Previous research using osteochondral autograft transfer (OAT) has shown poorer outcomes with increasing patient age. The aim of this article is to evaluate a cohort of patients that received an OAT and to correlate their clinical results with their age at procedure.
MethodsPatients that underwent an OAT to treat an osteochondral (OC) lesion with a minimum 24-month follow-up were included. Patients were categorized into two groups based on their age at procedure (<40 years and ≥40 years). Postoperatively, each patient completed the Knee injury and Osteoarthritis Outcome Score (KOOS), International Knee Documentation Committee (IKDC), and Lysholm scales.
Results51 patients were included (35<40 years, 16≥40 years). Mean follow-up was 4.2 years (2–7). For patients<40 years, IKDC averaged 80.8 (SD 15.9) versus 71.2 (SD 19.4) in ≥40 years (p=0.03). For patients <40 years, Lysholm averaged 85.9 (SD 10.8) versus 77.0 (SD 21.6) in ≥40 years (p=0.02). For patients<40 years, KOOS averaged 78.3 (SD 11.8) versus 68.9 (SD 18.5) in ≥40 years (p=0.01). There was a 100% sensibility in identifying all the patients with a poor IKDC and Lysholm from 34 years old (AUC 0.76 and 0.8).
ConclusionsOAT has better outcomes in patients younger than 40 years compared to patients older than 40 years. Based on the prognostic capacity of age, the ideal candidate for an OAT is a patient younger than 34 years old.
Investigaciones previas en las que se ha utilizado el trasplante osteocondral autólogo (OAT) han mostrado peores resultados con el aumento de la edad del paciente. El objetivo de este artículo es evaluar a una cohorte de pacientes que recibieron un OAT, y correlacionar sus resultados clínicos con su edad al momento de la intervención.
MétodosSe incluyeron pacientes que se sometieron a un OAT para tratar una lesión osteocondral (OC) con un seguimiento mínimo de 24 meses. Los pacientes fueron categorizados en 2 grupos según su edad al momento del procedimiento (<40 años y ≥40 años). Después de la operación, cada paciente completó las escalas de evaluación KOOS, IKDC y Lysholm.
ResultadosSe incluyeron 51 pacientes (35<40 años, 16≥40 años). El seguimiento medio fue de 4,2 años (2-7). Para los pacientes de <40 años, la media del IKDC fue de 80,8 (DE: 15,9) versus 71,2 (DE: 19,4) en ≥40 años (p=0,03). Para los pacientes de <40 años, la media de Lysholm fue de 85,9 (DE: 10,8) versus 77,0 (DE: 21,6) en ≥40 años (p=0,02). Para los pacientes de <40 años, la media del KOOS fue de 78,3 (DE: 11,8) versus 68,9 (DE: 18,5) en ≥40 años (p=0,01). Hubo una sensibilidad del 100% en la identificación de los pacientes con un puntaje IKDC y Lysholm bajo a partir de los 34 años (AUC: 0,76 y 0,8).
ConclusionesEl OAT tiene mejores resultados en pacientes menores de 40 años en comparación con los pacientes mayores de 40 años. Basado en la capacidad pronóstica de la edad, el candidato ideal para un OAT es un paciente menor de 34 años.
Chondral and osteochondral (OC) lesions present a treatment challenge, as expanding lesions and surrounding cartilage overload can lead to degenerative joint disease that may limit an individual's activity level and lifestyle significantly.1 Treatment options are variable and dependent on many factors, including patient age and activity level, location and size of the defect, meniscal status, limb alignment, concomitant knee pathologies, chronicity, and comorbidities.2
Osteochondral autograft transfer (OAT) utilizes grafts that are taken from lesser-weight-bearing portions of the knee and transferred to more weight-bearing portions of the knee.3 Because of the use of autograft, osseous integration is faster and more reliable than osteochondral allograft and has the advantage of transferring hyaline cartilage. Ideal candidates are young, healthy, and active individuals that have lesions that are less than 3cm2 in size.4
OAT has been reported to offer durable results with maintenance of clinical benefits at >10 years of follow-up.1 In a large systematic review, Jones et al.5 found that minimal clinically important difference (MCID) values for clinical scores were maintained for >10 years, demonstrating the durability of this surgical technique when patients are selected carefully.
Previous studies using OAT as mosaicplasty (multiple small plugs) had shown poorer outcomes with increasing age,6–8 with some authors emphasizing the importance of having an age limitation for the procedure (an upper limit of 50 years).9 However, controversial findings have also been reported by other authors who reported that clinical outcomes were independent of the age.10,11 Moreover, excellent and good results have been reported in studies in which patients older than 50 years of age were included.10–12
In recent years mosaicplasty had evolved, with current systems using larger plugs and thus limiting the number of plugs needed to be used in a single lesion. This advance was introduced to avoid complications when using multiple small plugs.
The objective of this study is to evaluate a cohort of patients that received an OAT as a single or double plug and to correlate their clinical results with the patients age when the procedure was performed.
Materials and methodsApproval was obtained from the institutional review board to collect and manage clinical scores and demographics in a prospective longitudinal database (REDCap; Vanderbilt University). Informed consent was obtained from all patients during pre-surgical medical evaluation. All patients were consented to participate in reporting outcomes to the database for potential future use in retrospective studies.
The database was queried to identify patients who had undergone an OAT (OATS, Arthrex, Naples, FL) in the knee by 2 senior surgeons between January 2015 and January 2020. Indications for OAT in our institution include patients that have a symptomatic OC lesion larger than 1cm2 and have failed conservative treatment, without any signs of knee osteoarthritis (Kellgren–Lawrence grade 0). The diagnosis of the injury was established through a knee magnetic resonance imaging (MRI) that revealed findings of an osteochondral lesion larger than 1cm2, with no imaging signs suggestive of knee osteoarthritis. Knee MRI was routinely conducted at our institution for all patients experiencing persistent symptoms after conservative management for three months. The protocol for conservative management prior to surgical intervention consisted of analgesic and anti-inflammatory treatment, along with physiotherapy over a period of 12 weeks. The postoperative protocol consisted of immediate unrestricted range of motion, complete weight bearing restriction for 2 weeks, followed by partial weight bearing (10–20% of the body weight) until the 6th week, after full weight bearing was initiated. Unrestricted physical activity was allowed after 4 months.
Surgical techniqueThe surgery was performed in a mini-open manner, with a lateral or medial parapatellar mini arthrotomy depending on the location of the lesion. The OATS system (Arthrex, Naples, FL) was used in all patients. The lesion was extracted down to the subchondral bone using the 10mm width device, making a cylinder of 15mm depth in all the cases. After harvesting the chondral lesion, the graft donor site was harvested. The medial or lateral paratrochlear groove was used as donor site depending on the location of the lesion. Once the grafts were in place, the range of motion was tested, checking the stability and fitting of the graft.
Eligibility and follow-upInclusion criteria were patients that underwent an OAT to treat a symptomatic OC lesion and had a minimum of 24 months follow-up and a neutral or corrected malalignment measured by long-length leg radiographs. Any patient with a follow-up shorter than 24 months was excluded. Patients with any sign of osteoarthritis or with osteochondral lesions larger than 2cm2 were also excluded. A chart review of electronic medical records was subsequently conducted to collect patient demographics and surgical variables for eligible participants. Eligible patients were categorized into two groups based on age at the time of surgery (<40 years old and ≥40 years old) based on previous studies in cartilage repair surgery.13,14
Postoperatively at final follow-up, each patient completed different clinical outcome scores, including the Knee injury and Osteoarthritis Outcome Score (KOOS), International Knee Documentation Committee (IKDC), and Lysholm clinical scales. Questionnaires were administered via a telephone interview. Any additional procedure in the knee was documented. Failure was defined as any procedure that removed or revised the OAT, including unicompartmental or total knee arthroplasty.
Statistical analysisStatistical analysis was done using Chi-square and Fisher's exact test to establish the comparison between groups regarding qualitative data. For quantitative data, Student's t and Pearson's correlation coefficient were used. A multivariate analysis was conducted for the scores, considering age, gender, number of plugs, concomitant procedures, and lesion size.
The prognostic capacity of age for the different scores was evaluated using the area under the receiver operating characteristic (ROC) curve. Statistical significance was established with a p<0.05 with a 95% confidence interval. The statistical program used was STATA version 17.0 (StataCorp, TX).
ResultsOut of fifty-six eligible patients, three patients were excluded due to presenting osteochondral lesions>2cm2, and two patients due to signs of knee osteoarthritis. Fifty-one patients met the inclusion and exclusion criteria (Table 1). Thirty-six were male patients and 15 were female patients. The mean follow-up was 4.2 years (2–7). The mean age of the cohort was 32.1 (14–51) years old. When divided into <40 years old (35 patients) and ≥40 years old (16 patients) the mean age was 26 (14–38) and 44 (40–51) years old respectively for each group. The mean size of the OC lesion was 1.2cm2 (1–1.7) without differences between groups (p=0.4). All lesions were located on the femoral condyles, 33 (64.7%) on the lateral femoral condyle and 18 (35.3%) on the medial femoral condyle. In 41 patients one plug was used, in 10 patients two plugs were used, there was no significant difference in the number of plugs used between groups (p=0.09). Thirty-two patients had additional procedures performed with no differences between groups (p=0.56) (Table 2).
Sample characteristics.
| <40 years (Mean±SD) | ≥40 years (Mean±SD) | p value | |
|---|---|---|---|
| Age at surgery (y) | 21.7±7.0 | 44.3±3.8 | 0.0001 |
| Follow-up (y) | 4.4±1.8 | 3.9±2.2 | 0.42 |
| Sex | |||
| Female, n (%) | 10 (28.6) | 5 (31.2) | |
| Male, n (%) | 25 (71.4) | 11 (68.8) | |
| Osteochondral characteristics | |||
| Defect area (cm2) | 1.3±0.7 | 1.2±0.5 | 0.4 |
Table 1 presents the demographic and osteochondral characteristics of the patients in this study. A significant difference in age was found between the groups of patients younger and older than 40 years (21.7±7.0 vs. 44.3±3.8 years, respectively; p=0.0001).
Additional procedures.
| Additional treatment | <40 years (n=35) | ≥40 years (n=16) | All cases (n=51) |
|---|---|---|---|
| Meniscal transplant | 5 | 1 | 6 |
| ACLR revision | 2 | 0 | 2 |
| Meniscectomy | 7 | 7 | 14 |
| ACLR revision+meniscectomy | 1 | 0 | 1 |
| Osteotomy | 1 | 0 | 1 |
| ACLR+meniscectomy | 2 | 1 | 3 |
| ACLR | 2 | 0 | 2 |
| Meniscectomy+meniscal repair | 1 | 0 | 1 |
| ACLR+meniscal repair | 1 | 1 | 2 |
| Total concomitant | 22 | 10 | 32 |
| Total isolated OAT | 12 | 6 | 19 |
Table 2 displays the additional procedures performed in patients categorized by age groups (<40 years and ≥40 years) in this study. In terms of additional procedures, the concomitant total was 32 cases, with 22 cases in the <40 years group and 10 cases in the ≥40 years group. Isolated osteochondral autograft transfer (OAT) procedures were performed in a total of 19 cases, with 12 cases in the <40 years group and 6 cases in the ≥40 years group.
Regarding clinical scores, the questionnaires were administered with a mean follow-up of 4.4 and 3.9 years for the <40 years and >40 years groups, respectively, without a significant difference between them (p=0.35). The mean IKDC was 77.8 (34–100), the mean Lysholm score was 83.1 (35–100), and the mean KOOS was 75.4 (38–94). For every year of age, the IKDC score decreased 0.7 points (p=0.004). The same was observed in Lysholm and KOOS scores decreasing 0.4 points (p=0.03) and 0.5 points (p=0.013) respectively. Apart from age, no other significant associations were found for score variation in the scales.
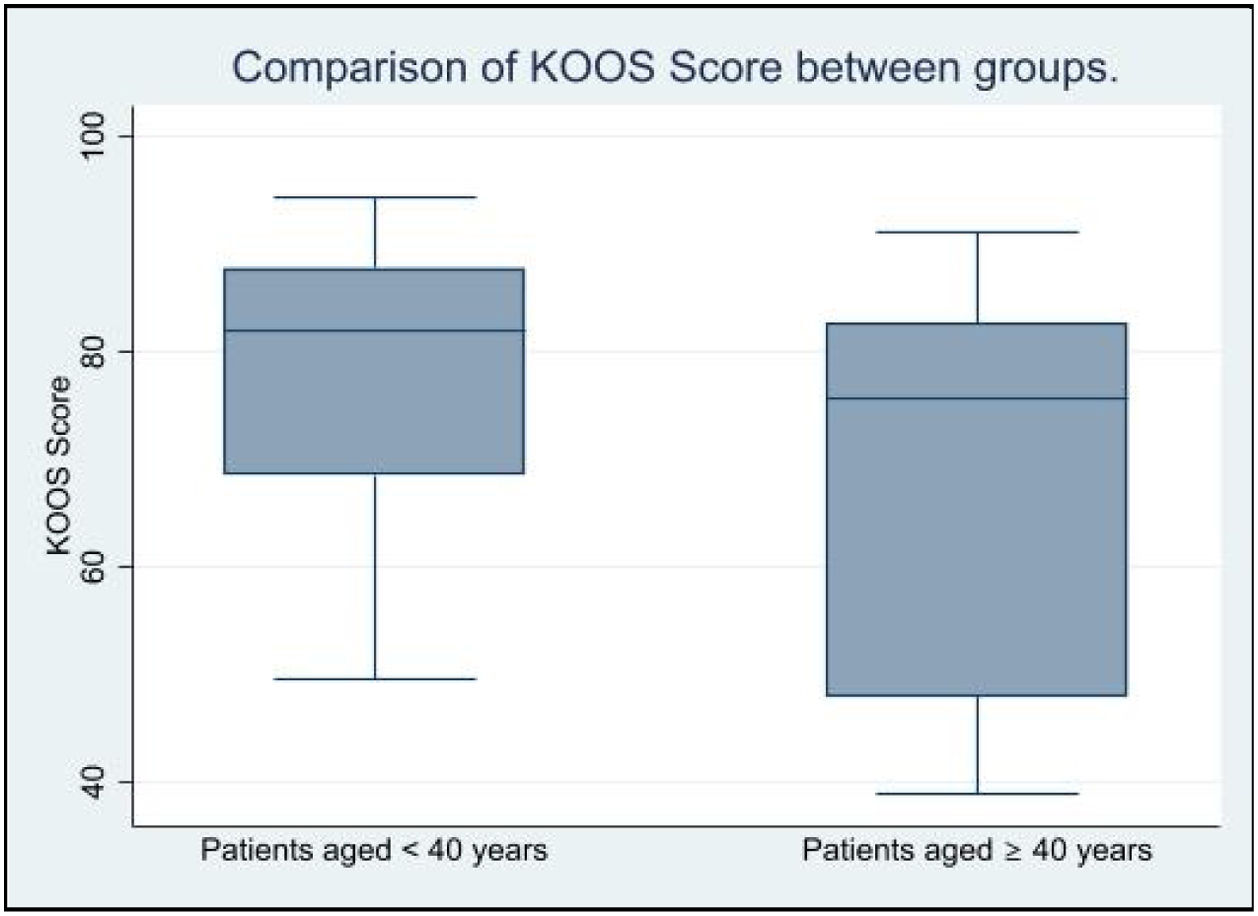
For patients <40 years old, the IKDC score averaged 80.8 points (SD 15.9) versus 71.2 points (SD 19.4) in ≥40 years old (p=0.03) (Fig. 1). For patients <40 years old, the Lysholm score averaged 85.9 points (SD 10.8) versus 77.0 points (SD 21.6) in ≥40 years old (p=0.02) (Fig. 2). For patients <40 years old, KOOS averaged 78.3 points (SD 11.8) versus 68.9 points (SD 18.5) in ≥40 years old (p=0.01) (Fig. 3). There were no failures in any group.
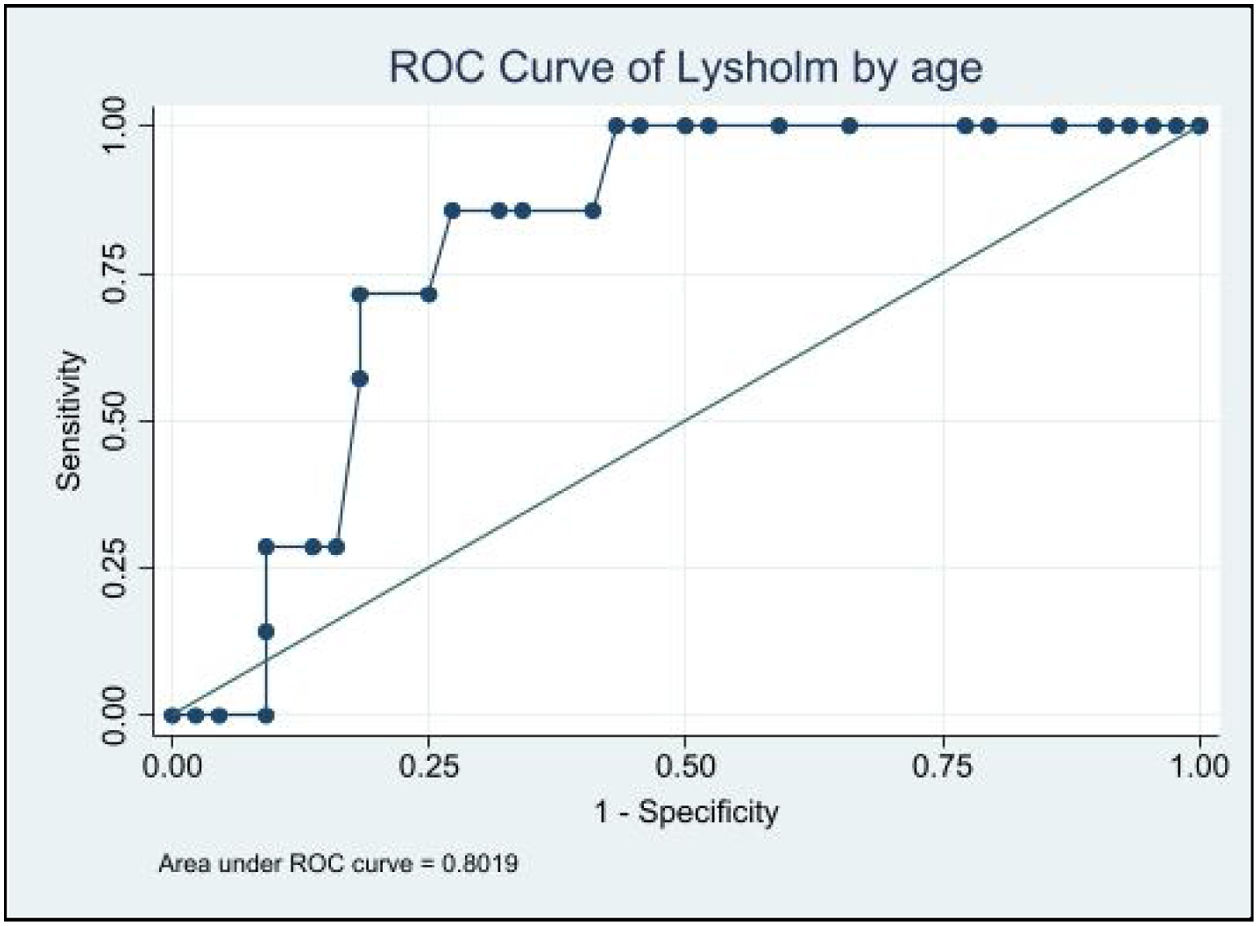
When analyzing the prognostic value of age for IKDC and Lysholm, there was a 100% sensibility to identify all the patients with a poor IKDC score (70 points or less) from 34 years old (AUC 0.76) (Fig. 4), a 100% sensibility to identify all the patients with a poor Lysholm score (65 points or less) from 34 years old (AUC 0.75) (Fig. 5), and a 100% sensibility to identify all the patients with a poor KOOS score (62.5 points or less) from 33 years old (AUC 0.8) (Fig. 6).
Age-stratified ROC analysis for IKDC scores in osteochondral autograft transplantation. This figure illustrates the receiver operating characteristic (ROC) curve for IKDC scores, providing a visual representation of its predictive capacity in the context of the study. The area under the curve (AUC) is calculated at 0.76, indicating a moderate to good discriminatory ability.
The principal findings of this study of single or double plug OAT in patients younger and older than 40 years old were as follows: (1) OAT has good outcomes in patients younger than 40 years old, and only fair outcomes in patients older than 40 years old; (2) clinical scores tend to decrease about half a point for each year older the patient is at the time of surgery; (3) There is a 75–80% probability in discrimination between good and poor results in the questionnaires using age, and 34 years is a cut-off point with excellent sensitivity and moderate specificity for each of the three questionnaires.
Upper age limit for mosaicplasty has been accepted as 50 years.15–17 Although there is little evidence-based proof for this limitation, it is known that both the bone and cartilaginous healing capacity decline with advanced age.18 Previous studies using mosaicplasty had shown poorer outcomes with increasing age.6–8 Emre et al.9 showed that age was a negative prognostic factor regarding Lysholm score in 152 patients that underwent a mosaicplasty procedure. Solheim et al.19 reported that patients over 40 years were more frequently affected by a poor result after a mosaicplasty procedure. Our results were consistent with this data, despite using a different system than mosaicplasty, with less plugs involved, where it could be thought that healing and thus clinical scores would be good regardless of the patient's age. From the data analyzed in our study, it can be concluded that the ideal indication for an OAT procedure is for the group of patients who are younger than 34 years old.
Chalal et al.20 in 2020 reported a MCID for Lysholm and IKDC scores after knee cartilage repair of 13 and 9.2 points respectively. Correlating this finding with our study, where a decrease of Lysholm and IKDC scores of 0.4 and 0.7 points per-year respectively was obtained, it would take 32.5 years to get a clinically significant reduction in Lysholm score and 13.1 years in IKDC score. That difference is mainly due to the nature of the Lysholm score, which encompasses simpler questions such as support, locking, and stair climbing, while the IKDC score addresses symptoms, sports activities, and functional performance.21 When studying younger patient populations, the primary outcomes are functional, primarily return-to sports. Unlike younger patients, however, those older than 40 years old are less likely to be engaged in organized sports for which return to play is a primary outcome, so pain reduction often represents a primary goal of intervention.13 That means that, despite the decreasing scores, OAT is still a good option for older patients with localized chondral lesions that failed with conservative treatment, at least to obtain reasonable pain management.
To date, the literature on outcomes after OAT not including the classic mosaicplasty technique in middle-aged patients is limited. Karmali et al.,22 in a study consisting of 13 patients (with 5 patients>40 years old) using OATS (Arthrex, Naples, FL), reported that there was no statistically significant correlation between age and IKDC scores. However, the study was probably underpowered because of the small numbers, as the mean improvement in IKDC scores from preoperatively to postoperatively was 50.0 in patients younger than 40 years old, while it was 30.5 in patients older than 40 years old, findings that are consistent with our study.
Contrarily to what was observed in our study, when the results of osteochondral allograft transplantation are analyzed, the results reported in patients over 40 years of age tend to be similar or even better than in young patients due to the lower demand and more strict indications in the older group.14,15,23 However, in spite of this, osteochondral allografts in our setting are used only for specific cases (chondral lesions larger than 2cm2) due to its high cost and low availability when compared to OAT.
The main limitation of this study is that even though OAT was performed to treat isolated OC lesions, 32 patients had additional procedures performed, which can confound the results. However, statistical analysis showed that there were no differences between groups regarding this issue. Other important limitations to consider include the fact that identifying age as a predictive factor in the success of autologous osteochondral transplantation may be considered a redundant finding, given the information already published in the literature. Regarding the questionnaires, these were administered by the researchers during the cohort follow-up, and although this is a common practice, it may introduce avoidable assessment biases if they had been administered by independent evaluators or as part of the natural follow-up of these patients. Additionally, owing to the retrospective nature of this study, we lacked access to preoperative questionnaires, rendering it unfeasible to ascertain a decline or improvement from baseline. Lastly, it is important to acknowledge that assessment scales are inherently subjective, and the absence of an anatomical verification through arthroscopy or MRI regarding the success of the procedure impacts the robustness of the clinical conclusions drawn.
OAT as a single or double plug has good outcomes in patients younger than 40 years old, and only fair outcomes in patients older than 40 years old; with clinical scores that tend to decrease about half a point for each year older the patient is at the time of surgery. Based on the prognostic capacity of age using the area under the ROC curve, the ideal candidate for an OAT procedure is a patient younger than 34 years old.
Level of evidenceLevel of evidence iii.
FundingThe authors report no involvement in the research by the sponsor that could have influenced the outcome of this work.
Conflicts of interestThe authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.