The Beckwith–Wiedemann syndrome is a congenital disorder with diverse clinical manifestations, among which the most prevalent are, macroglossia (97%), gigantism (88%), and abdominal wall defects (80%). Orthodontically, most patients present with anterior open bite and Angle Class III malocclusion. Macroglossia can cause cosmetic problems and functional abnormalities associated with speech, mastication, swallowing and breathing, with potential obstruction of the upper airways and decreased stability of orthodontal-surgical treatment. In order to avoid episodes like this, a partial glossectomy is necessary in some patients. This article looks at the diagnosis and treatment of macroglossia, while presenting the case of a patient with Beckwith–Wiedemann syndrome who underwent surgery by partial glossectomy using the technique advocated by Obwergeser et al. in 1964, and 3 years postoperatively showed good cosmetic and functional results.
El síndrome de Beckwith-Wiedemann es una alteración congénita con diversas manifestaciones clínicas, de entre las cuales las más prevalentes son la macroglosia (97%), el gigantismo (88%) y los defectos de la pared abdominal (80%). Ortodónticamente, la mayoría de los pacientes presentan mordida abierta anterior y relación de clase III de Angle. La macroglosia puede causar problemas estéticos y anomalías funcionales relacionadas con el habla, la masticación, fonación, deglución y respiración, con potencial de obstrucción de las vías respiratorias superiores y disminución de la estabilidad del tratamiento ortoquirúrgico. Con el fin de evitar episodios como este, es necesaria la realización de una glosectomía parcial en algunos pacientes. El presente trabajo realiza consideraciones con relación al diagnóstico y tratamiento de la macroglosia y relata el caso clínico de un paciente portador del síndrome de Beckwith-Wiedemann que fue intervenido por medio de glosectomía parcial, utilizando la técnica preconizada por Obwergeser et al. (1964) y que en un postoperatorio de 3 años presentó resultados cosméticos y funcionales satisfactorios.
The Beckwith–Wiedemann syndrome, first described by Beckwith1 and Wiedemann,2 is a rare congenital disease that involves an overgrowth disorder and affects one in 14,200 newborns.3 Its origin may be hereditary (15%) or originate in genetic alterations in the chromosome 11p15.5 region (75–80%).4
The main characteristics of the Beckwith–Wiedemann syndrome are: macroglossia (97%), gigantism (88%) and defects of the abdominal wall such as omphalocele, umbilical hernia and diastasis recti (80%), followed by abnormal creases in the ear lobes (76%), hypoglycaemia (63%), facial nevus flammeus (62%), kidney abnormalities (59%), haemihypertrophy (24%), congenital heart defects (6.5%), intestinal problems (5%), neoplasia (4%), mental retardation (4%), polydactyly (3%) and labial-palatal fissure (2.5%).3
Macroglossia is defined as a tongue that in the resting position protrudes beyond the teeth towards the alveolar ridge. It has a multifactorial aetiology and it is classified in true and relative macroglossia. The relative macroglossia occurs when the tongue has a normal size, but the intraoral space is insufficient and the true one is observed due to an increase in its volume.5
Among the characteristics of the Beckwith–Wiedemann syndrome, macroglossia represents 97% of the incidence, and this condition may cause a functional and aesthetic abnormality with speech, mastication, deglutition and suction difficulty.6 There is also the risk of upper airways obstruction during childhood and adolescence, of development of obstructive sleep apnoea syndrome and even of decrease in the stability of the orthosurgical treatment.3,7,8
As for the maxillofacial morphology, some specific findings may be found in patients carrying the Beckwith–Wiedemann syndrome, such as bimaxillary protrusion, mandibular protrusion, goniac angle and increased mandibular body. Orthodontically, most patients present anterior open bite, negative overjet, Angle Class III relationship and vestibular inclination of the anterior elements. These characteristics depend on the patient's degree of macroglossia.9
Many of those patients present important functional problems or may be candidate for orthognathic surgery and they need partial glossectomy for the oral functions dependent on the tongue to be restored and to obtain improvement of the foresee ability of the bone movements, especially all those that involve the jaw.
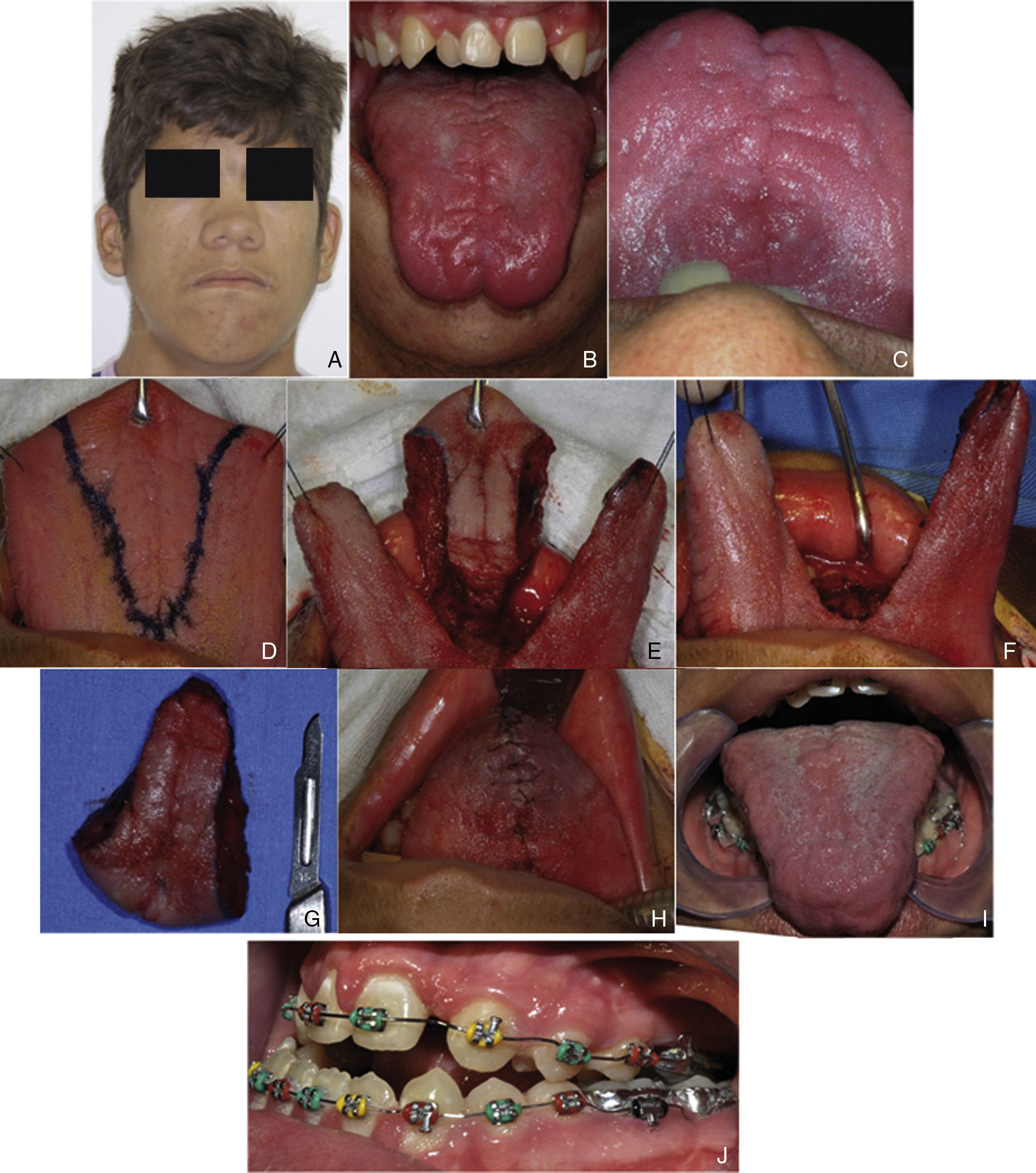
Case descriptionPatient receiving H.V.P.D., 16 years, presented with main complaint of phonation difficulty. During the physical examination, patient showed elevated height, facial pattern III, with severe maxillary hypoplasia, dental crowding, Angle Class III relationship, anterior open bite, bifid uvula and macroglossia (Fig. 1A–C). At the data collection during anamnesis, it was also revealed that, at birth, patient had an abdominal wall defect that was later corrected. All these findings contributed to the formation of the Beckwith–Wiedemann syndrome diagnosis.
(A) Facial pattern III, with severe maxillary hypoplasia, (B, C) dental crowding and macroglossia, (D) incision demarcation, (E) tongue fragment excision, (F) after tongue fragment removal, (G) surgical piece, (H) suture, (I) 3-year postoperative period, and (J) orthodontic treatment after glossectomy that shows class III malocclusion with anterior open bite.
Patient was included in the orthosurgical treatment, and deglutition and phonation problems and respiratory difficulties, with a strong correlation with macroglossia, were observed. Therefore, for this case, a surgical procedure of partial glossectomy was scheduled, before the orthognathic surgery procedure. The technique used was the one proposed by Obwegeser et al.,10 in which a resection of the central segment of the tongue and the tongue apex was performed, which achieved a decrease in its dimensions in the anteroposterior and transversal sense, to lessen the speech-related problems (Fig. 1D–H).
For appropriate transoperatory bleeding control and ease of execution, the surgery was performed under general anaesthesia with orotracheal intubation, due to the presence of nasal concha hypertrophy that prevented the passing of the nasotracheal tube. To perform the incisions, anatomical landmarks were established in the lateral and anterior extremities of the tongue with 2.0 cotton thread and an Allis tissue grasping clamp was used as auxiliary in the dissection. After stabilisation, incision demarcation with blue methylene and also infiltrations of local anaesthetic (lidocaine 2% with epinephrine 1:200,000) were performed. The removal of the demarcated segment was performed with an electrosurgical dissector (Colorado needle, Stryker Corporation®) in the apex-base direction, preserving the lateral edges and minimising the risk of lesions in the lingual nerve branches. The segment was removed and careful haemostasis was performed to minimise the risks of lingual haematoma and postoperative bleeding. After bleeding control, the segments were thoroughly approximated with resorbable thread (Vicryl 3.0-ETHICON) from the deepest to the superficial portion in the base-apex direction. In the immediate postoperative period, it was already possible to verify the anterior and transversal decrease of the tongue without airway involvement, and without any complication of haemorrhagic or infectious nature. Ten days after surgery, patient started phonoaudiologic therapy to assist in the recovery of tongue mobility and phonation.
Currently, 3 years after surgery, patient shows considerable decrease of the tongue in the transversal and longitudinal sense, without loss of sensitivity or taste in the region. He is following orthodontic and phonoaudiologic therapy with the purpose of performing a surgical procedure for the correction of the maxillomandibular discrepancy (Fig. 1I and J).
DiscussionThe clinical diagnosis of the syndrome is performed whenever the patient has the 3 main characteristics or whenever the patient has 2 main ones and 3 or more secondary ones.3 In this case, patient presents the 3 main characteristics: gigantism, abdominal wall defect and macroglossia, having the secondary characteristics associated: bifid uvula, mandibular prognathism and Angle Class III dental relationship.
According to Vogel et al.,5 the diagnosis of macroglossia is performed whenever the tongue in the resting position protrudes over the teeth or alveolar ridge and it may be classified as relative or true. In the case described, the macroglossia was related to muscle hypertrophy and, even though patient presented mandibular prognathism, the tongue protruded over the inferior teeth, which determined that it be considered a case of true macroglossia.
Macroglossia is present in 97% of the cases3 and it may cause, especially during childhood, dyspnoea, phonation, mastication, deglutition and suction difficulties.6,9,11 With the growth of the maxillofacial complex, there is an increase of the oral cavity volume, which enables a more comfortable fitting of the tongue, thus reducing the problems that arise as a consequence of the macroglossia. However, in some patients, with the maxillofacial growth, the improvement of tongue-dependent functions is not achieved successfully, so these patients (as in the case described) are candidates for a partial glossectomy.6,9,12
The hypertrophied tongue may be a factor that favours dentoskeletal deformities even in the growing phase, and it may also generate instability in the orthodontic and surgical treatment.7,8 Masubuchi et al.9 determined in their studies, after assessing 8 patients carrying the Beckwith–Wiedemann syndrome, that 100% of the patients assessed presented anterior open bite and class III facial pattern, 62.5% with negative overjet, characteristics that are present in the case described and that determine that the orthodontic treatment should be dependent on the degree of macroglossia.
The glossectomy is indicated in cases of functional problems such as airway obstruction, speech problems, deglutition problems, dental deformities, mandibular overgrowth, difficulty controlling the saliva, tongue trauma, lingual protrusion, cosmetic indications and in the improvement and stability of the orthodontic-surgical treatment.7,11,12 According to Medeiros et al.,8 the prognosis of the anterior open bite correction is less favourable in cases in which the tongue is related with the dentofacial deformity. Kadouch et al.12 after performing a retrospective study in 23 patients carrying the Beckwith–Wiedemann syndrome who were treated with partial glossectomy, found that 70% of the indications occurred based on a combination of lingual protrusion and functional deficiencies in mastication, breathing and phonation. In the clinical case described, the glossectomy indication occurred due to the speech difficulty and with the purpose of improving the stability of the orthodontic-surgical treatment the patient will be submitted to in the future, after orthodontic preparation.
Some authors have been treating the speech difficulty in patients with macroglossia with phonoaudiologic treatment only, but the case presented involves a patient with true macroglossia that would not be solved with conservative treatment, and that would not present improvement in the stability of the orthodontic-surgical treatment he will be submitted to.5,7–9,11
Several techniques, which may be classified in 6 groups, have been described for the correction of macroglossia: apex amputation; central reductions; wedge resections, dorsal flaps excision; marginal excisions and combined procedures. Among these techniques, central reductions and wedge resections are the most widely used.13,14 Obwegeser described a central reduction technique that includes incisions in the apex and in the middle part of the tongue, which promotes longitudinal and transversal reduction, even if it has as a limitation the maintenance of the tongue height.10,12,13 In the case described, patient had a tongue with dimensions accentuated in the anteroposterior and transversal sense, with thickness increased in the apex and in the middle part of the tongue. That is why the decision was made to use the Obwegeser technique10 that, due to its more rounded design in the middle part, promotes a thickness decrease in the apex and in the more posterior part of the tongue.
In the immediate postoperative period, there were no complications, such as excessive oedema or bleeding, that could cause a hypovoloemic shock or a haematoma with airways obstruction. To obtain this postoperative pattern, an efficient haemostasis is required, and the wound closing has to be performed with great accuracy, with sutures in the deep plane and in the more superficial planes of all the parts involved.
Other aspects to be observed in the selection of the surgical technique are the palate, and tongue sensitivity and mobility.14,15 Matsune et al.15 assessed the palate in 4 patients carrying the Beckwith–Wiedemann syndrome with paper filters soaked in bitter, sweet, salty and acid substances, after performing the partial glossectomy, and they found that the salty and bitter flavours needed a higher concentration to be tasted in comparison with patients that had not been intervened. According to Davalbhakta,14 regrowth after a partial glossectomy occurs mainly in children, since the impulse towards muscle hyperplasia in the Beckwith–Wiedemann syndrome may linger for long periods after birth. Because of that, it may be beneficial to postpone the partial glossectomy until the growth rates start to decrease. The glossectomy performed in the present case occurred after the patient was 15 years due to the difficulty in accessing a specialised service. After a 3-year follow-up, the tongue presents normal mobility and taste alterations were not perceived by the patient.
The partial glossectomy is a technique used very often in patients with Beckwith–Wiedemann syndrome and the indication and the ideal moment to perform the surgical procedure have to be taken into account to obtain the full benefits the procedure will generate.
Ethical disclosuresProtection of people and animalsThe authors state that no experiments were performed on human beings or animals as part of this investigation.
Data confidentialityAuthors state they have followed the protocols of their workplace about the data publication of patients.
Right to privacy and informed consentAuthors have obtained the informed consent from the patients or subjects referred to in the article. This document is in possession of the corresponding author.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Borborema dos Santos VD, de Assis GM, da Silva JSP, Germano AR. Glosectomía parcial en paciente portador del síndrome de Beckwith-Wiedemann: relato del caso. Rev Esp Cir Oral Maxilofac. 2015;37:202–206.