Scheuermann's disease is the most common cause of kyphosis in adolescence, and one of the most common causes of back pain in this age group. It is most commonly located in thoracic spine and is generally painless. Scheuermann's disease in the lumbar spine is less known and may go undetected in daily clinical practice. Blumenthal described this entity as atypical lumbar Scheuermann's disease. This form presents with Schmorl's hernias in one or two vertebral bodies, with narrowing of disc space and changes in the vertebral plates. It is more often painful and it can be confused with traumatic, infectious or tumour diseases. In most patients, a radiographic study is enough to establish the diagnosis and to differentiate both forms. Our series consists of six patients affected with the atypical form of lumbar Scheuermann's disease and diagnosed by us. All patients had a repeated history of back pain with associated Schmorl's hernias, and a very high increase in lateral diameter in radiographic views of the lumbar spine. Involvement of a single vertebral body was the most prevalent (50% of cases), and the 4th lumbar vertebra was the most commonly affected. All patients returned to normal activities after conservative treatment with temporary immobilization and NSAIDs during pain episodes.
La enfermedad de Scheuermann es el origen más común de cifosis de la columna dorsal en el adolescente. Es uno de los orígenes más comunes de la dorsalgia en este grupo de edad. Se trata de una enfermedad cuya localización más frecuente es la torácica, siendo generalmente indolora. La forma de enfermedad de Scheuermann en el raquis lumbar es menos conocida, pudiendo pasar desapercibida en la práctica clínica habitual. Esta entidad fue descrita por Blumenthal como enfermedad de Scheuermann lumbar atípica. La forma lumbar atípica consiste en la aparición de hernias de Schmorl en uno o 2 cuerpos vertebrales con estrechamiento del espacio interdiscal y cambios en los platillos vertebrales. Con mayor frecuencia es dolorosa, lo que puede ser confundida con afecciones traumáticas, infecciosas o tumorales. En la mayoría de los pacientes el estudio radiográfico es suficiente para establecer el diagnóstico y diferenciar ambas formas. Nuestra serie de 6 enfermos afectados de la forma atípica lumbar de la enfermedad de Scheuermann y diagnosticados por nosotros, presentaron una historia clínica de lumbalgias de repetición. Asociaban hernias de Schmorl y un aumento muy evidente del diámetro lateral en las proyecciones radiográficas de la columna lumbar. La afectación de un solo cuerpo vertebral fue la más predominante (50% de los casos) y la vértebra más comúnmente afectada fue la L4. Todos los pacientes se reincorporaron a sus actividades habituales tras ser tratados con medidas conservadoras de inmovilización temporal y antiinflamatorios durante los periodos de dolor.
Scheuermann's disease is the most common source of thoracic kyphosis in adolescents and one of the most common sources of back pain in this age group. The criteria for clinical and radiological diagnosis are established by the appearance of 3 or more vertebrae adjacent to the apex of the curve with wedging of 5° or more and without evidence of congenital, infectious or traumatic alterations.1–5 This type of thoracic kyphosis is greater than 45° Cobb and rigid. Its radiological characteristics include the existence of Schmorl nodes or hernias and irregularities in the endplates of the affected vertebrae. The most common location is thoracic, being generally painless unless there are severe deformities in the form of kyphosis.2,5,6
The manifestations of Scheuermann's disease in the lumbar spine are less well known. Blumenthal et al.7 described 2 forms of involvement depending on the radiographic manifestations: the classical form (CSD), similar to dorsal involvement as described above, and the so-called atypical lumbar form (ALSD). The atypical form consists in the appearance of Schmorl hernias in 1 or 2 vertebral bodies, with a narrowing of the intradiscal space and changes in the vertebral endplates. In this series, the classical form was usually asymptomatic, unlike the atypical form which was most often painful. In most patients, the radiographic study is sufficient to establish the diagnosis and differentiate both forms.8
We present a series of 6 patients affected with ALSD in order to report their symptoms and history since, if unknown, and due to the association with pain, they can often be confused with traumatic or infectious aetiologies and go undetected in everyday clinical practice.
Materials and methodsWe present the clinical features of patients diagnosed with this atypical form of involvement. Our series consisted of 6 patients, 4 males aged 30, 38, 39 and 42 years and 2 females aged 16 and 27 years. The professions of the males were of moderate physical intensity, including stock replenisher in a large supermarket, woodworker, policeman and baker, respectively, according to the previously specified ages. The professions of the females were student and fishmonger.
All patients presented lower back pain on numerous occasions prior to the establishment of the diagnosis. The mean time of onset of discomfort prior to diagnosis was 5 years. The mean follow-up time in the study was 6 years.
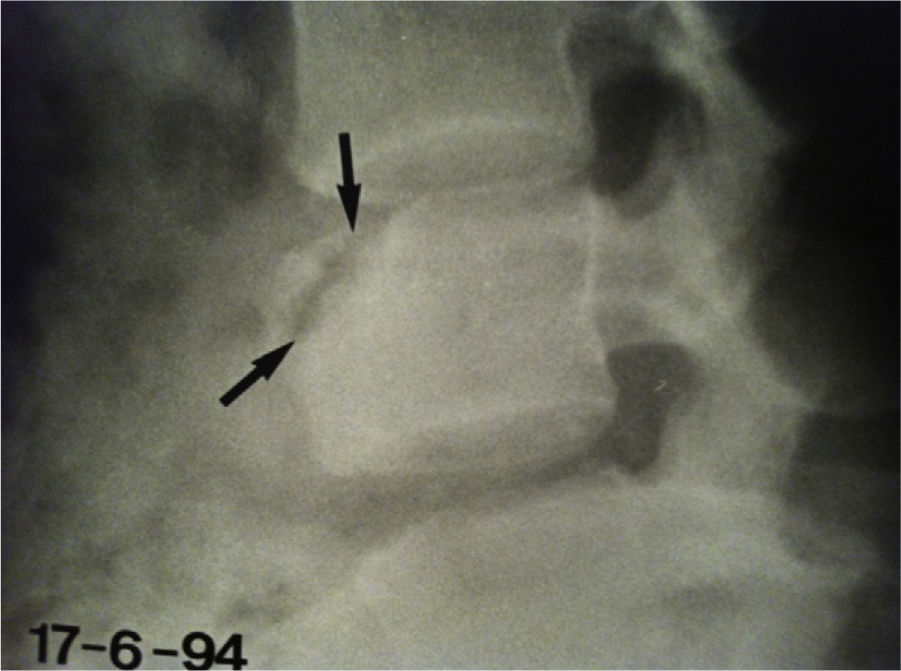
There was only 1 clear history of trauma, in the youngest female patient, relating to a bicycle crash 2 years earlier. In fact, this patient was sent to hospital with a diagnosis of pseudoarthrosis or nonunion of the L4 vertebral body (Fig. 1).
ResultsThere was a predominance of involvement of a single vertebral body, which in our series appeared in 50% of cases. In the remaining 3 cases, involvement was much more evident in 1 vertebral body, but there were Schmorl nodules in other vertebral bodies. None of the patients presented involvement of more than 2 lumbar vertebral bodies which, in addition, were always consecutive.
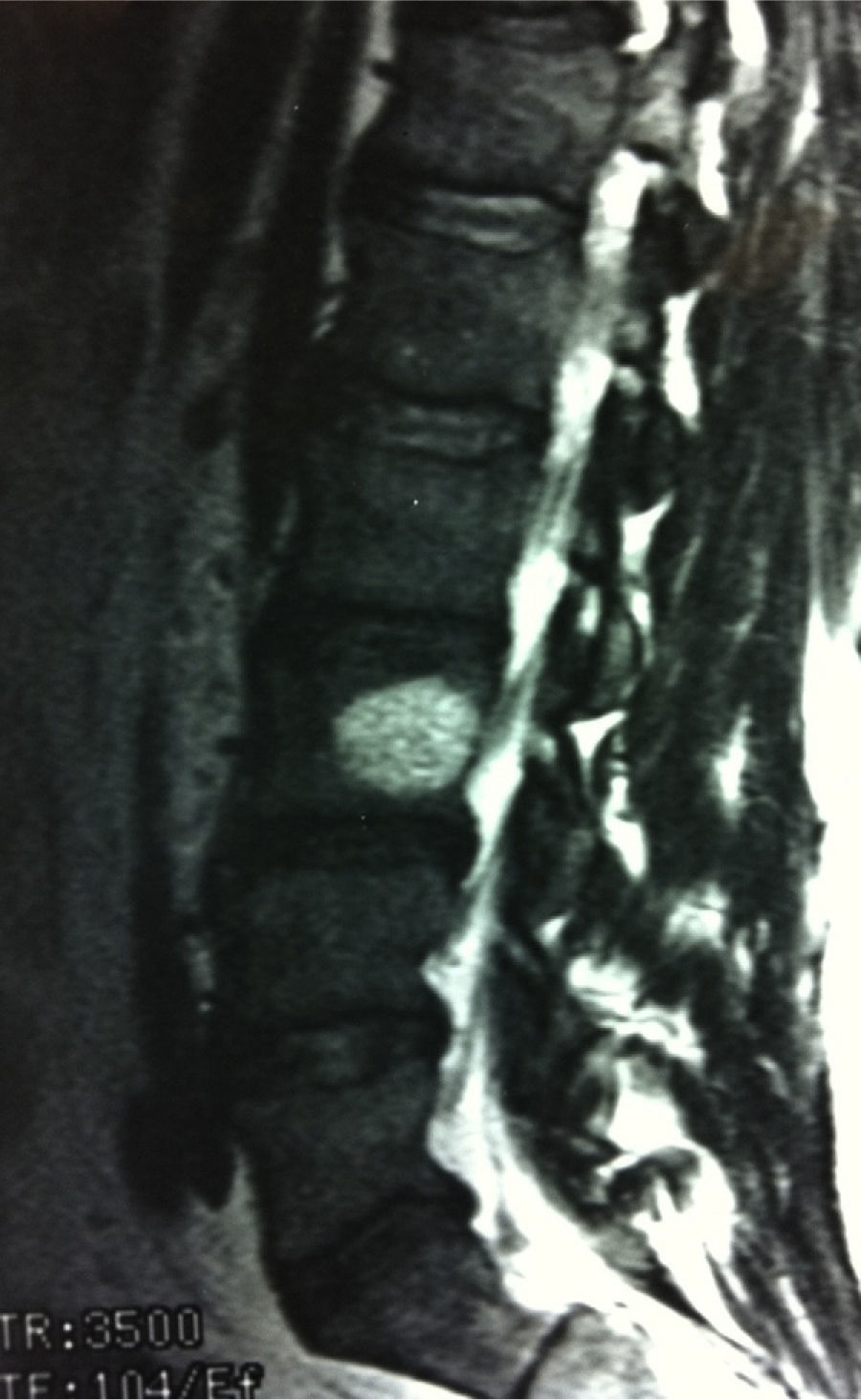
The radiographic study revealed Schmorl hernias in the patient with a previous history of trauma (Fig. 2). An increase of the lateral diameter was very evident in the vertebral radiographic projection (Knutsson vertebra, Fig. 3) in the other female patient who presented no detachment or solution of continuity in the upper vertebral vertex at the L5 level. Regarding the males, 1 of them suffered involvement of L5, 2 of them of L4 (Fig. 4), and the rest of L3 (Fig. 5). They also presented an increased lateral diameter compared to the remaining vertebrae, but this was much less evident than that reported in the female patient with L5 involvement.
The 2 older males showed signs of lumbar canal stenosis associated with the existence of short vertebral pedicles. The eldest patient also presented cervical canal stenosis secondary to spondylosis at the levels from C4 to C6.
There were also clear radiographic signs of dorsal Scheuermann's disease in 3 patients, who in turn presented the greatest narrowing of the intradiscal spaces at the lumbar level.
Regarding disc degeneration, there were images in the shape of vertebral limbus in the case of the patient with involvement of L5, in 2 patients with L4 condition (Fig. 4) and in 1 patient with L3 condition (Fig. 5). In the remaining 2 patients, the predominant condition was anterior disc degeneration at the level of L4 in 1 of them and of L5 in the other. There was 1 case with an evident case of Knutsson vertebra at the L5 level (Fig. 3).
All patients returned to their normal activities after receiving treatment with conservative measures including temporary immobilization with an orthesis and NSAIDs during periods of pain. However, following the monitoring period, there were episodic and recurrent periods of low back pain which were more or less common in 5 of the 6 patients in the series.
DiscussionScheuermann's disease affects between 0.4% and 8% of the population, depending on the series studied.2,5 It is important to note that there is no hyperuptake when performing a bone scintigraphy scan in the dorsal involvement form and in the typical lumbar form. On the other hand, this uptake is evident in the atypical form, thus increasing the possibility of diagnostic confusion with neoplasms or infections.2 The diagnosis of this form of lumbar involvement can be obtained through clinical and radiographic examination,8 thus avoiding a possible overtreatment in case the diagnosis is wrong. In fact, although pain crises are frequent, this condition responds well to conservative treatment, thus coinciding with the conclusions of Mandell et al.2 and Greene et al.9
Regarding the most commonly affected vertebrae, according to the series of 14 patients provided by Mandell et al.,2 these are L1 and L3. In our series there was greater involvement of L4 with 3 cases, followed by L5 in 2 cases and L3 in 1. The literature2,6 contains few cases of involvement at both levels with atypical and typical dorsal involvement (only 1 case in each of the series). In our series, there were 3 cases (50%) with involvement in the forms related to both levels.
According to Swischuk et al.,10 the form of disc degeneration may be central, anterior, posterior, in a vertebral limbus shape separating a part of the anterior epiphyseal ring and in the form of small, multiple extrusions.
Regarding the type of disc degeneration, there was anterior involvement in all patients, with 4 of them presenting a limbus shape. This situation was similar to the series described, as in that by Mandell et al.,2 in which there was only 1 form of posterior degeneration throughout the series. This form of lumbar vertebral involvement is often associated with scoliosis (46% in the series of Blumenthal et al.7).
Knutsson vertebra appears frequently in cases with dorsal involvement. Scoles et al.1 identified it in 94% of cases after conducting an anatomopathological study on 103 cadavers which had suffered Scheuermann's disease. Nevertheless, this deformity was not found in the cases suffering lumbar involvement (6 at that level). We observed 1 case (Fig. 3), which we believe was due to the fact that the herniated disc did not separate the superoanterior vertex from the vertebral body.
Regarding the aetiology, Greene et al.9 reported the possibility that excessive stress on an immature skeleton could break the discal material within the vertebral body. In the series of Blumenthal et al.7 trauma was present in 4 out of 7 cases, whilst McCall et al.11 provided a series of patients with intravertebral hernias following trauma. Swischuk et al.10 also reported that, although there were data associating Scheuermann's disease with traumatic epiphysitis, they believed in an aetiology due to disc degeneration, as claimed by Schmorl.12 Heithoff et al.13 found that 55% of patients with Scheuermann's disease presented images of disc alteration on magnetic resonance imaging scans, compared to a control group where these images only appeared in 10% of cases. These authors also suggested that the disease was due to an intrinsic defect of the disc or the vertebral epiphysis. The latter hypotheses would agree with our findings, where 50% of our cases also presented symptoms of lumbar spine condition, and could explain why only 1 patient throughout the series presented a clear history of trauma. However, it is also likely that a profession, through repetitive trauma or acute forms thereof, could be related to the onset of painful symptoms, although this may not condition the radiographic changes.14,15
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that this work does not reflect any patient data.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Lucas-García FJ, et al. Enfermedad de Scheuermann lumbar atípica: a propósito de 6 casos. Rev Esp Cir Ortop Traumatol. 2013;57:135-9.