricio Forero developed the erector spinae plane block (ESPB) for the treatment of thoracic neuropathic pain.35 Since then, this technique has been proven both effective and safe for intra- and post-operative analgesia in interventions involving the cervical spine,36,37 upper extremities,38,39 chest,40,41 abdominal cavity42,43 and lower extremities,44 and has also proven effective in reducing opioid requirements and improving postoperative pain management46 in open spine surgery.45 However, ESPB is a volume-dependent technique that requires a large volume of anaesthetic for adequate analgesia (30−40 ml per side).47,48 MRI imaging studies have shown that this volume of anaesthetic reaches not only the dorsal and ventral branches of the spinal nerve,49 but also extends deep to the spinal ganglion.50 A large amount of anaesthetic in the lumbar spine can spread to the lumbar plexus and cause weakness in the lower limbs after surgery.51
In our study, we injected just 20 ml of local anaesthetic on each side. This anesthetized the surgical site field but preserved sensitivity in the lower extremities (the mechanical pain threshold level was the same in both groups compared to baseline).
The quality of the technique is evidenced by the small volume of fentanyl required intraoperatively to achieve the blockade. Propofol also has a slight but significant analgesic action.52,53 Patients receiving local infiltration anaesthesia required more opioids and a higher volume of local anaesthetic to achieve the same level of sedation (2−3 score MOAA/S) as those receiving ESP. High-dose opioids during intravenous anaesthesia led to intraoperative complications such as vomiting, emergence agitation, O2 desaturation <80%, apnoea (not prolonged), and bradycardia, which required antiemetics, additional sedatives, airway repositioning, tactile stimulation, supplemental oxygen, atropine, and bag valve mask assisted ventilation. In the postoperative period, higher doses of opioids and anaesthetics resulted in a deeper level of sedation. However, pain levels and patient satisfaction were similar in both groups.
Despite the low rate of complications in our cohort, any complications can be harmful and should be taken into consideration when choosing the anaesthesia technique, because patient safety must be the anaesthesiologist’s main priority. ESP reduces the number of complications, and is therefore a good alternative to local anaesthesia in transforaminal percutaneous endoscopic discectomy.
Our study has some limitations. First, it was conducted in a single centre, thus limiting the range of eligible subjects and surgical techniques. Second, the treating anaesthesiologist was not blinded to group allocation, and this could have biased drug administration. Third, bilateral ESP required 2 shots, whereas local infiltration anaesthesia required only one. We cannot rule out the possibility that patients may have mentioned this to the researchers collecting the outcome data.
ConclusionErector spinae plane block plus sedation requires lower doses of fentanyl and propofol during surgery than local infiltration anaesthesia. Local infiltration anaesthesia results in deeper sedation and a higher complication rate, but was equal to ESPB in terms of pain management and patient satisfaction.
FundingThis work has not received any funding.
Registration number and name of registry: ClinicalTrials.gov (identification number NCT05483647).
Conflict of interestThe authors declare that they have no conflict of interest.