We report a case with coexistence of an avulsion of the deep flexor muscle of the 5th finger of the hand with an enchondroma at the base of the third phalanx. This is a rare combination; we describe the treatment given and review the literature.
Se presenta un caso clínico donde coexisten un arrancamiento del flexor profundo del dedo meñique con un encondroma en la base de la tercera falange. Se trata de una combinación poco frecuente; se expone el tratamiento realizado y se revisa la bibliografía existente.
Enchondromas are the most frequent bone tumour, with their most unusual location being the distal phalanx; avulsion of the flexor muscle is relatively common in contact sports and mainly occurs in the ring finger. The joint presence of both pathologies is exceptional and there are only 6 cases described in the literature.
Case reportWe present the case of a male patient, 54 years old, without any pertinent medical history, who came to the clinic complaining of the inability to flex the distal interphalangeal joint of the 5th finger on the right hand, following a small traction mechanism with a door.
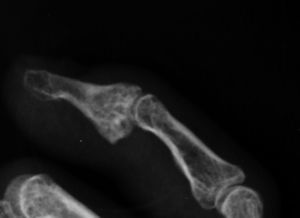
Radiology showed the presence of bone avulsion from the base of P3, together with an expansile osteolytic image in the same area, compatible with an enchondroma (Fig. 1).
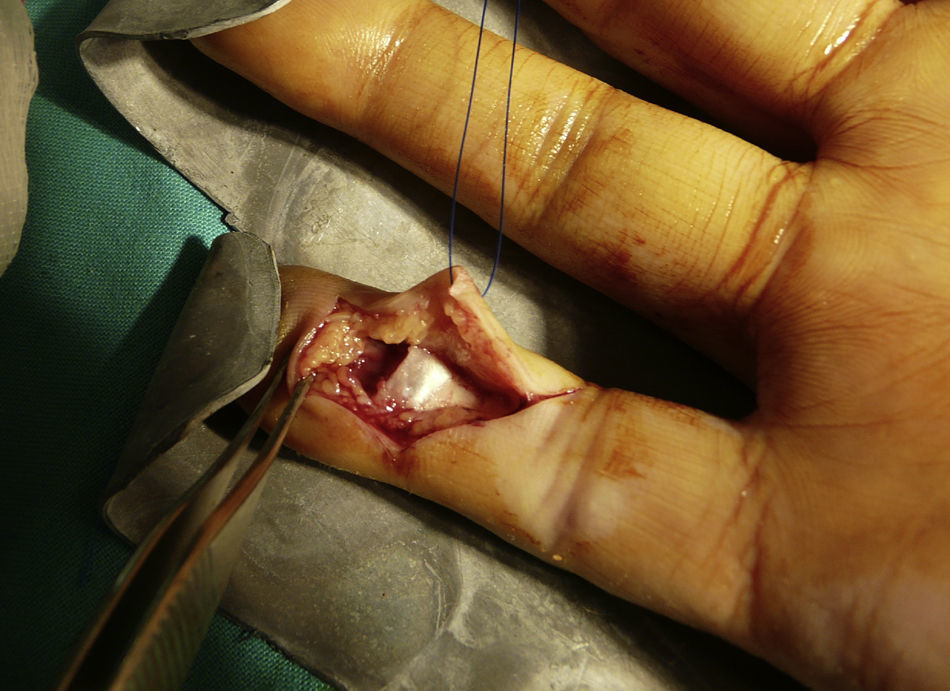
Four days after the lesion was incurred, it was surgically reviewed under locoregional anaesthesia by axillar block and preventive ischaemia at the root of the limb. A distal Bruner approach was used, revealing avulsion of the flexor, blockage at the A4 pulley, type III according to Leddy1 and a lytic lesion to the distal phalanx (Fig. 2); curettage of the lesion was performed and the tissue obtained was whitish and friable. The resulting cavity was filled by a bone graft taken dorsally from the distal radius, proximal to Lister's tubercle. The deep flexor tendon was reinserted with tendofil using the pull-out technique supported on the nail.
The finger was kept immobilized by a digitopalmar ferrule with flexion of the metacarpophalangeal joint and extension of the interphalangeal joints.
The pathology study described the presence of irregular fragments of cartilaginous tissue with abundant chondroid matrix and the existence of chondrocytes without cytological anomalies arranged in lagoons compatible with enchondroma.
After three weeks, immobilization was withdrawn and the patient was instructed to carry out passive and active flexion-extension movements. After 6 weeks, the tendofil was removed. After two months, he was advised to use a passive extension ferrule as he presented flexion of the proximal interphalanx.
Six months after the original lesion, the patient presents complete flexion of the finger with a 10° extension deficit in the distal interphalanx and 5° in the proximal one.
One year after surgery, mobility remains the same as after 6 months and radiologically there is no evidence of relapse in the lesion, signs of incipient arthropathy and with an increase in the thickness of the base of P3 due to calcification on the insertion of the flexor (Fig. 3).
DiscussionEnchondromas are the most frequent bone tumour lesion in the hand, mainly affecting the metacarpals and the proximal phalanges, while their presentation in the distal phalanx is much more infrequent. Clinical presentation varies from the presence solely of pain, pathological fracture or, relatively frequently, their chance identification in an X-ray.2
Avulsion of the deep flexor is frequent in certain sports such as American football or rugby, as it occurs while the finger is extended to grasp at the same time as there is a brusque contraction of the deep flexor.3
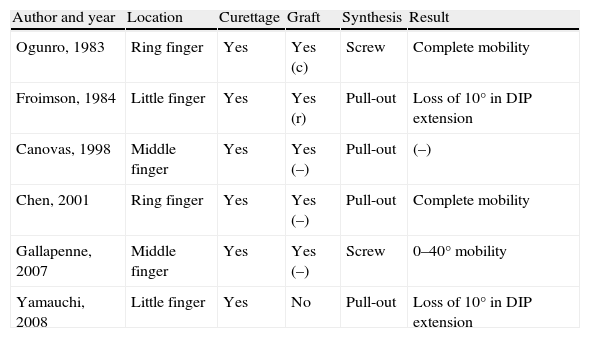
The association of both injuries is infrequent: we have been able to verify 6 prior cases in the literature4–9 and these are listed in Table 1 with the treatment applied. Enchondroma may be considered to be responsible for bone fragility that would make tendon avulsion easier, but is not the sole cause of the lesion as there are no case reports without prior trauma.
Case reports described in the literature.
| Author and year | Location | Curettage | Graft | Synthesis | Result |
| Ogunro, 1983 | Ring finger | Yes | Yes (c) | Screw | Complete mobility |
| Froimson, 1984 | Little finger | Yes | Yes (r) | Pull-out | Loss of 10° in DIP extension |
| Canovas, 1998 | Middle finger | Yes | Yes (–) | Pull-out | (–) |
| Chen, 2001 | Ring finger | Yes | Yes (–) | Pull-out | Complete mobility |
| Gallapenne, 2007 | Middle finger | Yes | Yes (–) | Screw | 0–40° mobility |
| Yamauchi, 2008 | Little finger | Yes | No | Pull-out | Loss of 10° in DIP extension |
c: iliac crest; r: distal radius; –: not known.
Involvement of the ring finger is the most frequent in cases of avulsion of the flexor profundus and is related to the presence of a common muscular belly for the middle, ring and little fingers and to the intertendinous connections of the extensors1; this does not occur when associated with an enchondroma. Of the 7 cases, two were in the middle fingers, two in the ring finger and three in the little finger. This may also be due to the fact that the muscle traction needed to provoke a lesion in the presence of an enchondroma is lower because of the existing bone fragility.
Treatment in all cases was bone re-insertion, with the synthesis varying depending on the size of the bone fragment avulsed; in only one case9 was no bone graft performed to fill the cavity following curettage of the enchondroma, probably due to the small size of the cavity. We consider that bone graft should be provided if the size of the cavity after the curettage is significant.
Level of evidenceLevel of evidence IV.
Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors will declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Please cite this article as: Méndez López JM, et al. Arrancamiento del flexor profundo a través de un encondroma: a propósito de un caso y revisión de la bibliografía. Rev esp cir ortop traumatol. 2011;55(5):389–391.