To analyse the results of arthroscopic repair of acromioclavicular dislocation in terms of health-related quality of life.
Material and methodProspective study of patients with acromioclavicular dislocation Rockwood grade iii–v, treated arthroscopically with a mean follow up of 25.4 months. The demographics of the series were recorded and evaluations were performed preoperatively, at 3 months and 2 years with validated questionnaires as Short Form-36 Health Survey (SF-36), visual analogue scale (VAS), The Disabilities of the Arm, Shoulder and Hand (DASH), Constant–Murley Shoulder Outcome Score (Constant) and Walch–Duplay Score (WD).
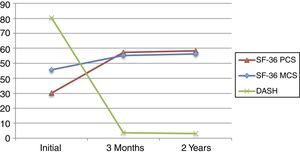
ResultsTwenty patients, 17 men and 3 women with a mean age of 36.1 years, were analysed. According to the classification of Rockwood, 3 patients were grade iii, 3 grade iv and 14 grade v. Functional and clinical improvement was detected in all clinical tests (SF-36, VAS and DASH) at 3 months and 2 years follow up (P<.001). The final Constant score was 95.3±2.4 and the WD was 1.8±.62. It was not found that the health-related quality of life was affected by any variable studied except the evolution of DASH.
ConclusionsThe health-related quality of life (assessed by SF-36) in patients undergoing arthroscopic repair of acromioclavicular joint dislocation grades iii–v was not influenced by gender, age, grade, displacement, handedness, evolution of the VAS, scoring of the Constant or by the WD. However, it is correlated with the evolution in the DASH score.
Analizar los resultados de la reparación artroscópica de la luxación acromioclavicular en términos de calidad de vida percibida.
Material y métodoEstudio prospectivo de pacientes con luxación acromioclavicular grados iii-vde Rockwood, tratados artroscópicamente con un seguimiento medio de 25,4 meses. Se registraron los datos demográficos de la serie y se realizaron evaluaciones antes de la cirugía, a los 3 meses y a los 2 años con los cuestionarios validados Short Form-36 Health Survey (SF-36), escala visual analógica (EVA), The Disabilities of the Arm, Shoulder and Hand (DASH), Constant–Murley Shoulder Outcome Score (Constant) y Walch–Duplay Score (WD).
ResultadosSe analizaron 20 pacientes, 17 hombres y 3 mujeres, con una edad media de 36,1 años. Según la clasificación de Rockwood, 3 pacientes fueron grado iii, 3 grado iv y 14 grado v. Se objetivó mejoría tanto funcional como clínica en todos los test clínicos analizados (SF-36, EVA y DASH) tanto a los 3 meses como a los 2 años (p<0,001). El valour final del test de Constant fue de 95,3±2,4 y el WD medio fue de 1,8±0,62. No se encontró que la calidad de vida percibida se viera afectada por ninguna variable a estudio, excepto por la evolución del DASH.
ConclusionesLa calidad de vida percibida (valorada mediante el SF-36) en pacientes intervenidos artroscópicamente de luxación acromioclavicular grados iii-v no se ve influida por el sexo, la edad, el grado, el desplazamiento, la lateralidad, la evolución de la EVA, la puntuación del Constant ni por el WD. Sí se correlaciona con la evolución en el DASH.
Acromioclavicular joint dislocations (AC), which are classified by Rockwood1 in degrees i to vi, are a challenge for orthopaedic surgeons as they are difficult to treat and there is no consensus on which one of the many techniques described should be used.2 This lack of agreements centres especially on degrees iii–v.
Arthroscopic procedures that use coracoclavicular suspension devices (CC) placed isometrically or anatomically make it possible to reduce AC dislocations during the scarring of the CC ligaments.3–6 The anatomical technique places 2 CC suspension devices, emulating the trajectory of the conoid and trapezoid ligaments, while the isometric technique places a single device centrally, between the conoid and trapezoid ligaments.3–6 These procedures make it possible to reduce AC dislocations during the hypothetical scarring of the CC ligaments.
Injuries to the AC joint are important for perceived quality of life (PQL) for the patient. These dislocations represent approximately 10% of injuries to young active patients.1 The clinical results described to date (using arthroscopic techniques) describe a favourable clinical and functional recovery, although there is up to 40% residual displacement which may or may not affect the subsequent clinical symptoms of the patient.7
There are many functional measurement instruments for evaluation following AC dislocations. In spite of this, such instruments do not seem able to determine overall quality of life. The Short Form-36 Health Survey (SF-36)8 is the most widely accepted means of detecting the overall quality of life of patients8–10 on a scale of from 0 to 100 (where 100 is the maximum score). The fact that this questionnaire asks more questions about the lower limbs than it does the upper ones must be taken into account.
Other scales, such as the visual analogue scale (VAS), make it possible to rank the pain perceived by a patient from 0 to 10.11 When the aim is to analyse shoulder working tools such as The Disabilities of the Arm, Shoulder and Hand (DASH) are usually selected. This offers information on symptoms, as well as the capacity for performing certain activities with the arm.12 The Constant–Murley Shoulder Outcome Score (Constant) is also used. This includes a pain score, functional evaluation, amplitude of movement and strength measurements.13 Lastly, the Walch–Duplay Score (WD) analyses stability, pain, sports recovery and mobility.14
This study evaluates the results of arthroscopic repair of AC dislocation in terms of PQL. The SF-36 was used for this, comparing it with specific instruments that measure pain such as the VAS and others which evaluate the shoulder, such as the DASH, the Constant and the WD. The results are associated with the demographic parameters of the series to determine which factors influence clinical and functional evolution after surgery of this type.
Material and methodA prospective study of a consecutive series of patients with Rockwood degree iii to v AC dislocation, treated by arthroscopic reconstruction. The average follow-up lasted for 25.4 months (from 18.5 to 34.6).
The demographic data of the series were recorded, as well as the injury mechanism. For the purpose of the follow-up measurements were taken before surgery and then at 3 months and at 2 years after the operation. There were no losses during the follow-up period of the study. This research was approved by the ethics committee of our institution.
The radiographic study included an anteroposterior X-ray and axial projection (Alexander). Secondary displacement was said to exist when it was greater than 50%. The degree of satisfaction was expressed on a scale of 0–10, where 0 represents not satisfied at all and 10 is totally satisfied. Pain was analysed using the VAS, and functional evaluation was performed using the DASH and the Constant, while the WD scale was used to evaluate the level of activity. PQL was analysed using the SF-36.
The inclusion criteria were patients aged from 18 to 55 years old who are physically active, with no history of previous surgery or injury in the shoulder to be studied, as well as the indication for surgical isometric arthroscopic treatment. Patients treated during the same period with anatomical arthroscopic reconstruction (2 CC suspension devices) were excluded, as were those who presented concomitant disease together with the AC injury. All of the patients who fulfilled the inclusion criteria signed an informed consent form to be included in the study.
Surgical techniqueIsometric repair was performed, so that under general anaesthesia together with an interscalene nerve block the patient was placed in a semi-seated (deck chair) position with the arm in anterior flexion at 50–70° and 2–3kg traction. The subacromial arthroscopy was created with an anterolateral vision portal (2–3cm of the side edge of the acromion) with an anterior working portal through which debridement of the subacromial bursa was performed until the coracoacromial ligament was visible (the point of reference to find the end of the coracoid ligament) together with the base of the coracoid apophysis (inferior view of the same). An incision (2cm) was made about 3cm from the acromial end of the clavicle (the central point between the conoid and trapezoid ligaments), opening the deltotrapezoid fascia until it was visible. The guide of the CC suspension system was inserted (ZipTight Zimmer Biomet, Warsaw, Indiana, United States) positioning it in the lower zone of the base of the coracoid apophysis, with the other part of the guide centred over the clavicle at an angle of approximately 70–90°. The tunnel was bored using a cannulated 4.5mm drill bit from the clavicle to the coracoid over a 2.4mm guide needle, through which a transporter suture was passed that was recovered from the anterior portal. The suspension system was then inserted guided from the cranial edge (clavicle) towards the caudal edge (coracoid process). The rectangular titanium implant was fitted in the coracoid apophysis and the washer was fitted in the clavicle, thereby reducing the AC dislocation and fixing the device.
Postoperative treatment consisted of wearing a sling for 4–6 weeks, starting pendular exercises in the fourth week and then gradually more exercise from the sixth week to gain range of mobility. Contact sports and major efforts were avoided during 4–6 months.
Statistical analysisThe percentage and number of cases were calculated for categorical variables, and the inference was calculated using Fisher's exact test or the Chi-squared test, depending on the dimension in the contingency table. The quantitative variables were described in terms of their average and the standard deviation. Range and inference were calculated using a t-test of related samples, without assuming the existence of homocedasticity. Pearson's lineal correlation coefficient was calculated to study the correlation between the different variables. More specifically, to study the variables of age, displacement, VAS, DASH, Constant and WD Pearson's lineal correlation was used; for the variables of sex and the affected or dominant side, a t-test was used. Finally, for the classification variable a variance analysis was performed. In the main variables, to study evolution over time (measurements before the operation and at 3 months and at 2 years afterwards) variance analysis of repeated measurements was used, correcting a possible sphericity problem using the Greenhouse–Geisser test; in the case of significance, the values prior to surgery were compared post hoc with the 2 subsequent values after the Bonferroni correction. The changes in PQL (SF-36) were also studied in association with the other variables at the first and final controls.
The level of significance was the usual 5% (alpha=.05), bilateral approximation. All analyses were undertaken using the SPSS 19 statistical package (SPSS Inc., Chicago, IL, United States).
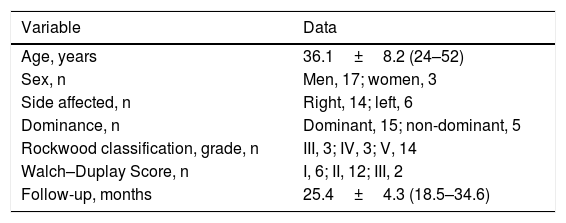
Results42 patients were treated for AC dislocation during the period studied, and of these 20 fulfilled the inclusion criteria described above (Table 1). The series studied was composed of 17 men (85%) and 3 women (15%) with an average age of 36.1 years old (from 24 to 52). The right side was involved in 14 cases (70%), while the left side was involved in 6 cases (30%). The arm involved was found to be the dominant arm in 75% of the cases. According to the Rockwood classification 3 patients (15%) were grade iii, 3 (15%) were grade iv and 14 (70%) were grade v.
Demographic data of the series studied.
| Variable | Data |
|---|---|
| Age, years | 36.1±8.2 (24–52) |
| Sex, n | Men, 17; women, 3 |
| Side affected, n | Right, 14; left, 6 |
| Dominance, n | Dominant, 15; non-dominant, 5 |
| Rockwood classification, grade, n | III, 3; IV, 3; V, 14 |
| Walch–Duplay Score, n | I, 6; II, 12; III, 2 |
| Follow-up, months | 25.4±4.3 (18.5–34.6) |
Expressed as an average ±standard deviation (range) or indicated after the name of the variable.
In the evaluation of satisfaction with the procedure at the end of follow-up, 70% of the patients awarded it a score corresponding to totally satisfied (9 or 10), while 30% awarded it a score expressing notable satisfaction (7 or 8). No patient awarded it a score lower than 7 points. The average percentage of displacement was 37.5±32.7%. When the relationship between the degree of displacement and the results obtained in the different questionnaires was studied, a relationship was only detected with the VAS at the end of the follow-up period (Pearson .56). If we take into account the fact that the value of the correlation index varies within the interval [−1 to 1], a value above 0 indicates a positive correlation, and the closer it is to 1, the more positive the relationship is. That is, there is a positive relationship between the pain patients perceive at the end of follow-up and the degree of displacement they have.
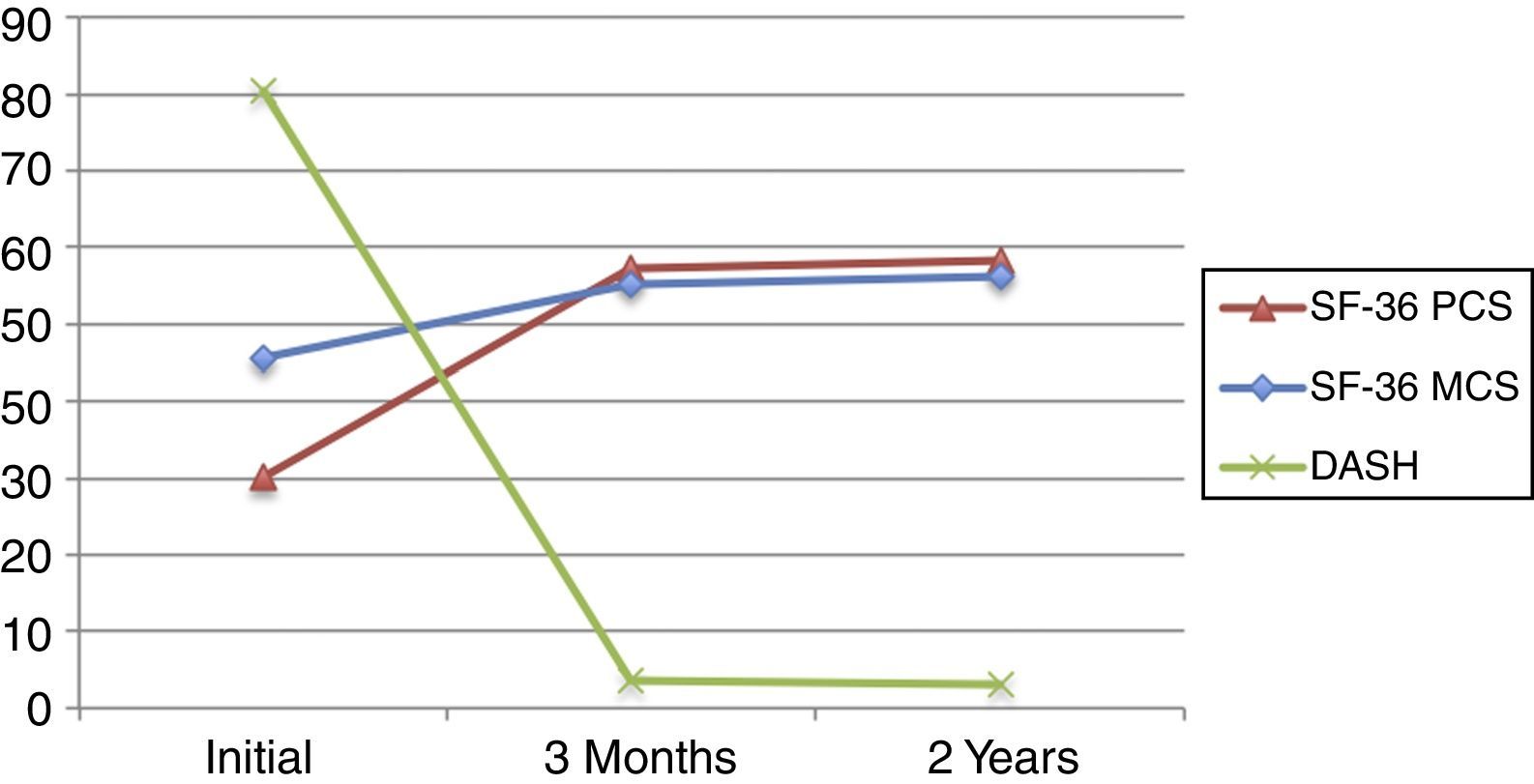
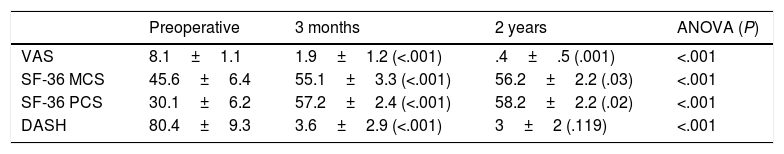
Functional as well as clinical improvement was found in all of the clinical tests analysed (Table 2). The values of the SF-36 in the physical section (PCS) as well as in the mental section (MCS) showed a significant improvement in evaluation at 3 months after surgery, and they stood at 30.1±6.2 at the end of follow-up. The evolution of the dominant side was more significant than the evolution of the non-dominant side, and this fact is associated with the finding that 75% of the patients suffered the AC dislocation on their dominant side.
Results of the clinical and functional evaluation questionnaires during the whole follow-up.
| Preoperative | 3 months | 2 years | ANOVA (P) | |
|---|---|---|---|---|
| VAS | 8.1±1.1 | 1.9±1.2 (<.001) | .4±.5 (.001) | <.001 |
| SF-36 MCS | 45.6±6.4 | 55.1±3.3 (<.001) | 56.2±2.2 (.03) | <.001 |
| SF-36 PCS | 30.1±6.2 | 57.2±2.4 (<.001) | 58.2±2.2 (.02) | <.001 |
| DASH | 80.4±9.3 | 3.6±2.9 (<.001) | 3±2 (.119) | <.001 |
ANOVA: variance analysis; DASH: The Disabilities of the Arm, Shoulder and Hand; VAS: visual analogue scale; SF-36 MCS: the mental component of the Short Form-36 Health Survey; SF-36 PCS: the physical component of the Short Form-36 Health Survey.
Expressed as an average±standard deviation. The P values (in brackets) have been calculated by comparison with preoperative values.
The DASH, in turn, evolved from 80.4±9.3 at first to 3.6±2.9 after 3 months and 3±2 after 2 years (P<.001). Perceived pain evolved from 8.1±1.1 to 1.9±1.2, and it fell to .4±.5 at the end of the follow-up (P<.001). The final value of the Constant test was 95.3±2.4, and the average WD was 1.8±.62.
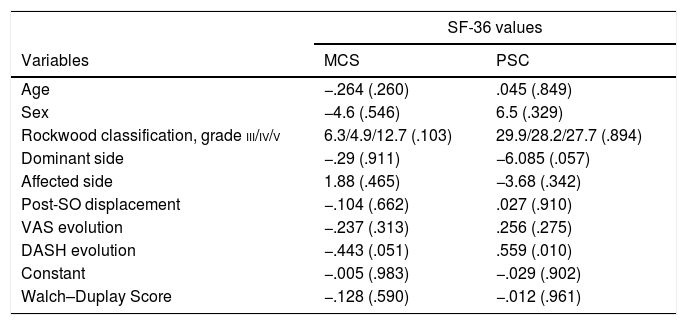
When the evolution of the PQL (SF-36) is correlated with all of the variables studied (Table 3) it was found to be unaffected by age, sex, Rockwood classification, the affected or dominant side, the degree of postoperative displacement or the evolution of the VAS. Likewise, nor was it related to the Constant or WD score. It was found to be statistically significantly correlated with the evolution of the DASH, for the SF-36 MCS (.051) as well as the SF-36 PCS (.010). It should be pointed out that while the correlation of the DASH with the SF-36 PCS was positive, the correlation of the DASH with the SF-36 MCS was negative (Fig. 1).
Relationship between the evolution of the SF-36 and the different study variables.
| SF-36 values | ||
|---|---|---|
| Variables | MCS | PSC |
| Age | −.264 (.260) | .045 (.849) |
| Sex | −4.6 (.546) | 6.5 (.329) |
| Rockwood classification, grade iii/iv/v | 6.3/4.9/12.7 (.103) | 29.9/28.2/27.7 (.894) |
| Dominant side | −.29 (.911) | −6.085 (.057) |
| Affected side | 1.88 (.465) | −3.68 (.342) |
| Post-SO displacement | −.104 (.662) | .027 (.910) |
| VAS evolution | −.237 (.313) | .256 (.275) |
| DASH evolution | −.443 (.051) | .559 (.010) |
| Constant | −.005 (.983) | −.029 (.902) |
| Walch–Duplay Score | −.128 (.590) | −.012 (.961) |
Constant: Constant–Murley Shoulder Outcome Score; DASH: The Disabilities of the Arm, Shoulder and Hand; VAS: visual analogue scale; SO: surgical operation; SF-36 MCS: mental component of the Short Form-36 Health Survey; SF-36 PCS: physical component of the Short Form-36 Health Survey.
Results of the comparison of averages (t-test), difference between averages or correlation coefficient expressed depending on their value and statistical significance P (in brackets) as appropriate.
Three complications occurred: one mechanical failure of the implant which required repeat surgery and 2 granulomas of the surgical wound.
DiscussionThe chief finding of this study was that results in terms of PQL (analysed using the SF-36 questionnaire) in patients operated arthroscopically for grades iii–v AC dislocations are only related with the results obtained in the DASH questionnaire. They are unrelated to sex, age, grade, displacement or the side involved. Secondarily it was found that all of the questionnaires on functioning and quality of life showed a statistically significant improvement at 3 months after surgery, and that this was maintained until 2 years after surgery.
PQL was defined as the capacity of an individual to live a full life.15 Study of PQL has become more important in recent years, and this is partially due to the introduction of techniques such as arthroscopy. These techniques seek to minimise surgical aggression by improving results or achieving similar results to those obtained using more invasive techniques, such as open surgery. Lesions of the AC joint are common in active young patients and have an important impact on PQL, causing pain and functional limitation, while they sometimes make it impossible even to undertaken everyday activities.
The PQL parameters of the SF-368–10 questionnaire make it possible for the evaluator to analyse subjective and objective values associated with the therapeutic option used. The VAS11 is often used to evaluate pain, as it supplies information quickly and directly about how a patient perceives pain. When healthcare professionals or researchers wish to analyse shoulder function, they usually select a questionnaire such as the DASH,12 the Constant13 or the WD.14 This study used these questionnaires, given that the DASH supplies us with data on the symptoms and capacity to perform certain activities with the arm, while the Constant, as well as scoring pain and function, also informs us of amplitude of movement and measurements of strength. Finally, the WD is used to analyse stability, pain, sports recovery and mobility.
When the differences between the preoperative parameter scores and those at 3 months and at 2 years after surgery are analysed, all of the values for pain, functioning, mobility and satisfaction improved. Nevertheless, the main aim of this study was to show how these values influence PQL for the patient after the arthroscopic repair of grade iii–v AC dislocations. Only the DASH was found to be associated with PQL.
Although the literature contains several studies that show improved PQL after shoulder surgery, they centre on rotator cuff injuries. Authors such as Vitale et al.16 report improved PQL after analysing the Health Utility Index and the European Quality of Life Survey. The same occurs with Baysal et al.,17 as they show that repair of complete rotator cuff thickness injuries using a mini-open technique improved PQL. They analysed its function using the specific rotator cuff questionnaire, the Western Ontario Rotator Cuff Index.
If we centre on studies that analyse PQL after surgery on the same scale that was used in this study (the SF-36), Gartsman et al.18 as well as McKee and Yoo,19 in their respective studies, show an increase in SF-36 scores after rotator cuff reconstructive surgery.
No factors were found in this study which affect PQL results after surgery. When the results are analysed according to sex, the results disagree depending on whether they are on the physical or mental scale. The improvement is greater in the PCS for men (29.08) than it is for women (22.6). The result in the MCS is 9.9 for men and 14.5 for women, although all of these differences are not statistically significant. This is probably due to the clear imbalance between the number of men (17) and women (3). Discrepancies in the results of the SF-36 depending on sex have also been reported in rotator cuff studies such as the one by Razmjou et al.20
In connection with age, Han et al.21 showed that there is a negative correlation between the SF-36 and age. We did not detect this in our study, probably because its series is composed of younger patients who are more homogeneous in terms of age.
It should be underlined that the patients in the series analysed had a secondary displacement of around 40%. This is probably due to the use of a single AC suspension system. Because of this, after the study ended we switched to using 2 devices in anatomical configuration.
This study has some limitations. Firstly, its series is relatively short (20 patients), although it also has to be said that there were no losses during follow-up. Secondly, the average duration of follow-up was 25.4 months (from 18.5 to 34.6 months). This may seem relatively short, as the results of the SF-36 are valid over the long term. In spite of this, we believe that for repairs of AC dislocations the result after 2 years is sufficiently significant. It must be kept in mind that the correlation of the SF-36 questionnaire with the specific tests for each ailment has been described as weak to moderate; it therefore has to be used together with other specific questionnaires for the injury or anatomical region studied.
Lastly, although the SF-36 has been used in many studies to evaluate PQL, it may be considered to lack sufficient sensitivity to detect specific shoulder problems. Nevertheless, in the literature there are no specific PQL questionnaires for the upper limbs. Additionally, the aim was to centre analysis of PQL in general to a greater degree than would be possible with specific questionnaires such as the DASH, Constant or WD.
In spite of the limitations described above, as far as the authors are aware this paper is the first study which specifically analyses the factors that affect PQL (using the SF-36) in patients operated arthroscopically for grade iii–v AC dislocation.4,22
ConclusionPQL (evaluated using the SF-36) in patients operated arthroscopically for grade iii–v AC dislocation is not influenced by sex, age, grade, displacement, laterality, VAS evolution, the Constant or the WD score. It is correlated with evolution in the DASH, probably because it scores similarly to the SF-36.
Level of evidenceLevel of evidence iv.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Abat F, Gich I, Natera L, Besalduch M, Sarasquete J. Factores clínicos que afectan a la calidad de vida percibida en la reconstrucción artroscópica de las luxaciones acromioclaviculares. Rev Esp Cir Ortop Traumatol. 2018;62:121–126.