Cataract surgery is one of the most common procedures in outpatient surgery units. The use of information and communication technologies (ICT) in clinical practice and the advent of new health scenarios, such as the Covid pandemic, have driven the development of pre-anaesthesia assessment models that free up resources to improve access to cataract surgery without sacrificing patient safety. The approach to cataract surgery varies considerably among public, subsidised and private hospitals. This raises the need for guidelines to standardise patient assessment, pre-operative tests, management of background medication, patient information and informed consent.
ResultsIn this document, the SEDAR Clinical Management Division together with the Major Outpatient Surgery Division SEDAR Working Group put forward a series of consensus recommendations on pre-anaesthesia testing based on the use of ITCs, health questionnaires, patient information and informed consent supervised and evaluated by an anaesthesiologist.
ConclusionsThis consensus document will effectivise pre-anaesthesia assessment in cataract surgery while maintaining the highest standards of quality, safety and legality.
La cirugía de cataratas es uno de los procedimientos más frecuentes en las unidades de cirugía ambulatoria. La irrupción de las tecnologías de la Comunicación en la práctica clínica y nuevos escenarios sanitarios como la Pandemia Covid han propiciado soluciones a las necesidades de accesibilidad de los pacientes, liberando recursos manteniendo altos niveles de seguridad. El proceso asistencial para la intervención de cataratas varía sustancialmente entre los diferentes hospitales públicos, concertados y privados. Se precisan recomendaciones que propongan un marco de trabajo sobre la valoración física, solicitud de pruebas preoperatorias, manejo de la medicación perioperatoria e información y firma del consentimiento informado.
ResultadosSe establecen recomendaciones sobre el manejo de la consulta de anestesia, incorporando tecnologías de la información, cuestionarios de salud, información al paciente y firma de los consentimientos siempre supervisados y evaluados por especialistas anestesiólogos.
ConclusionesLa Sección de Gestión Clínica junto con la Sección de Cirugía Mayor Ambulatoria de la Sedar han desarrollado un documento de consenso para una gestión eficiente de la valoración pre anestésica del proceso de la cirugía de cataratas, dentro de un marco referencial centrado en la calidad, seguridad y legalidad.
Cataract surgery is one of the most common procedures in outpatient surgery units. Approximately 20 million extractions are performed worldwide, of which 4.5 million take place in the European Union. In Spain, 450,000 cataract surgeries were performed in 2019, making it one of the most sought-after surgical interventions and one that contributes significantly to hospital waiting lists. Because of its potential benefits to both individual patients and society as a whole, cataract surgery is now a priority intervention. According to current scientific evidence, delaying surgery by more than 4 months increases the risk of complications, falls, hip fractures and traffic accidents, and is detrimental to the patient’s quality of life.1
The approach to cataract surgery varies substantially between public, subsidized, and private hospitals in terms of ordering preoperative tests, the management of perioperative medication, and the need for an anaesthesiologist to be physically present or on call during the procedure.
Cataracts with an indication for surgery usually occur in elderly individuals in whom comorbidities such as hypertension, diabetes, obesity, smoking-related lung injuries, and polypharmacy are common.
Physiologically, cataract surgery is characterized by minimal surgical stress, no loss of blood or other fluids, and few, if any, inflammatory or endocrine repercussions; therefore, there is usually no need to adjust or suspend the patient’s background medication.
The use of minimally invasive techniques to extract the lens has eliminated the risk of most intra- and postoperative complications in cataract surgery.
However, some intraoperative complications such as the oculocardiac or Aschner reflex, characterized by bradycardia due to traction on the extraocular muscles or globe pressure, can still occur. The oculocardiac reflex is observed mainly during strabismus and vitreoretinal surgery, but only occasionally in cataract surgery under topical anaesthesia.
The incidence of subchoroidal or expulsive haemorrhage during phacoemulsification is less than 0.094%.2 Choroidal blood volume is determined primarily by central venous pressure. This volume, and consequently intraocular pressure, remains largely unchanged despite fluctuation in blood pressure of between 25 and 215 mm Hg.
The most common intraoperative complication in cataract surgery is intraoperative arterial hypertension (ioHBP, defined as an increase of more than 20% over baseline blood pressure or a mean arterial pressure (MAP) of more than 130 mm Hg). The main risk factors are anxiety, previous history of high blood pressure, and non-compliance with prescribed chronic antihypertensive medication. There is no evidence that ioHBP affects medical or surgical outcomes in cataract surgery.3 The need for aggressive treatment should be individualized and is recommended only if HBP causes difficulties in the surgical technique.4
The estimated overall risk of mortality or serious complications associated with cataract surgery is only 0.014%.5,6 Cataract surgery using phacoemulsification and topical anaesthesia, therefore, can be considered a low-risk, safe procedure with a very low incidence of complications.
There is growing interest in improving access to cataract surgery, particularly among elderly patients, due to its beneficial effect not only on their health and well-being, but also on their social situation. Prior to the COVID-19 pandemic in 2020, the average overall waiting time for cataract surgery in Spain was 73 days (SISLE-SNS 2019), but this now has increased to more than 160 days in some Spanish autonomous communities (SISLE-SNS 2021). Anaesthesiologists, together with hospital managers, are in a position to improve access and treatment by introducing care pathways that reduce delays without sacrificing care quality and patient safety.
Cataract surgery under topical anaesthesia accounts for 10%–15% of all pre-anaesthesia evaluations and 30% of all major outpatient surgery programs (Statistical portal, CMBD specialized care registry, Ministry of Health).7
In 2020, 3,418,000 surgeries were performed in Spain, of which 388,544 were cataract interventions.7 This gives an idea of the magnitude of these interventions, their impact on healthcare resources, and the pressing need to eliminate the use of non-essential resources. The current cataract surgery pre-anaesthesia assessment protocol needs to be re-designed to avoid exposing patients, particularly elderly and more vulnerable individuals, to respiratory infections due to repeated hospital visits, and to eliminate unnecessary travel expenses and possible sick leave.
In order to optimise our approach to cataract surgery we need to remove barriers and procedures that have little benefit for the patient without compromising the safety and quality of their care. Since 2020, patient-centred care and the need to assess the risk-benefit of medical acts and consultations that can expose patients to respiratory or contact infections (SARS-CoV 2 virus) has acquired particular relevance. New care programs need to be developed in order to reduce the number of patients in hospital waiting rooms and public spaces. These programs must meet the overall healthcare needs of the Spanish population and improve efficiency and accessibility while eliminating unnecessary procedures, tests and consultations and their associated costs.
The following recommendations have been drawn up to create speedy, effective, care pathways centred on a population that is usually elderly, comorbid, with reduced mobility. Our goal is to provide safe, high-quality care programs that are tailored to our circumstances, needs, and legislation.
ObjectivesTo develop a cataract surgery management model that can be adapted to the needs of each unit and meets two prerequisites:
- -
The need to promote efficient management and sustainability by assigning only those resources that have proven to be effective without sacrificing quality of care and patient safety.
- -
The need to perform a preoperative assessment that is proportional to the complexity of the surgery and anaesthesia, that complies with current legislation, and that guarantees quality of care and patient safety.
Patients with ocular problems are first seen by an ophthalmologist. These specialists play a key role in the cataract surgery pathway because it is their responsibility to include the patient on the surgery waiting list and determine the existence of certain ocular or systemic factors that indicate whether the procedures can be performed under topical anaesthesia or whether sub-tenon block is required.
These factors include the characteristics of the cataract, the patient’s monocular vision, and a high risk of bleeding. Some hospitals use the Surgical Complexity Score to predict technical difficulties and estimate the duration of surgery – a factor that will facilitate scheduling.
Other patient-related risk factors are also taken into account, such as high comorbidity, lack of collaboration, anxiety, and serious or disabling musculoskeletal disorders. Ophthalmologists can also detect these risk factors by administering validated health questionnaires to identify patients with comorbidities.
The European Society of Anaesthesiology guidelines for the preoperative evaluation of adults undergoing elective noncardiac surgery (2018), establishes the following 1C recommendation on the preoperative evaluation: “Pre-operative assessment may be carried out by a nurse or physician, but we recommend that it should be concluded by a physician anaesthetist“.
Health questionnaireThe use of questionnaires to evaluate a patient’s health status is common practice in healthcare. Scientific societies in the United States and Canada have included questionnaires as an alternative in the pre-anaesthesia evaluation. In Spain, some autonomous communities already include paper or online health questionnaires in their preoperative assessment protocols. Evidence has shown that questionnaires are effective and reliable in assessing clinical status, clearly show the medication required, and eliminate the risk of mislaying or forgetting to collect certain information. The use of questionnaires is also associated with a high level of patient satisfaction and does not increase preoperative anxiety when compared with a conventional evaluation.8
Although preoperative questionnaires can be administered by the ophthalmologist, they are time-consuming and add to their workload. This, in turn, can jeopardise patient safety. Therefore, patients can be evaluated in pre-anaesthesia consultations using different formats: “high resolution consultation”, telematic/telephone consultation, or conventional in-person consultation. All these options can effectively optimise the work flow. The final evaluation should always be carried out by an anaesthesiologist.
The number of studies analysing the use and validation of electronic questionnaires has recently increased, and have shown that these tools can aid care planning by reliably and accurately stratifying patients for referral to preoperative assessment.9 One disadvantage, however, is that they can only be administered to patients with computer skills and access to a computer, so they are often unsuitable for elderly patients - the group that is most likely to require cataract surgery.10
There are several different preoperative assessment questionnaires available, but few have been validated in Spanish. For reference purposes, we attach the Spanish version of the Hamilton Regional Eye Institute questionnaire in Appendix A.
Pre-anaesthesia consultationThe pre-anaesthesia consultation, a key factor in Perioperative Medicine, assesses the risk of administering anaesthesia to a patient scheduled for surgery. The immediate aim of the assessment is to adjust the patient’s background medication and optimize their health status in preparation for surgery. There is also evidence that this consultation can reduce the patient’s preoperative anxiety and minimise the number of surgery cancellations.
SEDAR recommends evaluating, examining, and updating the medical history of all patients scheduled for diagnostic or therapeutic interventions that require anaesthesia. However, in the case of cataract surgery, the pre-anaesthesia assessment can be streamlined to improve efficiency and save time and resources.6,11
Cataract surgery is considered a very low risk intervention, even though it is usually performed in elderly patients with multiple comorbidities. Preoperative tests, irrespective of the type of surgery, are only indicated in patients with serious medical conditions.12
Anaesthesiologists are encouraged to use the latest technology in their office to view and update the patient’s history and to optimise patient schedules and waiting lists. Several studies have shown that electronic assessment forms (e-forms) are more effective than their paper counterparts. Specifically, e-forms reduce the risk of forgetting to collect certain items and of losing data due to illegibility or damage to the paper on which they are printed. In addition, e-forms can be accessed from all hospital computers.12
Ophthalmological anaesthesia services should draw up specific protocols for assessing patients taking antiplatelets or anticoagulants (other than ASA 100 mg) who are scheduled for retro/peribulbar surgery, and the office nurse must consult the anaesthesiologist before scheduling surgery.
Pre-operative testsCataract surgery is considered a very low-risk procedure, and evidence from large systematic reviews and studies has prompted scientific societies in several countries (France, United Kingdom, Spain, United States, Canada, etc.) to recommend foregoing preoperative tests (blood count, biochemistry, coagulation, chest X-ray, etc.) in these patients.13,14
The routine performance of complementary tests substantially increases the cost of the procedure15 and the corresponding delays can worsen the patient’s clinical status, thereby increasing the risk of perioperative complications.16,17
The indication for NOT performing routine preoperative tests in cataract surgery is included in the 5 “do not do” recommendations of the Spanish Society of Anaesthesia18; however, instead of being based on the patient’s clinical history and examination, testing is usually an individual decision or a hospital requirement motivated by medicolegal or economic factors, and continues to be common practice in many outpatient surgery units. As such, the tendency to order preoperative tests appears to be on the increase.19,20
Most cataract surgeries (over 90% of procedures) can be performed under topical or sub-tenon anaesthesia. If neither of these techniques is used, peribulbar anaesthesia is recommended.21 A small percentage of patients may be candidates for general anaesthesia, either due to lack of cooperation, excessive trembling, or other reasons. Surgery is still considered very low risk, even in these cases, so routine preoperative tests would not be indicated. Additional testing, if required, should be ordered ad hoc, on the basis of the patient’s clinical history and their baseline status.
In patients treated with vitamin K antagonists, clinical practice guidelines and consensus documents recommend verifying coagulation status by determining preoperative INR values.22,23
Management of background medication. Anticoagulants and antiplatelet agentsPatients scheduled for cataract surgery under topical anaesthesia should continue to take all their background medication. The protocols in place in each hospital should be followed in the case of insulin-dependent diabetic patients. The usual recommendations should be followed in patients receiving general anaesthesia.
The preoperative management of anticoagulants and/or antiplatelets deserves special mention. The surgeon must stratify the patient’s bleeding risk on the waiting list registration form, taking into consideration all local and systemic factors. Generally speaking, cataract procedures under topical or sub-Tenon block are considered to have a low risk of bleeding.24
Peribulbar anaesthesia is a superficial block with a low risk of bleeding. Retrobulbar anaesthesia has a moderate risk of bleeding, and may be required due to the characteristics of the cataract or the patient. For this reason, all anticoagulant and/or antiplatelet medication should be maintained in patients undergoing cataract surgery under topical and/or peribulbar anaesthesia.25,26 According to the Royal College of Ophthalmologists and the British Society for Haematology, cataract surgery under topical anaesthesia can be performed in patients taking dual antiplatelet therapy.27 In patients treated with warfarin or clopidogrel, peri-orbital (peribulbar or retrobulbar) injection has been associated with an increase in minor complications, but not in the risk of surgical bleeding or major complications that could compromise subsequent visual acuity.28,29 In these cases, the use of topical anaesthesia should be prioritized, but there is no contraindication for regional anaesthesia.
In patients taking direct oral anticoagulant drugs, consensus documents23 recommend maintaining this treatment during procedures with a low risk of bleeding. In procedures with high risk of bleeding (due to local factors and/or need for regional anaesthesia), the surgical team should reach a consensus after assessing the risk of bleeding or thrombosis. It should be noted that current European guidelines consider peribulbar block to be a “superficial block”, so the patient’s antithrombotic medication should be maintained.30
Informed consentInformed consent is the process in which a patient freely, voluntarily, and expressly accepts or rejects a medical procedure that affects their health after receiving sufficient, clear, individualised information about the proposed procedure, its purpose, benefits, risks, possible consequences, including alternative procedures, and the consequences of not performing the proposed procedure. Informed consent is not only a clinical procedure, but also a deontological obligation and legal compulsion that has important legal consequences. It is now also considered a human right and is enshrined in the Spanish Constitution.31–34
All patients scheduled for cataract surgery must sign the corresponding informed consent form. The SEDAR Informed Consent working group (2020) drafted the following recommendations applicable for patients requiring sedation, monitored anaesthesia care or general anaesthesia.35
Written informed consent is essential and complements verbal information.
- •
The signed informed consent form is part of the patient’s medical history, and as such must be kept on file for a minimum or 5 years or the number of years legally established by each autonomous community from the date of discharge from the care process (article 17.1 of Act 41/2002).
- •
It must be obtained by the anaesthesiologist; in no case is it permissible to delegate this obligation to other professionals.
- •
The information required by the patient to freely decide to grant or refuse consent must be provided far enough in advance to enable the patient to adequately consider their decision. The autonomous communities of Valencia, Extremadura and the Basque Country require informed consent to be obtained at least 24 h before the procedure is performed.
- •
The corresponding Spanish law requires the information be provided with sufficient advance notice, without mentioning the signing of the informed consent form. It is perfectly acceptable for the patient to wish to sign the informed consent form after having had time to consider the information received. The mandatory advance notice period starts the moment the patient is given the information.
- •
Advance information is not required prior to anaesthesia in the following circumstances:
- -
The patient is asleep or his or her judgement is impaired.
- -
The patient is already inside the operating room or the room where anaesthesia will be administered. By extension, this implies that advance information is not required when the patient is in other areas in the surgical suite, such as the patient reception area or the holding area.
- •
The patient can be provided with information about the procedure at any time before being given the informed consent form.
- •
In cataract surgery involving both eyes, informed consent for administering anaesthesia in both eyes or in each separate eye can be obtained during the same pre-anaesthesia assessment, as long as this is specified in the consent form and in the medical history.
- •
Centres that give patients the option of signing the informed consent form digitally must be aware the Act 59/2003, of December 19, on electronic signatures distinguishes between 2 types of signature: the “advanced electronic signature” and the “qualified electronic signature”. By law, only a qualified electronic signature can be considered equivalent to a handwritten signature.
- •
Spanish Act 59/2003 on electronic signatures provides that no paper document is required when the patient signs electronically with a qualified electronic certificate, such as the one included in their eDNI or a digital certificate issued by a trusted provider.
- •
The advanced digitized handwritten signature detects the patient’s biometric data and affixes a time stamp, and is legally binding provided other conditions included in Regulation (EU) 910/2014 of the European Parliament and of the Council of 23 July 201436 or the IDAS regulation are met.
- •
Electronic signature systems that use an OTP (one time password) for signing informed consent are not currently recommended.
In all cataract surgery pathways, the ophthalmologist performs the first evaluation and fills out the waiting list registration form. Following the recommendations made by various ophthalmology associations, the patient must be assessed to determine the existence of local and systemic factors, and these must be recorded in their clinical history. This assessment includes the risk of perioperative bleeding, the presence of monocular vision, and individual factors such as motor or psychological and intellectual difficulties. These factors indicate the need for sedation and/or general anaesthesia. The preliminary evaluation plays a key role in screening for patients with particular physical or psychological conditions so that they can be referred to different pre-anaesthesia assessment models. Several authors consider that routine clinical evaluation of all patients scheduled for cataract surgery has “little value” in low-risk patients16 and adds considerably to the cost of the intervention.16,37
The Anaesthesiology Service can perform the pre-anaesthesia assessment using different models: a “high-resolution consultation” or a conventional model, either in person or by telephone/online.
High resolution consultationPatients scheduled for cataract surgery are initially candidates for topical local anaesthesia techniques, with or without sedation regardless of their ASA class.
High-resolution consultations [in which the patient is assessed in a single visit] are recommended in all collaborative patients with ASA class I to III scheduled for lens, cataract, or clear lens surgery under topical anaesthesia. This model facilitates the pre-anaesthesia assessment for the patient and/or their family. It is a cost-effective approach that does not endanger patient safety.38
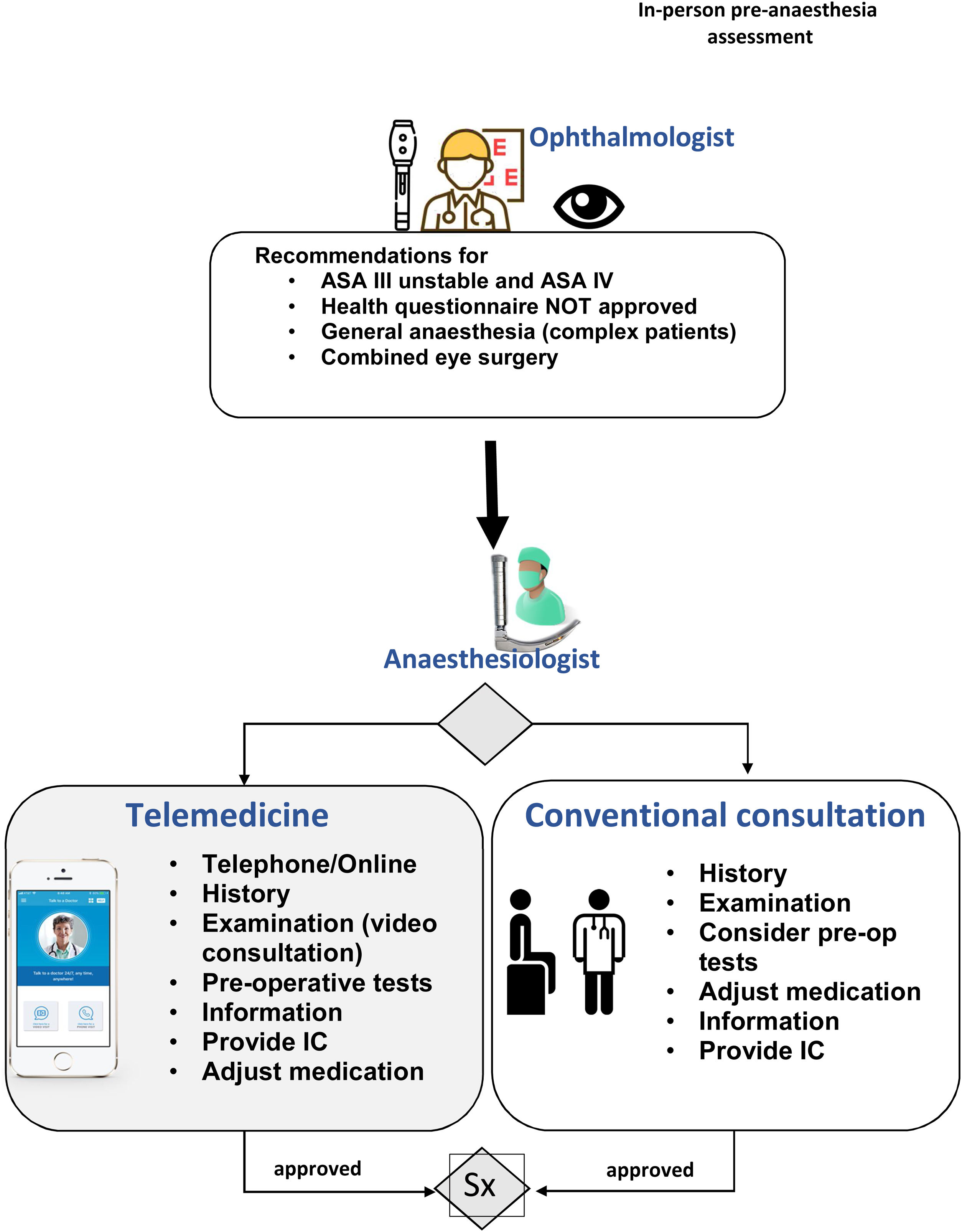
Depending on the regulations in force in each autonomous community and the availability of technological and human resources, the patient can be assessed using different care pathways (Fig. 1).
- •
Preoperative assessment using self-reported health questionnaires. The questionnaire can be made available on an app, downloaded from a website, or sent by email, and can be used to classify the patient according to their health status and their need for preoperative optimization (suspension of drugs, complementary tests, optimization of health status), in which case they can be referred to an in-person consultation.
- •
Preoperative telephone/online assessment supported and validated by an anaesthesiologist. Patients that are considered unsuitable are referred to an in-person consultation for further study and preparation before the intervention. The Anaesthesia and Ophthalmology services should work together to develop specific protocols for patients scheduled for retro/peribulbar surgery who are taking antiplatelets or anticoagulants other than ASA 100 mg.
- •
After prior screening by the ophthalmologist and the anaesthesiologist, the patient’s clinical history and the results of their physical examination and preoperative tests are assessed and they are given an informed consent form to consider before the intervention.
As shown in Fig. 2, the ophthalmologist refers all patients classified by the health questionnaire as unsuitable, unstable ASA III patients, ASA IV patients, and complex patients requiring general anaesthesia to an anaesthesiologist for assessment. The pre-anaesthesia assessment can performed over the phone or online (depending on the technology available in the health centre) or in person.
In both the in-person and online assessment, the patient’s medical history must be taken and they must be informed about the anaesthetic procedure, their background medication must be adjusted, if necessary, and the need for tests or consultation with other specialists must be assessed.
If the pre-anaesthesia assessment has been performed over the phone, the airway examination can be performed prior to the intervention, and the findings should be recorded in the patient’s clinical history.
If a telematic assessment is performed, the patient will need to sign the informed consent before surgery, within the established legal deadlines. This can be done using a qualified electronic signature, and advanced digitalized signature, and a handwritten signature prior to the surgical procedure.
ConclusionsEfficient cataract surgery management is a priority objective of our health system, and as anaesthesiologists we must introduce a management model that is adapted to our setting and requirements while ensuring quality of care, patient safety and legal compliance. The aim of this consensus document is to provide anaesthesiologists with a flexible decision-making strategy that can be used to implement these models in a variety of care settings.
Conflict of interestThe author declares that they have no conflict of interest.