The aim of this study was to evaluate the predictability of immediate loading in conjunction with one-piece post-extraction implants in the mandible using atraumatic threaded bone expanders.
Material and methodsA total of 56 patients were enrolled in this retrospective study and received 448 implants in the mandible, each patient received 8 implants; 4 in the anterior mandible and 2 in each side in the posterior mandible. Atraumatic threaded bone expanders were used to prepare the osteotomy site before the insertion of one-piece post-extraction implants, followed by immediate loading. The definitive prostheses were delivered to patients after 3–4 months.
ResultsA total of 9 implants were lost in 3 patients (2%) during the period of osseointegration indicating a survival and success rate of 98% in a study period of 1–10 years. No other implant failed after that nor have been any complication during the rest of the follow up period.
ConclusionsOne-piece implants submitted to this technique have converted to a predictable procedure, it is success in the mandible in this study of 10 years was 98%. However, it is necessary to determine the cases that are indicated for this procedure, as well as the characteristics of the implant, which favour immediate implantation.
El objetivo del presente estudio era valorar la predictibilidad de la carga inmediata con implantes monofásicos postextracción en el maxilar inferior, utilizando los expansores roscados atraumáticos.
Material y métodosSe realizó un estudio retrospectivo en 56 pacientes rehabilitados con 448 implantes en el maxilar inferior: 8 implantes a cada paciente, 4 en la zona intermentoniana y 2 en la zona posterior en cada hemiarcada. Los expansores roscados atraumáticos fueron utilizados para preparar la osteotomía antes de la inserción de los implantes monofásicos postextracción, seguida por carga inmediata. Las prótesis definitivas se adaptaron a los 3-4 meses.
ResultadosSe perdieron 9 implantes en 3 pacientes (2%) durante la fase de oseointegración, indicando una supervivencia y éxito del 98% en un periodo de estudio entre uno y 10 años. Ningún implante se ha perdido después, ni se evidenciaron complicaciones durante el resto del seguimiento clínico.
ConclusionesTras haber analizado toda la secuencia referida a la carga inmediata, podemos concluir que los implantes monofásicos insertados con la aplicación de esta técnica son un procedimiento predecible: su éxito en el maxilar inferior en nuestro estudio de 10 años fue del 98%. Sin embargo, es necesario determinar los casos candidatos para dicho procedimiento, así como las características del implante que favorecen la implantación inmediata.
Over the last 40 years the rehabilitation of endontodeous patients with implant-supported dentures has evolved as a feasible and predictable treatment option. Long-term studies have shown high survival rates with original protocols. Based on these premises, researchers have described osseointegration. In consequence, implants have been used in more adverse situations and for broader indications.1,2
The concept of immediate load is a significant line of research in modern implantology. Brånemark's original protocol recommended long periods of rest out of function, to attain the osseointegration of dental implants. However, this mandatory clinical recommendation has been questioned in recent years. A large number of professionals support immediate or early load of implants. The benefits of immediate load are clear: it requires shorter treatment periods and allows for an immediate recovery of functions and aesthetics. The high success rates of immediate-load dentures have been thoroughly reported in previous reviews.3,4
Another concept is the immediate placement of dentures after tooth extraction. This type of procedure has clear advantages compared to deferred loading of the implant after tissues have formed; for example, post-extraction bone re absorption is reduced and the collapse of soft tissues around the bone is minimised. The elimination of the use of surgical drills in the formation of the alveolar bed reduces the potential for heating in the perforation area during preparation, resulting in a reduction in the rehabilitation time by combining post-extraction healing and bone regeneration around the implant.5
The high predictability of both concepts has led to a bimodal approach in which the placement of implants after extraction is combined with the immediate load of the dentures. The main advantage of this approach is a combination of the preservation of the alveolar bone by the implants and the preservation of the peri-implant mucosa by the immediate loading.6
The evolution of oral implantology has also delivered significant technological developments; the design of implants has changed, with improved thread patterns and surface treatments that have demonstrated higher primary stability of the implants and faster healing. Consequently, in recent years a significant number of professionals have used monophasic implants that protrude from the soft tissue with a temporary denture in immediate load.7 The design of one-piece implants eliminates the structural weakness of a two-piece implant system and avoids the manipulation of the soft tissues around the implant after the initial healing.8 Additionally, this system is designed to reduce marginal bone re absorption, since there are no submucosal microspaces between the implant and the gum.9
Another development in implantology is the use of extended threads to place the dental implants, albeit in a moderately traumatic manner. This technique is based on a bone condensation process which results in enhanced bone density and improves the reorientation of the axis of the implant, thus enhancing primary stability. This relatively non-invasive technique attains success rates similar to those of conventional implant insertion techniques.10–12
With the aim of reducing the process of bone re absorption and the duration of the treatment, the present study was carried out to assess the clinical results of treatment with monophasic implants placed in the inferior maxillary bone after extraction, by means of bone condensation techniques, using non-traumatic thread extensors and immediate load.
Material and methods56 patients aged between 45 and 62 years were selected to participate in this study between 2001 and 2011. This retrospective study was approved by the Ethics Committees and the Institutional Review Board from the Oral and Maxillofacial Surgery Department of the Faculty of Dentistry in Alexandria (Egypt), and was conducted through an agreement between a private centre and the university department, both directed by the same surgeon.
The patients selected for this study had teeth affected with periapical disease or advanced adult periodontal disease, with several degrees of mobility or radicular remains, and required the complete rehabilitation of their inferior maxillary bone. The selected patients were considered to have sufficient posterior bone height to receive 10–12mm implants.
The patients who had acute systemic disorders that could compromise osseointegration were excluded. Patients with metabolic disorders (for example, osteoporosis or uncontrolled diabetes) that could interfere with implant healing or could affect the mandible bone were not included. Patients who had received radiation, who were smokers, or who were considered high-risk patients for other reasons were also not included.
All the patients treated in this sample were informed about the protocols regarding treatment with implants, the surgical and prosthodontic aspects of the treatment, the duration of the treatment, the subsequent clinical follow-up and the potential for complications, including the loss of implants. All the patients authorised the implant treatment by signing an informed consent form.
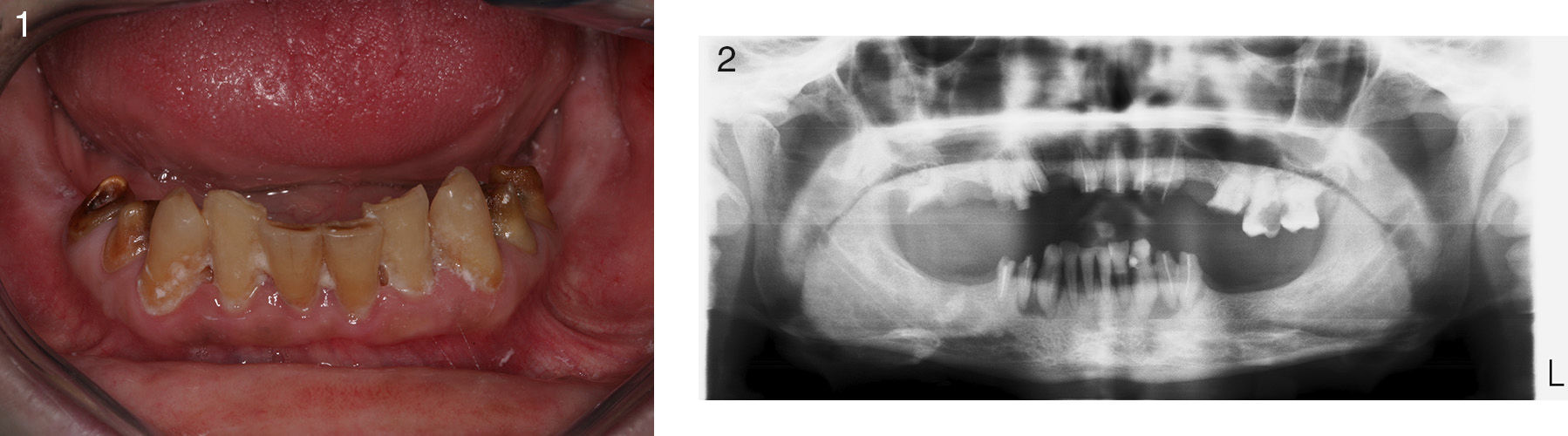
Before performing the implant treatment, all the patients were radiologically assessed using orthopantomography. Where the clinical and anatomical features of the patient required it, an axial computerised tomography scan was performed, which enabled a further assessment of the size of the anatomical structures (Figs. 1 and 2).
After conducting a radiographic diagnosis, imprints were taken and models were created in order to reproduce the patient's occlusion as accurately as possible. Surgical guidance appliances were prepared in order to simplify the placement of implants in the mandibular arch.
Surgical techniqueAn hour before surgery, we injected the patients with a compound of sodium succinate methylprednisolone (Solu-Moderín® 125mg, Pfizer, Barcelona, Spain) and lincomycin HCL (Lincocin® 600mg, Pfizer, Barcelona, Spain). Also before the intervention, the patients washed their mouths with 0.2% chlorhexidine gluconate and then disinfected with iodate povidone.
To perform the extractions and the curettages thoroughly, preserving the cortical layers of bone and ensuring the primary stability of the implants, surgery to the posterior area was performed under buccal and crestal infiltration anaesthesia. To approach the risk areas without damaging the frontal area, truncal anaesthesia of the inferior dental nerve and the lingual nerve was established using articaine HCL 4% and epinephrine 1:100,000 (Septocaine®, Septodont, France).
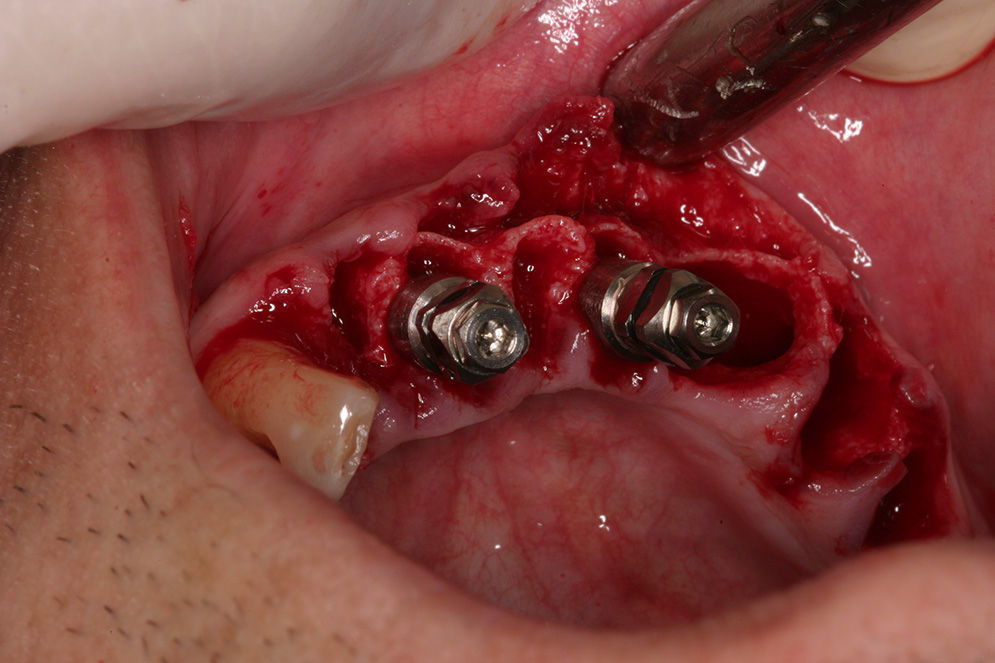
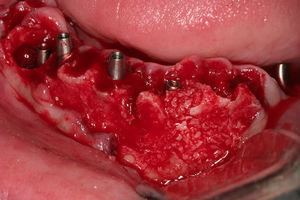
The mucoperiosteal flap design was a total extension to the free ends. Where the width of the bone was below 3mm (measured by an ostheometer), advanced bone expansion techniques were implemented. This was the case in 76.8% of the patients, where a piezosurgery tool was used to perform the corticotomy. In the subsequent bone expansion, we used thread extensors (Microdent Implants System™, Barcelona, Spain), applied progressively with a ratchet, until the implant bed was formed. In the other 23.2% of the patients whose bone width was equal to or above 3mm and who had properly keratinised gums, we opted for a non-traumatic technique performed with punch flaps and the implementation of bone condensation, using a 1.80mm pilot drill and the non-traumatic bone extensors described above. After forming the implant bed, monophasic implants were fixed, of which the selected lengths were between 10 and 12mm (Fig. 3).
Surgery to the frontal area was carefully carried out around the papillae and the crestal bone, extracting the dental pieces and preserving the integrity of the vestibular and lingual layers of the bones. After the extractions, the granulation tissue in the periapical area was thoroughly curetted with Bunge evisceration spoons, a rounded carborundum wolfram drill, surgical hand tools and an irrigation solution.
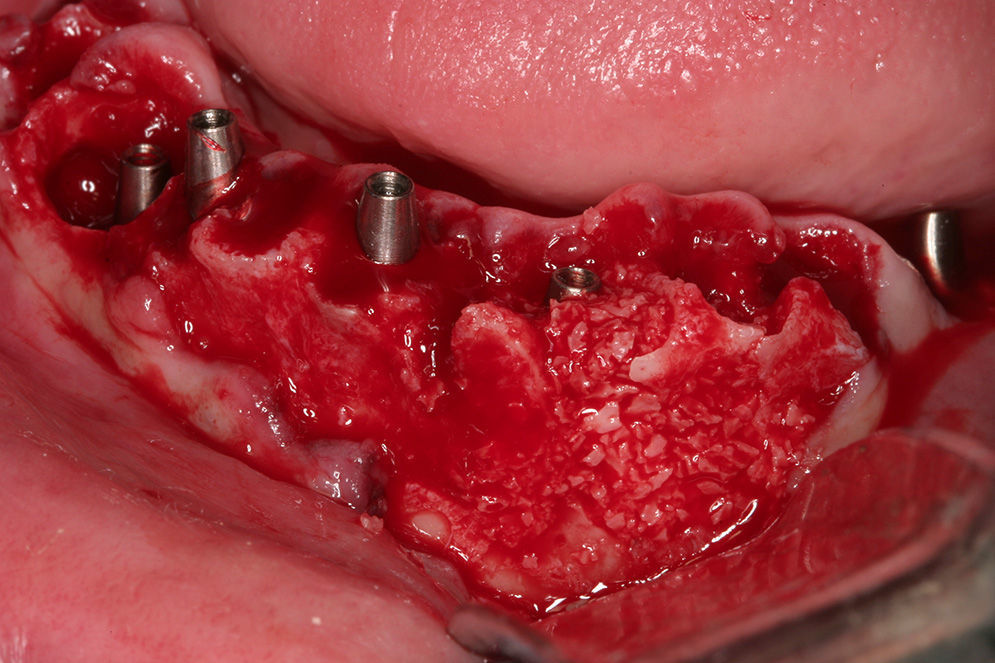
Once the alveolus was released from pathological tissues, we used a 1.80mm diameter pilot drill to perforate 3mm below the alveolus’ apex. We then identified an adequate position for the implant in both the corono-apical direction and vestibular-lingual direction, with a 30° lingual inclination. After performing the osteotomy, we applied the bone condensation technique using thread extensors to improve the density of the trabecular bones and generate a bone apposition mechanism. We followed this procedure in the adjacent teeth, maintaining proper distance between implants, which did not obstruct the design of the posterior denture (Fig. 4).
In the frontal area between the foramina, 14mm monophasic implants were used. The difference between the alveolus and the implants, caused by previous fractures in the bone layers, during surgery or by the elimination of granulation tissue, was filled with cortical bone block particulate using a gouge (dental Osteobiol Tecnoss®, Torino, Italy) (Fig. 5).
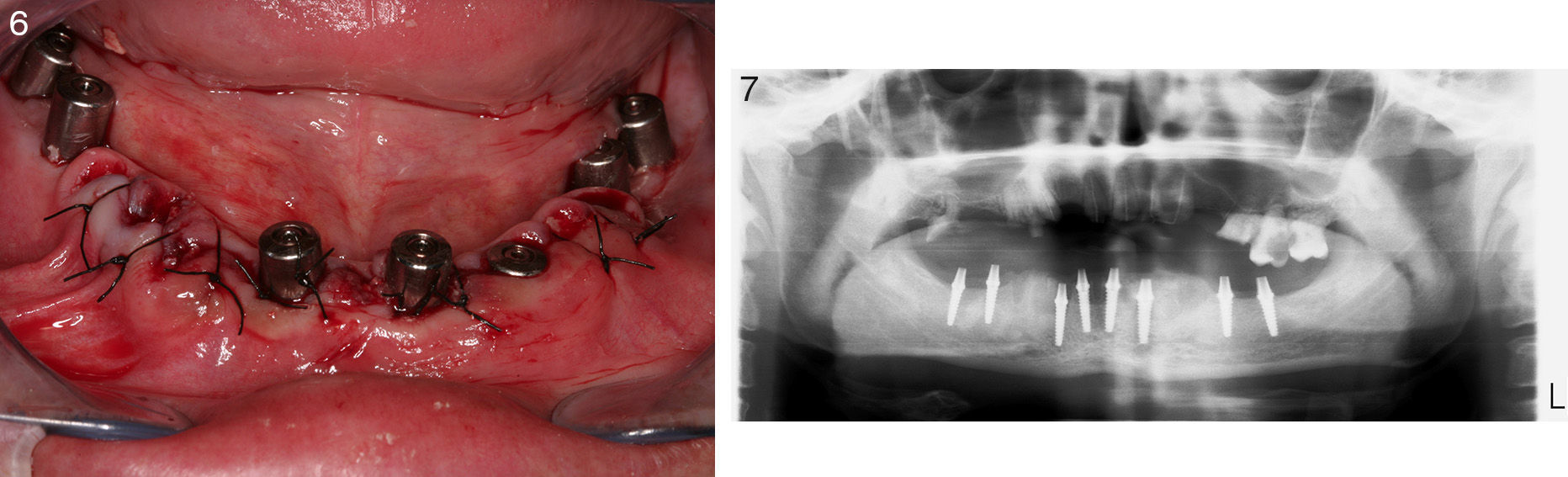
The implants were placed with a primary stability of 40N/cm. Eight implants were placed in the inferior maxillary bone of each patient: Four implants were placed in the frontal area and two in each posterior quadrant. The implants used were monophasic: the body of the implant and the base were one piece (MRT™ implants, Microdent Implants System, Barcelona, Spain). MRT implants are designed for immediate load, they can be cemented or screwed, and they can be sculpted and shaped in the mouth to correct their angle (Fig. 6).
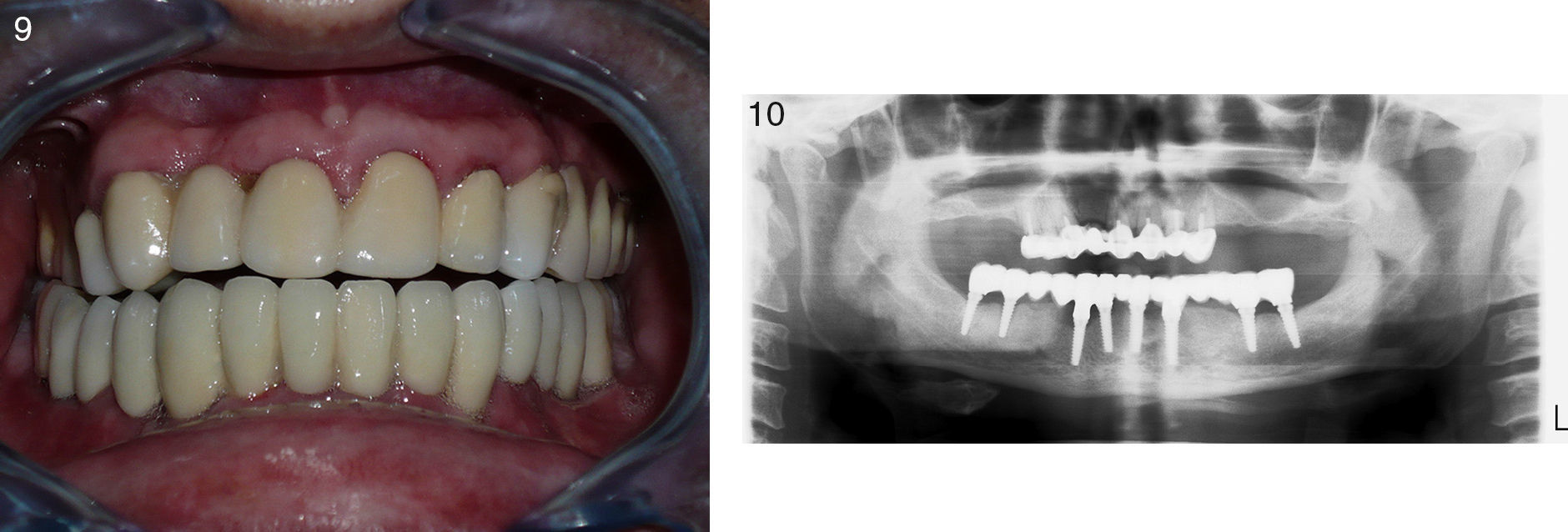
The flaps were repositioned and sutured with single separated stitching using vicryl 5/0. Surgical guidance appliances were used to encourage the immediate rehabilitation of the temporary dentures, with mutually protected occlusion, according to the group. These guidance appliances were filled with resin and became temporary dentures for immediate load; they were easy to prepare by casting a mould on the implants’ pillars. To add more resistance, we splinted the temporary dentures with orthodontic wires and they were cemented with oxyphosphate. Once the temporary dentures were in place, we performed a radiography to verify the positions and angles of the implants (Figs. 6 and 7).
All patients were prescribed a pharmacological treatment of intramuscular injections of sodium succinate methylprednisolone 125mg and lincomycin 600mg for three days, and ibuprofen in 600–800mg doses depending on weight, every 6 or 8h for one week. Ten days after the intervention, we removed the stitches and re-cemented the temporary dentures with permanent cement, which would remain in the mouth for a period of three to four months depending on the bone density that the mandibular bone provided.
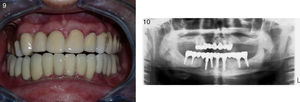
After three to four months the temporary dentures were removed. We took imprints to prepare the permanent ceramo-metallic dentures and screwed or cemented them in place (Fig. 8). We performed a radiographic analysis of the adjustment of the final placement of the dentures and passive adjustment, and a further radiographic analysis was performed after one year.
ResultsThis study included 56 patients who presented for tooth extraction due to periapical affectation (62.9%) or advanced adult periodontal disease (34.6%), and with radicular remains (2.5%). 41 (73.2%) were females and 15 (26.8%) were males, with an average age of 51 years (range 45–62 years).
Patients did not suffer any immediate postoperative symptoms such as pain, oedema, trismus or paresthesia. None of the patients had postoperative infections.
A total of 448 implants were inserted. After the extractions, four implants were inserted in the frontal area of the inferior maxillary bone in each patient. The implants were 14mm long and 3.85mm in diameter. The other 224 implants were fixed on the free ends of each mandible quadrant, positioned between the areas of the second premolar and the second molar, with a diameter of 3.85mm and lengths between 10mm (69%) and 12mm (31%).
From the 448 implants inserted with immediate load via fixed temporary dentures directly after surgery, nine (2%) were lost from the posterior sector; in two patients the implants were lost when taking the imprints and one patient lost the implants during the healing stage, when he exhibited pain and movement of the implants. None of the implants were lost following the insertion of the final dentures or during the clinical follow-up period.
The radiographic analyses conducted during the follow-up period revealed an absence of peri-implant radiolucency that could indicate signs of implant failure, representing a 98% success rate (Figs. 9 and 10).
DiscussionThis long-term study assessed the clinical results of treatment with monophasic osseointegrated implants using a technique consisting of the insertion and immediate load of dentures. The retrospective study carried out by Sohn et al. described a 100% success rate for monophasic implants over a follow-up period averaging 23 months after placement.13 Similarly, Reddy et al. reported a 96.7% success rate in 17 patients treated with 31 monophasic implants.14
In this study, none of the patients had postoperative symptoms or complications. Due to the complexity and length of the procedure, a combination of lincomycin and methylprednisolone was used after surgery. Lincomycin is an antibiotic of the lincosamide group, similar to clindamycin. The effectiveness and safety of clindamycin for the prevention of dental infections has been demonstrated by Brook et al.15 and Gutiérrez et al.16 According to these studies, implant insertion is a high-risk procedure and because clindamycin is very effective within the field of dentistry, it must be considered as a first-line antibiotic for the treatment of any type of dental infection.
Regarding the use of methylprednisolone, Prieto et al.17 reported that dexamethasone and methylprednisolone were the most frequently used corticosteroids, being the most effective in controlling inflammation and trismus symptoms in third-molar surgeries. Similarly, Carranza and Abanto18 report using corticosteroids in third-molar surgery procedures.
The protocol for immediate implant insertion was performed in this study with the aim of shortening the process of bone re absorption and treatment times.19 We implemented this technique after extracting the remaining teeth. We used a 1.80mm diameter pilot drill to increase the depth of the alveolus following extraction in the mandibular symphysis, in order to insert long, 14mm implants. To this effect, we aimed for primary retention of the implants, with bone condensation by means of a bone apposition process, conformed by non-traumatic thread extensors to dilate and conform a new alveolus. After forming the implant bed, we immediately inserted the implant applying torque of 40N/cm.
It is essential for the implant to have clear primary stability for immediate load. This is generally obtained using long implants, in excess of the 3–5 apex.20 Gatti et al.21 and Ericsson et al.22 recommend implants no shorter than 10mm. In addition, Horiuchi et al.23 recommended immediate load for only those implants that were placed with a torque equal or larger than 40N/cm. Wörhle24 reported placing 14 implants in the alveolus following extraction where the insertion torque was 45N/cm, and obtained 100% success after 9–36 months.
The clinical results of the implant insertion by means of osteotomes are usually similar to those inserted in a conventional manner.25 This technique multiplies bone neoformation and stimulates osseointegration mechanisms in the trabecular bone. In this regard, the technique increases bone density and primary stability of the inserted implants. In addition, the use of thread extensors involves reduced potential for overheating the bone bed in comparison with classic cutting.26,27
The success rate of this study was 98%, taking into account the clinical and radiographic results after a 10-year follow-up. From the 448 implants, nine (2%) failed during the osseointegration period. The location of failed implants was in the posterior free ends of the mandible; none of the implants in the mandibular symphysis failed.
Treatment in the frontal mandibular area, with immediate load, had a success rate over 93% for a minimum of four implants in the intermental region. This level of success is similar to that reported in other studies; Ericsson et al.22 placed between five and six intermental implants in 16 patients, and after a five-year follow-up none had failed; Ganeles et al.28 reported only one failure among 161 mandibular implants where between five and eight implants were placed in each of 27 patients with an average follow-up period of 25 months and Jaffin et al.29 attained a 93% success rate treating 27 patients with four intermental implants each, with a follow-up period between 6 and 60 months. In the posterior mandibular area, success rates are not as favourable. Schnitman et al.30 reported the loss of four (15.3%) out of 28 implants in the inferior maxillary bone within a period of ten years and they suggested a long-term guarded prognosis in immediate load of distal mandibular implants in the mental region.
The success rate in this study coincides with other studies, for example, Grunder,31 who placed 66 post-extraction implants with load after 24h. The success rate in the mandible was 97.2% after two years. Colomina32 also had a 96.7% success rate after 18 months in 32 mandible implants with immediate load.
The existence of periapical conditions did not affect the success of this study. All the implants that were placed in areas where there was a periapical process exhibited similar survival rates to those of the implants placed in locations without chronic conditions. Recently, several studies have been conducted to assess the clinical success of implants after extraction in locations with periapical conditions. The results show high success rates, provided that proper clinical procedures are conducted prior to the placement of the implant, for example, meticulous curettage of the alveolus, rinsing with chlorhexidine and the administration of antibiotics prior to and after surgery.33–35
This supplementary approach provides a promising treatment option with the advantages of minimising treatment time, preserving both the soft tissues and the bone around the implant and offering the patient immediate and more comfortable rehabilitation in a single visit.
The implementation of new technologies has enabled the evolution and development of surgical techniques that have been broadly used in implantology, aiming at reducing surgical morbidity and offering the patient a less invasive surgical/prosthetic treatment. Further to this, computer tomographies and specialised software now allow surgical-prosthetic planning in a virtual setting imformed by an accurate three-dimensional bone visualisation and its relationship with the future denture. In virtual planning, it is possible to assess and measure bone density; to select the type, size and amount of implants; to verify their location, angle and depth level in relation to the bone; to verify the chances of implant bicorticalisation and to analyse the features of the intermediaries and the fixing screw of the future denture.36,37
When compared to the traditional technique, the installation of implants by means of guided techniques requires greater financial investment and more detailed planning; however, they offer positive clinical results, in that they eliminate or minimise errors and allow the systematic reproduction of treatments with success and longevity.38
ConclusionAfter analysing all factors concerning immediate load, we can conclude that monophasic implants subjected to this technique constitute a predictable procedure: their success rate in inferior maxillary bones in our 10-year study was 98%. However, it is necessary to specify the candidate cases for this procedure, and the characteristics of the implant that best favours immediate implantation.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestNone.
Please cite this article as: Eldibany RM, García-Rodriguez J. Carga inmediata de implantes monofásicos postextracción utilizando los expansores roscados atraumáticos: estudio retrospectivo 2001-2011. Rev Esp Cir Oral Maxilofac. 2015;37:207–214.