This is a retrospective study of 98 diaphyseal forearm fractures in adults, treated by a percutaneous technique with intramedullar Kirchner wires.
Materials and methodWe reviewed 64 patients with 98 forearm fractures with a radiographic follow-up, assessing the presence of pseudoarthrosis or delayed bone union and evaluating functional outcomes with the Anderson and the Disability of the Arm, Shoulder and Hand scale.
ResultsClinical and radiological bone union was achieved in an average of 12 weeks. We obtained 77% of excellent and good results following Anderson's scale. There were 4 cases of pseudoarthrosis and 6 cases of delayed bone union.
ConclusionThis surgical technique provides several advantages, such as a low incidence of complications and a total absence of infections, refractures and iatrogenic neurovascular injuries. It allows a lower hospital stay and a shortening of the surgery time compared with other techniques such as plates and intramedullary nails, that have similar results, in terms of bone union and functional outcomes, as we have verified from the published literature.
Estudio retrospectivo de 98 fracturas diafisarias de antebrazo en adultos tratadas mediante osteosíntesis percutánea intramedular con agujas de Kirchner.
Materiales y métodoSe revisan 64 pacientes que presentaban 98 fracturas de antebrazo con un seguimiento clínico-radiológico, evaluando la presencia de seudoartrosis o retardo de la consolidación y valorando los resultados funcionales mediante la Escala de Anderson y el Disability of the Arm, Shoulder and Hand.
ResultadosLa consolidación clínica y radiológica se consiguió con una media de 12 semanas, obteniendo un 77% de excelentes y buenos resultados con los criterios de Anderson. Se registraron 4 casos de seudoartrosis y 6 casos de retardo de consolidación.
ConclusiónLa osteosíntesis percutánea presenta una serie de ventajas con respecto a otras técnicas como son una baja incidencia de complicaciones, ausencia de infecciones, refracturas y lesiones yatrogénicas vasculonerviosas. Se consigue una menor estancia hospitalaria y un acortamiento del tiempo quirúrgico, con unos resultados similares al tratamiento con placas y clavos endomedulares en cuanto a consolidación y resultados funcionales, como comprobamos al consultar la bibliografía publicada.
The aim of treating diaphyseal forearm fractures in adults is to obtain suitable axial and rotational stability,1 and this is why plates are still considered to be the treatment of choice.2,3
In 1957 Smith4 invented intramedullary fixation, underlining its eminently periostic consolidation and the non-aggressive nature of the operation. High rates of pseudoarthrosis and its long immobilisation time made this method unpopular, although this has now been overcome with newly designed pins.5–8
Our hospital has traditionally been a promoter of percutaneous treatment for diaphyseal fractures of the forearm, using Kirschner needles (KN). This is largely due to the works by Morote and Pérez Sicilia9 on forearm fractures in children and adolescents, and it is now recognised internationally as the treatment of choice.
Before osteosynthesis using plates became widespread, fractures of this type in adults were treated using intramedullary KN. It gave good results in spite of the data in some studies.1,4,5 This method has continued to be used in our hospital to date, as although it is not considered to be the standard technique, it is often used under certain circumstances to treat forearm fractures in adults.
Although this treatment has many detractors, there are currently no recent studies which compare its results with those obtained using other osteosynthesis techniques.
The results obtained in our series show that it is a totally valid alternative treatment for fractures of this type, on condition that it is accompanied by careful indication and exquisite surgical technique. The aim of this study is to describe surgical technique using intramedullary needles and to evaluate its efficacy and the results obtained in our series in the surgical treatment of adults with fracture of the radius, ulna or of both. These results are then compared with those described in the published literature on treatment with plates and intramedullary pins.
Material and methodPatients and methodAll of the cases of forearm fracture treated in our hospital from January 1995 to March 1999 were evaluated retrospectively.
The study inclusion criteria were diaphyseal fracture of the radius, ulna or both, including closed fractures as well as all degrees of open ones. Patients had to be over the age of 18 years old and had to have been treated only by percutaneous osteosynthesis with KN. Patients who had proximal or distal radius and ulna dislocations were excluded from the study (Monteggia or Galeazzi), as were those with intrajoint fractures of the distal epiphysis of the radius or ulna, and fracture of the olecranon or head of the associated radius.
Surgical techniqueGeneral anaesthesia or blockage of the brachial plexus. Patient in supine decubitus. The affected limb with the shoulder in abduction at 90° and elbow in 90° flexion, held by a lateral support at the level of the elbow. Traction is applied by bandages around the bottom of the first 4 fingers, which are tied to the waist of the surgeon while he reduces the fracture with the aid of radioscopy.
This technique is not considered indicated when it is not possible to restore the length due to defects in reduction or comminution, or when neighbouring joint surfaces are affected.
It is recommendable to firstly pin the fracture that is the most displaced, as the fact that both bones are fractured facilitates the reduction manoeuvres. A fracture of the radius that is difficult to reduce is even harder to reduce when the ulna is fixed. Once the radius is fixed, if the ulna is impossible to reduce then the approach is simpler.
To insert the KN in the radius the radial styloid is located at the dorsolateral level. With a 3 or 4mm KN and using circular movements an entry hole in the bone is created that is wide enough to allow the KN chosen for osteosynthesis to pass through. A smaller diameter KN than the previous one is prepared, of about 2mm, and it is preformed to adapt it to the curve of the radius in the AP plane. One of its ends is also prepared to create a skid, suitably curved to easily pass the distal epiphysis of the radius. Once the centre of the fracture has been passed the pin will be lodged in the most proximal end of the radius, always inserting other KN to the degree that this is made possible by the diameter of the medullary canal.
For osteosynthesis of the ulna the tip of the olecranon is located, making an entry orifice in the way described above. A 2–3mm KN is selected and its point is cut. The flattest end is bent about 20° to facilitate its entry and passage through the centre of the fracture when the reduction is not anatomical. Working with a blunt point prevents the creation of false routes and improves our awareness that we are at all times in contact with the medullary cavity. The needle is inserted gradually until the fracture is passed, taking it to the distal epiphysis of the ulna. Other KN may also be inserted, without a distal angle, to fill the medullary canal as much as possible.
After affixation the fracture centre is compressed by applying forces to the wrist and elbow, after which the end of the KN is buried under the subcutaneous tissue. Immobilisation takes place using a plaster brachial rod, completed with closed plaster after 15 days in the first check-up visit. Functional articulated plaster is used at the elbow when the limb is not swollen and permits a good fit. In some very stable fractures at 2 months it is possible to fit a functional forearm plaster. All of the patients were sent to rehabilitation to gain joint and muscle balance.
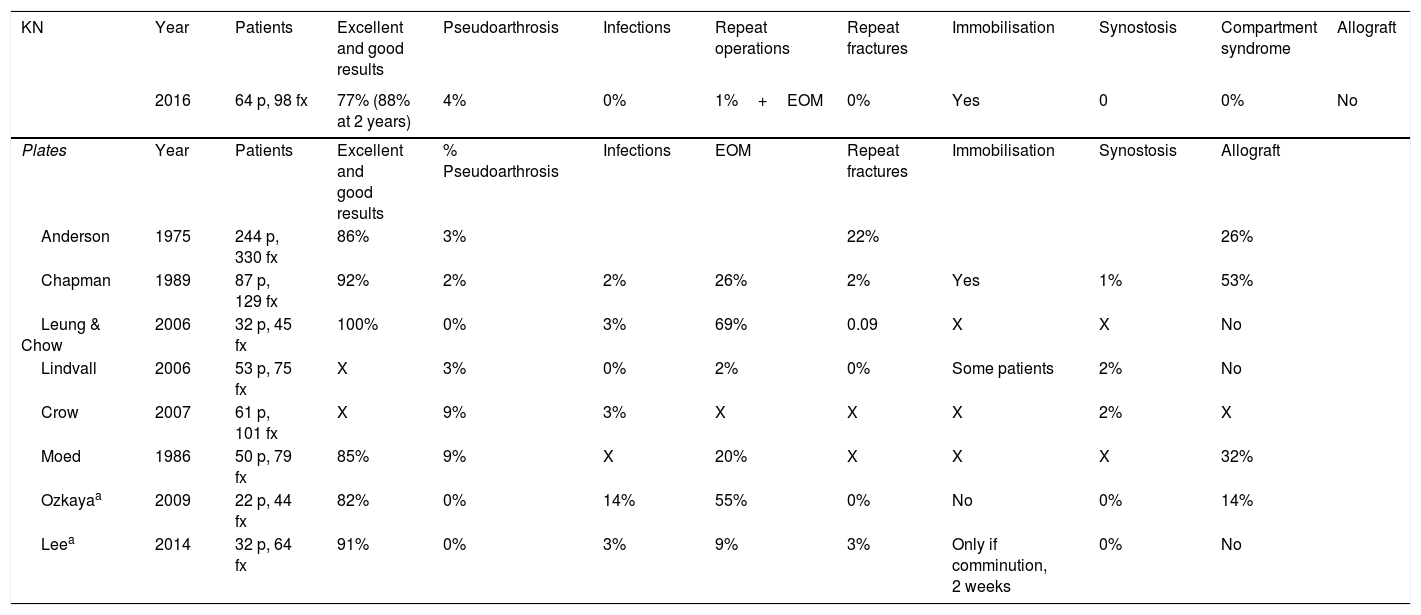
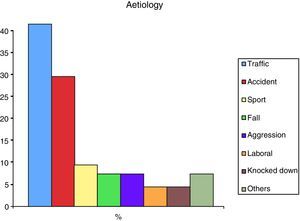
Evaluation of the patientsOf the 81 clinical histories that fulfilled the criteria, 17 patients were lost during the 18 month follow-up. The data of 64 patients were analysed (42 men, with an average age of 39 years old [range 18–88]) with 98 diaphyseal fractures of forearm bones. Thirty-four patients had fractures of both bones, 19 only had fracture of the ulna and 11 had isolated fractures of the radius. The injury was to the left forearm in 38 cases and the right forearm in 26. The most frequent cause was traffic accident (40%), followed by an accidental fall (28%), a sports injury (8%), falling (6%), aggression (6%), being knocked down by traffic (3%) and accident at work (3%) (Fig. 1).
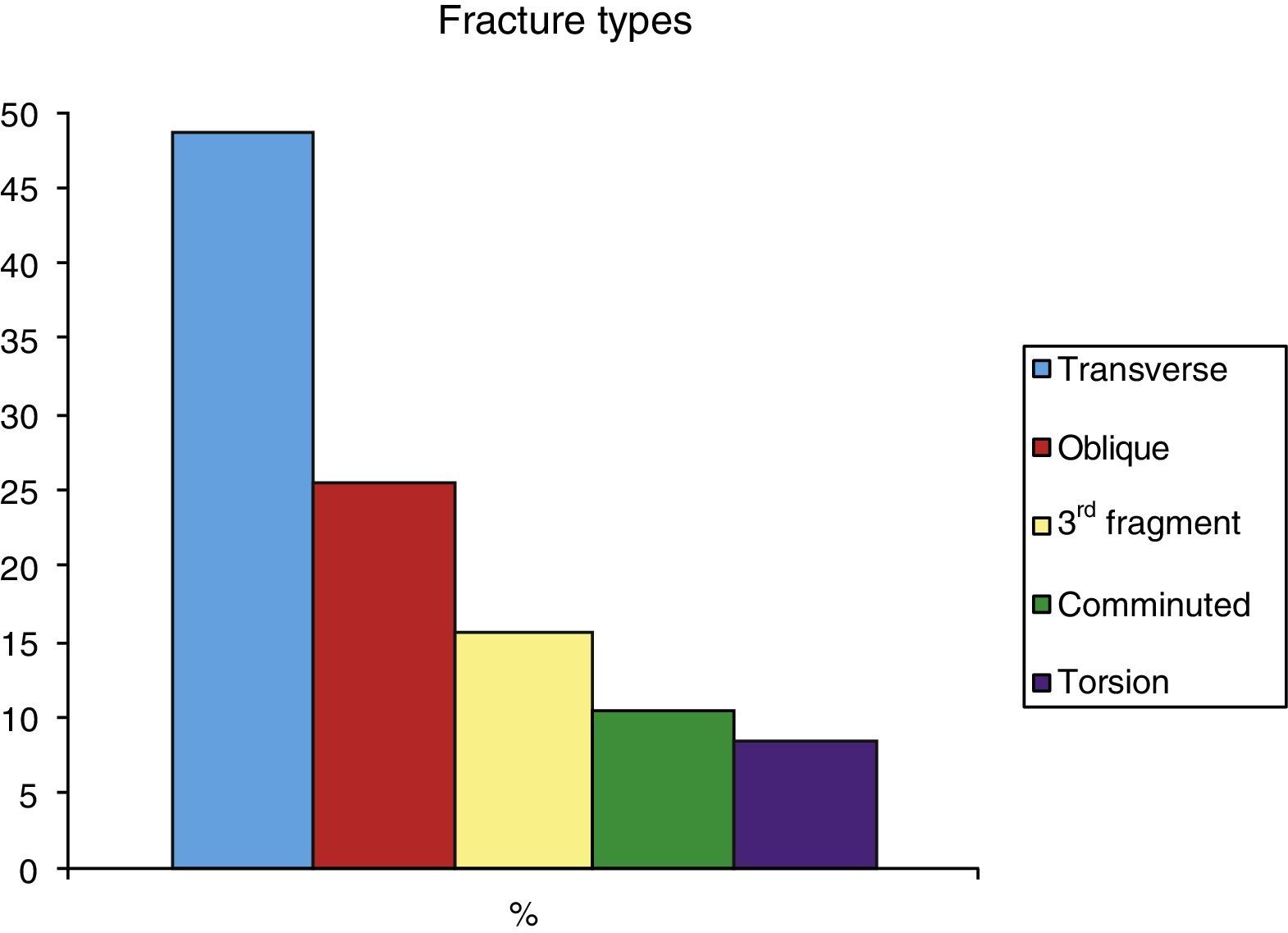
The most frequent type of fracture was transversal (46%), followed by oblique (23%) and with a third fragment (13%). Comminution and spiral fractures were less common (10% and 8%, respectively). Fractures were most often located in the median third (55%), followed by the distal third (32%) and the proximal third (13%) (Fig. 2).
28% of the total were open fractures (using Gustilo's classification: 10 cases were grade I, 4 cases were grade II, 3 cases were type IIIA and one case type IIIC). One case had radial nerve sensory paresis at admission and there was one case of muscle hernia. A total of 25 cases (39% of the total) were diagnosed with associated injuries at other locations when they were admitted.
The average delay until surgery was 27h, and the operation took place under general anaesthesia in 2/3 of patients and regional blockage in the remaining third. The average duration of anaesthesia for the operation was 44min (including patients who had associated surgical wounds that were resolved within the same surgical time). Excluding these procedures the time falls to 33min. Five cases required opening of the fracture centre as an appropriate reduction was not achieved. The average duration of hospitalisation was 1.6 days, excluding the patients with associated injuries. The average duration was 5.2 days when patients with multiple injuries are included.
All of the patients were evaluated clinically and radiologically after one month and at 3, 6 and 12 months. The final check-up took place 18 months after the injury, or 6 months after removal of the implant in those cases where one had been necessary, without incidents and in a regime of major outpatient surgery (MOS). The final check-up included clinical evaluation of pain and function.
Bone consolidation was defined as the obliteration of the space of the fracture or the presence of a periosteal callus in X-rays. Delay in consolidation was defined as the persistence of the fracture or the absence or slowness in gradual formation of the callus during the expected time corresponding to the location and type of fracture, i.e., 3–6 months after the operation. When this condition lasted for more than 6 months it was defined as pseudoarthrosis.
The functional results of fracture setting were classified according to the state of fracture healing and range of movement according to Anderson's criteria.10 The patients also completed the Disabilities of the Arm, Shoulder and Hand11 questionnaire, which measures quality of life in connection with upper limb problems. It is based on the symptoms or limitations patients have found in terms of pains and their everyday activities.
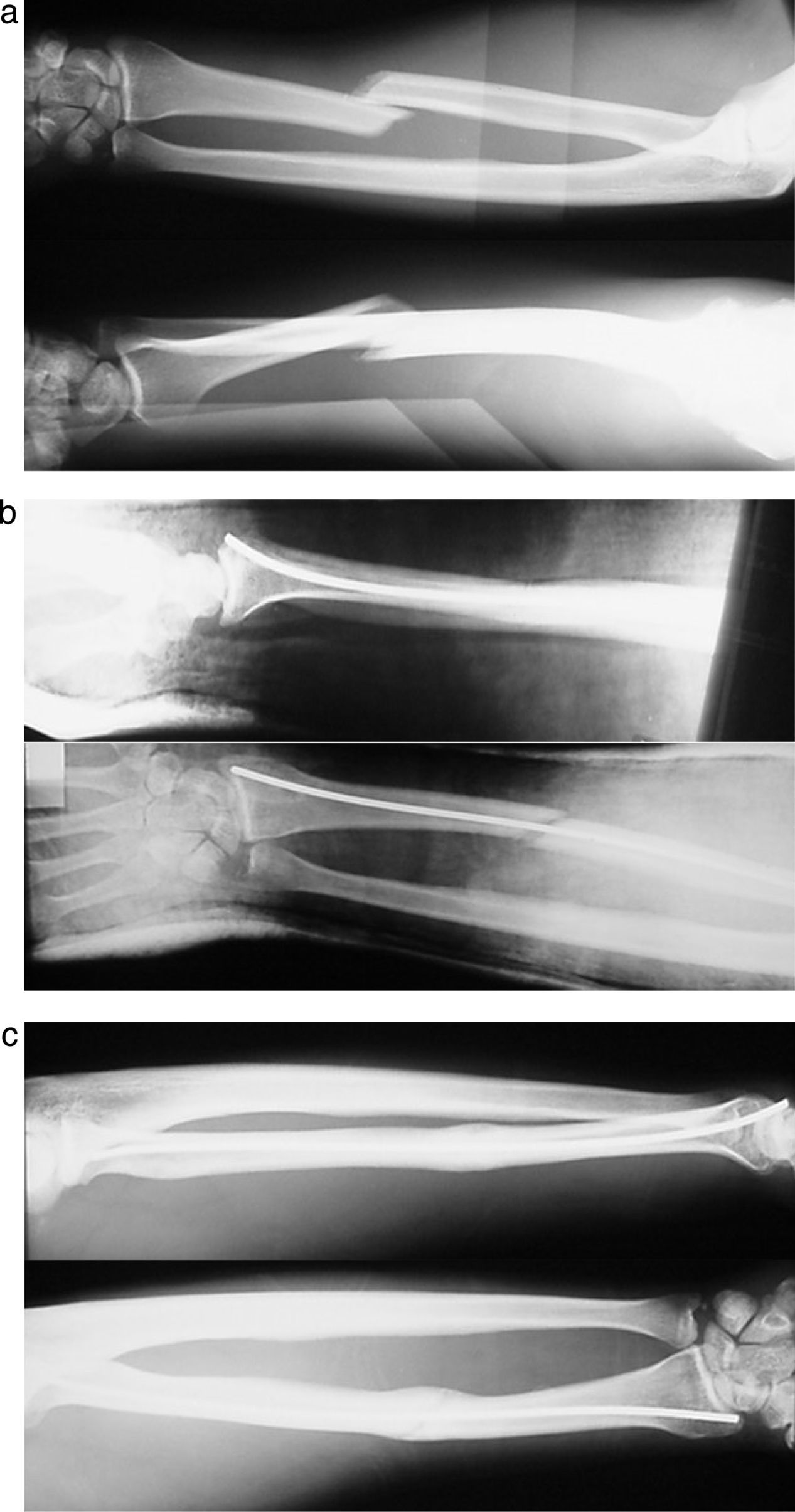
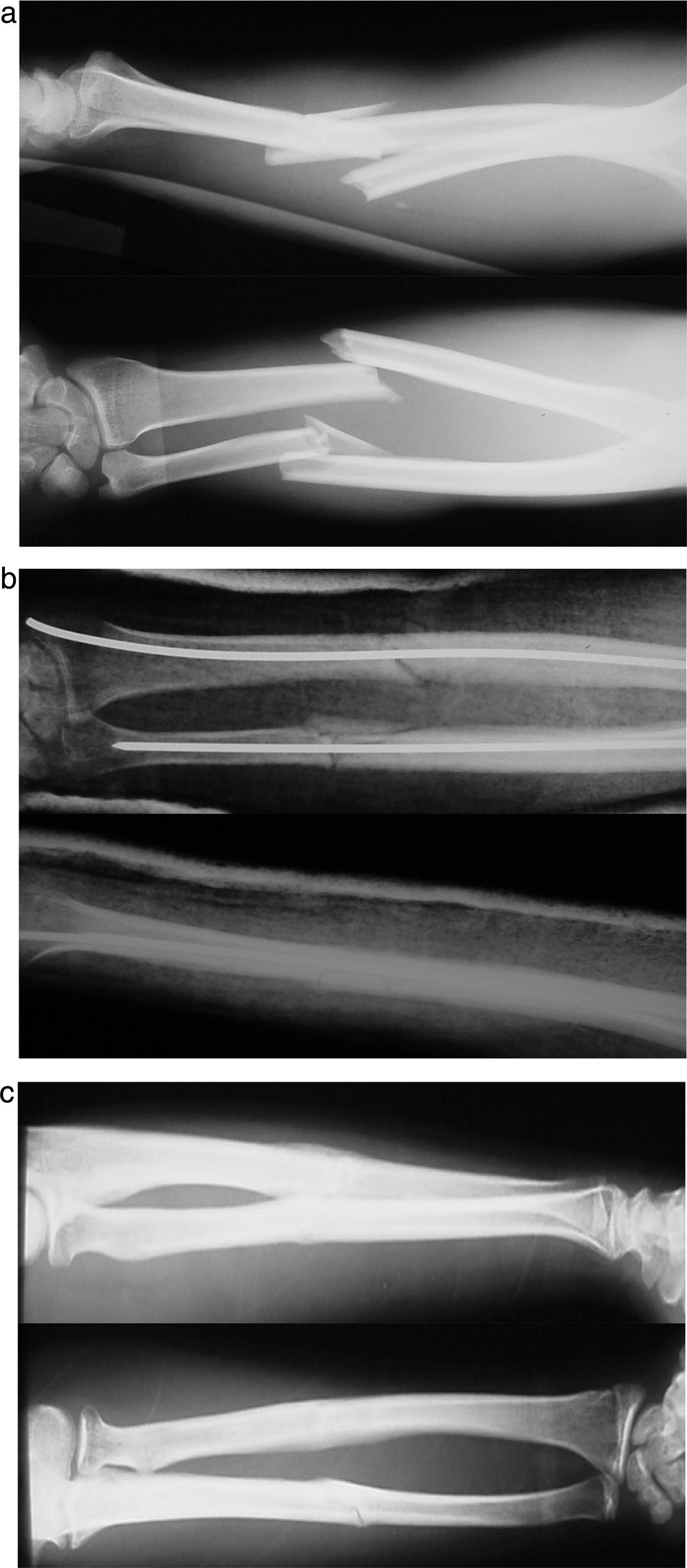
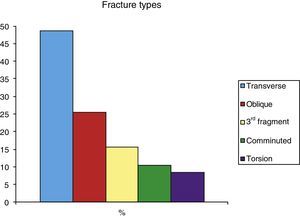
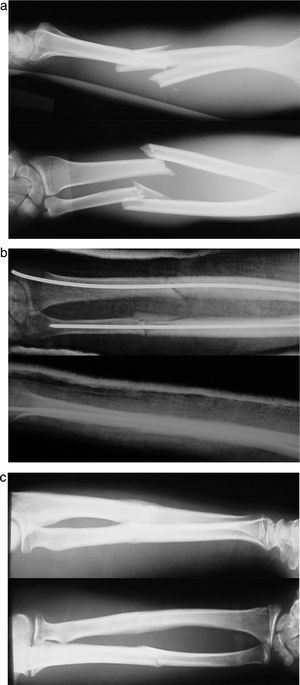
ResultsClinical and radiological consolidation was attained in an average of 12 weeks. Eighty-six fractures (88%) consolidated without incidents (Figs. 3 and 4).
Regarding associated complications, 6 cases were recorded of delayed consolidation together with 4 cases of pseudoarthrosis.
Of the 6 cases (6%) classified as delayed consolidation, 5 corresponded to ulna fractures and a sixth case was caused by insufficient KN within the radius. Three of these cases (50%) occurred in open fractures. None of the cases of delayed consolidation required any action by us to achieve complete healing, except for the preservation of the intramedullary KN until the bone callus was observed to have commenced forming. Fracture consolidation was achieved after an average 7 months, except for one open fracture of the ulna that consolidated after 10 months.
Four patients were diagnosed with pseudoarthrosis: one isolated pseudoarthrosis of the ulna was detected, together with one of the radius and 2 of both bones. These cases correspond to 4% of the total, with the special circumstances that all of them were synthesised with a single KN. Three cases of pseudoarthrosis corresponded to open fractures (2 grade I and one grade IIIA in Gustilo's classification).
The isolated pseudoarthrosis of the ulna was in a patient who had fallen from a height, with fracture of both bones of the forearm in the middle third. When pseudoarthrosis of the ulna was detected a new osteosynthesis was performed using a plate and an autologous graft, after which the fracture consolidated without further incidents.
The pseudoarthrosis in the radius corresponded to a patient with fracture of the distal third of the radius and ulna, requiring the opening of the centre of the fracture to be affixed using KN. After the failure of the percutaneous osteosynthesis an open reduction was performed with support by a plate together with autologous graft material, with excellent clinical and radiological results.
The other 2 cases were of pseudoarthrosis of both forearm bones. The first case corresponded to a patient with multiple trauma and concomitant injuries: at admission the patient had open grade IIIA fractures of both forearm bones. A skin graft was needed to cover the defect, and after detecting pseudoarthrosis it was decided to re-operate 9 months after the fracture for a new osteosynthesis using a plate and petalisation of the centre of the pseudoarthrosis. The case was complicated by breakage and infection of the material; finally, after removal of the material and control of the infection the patient was operated on again and fitted with a new plate, this time with a bone allograft. The fracture consolidated at 24 months with a good functional result.
The second case of failure to consolidate in both bones was in a patient who had suffered a traffic accident. The diagnosis was of comminuted fracture of the ulna and fracture of the radius with a third fragment. Repeat surgery was needed to join the fractures using plates and iliac crest graft. This caused synostosis of the radius and ulna that required another operation. Finally a good functional result was achieved, with less than 20° limitation of supination.
We had no case of compartment syndrome, Volkman's syndrome or intraoperative vascular or nerve injury. The only incident recorded was post-traumatic sensitive paresis of the radial nerve at admission. This resolved spontaneously after 3 weeks, without requiring treatment.
No deep or superficial infections occurred.
We had no case of synostosis of the radius or ulna with this technique.
An isolated case of shortening of the radius with sub-dislocation of the ulna occurred. This was in an open grade IIIA fracture due to dog bite in a destitute patient. The fracture consolidated after 5 months and the patient did not agree to further interventions, accepting the consequence with an acceptable result on Anderson's scale.
There was a single case of acute breakage of the long extensor of the thumb due to contact with the needle. Tendon transfer was performed of the index finger extensor to the long extensor of the thumb with an excellent functional result in all aspects.
Two cases of reflex sympathetic dystrophy were diagnosed. They evolved well without consequences after medical treatment and rehabilitation.
There was no case of material breakage. The KN were removed after an average of 5.9 months in 39 patients of the 64 studied, in MOS regime and without any noteworthy incidents. The other patients did not require removal as the material caused them no discomfort.
Reinforcement of the callus was found in all of the patients from whom KN were removed, as the intramedullary motion during extraction of the preformed needle damages the centre of the fracture again, thereby increasing the previous effect and making further preventive immobilisation unnecessary. No repeat fractures were observed in any of the patients included in the study.
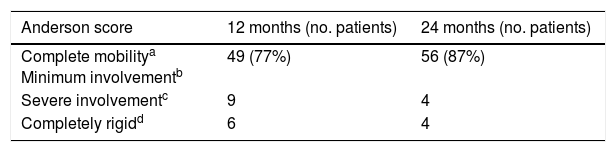
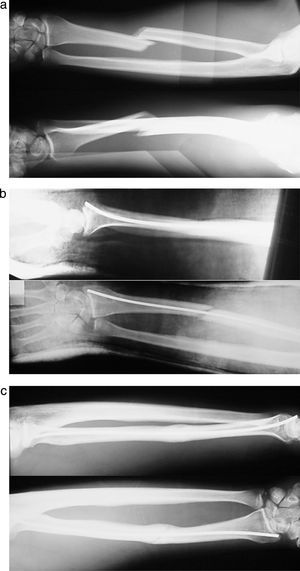
The functional results evaluated using Anderson's criteria after the first 12 months were excellent or good in 77% of cases. Re-evaluation of the functional results after 24 months showed 88% of excellent or good functional results (Table 1). The unsatisfactory results all involved cases when the fracture centre had to be opened for reduction.
Functional results – Anderson scale.
| Anderson score | 12 months (no. patients) | 24 months (no. patients) |
|---|---|---|
| Complete mobilitya Minimum involvementb | 49 (77%) | 56 (87%) |
| Severe involvementc | 9 | 4 |
| Completely rigidd | 6 | 4 |
Excellent means healing of the fracture, loss of less than 10° in flexion–extension of the elbow or wrist and less than 25% loss in pronation and supination.
The clinical re-evaluation of these patients is pending, to check the long-term functional results at 16 years.
The average score in the Disabilities of the Arm, Shoulder and Hand questionnaire was 18 points, showing a slight deterioration in functionality. Nevertheless, all of the patients stated that they had recommenced their activity prior to the accident, and none of them required chronic medication for painful symptoms.
DiscussionThe main aim of treating diaphyseal fractures of the forearm bones is to obtain good functionality after bone consolidation. Good rotational and axial stability has to be conserved to achieve this. The most important thing is to preserve the curvature of the radius as well as the integrity of the joints of the radius and ulna.
Osteosynthesis using plates is now the standard surgical technique.1,10,12 However, it is not free of risks and complications: treatment using plates is more aggressive for the vascularisation of the fracture centre, given that it is accompanied by harm to the periostium as well as the surrounding soft tissues, and it also requires evacuation of the fracture haematoma.1,10,13,14 The aim of the whole process is to achieve an anatomical reduction that may eventually cause a higher number of cases of pseudoarthrosis, especially if it also involves excessive de-periostisation.7,12 In the series studied the rates of pseudoarthrosis recorded run from 0%1,7,13 up to 9%.3,15 In our series the rate was 4%.
Another intrinsic and counterproductive effect of the osteosynthesis technique using a plate is the drilling of the cortical bone to insert the screws, as this weakens the bone mechanically.3,16 Likewise, the interbone membrane is harmed, and this is considered to be an important factor in the causation of synostosis of the radius and ulna.17 Another hypothesis is that harmful effects are connected with endostic circulation, the increase in local temperature when drilling and the alteration to bone structure3,16 which may interfere with the normal process of fracture callus formation.
It has to be said that in many of the papers that were reviewed1,10,15,18 an autologous bone graft is used in the first surgical operation to aid consolidation. This increases morbidity,19 the duration of the operation and the costs associated with surgery.
Nor is the risk of infection insignificant in osteosynthesis with a plate. The combination of 2 special circumstances, the broad approach for osteosynthesis and the high percentage of these fractures that are open, make this complication more probable. In the series studied the infection rate stands at up to 14%.1 In our cases of osteosynthesis with KN there was no case of infection.
Finally, another complication that is not at all exceptional consists of repeat fractures after the removal of material.20–22 They are very common in injuries of this type, with rates of incidence reported in the literature from 4% to 22%,1,17,23 leading patients to be subjected to further operations.
The rates of osteosynthesis material extraction shown in different studies and due to different causes (deep infection, pseudoarthrosis, protrusion or breakage of the material) are high, amounting to up to 69%.3,13 Nevertheless, this datum is not described in all of the papers that were revised.
As is logical, all repeat operations involve an exponential increase in the rate of associated complications and comorbidities. Additionally, in the case we are describing, the removal of material makes preventive immobilisation necessary during approximately 6 weeks.1,6,17,18 This reduces the advantage of the said method in comparison with percutaneous osteosynthesis (PO).
Open reduction and osteosynthesis with plates is still the treatment of choice. It gives excellent results on condition that the technique is performed carefully and with a high standard for achieving the desired results.
Endomedullary osteosynthesis in forearm fractures has once again become more widespread in recent years. This is due to the improved design of locked endomedullary nails, which are now being used more frequently.7,23–25
Several studies find that, contrary to hypotheses, treatment using intramedullary nails delays fracture consolidation.5 It has also been found that consolidation rates are comparable to those obtained when a plate is used.1,7
One of the main advantages of intramedullary nails that they share with our series is that they affix the fracture at a distance without affecting the fracture haematoma,12,26 favouring the creation of the bone callus.23,26 On the other hand, other advantages of percutaneous osteosynthesis should be considered, and these are described below.
A disadvantage with nails that we found in many of the authors1,7,8,25 is that they require immobilisation, in some case during up to 6 weeks. In this respect nails offer no benefit in comparison with percutaneous treatment with KN. Additionally it does not block rotation of the forearm bones, giving rise to an unstable structure that requires immobilisation in plaster. Compared to previous studies (Table 2) we found that both techniques, plates and above all intramedullary nails, use an additional external support to control the soft tissues and favour the formation of the fracture callus.1,7,8,18,24,27
Comparative table of results.
| KN | Year | Patients | Excellent and good results | Pseudoarthrosis | Infections | Repeat operations | Repeat fractures | Immobilisation | Synostosis | Compartment syndrome | Allograft |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2016 | 64 p, 98 fx | 77% (88% at 2 years) | 4% | 0% | 1%+EOM | 0% | Yes | 0 | 0% | No | |
| Plates | Year | Patients | Excellent and good results | % Pseudoarthrosis | Infections | EOM | Repeat fractures | Immobilisation | Synostosis | Allograft | |
| Anderson | 1975 | 244 p, 330 fx | 86% | 3% | 22% | 26% | |||||
| Chapman | 1989 | 87 p, 129 fx | 92% | 2% | 2% | 26% | 2% | Yes | 1% | 53% | |
| Leung & Chow | 2006 | 32 p, 45 fx | 100% | 0% | 3% | 69% | 0.09 | X | X | No | |
| Lindvall | 2006 | 53 p, 75 fx | X | 3% | 0% | 2% | 0% | Some patients | 2% | No | |
| Crow | 2007 | 61 p, 101 fx | X | 9% | 3% | X | X | X | 2% | X | |
| Moed | 1986 | 50 p, 79 fx | 85% | 9% | X | 20% | X | X | X | 32% | |
| Ozkayaa | 2009 | 22 p, 44 fx | 82% | 0% | 14% | 55% | 0% | No | 0% | 14% | |
| Leea | 2014 | 32 p, 64 fx | 91% | 0% | 3% | 9% | 3% | Only if comminution, 2 weeks | 0% | No |
| Nails | Year | Patients | Excellent and good results | Pseudoarthrosis | Infections | EOM | Repeat fractures | Immobilisation | Synostosis | Compartment syndrome |
| Street | 1982 | 7% | ||||||||
| Hong | 2005 | 18 p, 32 fractures | 72% | 0% | 13% | 6% | X | Yes, 2–3 weeks | 5% | 0% |
| Visna | 2008 | 78 p, 118 fx | 90% | 0% | 1% | 34% | 0% | 22%, 3.5 weeks | 3% | 1% |
| Wechback | 2009 | 32 p, 40 fractures | 79% | 3% | 0% | 56% | 0% | No | 6% | X |
| Leea | 2014 | 35 p, 70 fx | 95% | 3% | 0% | 6% | 0% | Yes, 6 weeks | 0% | 0% |
| Ozkayaa | 2009 | 20 p, 40 fx | 90% | 0% | 0% | 35% | 0% | Yes | X | 0% |
| Saka | 2013 | 43 p, 59 fx | 100% | 0% | 5% | X | 0% | No | 0% | 0% |
EOM: extraction of osteosynthesis material; Fx: fractures; Results E and B: excellent and good results; Comp. syn.: compartment syndrome; X: no data in study.
It should also be said that nails do not completely resolve the problem of the natural angle of the radius,5,6 which is easier to achieve using flexible fixation methods.
Respecting the other frequent problems, fixation of this type using nails does not completely resolve the problem of infections, although rates of infection when it is used seem to be somewhat lower than those associated with open reduction and fixation with plates (Table 2).
Nor does it completely eliminate the risk of damaging neighbouring structures, as injuries to the posterior interosseus nerve28,29 have been described, as well as breakage of the long extensor of the thumb30 (one case in our series).
Synostosis is one of the most severe complications of this technique, and it occurs at a rate of up to 6%.8 This figure is not insignificant given the poor functional result and the consequences which this terrible complication usually causes.
Although the extraction of osteosynthesis material is habitual practice in these patients,1,5,8 it adds associated complications due to the loosening of osteosynthesis material and the locking system, with the risks and difficulties that this involves. In favour of this practice it has to be said that no repeat fractures were observed in the studies that were reviewed.
However, and in spite of the fact that intramedullary nails will not be considered to be the treatment princeps, the results of patient satisfaction surveys seem to be slightly better with them than is the case for those about plates (Table 2).
PO is considered to be a “classic” treatment, and there are data on its use in the 1920s. Nowadays there is debate about the use of this treatment as a solution for these fractures. Nevertheless, some authors12,17 consider that this type of osteosynthesis will still have its place among the surgical indications for fractures of both forearm bones. We agree with them that when these fractures are present in patients with multiple trauma or multiple fractures, the most important thing is to establish a definitive treatment with the best results in the shortest possible time. In these cases we can be sure that the patient will be immobilised for a certain time due to associated processes; patients with multiple comorbidities and/or poor quality bone, cases that present poor condition of the soft tissues with the risk of developing compartment syndrome or associated infections, including open fractures which compromise the surgical approach zone. This technique has the advantages of minimising aggression to tissues and achieving fixation at a distance, so that the patient types described above are ideal candidates for considering its use.
PO has been said to have low rates of consolidation, poor functional results and a range of associated complications23; nevertheless, in an exhaustive search of the bibliography we found no recent, well-documented and systematic studies that could be compared to ours. There is one study by Mseddi in 200812 that retrospectively reviewed a far smaller series than the one we present here, and it also in fact considered that percutaneous KN is under certain circumstances an optional treatment.
High rates of non-joining were classically reported with this treatment, at up to 20%.1,4,26 This result is not comparable when our series is reviewed, as it shows a rate of only 4% of pseudoarthrosis, and this is very similar to the results obtained using nails and plates.
The poor results described with PO technique are probably due to poor technique involving failure to stably fill the medullary canal with one or two needles, as we found in our series. The cases of pseudoarthrosis coincide in that the affected patients had a single intramedullary KN, so that it may perhaps be considered to be a failure of surgical technique.
The strength of this technique lies, in part, in fixation by means of least 2 intramedullary KN that create sufficient stability in the fracture.
An outstanding advantage of PO with KN is the absence of infection. No case of deep infection was recorded in our series. This notable advantage, together with its minimum harm to soft tissues and better cosmetic results, shows that it is superior to plates in this respect.
Another clear advantage over the use of plates concerns the removal of material and repeat fractures. Regarding the removal of the KN material, the tolerability of the extraction technique, which is simple and innocuous, as well as the subsequent results were excellent in all of the patients, and no case of repeat fracture was observed.
Although the results obtained with nails are quite similar to those of our series, they too have certain disadvantages. They require the centre of the fracture to be opened by 40%,5 thereby increasing the duration of surgery (which lasts for longer than 60min,1,5,8,28 double the time taken with PO technique in our series). They also lead to a high rate of rigidity in comparison with KN. The flexibility which KN give to the medullary diameter, making it possible to recover the physiological diaphyseal curve of the radius and ulna, is hard to surpass using nails and plates.
When PO is performed using meticulous technique under suitable indications, it achieves results similar to those obtained with nails and plates in terms of functionality and consolidation rates. It gives rise to shorter surgery and has the advantages of percutaneous surgery such as a lower infection rate, good cosmetic results and a minimum of harm to neighbouring structures. We found no cases of synostosis, compartment syndrome, repeat fractures or complications due to the extraction of material.
Some of the weak points classically attributed to the technique, such as high rates of pseudoarthrosis, do not correspond to the study performed. Likewise, we found that temporary immobilisation is not a disadvantage that is specific to this technique, but rather that it also applies to the use of nails or plates.
One weakness of this study is its retrospective nature, but it does add to the possibility of using a surgical technique that is considered to be obsolete.
Finally, due to the current economic situation it is important to underline the low cost of minimally invasive osteosynthesis using KN. This is so in terms of the direct cost of osteosynthesis material, as well as in connection with the savings in operating theatre resource consumption, staff and beds for hospitalisation. Given the frequency of forearm fractures, it is necessary to take into consideration the advantages in terms of cost-effectiveness that this technique offers.
ConclusionsPO is a reproducible technique with major advantages that should be taken into account when it is properly indicated in diaphyseal forearm fractures.
This method is particularly useful in patients with multiple trauma and fractures because of its special characteristics: it is a simple technique that is fast to execute, with minimum harm to soft tissues and an almost insignificant risk of infection.
The results of this series of 64 patients with diaphyseal forearm fractures treated by intermedullary osteosynthesis with KN indicate that this treatment has several advantages: it causes few complications, reduces the duration of hospitalisation and the consumption of resources, and when a proper technique is used it achieves functional results that are similar to those of other osteosynthesis systems.
Thus the PO technique for diaphyseal forearm fractures in adults using KN, when it is properly indicated and executed, is a totally valid alternative that should be considered to be another equally good option for treatment.
Level of evidenceLevel of evidence III.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Fernández-Marín MR, Hidalgo-Pérez M, Arias-Rodríguez G, García-Mendoza A, Prada-Chamorro E, Domecq-Fernández de Bobadilla G. Fracturas diafisarias de antebrazo, 20 años después. ¿Está indicada la osteosíntesis percutánea? Rev Esp Cir Ortop Traumatol. 2018;62:112–120.