Ankle sprains are one of the most common injuries. Despite appropriate conservative treatment, approximately 20–40% of patients continue to have chronic ankle instability and pain. In 75–80% of cases there is an isolated rupture of the anterior talofibular ligament.
Material and methodA retrospective observational study was conducted on 21 patients surgically treated for chronic ankle instability by means of an arthroscopic anatomical repair, between May 2012 and January 2013.
There were 15 men and 6 women, with a mean age of 30.43 years (range 18–48). The mean follow-up was 29 months (range 25–33). All patients were treated by arthroscopic anatomical repair of anterior talofibular ligament.
Four (19%) patients were found to have varus hindfoot deformity. Associated injuries were present in 13 (62%) patients. There were 6 cases of osteochondral lesions, 3 cases of posterior ankle impingement syndrome, and 6 cases of peroneal pathology. All these injuries were surgically treated in the same surgical time.
ResultsA clinical-functional study was performed using the American Orthopaedic Foot and Ankle Society (AOFAS) score. The mean score before surgery was 66.12 (range 60–71), and after surgery it increased up to a mean of 96.95 (range 90–100). All patients were able to return to their previous sport activity within a mean of 21.5 weeks (range 17–28). Complications were found in 3 (14%) patients.
ConclusionsArthroscopic anatomical ligament repair technique has excellent clinical-functional results with a low percentage of complications, and enables patients to return to their previous sport activity within a short period of time.
Los esguinces de tobillo son una de las patologías traumatológicas más frecuentes. A pesar de un tratamiento conservador adecuado, este fracasa en el 20-40% de los casos. Estos pacientes suelen desarrollar una inestabilidad crónica de tobillo. En el 75-80% de las ocasiones existe una rotura aislada del ligamento talofibular anterior.
Material y métodoEstudio retrospectivo observacional de 21 pacientes intervenidos quirúrgicamente mediante técnica de reparación anatómica artroscópica, por inestabilidad lateral crónica de tobillo, entre mayo de 2012 y enero de 2013. Se realizó un seguimiento medio de 29 meses (rango de 25-33). La distribución por sexos fue de 15 hombres y 6 mujeres; la edad media fue de 30,43 años (rango de 18-48).
En 4 pacientes (19%), se diagnosticó una deformidad en varo del retropié asociada. En 15 pacientes (71,4%), se diagnosticaron lesiones intraarticulares: 6 pacientes presentaron lesiones osteocondrales (LOC) talares, 3 presentaban un pinzamiento posterior de tobillo y 6 pacientes presentaban distintas patologías de los tendones peroneos. Todas estas lesiones fueron abordadas quirúrgicamente en el mismo acto quirúrgico.
ResultadosSe llevó a cabo una revisión clínico-funcional, utilizando la escala American Orthopaedic Foot and Ankle Society (AOFAS). La media preoperatoria fue de 66,12 puntos (rango de 60-71) y la postoperatoria se incrementó hasta una media de 96,95 puntos (rango de 90-100). Todos los pacientes pudieron retomar sus actividades deportivas previas en una media de 21,5 semanas (rango de 17-28). Encontramos complicaciones en 3 pacientes (14%).
ConclusionesLa reparación anatómica del ligamento talofibular anterior mediante esta técnica presenta unos resultados clínico-funcionales excelentes, con una temprana reincorporación del paciente a sus actividades deportivas y un bajo índice de reintervenciones y complicaciones.
Sprained ankles are one of the most frequent musculo-skeletal pathologies, constituting more than 10% of daily traumatological emergencies.1 The most common mechanism of lesion is ankle inversion with the foot in plantar flexion. In this position, the anterior talofibular ligament talofibular anterior (ATFL) acts as the main stabiliser of the ankle. This ligament is the weakest in the lateral ligament complex.2 The initial treatment in the great majority of ankle sprains is conservative, with a high percentage of good results. This treatment should include a complete programme of rehabilitation, with proper proprioception exercises. In spite of this conservative treatment, there have been reports of failure in between 20% and 40% of the cases, which end up developing chronic ankle instability.3,4
Chronic lateral ankle instability can be linked to multiple pathologies, both intra-articular and extra-articular, as well as varus misalignment of the hindfoot.4–6 When conservative treatment of chronic ankle instability fails, surgical treatment is indicated. Numerous surgical techniques to approach this pathology have been described, with direct anatomical repair being the “gold standard”. This technique of open surgery was described by Broström in 19667; after that, modifications of this technique and techniques arthroscopic anatomical repair have been described.8,9 However, the success of such repair depends on the quality of the residual tissue. In patients with long-term ankle instability, with poor quality residual tissue, obesity or severe deformities associated, anatomical reconstruction with plasties might be indicated.10,11
Several techniques for arthroscopic repair of the ATFL, without associated percutaneous manoeuvres (all-inside), have recently been described. These techniques allow treating both the instability and the associated intra-articular lesions in the same operation.2,12–14
The objectives of this study were to assess the preliminary results of all-inside arthroscopic anatomical repair of the ATFL and to analyse the intra-articular lesions associated.
Material and methodStudy populationBetween May 2012 and January 2013, a total of 21 patients were surgically intervened for lateral chronic ankle instability in our centre. With respect to distribution by sex, 15 patients were male and 6 were female; mean age was 30.43 years (range: 18–48 years). Mean follow-up was 29 months (range: 25–33 months). All the patients were treated using the all-inside technique of arthroscopic anatomical repair, always by the same surgeon.
Criteria of inclusionAs criteria of inclusion in the study, to guarantee the viability of the tissue repaired, we included patients with a maximum of 3 ankle sprains, with the last of them being of fewer than 9 months of evolution. The mean number of episodes was 2.36 (range: 1–3 episodes), with a mean time since the last inversion trauma of 6.7 months (range: 3–9 months). Patients with obesity, recurrence over prior direct repair, severe associated deformities or neuromuscular diseases and high sport demand patients were excluded.15
Only patients that had complied with a minimum postoperative follow-up of 6 months, attending periodic revisions regularly, were studied. The revisions were established during the early postoperative period at 2, 4, 8 and 12 weeks and, after that, at 6 months and the first year postoperatively. All the patients studied had carried out a specific postoperative rehabilitation programme.
Clinically, all the patients had a history of previous ankle sprain as relevant trauma. They presented pain spontaneously and upon palpating the lateral side of the ankle. The patients reported sensations of instability and failure during their daily and/or sport activities. The physical examination revealed a varus deformity of the hindfoot in 4 patients. The manoeuvres for exploration of ankle instability, as well as the anterolateral translation test and the varus stress test, were positive in all the patients.16
As complementary tests, load X-rays were performed, including the Saltzman projection, as well as magnetic resonance imaging (MRI), in all the cases.17
The results were evaluated based on the American Orthopaedic Foot and Ankle Society (AOFAS) scale18 before surgery and at 18 months postoperative follow-up. This gave us the data for a functional-clinical study, analysing the results of the AOFAS scale and the moment of restarting prior sport activity.
Surgical techniqueIn all the cases, the surgical intervention was performed under intrathecal regional anaesthesia. As antibiotic prophylaxis, 2g of intravenous (i.v.) cephalosporin was administered; if the patient was allergic to the beta-lactams, we used 1g i.v. vancomycin.
As for the operation itself, the patient was placed in the supine position. Ischaemia of the limb was performed with a pressure cuff located at the root of the member. The limb affected was positioned with a flexion of the hip and knee of approximately 30° and a support under the proximal third of the leg, so that the ankle was parallel to the floor and free of supports and the operating table. This was done to enable all the plantar and dorsal flexion movements that would be needed during the surgery (Fig. 1).
The ankle arthroscopy was carried out using the classic anteromedial and anterolateral portals. No accessory portals were needed in any of the cases. The associated lesions, such as the peroneal tendons, posterior ankle pinching syndrome or osteochondral lesions (OCL), were surgically treated during the same surgical intervention.
The cases of varus misalignment of the hindfoot were also treated in the same surgical intervention, associating an osteotomy of lateral calcaneus sliding, before the arthroscopy was performed.
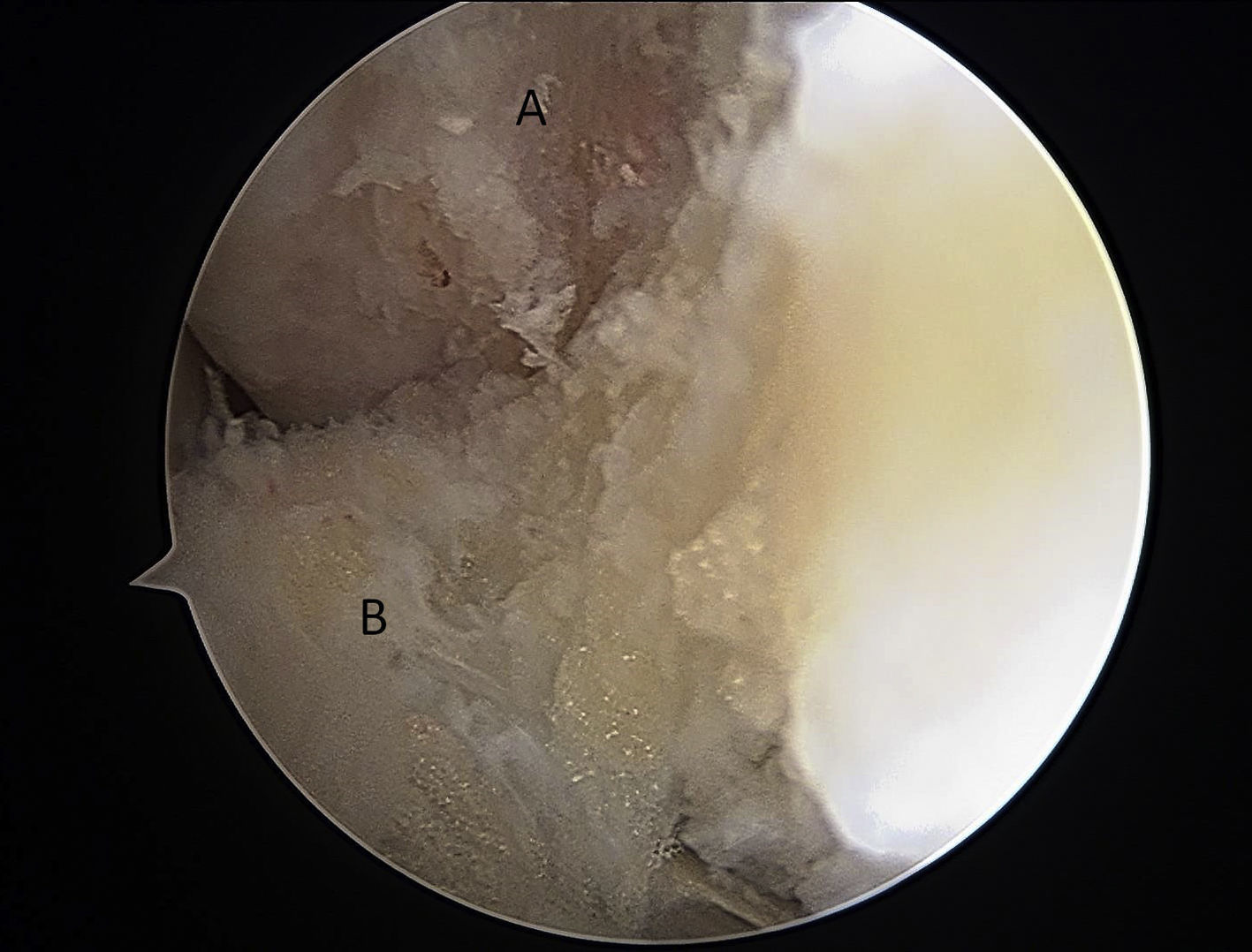
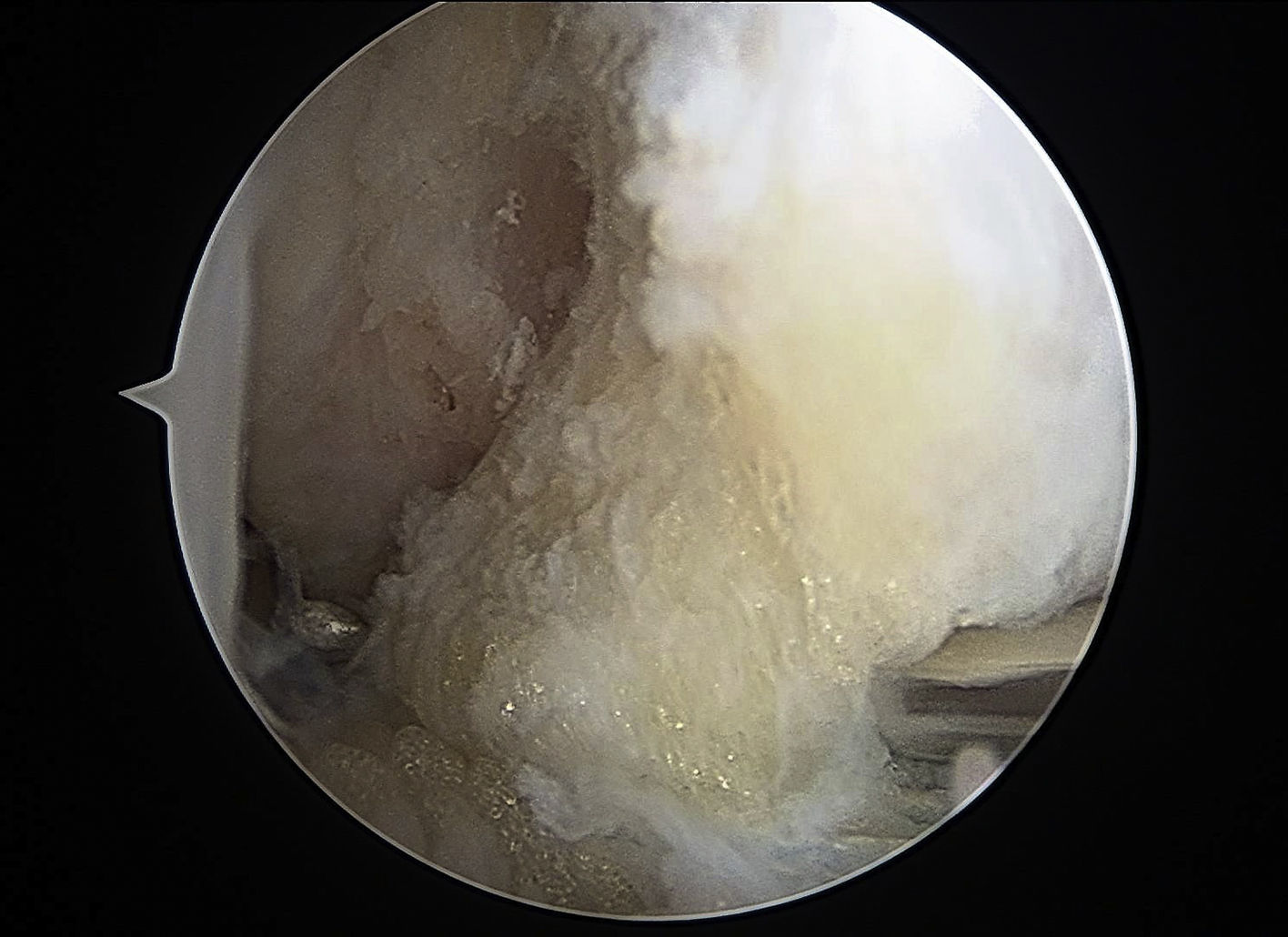
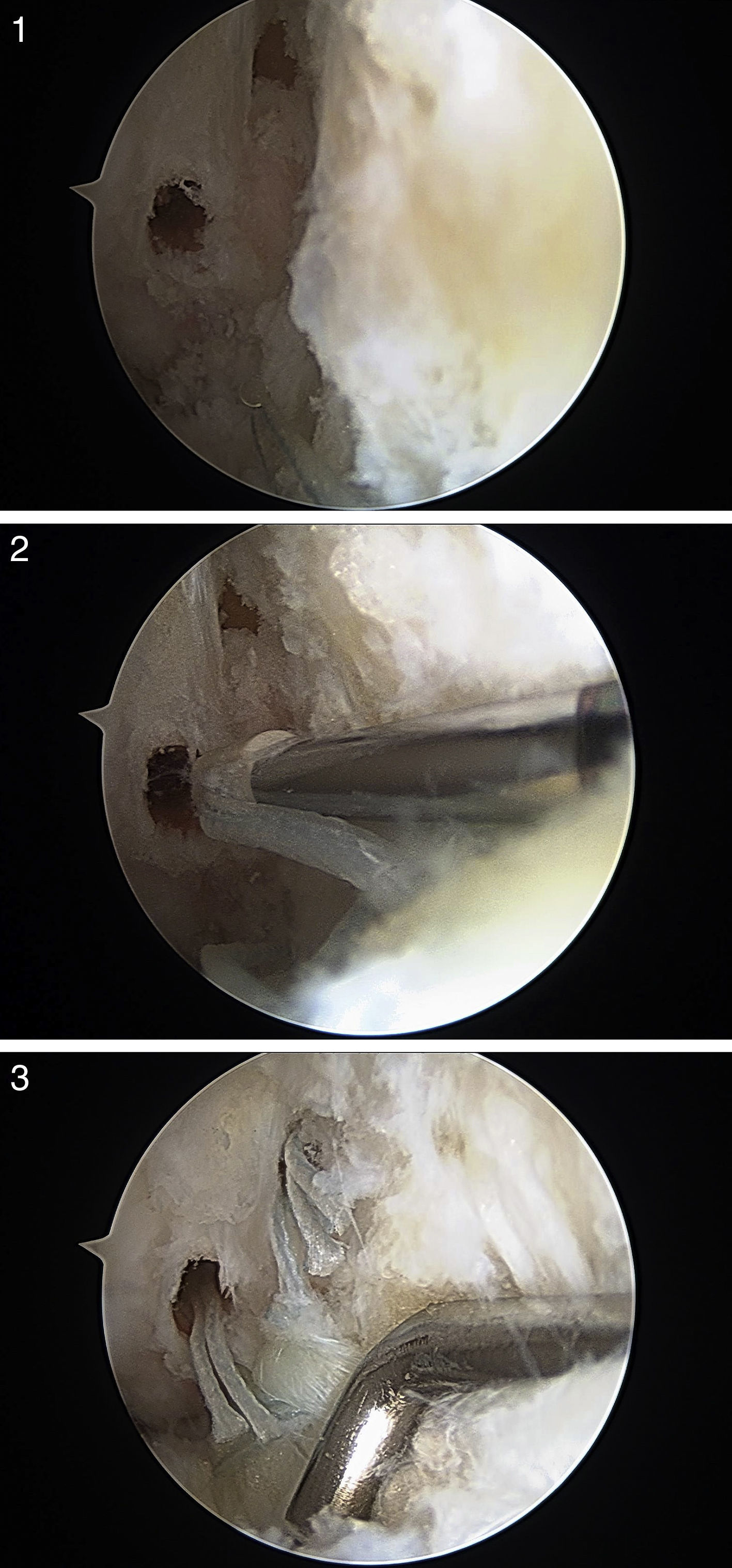
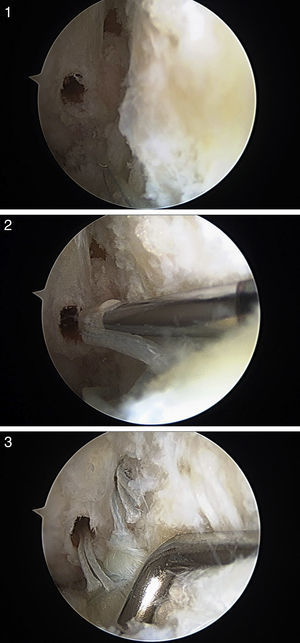
The anterior chamber was arthroscopically explored completely, with treatment of the associated lesions. The ATFL was then repaired under direct vision. The first step was the insertion of the ATFL in the fibula; to do so, the bony landmark was debrided through the anterolateral portal (Fig. 2). The remainder of the ATFL was pierced, from lateral to medial, with a Micro SutureLasso (Arthrex, Naples, FL, USA) (Fig. 3). The fiberwire was passed and, through it, a double 2/0 high-resistance suture. All these surgical steps were carried out through the anterolateral portal, with the optics located in the anteromedial portal. The same manoeuvre was then repeated with a second suture point proximal to the previous one. In that way, the surgeon could pull on the rest of the ligament to ascertain the quality of the tissue to be repaired. The drill guide was then inserted through the anterolateral portal and placed in the bony landmark of the ATFL, just distal to the insertion of the distal anterior inferior tibiofibular ligament (DAITFL). The 2.0-mm drill was directed from anterior to posterior, parallel to the plantar plane and to the lateral aspect. Next, the 2 holes were drilled, vertically in the bony landmark (Fig. 4A). After that, the most distal suture point was passed through a 2.5-mm knotless Bio-PushLock anchor (Arthrex, Naples, FL, USA) and introduced in the first hole (Fig. 4B). During the implantation of the Bio-PushLock anchor, it was important to maintain a fixed foot position, in a slight dorsal flexion of 5° and eversion of 5°–10°. The same process was repeated with the second suture point (the most proximal). We prefer to use 2 implants because they permit greater surface contact of the ATFL with the fibular bony landmark, as well as better distribution of the tensions, from a biomechanical point of view (Fig. 4C).
(1) Drilling of two openings, located vertically in the bony landmark; (2) the most distal suture point is passed through a 2.5-mm Biopush Lock knotless anchor (Arthrex, Naples, FL, USA) and inserted into the first hole; (3) 2 implants are used, because they allow a greater surface contact of the ATFL with the fibular bony landmark, as well as better tension distribution, from the biomechanical point of view.
Following proper postoperative protocol was important. Following the intervention, the ankle had to be immobilised with an orthopaedic splint, having the ankle in neutral position (90°) and slight eversion (10°), for 3 weeks. After that, it was replaced with a Walker-type orthosis (DonJoy, Surrey, UK). From 1 month postoperative, the patient began with progressive partial load, using 2 crutches based on tolerance, and the patient started a rehabilitation programme. If treatment of OCL was required, the patient remained off the foot for a period of 4–6 weeks. The patients who underwent calcaneus osteotomy received the same postoperative protocols indicated previously.
From 8 weeks postoperative, the patients began to carry out specific sport activities that did not involve physical contact (swimming and static or elliptical cycling), beginning continuous running at 10–12 weeks. The patients could commence their usual sport activities again in a progressive and controlled manner after some 4 and 6 months.
ResultsA total of 21 patients with chronic ankle instability were surgically treated in our hospital, with arthroscopic anatomical repair of the ATFL being performed in all of the cases.
In 4 patients (19%), physical examination yielded the diagnosis of a varus deformity of the hindfoot associated with lateral ankle instability. This deformity was treated in the same intervention, carrying out an inverse Koutsogiannis osteotomy.19
As for the X-ray results, the various projections used confirmed varus misalignment of the hindfoot in 4 patients and diagnosed posterior impingement of the joint in 3 patients.
An ATFL lesion was the conclusion in 100% of the MRI reports. With respect to the associated lesions found, the results were as follows:
- -
In 6 cases (28.57%), there was an OCL associated, which was later confirmed at the time of the associated OCL arthroscopy in all of them.
- -
In 3 cases (9.52%), there was a posterior impingement of the joint, which was confirmed with the arthroscopy.
- -
The finding most often associated with ATFL rupture in the MRI was the partial rupture of the peroneus brevis tendon, found in 9 patients (42.86%). However, in the intervention, it was seen that in 6 of the patients there was no type of associated pathology. In 1 case, the only associated finding was a posterior ankle impingement (also seen in the MRI); in 2 patients, peroneal tendon lesions were indeed found: 1 case of intrasheath luxation and 1 case of partial rupture of the peroneus brevis tendon.
- -
Lastly, in 4 patients (19.04%), the MRI revealed the ATFL lesion associated with a complete rupture of the peroneus brevis tendon. In those cases, there was no good correlation with the intraoperative findings either. During the intervention, 2 cases of partial peroneus brevis tendon, 1 case of intrasheath luxation and 1 case of isolated tenosynovitis were found.
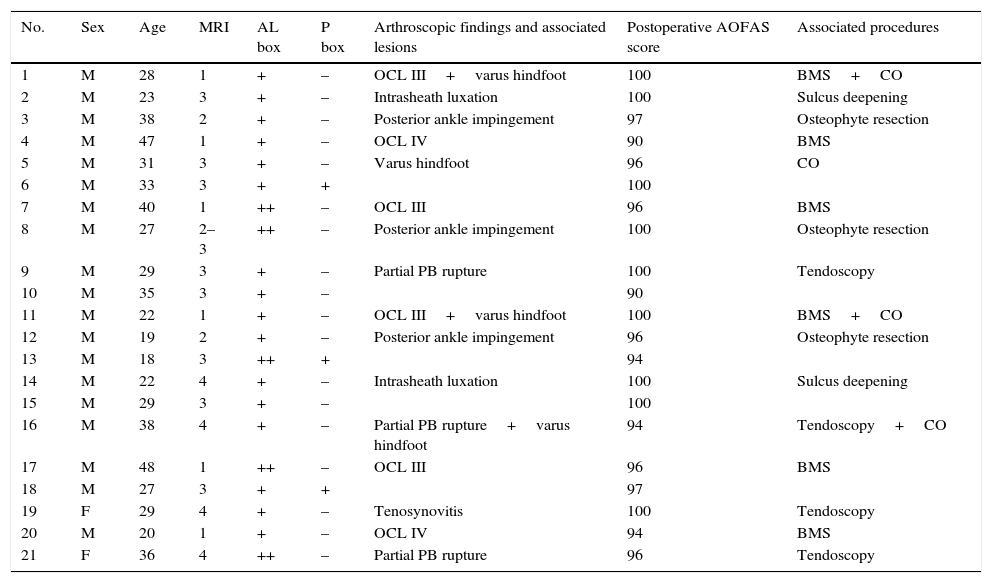
As for the intraoperative results, intra-articular lesions were diagnosed in 15 patients (71.4%). A total of 6 patients presented OCL, posterior impingement of the ankle was found in 3 patients and, in 6 patients, some type of pathology of the peroneal tendons was found. All of these lesions were surgically approached in the same surgical intervention (Table 1).4
Description of the population studied.
| No. | Sex | Age | MRI | AL box | P box | Arthroscopic findings and associated lesions | Postoperative AOFAS score | Associated procedures |
|---|---|---|---|---|---|---|---|---|
| 1 | M | 28 | 1 | + | – | OCL III+varus hindfoot | 100 | BMS+CO |
| 2 | M | 23 | 3 | + | – | Intrasheath luxation | 100 | Sulcus deepening |
| 3 | M | 38 | 2 | + | – | Posterior ankle impingement | 97 | Osteophyte resection |
| 4 | M | 47 | 1 | + | – | OCL IV | 90 | BMS |
| 5 | M | 31 | 3 | + | – | Varus hindfoot | 96 | CO |
| 6 | M | 33 | 3 | + | + | 100 | ||
| 7 | M | 40 | 1 | ++ | – | OCL III | 96 | BMS |
| 8 | M | 27 | 2–3 | ++ | – | Posterior ankle impingement | 100 | Osteophyte resection |
| 9 | M | 29 | 3 | + | – | Partial PB rupture | 100 | Tendoscopy |
| 10 | M | 35 | 3 | + | – | 90 | ||
| 11 | M | 22 | 1 | + | – | OCL III+varus hindfoot | 100 | BMS+CO |
| 12 | M | 19 | 2 | + | – | Posterior ankle impingement | 96 | Osteophyte resection |
| 13 | M | 18 | 3 | ++ | + | 94 | ||
| 14 | M | 22 | 4 | + | – | Intrasheath luxation | 100 | Sulcus deepening |
| 15 | M | 29 | 3 | + | – | 100 | ||
| 16 | M | 38 | 4 | + | – | Partial PB rupture+varus hindfoot | 94 | Tendoscopy+CO |
| 17 | M | 48 | 1 | ++ | – | OCL III | 96 | BMS |
| 18 | M | 27 | 3 | + | + | 97 | ||
| 19 | F | 29 | 4 | + | – | Tenosynovitis | 100 | Tendoscopy |
| 20 | M | 20 | 1 | + | – | OCL IV | 94 | BMS |
| 21 | F | 36 | 4 | ++ | – | Partial PB rupture | 96 | Tendoscopy |
AL: anterolateral; AOFAS: American Orthopaedic Foot and Ankle Society; ATFL: anterior talofibular ligament; BMS: bone marrow stimulation techniques; CO: calcaneal osteotomy; F: female; M: male; MRI 1: ATFL lesion+OCL; MRI 2: ATFL lesion+posterior articular impingement; MRI 3: ATFL lesion+partial PB rupture; MRI 4: ATFL lesion+complete PB rupture; OCL: osteochondral lesions; P: posterior; PB: peroneus brevis tendon.
Of the 6 cases with OCL (28.5%), 4 cases were grade IIIB and 2 cases were grade IV of the International Cartilage Repair Society (ICRS)20 classification. All the cases were treated with bone marrow stimulation techniques, which consisted of debridement of the lesion and microperforations.
The 3 cases with posterior ankle impingement (14.2%) were treated by osteophyte resection, by means of the posterior endoscopic portals described by Van Dijk.21 In these cases, it was necessary to reposition the patient in the prone position.
The 6 patients with pathology of the peroneal tendons (26.5%) required tendoscopic surgery: in 1 case, the finding was isolated tenosynovitis; in 3 cases, partial rupture of the peroneus brevis tendon was found and 2 cases presented intrasheath luxation. The 4 cases with tenosynovitis and partial ruptures were treated using tendoscopic synovectomy, while the 2 patients with intrasheath luxation required tendoscopic deepening of the peroneal sulcus.22
A functional-clinical review was carried out, using the AOFAS scale. The mean preoperative AOFAS was 66.12 points (range: 60–71), while the postoperative AOFAS increased to a mean of 96.95 points (range: 90–100). All of the patients could take up their previous sport activities again in a mean of 21.5 weeks (range: 17–28).
We found complications in 3 patients (14%). The first patient presented joint rigidity, which required arthroscopic debridement and immediate rehabilitation; the final result was good. Another patient presented infection of the arthroscopic portals, with superficial cellulitis; this patient was treated with oral antibiotics and evolved satisfactorily. Lastly, there was 1 case of neuropathy of the superficial peroneal nerve, which also evolved favourably, without any current symptoms.
DiscussionSprained ankles are the most frequent cause of injury to the lateral ankle ligament complex. In the majority of the cases, they are treated as a banal pathology. However, the percentage of patients that develop chronic ankle instability after this injury ranges between 20% and 40%.3,4
With these patients, it is essential to take an appropriate clinical history and physical examination. The physical exam should focus on ruling out factors predisposing for chronic ankle instability, such as the coexistence of varus hindfoot or fixed plantar flexion of the first metatarsal. These deformities should be treated surgically, during the same operation, given that they are the fundamental reason for failure of surgical treatment of chronic ankle instability.23 Likewise, complementary imaging tests should be performed. These are very useful for ruling out associated intra-articular pathologies, such as OCL, fractures, peroneal tendon pathology and joint impingements.
Kim et al.24 analysed the validity of MRI images in the diagnosis of ATFL lesions and the relationship with arthroscopic findings. As indicated in their article, they conclude MRI sensitivity and positive predictive value for the diagnosis of ATFL lesions are very high. In our study, there is also excellent correlation between the MRI reports and the arthroscopic findings, with respect to the diagnosis of ATFL lesions; the ATFL lesion was reported in 100% of the cases.
However, we have not found any studies published that specifically analyse the correlation of radiological and arthroscopic findings with respect to associated lesions. Small size lesions are difficult to diagnose using MRI; this is the reason why many authors recommend that arthroscopic examination of the ankle should routinely be performed before treatment of chronic ankle instability.25,26
Lee et al.4 studied the associated intra-articular lesions in patients with chronic ankle instability. They found 100% anterolateral synovitis, 30% superficial lesions of the talus cartilage with 7% of OCL, 14% anterolateral articular impingement, 14% with anterior osteophyte in the distal tibia and 11% with presence of free joint bodies. Hintermann et al.25 described damage to the joint cartilage in up to 66% of the cases and Ferkel and Chams26 found intra-articular lesions even in 95%. These finding agree with those of our series, in which we found associated lesions in up to 71% of the cases.
Arthroscopic ankle surgery is currently a technique in constant evolution. Arthroscopic treatment of patients with chronic ankle instability makes diagnosis and treatment of all these associated intra-articular pathologies possible. Hawkins27 was the first to describe, in 1987, ankle arthroscopy as a possible treatment for chronic ankle instability. More recently, other authors have described different arthroscopic techniques for this pathology, with excellent results.2,13,14
The first surgical technique, described by Hawkins,27 used staples to re-anchor the ATFL. Since then, the evolution up to the most modern surgical techniques has been constant. In 2013, Cottom and Rigby13 described an arthroscopic technique using osseous spears implanted in the ATFL landmark and a mini-open, needed to introduce the suture knots. Vega et al.2 described their arthroscopic technique, using implants without knots, but with the need for a complementary portal in the most anterior part of the peroneal malleolus. Our technique allows arthroscopic ATFL repair using implants without knots and without the need to make complementary portals. Consequently, we avoid the complications that stem from prominence of the suture knots.
Other complications described in the arthroscopic techniques are neuritis of the superficial peroneal nerve and of the sural nerve.28 It is a good idea to mark the subcutaneous path of the superficial peroneal nerve before beginning the ankle arthroscopy. In addition, it should be taken into account that this nerve can move laterally with ankle dorsiflexion; when a position in plantar flexion and inversion is changed to one in 5° dorsiflexion, the nerve will displace laterally up to a mean of 3.6mm. Damage to the sural nerve is much lower with all-inside arthroscopic techniques, given that no cutaneous incisions are required.
It is important to emphasise that this technique is aimed at isolated ATFL repair, without involving any possible lesions of the calcaneofibular ligament (CFL), which may be injured in up to 15% of the cases. In 2011, Lee et al.4 published a study on the long-term results (10.6 years of mean follow-up) of the modified Broström technique, with no associated procedure in the CFL. They obtained a mean AOFAS score of 91 points and observed integrity of the repaired ATFL, with slight anterior translation (6.9mm against 6.1mm in the contralateral). The measurements of CFL function were also satisfactory, with a 3° talar tilt in the ankle treated, against 2.5° in the contralateral.
As possible limitations of our study, we should point out the relatively small number of cases studied, as well as the retrospective nature, with the lack of a control group. Another limitation of the study is that the preoperative ankle instability is not quantified, accepting the clinical diagnosis with radiographic support. This is a common limitation for the majority of the studies on chronic ankle instability. Prospective, comparative and randomised studies will be needed to be able to state that arthroscopic surgery is superior to open surgery.
ConclusionsArthroscopic surgery is fundamental in confirming the existence of intra-articular lesions associated with chronic ankle instability and is essential if treatment for such lesions is necessary. Among its advantages over open surgery worth pointing out are its lower aggressiveness, less associated morbidity and its better aesthetic results. Sin embargo, its superiority over open surgery is yet to be demonstrated.
Anatomical repair by means of the all-inside technique presents excellent functional-clinical results, with early patient reincorporation to sport activities and a low index of reinterventions and complications.
Level of evidenceIV.
Ethical disclosuresProtection of people and animalsThe authors declare that no experiments on human beings or on animals have been performed for this research.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: Arroyo-Hernández M, Mellado-Romero M, Páramo-Díaz P, García-Lamas L, Vilà-Rico J. Inestabilidad crónica de tobillo: reparación anatómica artroscópica. Rev Esp Cir Ortop Traumatol. 2017;61:104–110.