Herbert type B1 and B2 scaphoid fractures can be treated by orthopaedic treatment or surgery. The aim of this study is to analyse results and complications of scaphoid waist fractures treated using the percutaneous volar approach.
Material and methodWe present a retrospective study of 92 patients, treated in our institution from 2006 to 2016 using a volar percutaneous fixation. Mean Follow-up was 16 months (range 12–48). Injuries were classified using Hebert's classification, including B1 and B2 fracture types; the other fracture types following this classification system were excluded. Polytrauma patients, dorsal approach, fractures associated with distal radius injuries, patients treated using another surgical technique and patients with non follow-up were also excluded. Functional results were evaluated using the DASH questionnaire. Consolidation was established as the presence of bony bridges crossing the fracture site on X-rays, associated with absence of pain.
ResultsThe average time to fracture healing was 6.6 weeks (range 5–11). After 12 months of follow-up, the average wrist range of motion was 70° of extension (range 58–75) and 70° of flexion (range 62–80). Regarding functional evaluation, the average DASH questionnaire score was 42. The most frequent complication was non-union in 4 cases (4.44%). Average surgical time was 25min.
ConclusionsVolar percutaneous fixation is a simple and quick technique for a specialist surgeon, characterised by low morbidity and complication rates compared to ORIF and orthopaedic treatment, which accelerates the patient's functional recovery.
Las fracturas de escafoides Herbet tipo B1 y B2 se pueden tratar tanto de manera ortopédica con inmovilización como de manera quirúrgica. El objetivo de este estudio es analizar los resultados clinicofuncionales y las complicaciones de las fracturas de escafoides tratadas con fijación percutánea mediante abordaje volar.
Material y métodoEstudio retrospectivo de 92 pacientes, tratados en nuestro centro, entre 2006 y 2016, mediante fijación percutánea volar. Seguimiento medio de 16 meses (rango 12-48). La clasificación de las fracturas se realizó según la clasificación de Herbert, incluyendo los tipos de fractura B1 y B2. El resto de los tipos fueron excluidos. Se excluyeron a los pacientes politraumatizados y los abordajes dorsales, las fracturas asociadas a fracturas de radio y a los pacientes sin seguimiento. Los resultados funcionales se evaluaron utilizando el cuestionario DASH. El criterio de consolidación se estableció con ausencia de dolor en el examen físico y presencia de consolidación en las proyecciones radiográficas.
ResultadosEl tiempo medio para la consolidación fue de 6,6 semanas (rango 5-11). A los 12 meses de seguimiento, el rango promedio de movimiento fue 65° de extensión (rango 58-75) y 75° de flexión (rango 72-80). Obtuvimos una media de 42 puntos según el cuestionario DASH. La complicación más frecuente fue la seudoartrosis en 4 casos (4,4%). El tiempo de cirugía medio fue de 25 min.
ConclusionesLa fijación percutánea volar es una técnica simple y rápida para un cirujano especializado, caracterizada por bajas tasas de morbilidad y complicaciones, en comparación con otras técnicas. Permite acortar el tiempo de convalecencia y acelera la recuperación funcional del paciente, aparte de ser coste-efectiva.
Scaphoid fractures are the most common carpal fracture and account for almost 60% of all of them.1 The incidence of these fractures varies depending on the references that are consulted, from 22 to 141 per 100,000 individuals per year in the European population.1–5
In spite of their frequent occurrence, these fractures are always a challenge for diagnosis as well as treatment. Early diagnosis and appropriate treatment are necessary to prevent kinetic alterations in the wrist, together with the feared early onset arthritis that is associated with incorrect consolidations or pseudoarthritis.6–9
The aim of this study is to analyse our clinical-functional results in the treatment of Herbert B1-B2 carpal scaphoid fractures using percutaneous surgery with a volar percutaneous approach, as well as to evaluate the radiological and functional results of the same 12 months after surgery. All of this forms the basis of a preliminary study.10
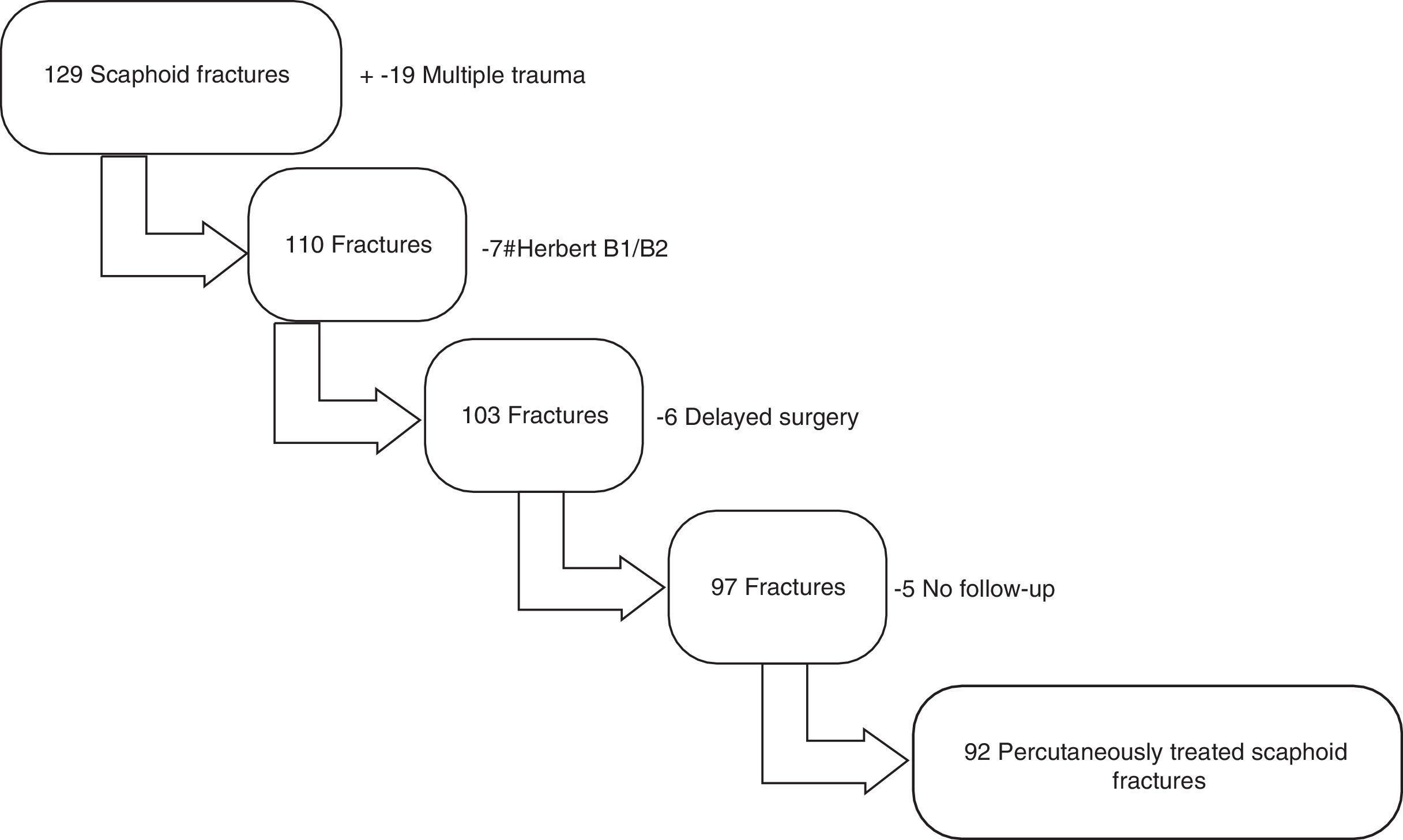
Material and methodA retrospective study was undertaken of a total of 129 consecutive cases of carpal scaphoid fractures treated in our hospital. The study covers the period from January 2006 to January 2016. A series of inclusion criteria were established: fractures that occurred from 2006 to 2016, B1-B2 type fractures according to Herbert's classification, i.e., transverse or short oblique fractures, ones treated using percutaneous volar surgery, and lastly treatment of the fracture within the first 12 days. Exclusion criteria were also set: any other type of fracture classification, fractures associated with fractures of the distal third of the radius, ones treated using any other kind of approach, patients with multiple trauma and lastly, those who were not followed up or when this took place earlier than 12 months, or when they were followed-up in other hospitals.
Of the 129 cases, 19 patients had multiple trauma and 7 had types of fracture other than the B1-B2 types in Herbert's classification, and in 6 cases treatment occurred after the 12 day limit. In 5 cases the requisite follow-up was lacking. This left 92 cases of scaphoid fracture in 92 patients (Fig. 1).
Demographic data were recorded, together with the injury mechanism, associated lesions and postoperative complications in the final group of patients. Of the 92 patients, 80 were men and 12 were women, with an average age of almost 27 years old. The B1 type of fracture was the most frequent, at 63 cases, as opposed to 29 B2 fractures. The average follow-up in our sample was 16 months, with a range of from 12 to 48 months.
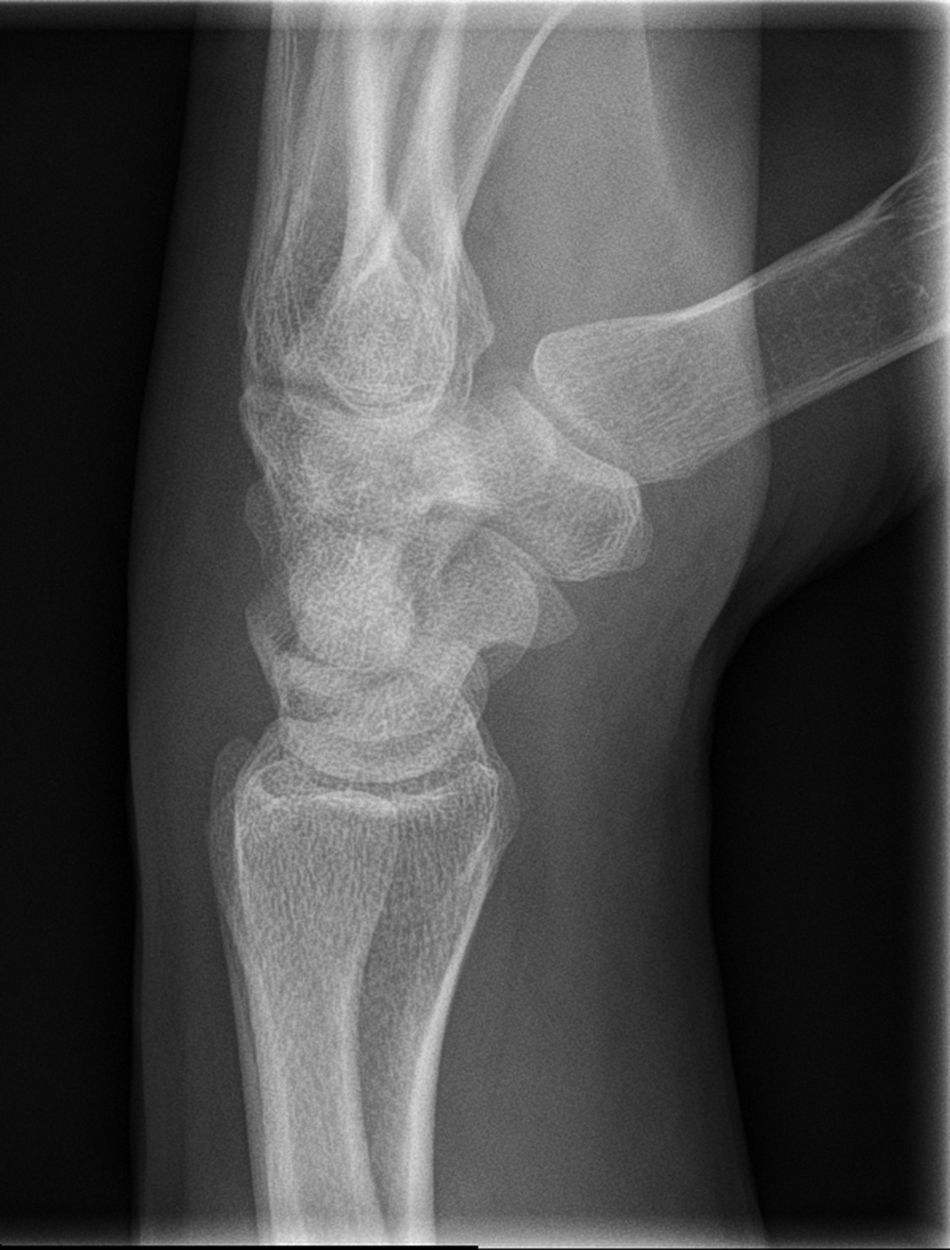
Protocol for action in carpal scaphoid fracturesApart from physical examination, when there is the suspicion of carpal scaphoid fracture a series of radiological images are firstly used for diagnosis: posteroanterior, posteroanterior with cubital deviation and pure lateral (Figs. 2–4).
Only surgeons specialised in this technique performed this procedure. Osteosynthesis is carried out according to the technique described by Cecilia-López et al.10 Once the patient is in the operating theatre and apart from the usual radiological images for this fracture, an oblique image is taken with the wrist in pronation.11 This gives a more accurate image of the whole bone.
With the patient in supine decubitus his upper arm is extended with the forearm in supination on a hand table. The tuberculus of the scaphoid is marked and the wrist is slightly extended in cubital deviation to facilitate the process.
It is true that when performed by expert surgeons, percutaneous scaphoid fracture surgery may only last a few minutes. Nevertheless, and even in expert hands these operations may last for longer. Suitable implantation of the guide needle is of fundamental importance in preventing such prolongation. The surgeon must be sure to have properly located all of the images before implantation of the needle, as failures in implantation will perforate the bone and hinder surgery. This will not only shorten the time taken for surgery, but will also prevent one of the most feared complications, pseudoarthrosis.
The implantation of the first needle is often not definitive. It is therefore possible to use it as a guide for the implantation of a second needle, although it cannot be used to apply traction as it is incapable of transmitting the necessary force. In our experience it is better to remove the first needle before drilling to prevent it from breaking. This may cause discomfort to the patient and even lead to future migrations of the same that would require a second surgical operation.
Once the guide needle has been implanted in the correct position, only the distal fragment of the fracture should be drilled to prevent the traction forces that would arise. In this case the selected implant should be a screw with 3 properties: it should be cannulated, compress the fragments together and be in an appropriate position, i.e., in the centre of all of the images taken (Figs. 5–7).
The patient is discharged on the same day with a bandage, and is able to use the hand for normal everyday life activities that do not require strength. The suture is removed in the first visit (after 2 weeks) and the patient is referred to rehabilitation. X-ray check-ups take place at 1, 3, 6 and 12 months (Fig. 8).
Clinical and radiological evaluation are carried out on an out-patient basis. Functional results are evaluated used the DASH questionnaire translated into Spanish.12 The consolidation criterion is established as the presence of bone bridges that cross the fracture site in all X-ray images, and this is associated with the absence of pain when pressure is applied in the physical examination.
Statistical analysisA descriptive analysis was performed of each variable. Version 14.0 of the STATA system (StataCorp.) was used in the statistical analysis. P<.05 was taken as the level of statistical significance.
ResultsThe average time to surgery was 4.26 days, with a range of from 1 to 12 days. No statistically significant association was found between time to surgery and the development or not of pseudoarthritis in those patients who did or did not develop this condition (P>.05).
Nor was the development of pseudoarthritis associated with the type of high energy mechanism (motorcycles and vehicles) (P>.05), and this was also the case for sex and age (P>.05).
Consolidation was defined as the presence of bone bridges that cross the centre of the fracture in X-ray images, as well as the absence of pain when pressure was applied to the centre of the fracture. The average time taken for consolidation was 6.6 weeks, with a range of from 5 to 11 weeks.
Mobility was evaluated in all of the patients 12 months after the date of fracture. An average range of movement was found of 65° in extension (range 58-75) and 75° in flexion (range 72–80). The subjective sensations o the patients were excellent in all of the cases in which consolidation had been achieved, with ranges of movement that were practically indistinguishable between both arms. No case of medial-carpal instability was reported, and grasping power could not be distinguished from that of the other hand.
Functional evaluation used the DASH questionnaire translated into Spanish,12 with an average score of 42 points.
Complications were divided into those that occurred during the operation and those that arose over the long term. The intraoperative complications were 2 cases of breakage of the guide needle (2.17%), without any vascular or nerve lesion. 9 complication arose over the long term: 5 extractions of material (5.43%) due to discomfort in the osteosynthesis material, and 4 cases of pseudoarthrosis (4.34%). In all they represent less than 10% of the sample. OF the 4 cases of pseudoarthrosis, only one was symptomatic and required a repeat operation in which a new osteosynthesis was created using a graft from the iliac crest.
The average duration of surgery was 25min, with a very broad range from 10 to 75min.
DiscussionVan Tassel et al., using the National Electronic Injury Surveillance System Database, obtained a far lower incidence of 1.47 cases per 100,000 individuals per year.13 In spite of the differences in incidence, the majority of papers agree that these fractures are typical of young people and are more prevalent in men.2,5,13,14
When fractures of this type have no or minimal displacement they always lead to debate on their management and treatment.15–17 All types of treatment, orthopaedic with plaster or surgery, open reduction and internal or percutaneous fixation, have their advantages and disadvantages.
The advance in the technological development of implants has largely reduced the complication deriving from surgery.18,19 The greatest advance, apart from the ease arising from the availability of cannulated screws, is the interfragmentary compression that aids better consolidation of the fracture.
Treatment by percutaneous approach and osteosynthesis under compression with a screw has been widely proven to make fractures more stable than closed plaster. It also accelerates recovery and allows patients to return to work far sooner than is the case with orthopaedic treatment. Nevertheless, the complications associated with surgery should not be forgotten.
All of our patients are routinely referred to rehabilitation to prevent rigidity developing due to the lack of mobility associated with postoperative pain. Even so, very few patients undergo suitable rehabilitation, due either to their own decision or a delay in their appointment due to overloading of the rehabilitation departments.
It is true that in 2 of the 4 cases of pseudoarthrosis the implanted screw was not in the ideal position, i.e., in the centre of the scaphoid bone in all radiological images. However, in the other 2 cases we could detect no error in the implant, and this leads us to think that the cause of the lack of consolidation is due to involvement of the vascularisation when the fracture occurred.
On the other hand, arthroscopy is a very valid alternative when treating fractures of this type together with percutaneous surgery, as it offers us a series of advantages: direct visualisation of the fracture, of the screw entry point and the compression it creates in the osteosynthesis material, as well as its correct positioning. It also makes it possible to evaluate any associated lesions. On the other hand, it prolongs the duration of surgery and requires experienced personnel to perform it properly.
Lastly, as has been proven,20,21 treatment using percutaneous surgery with a volar approach is clearly cost-effective. And not only this, because as functional recovery is faster less time is spent off work. It avoids the complications associated with immobilisation that are associated with orthopaedic treatment. It also causes less damage to the soft tissues than open reduction and internal fixation.
ConclusionThe percutaneous synthesis of Herbert type B1/B2 scaphoid fractures is a beneficial treatment for patients in terms of functional recovery. In the hands of specialists this technique is fast and simple, giving excellent clinical and radiological results. Few complications arise and the majority of those that do are not important.
Ethical responsibilitiesNone.
Level of evidenceLevel of evidence IV.
Conflict of interestsThe authors state that there's no conflict of interests or funding to declare and are sure that this statement doesn’t influence the editorial board, as the final decision will be based on the intrinsic value that the article represents for the readers.
Please cite this article as: Luengo Alonso G, Jiménez Díaz V, Garcia Lamas L, Porras Moreno MA, Cecilia López D. Fracturas de escafoides tratadas con técnica percutánea volar. Análisis y resultados de 92 casos. Rev Esp Cir Ortop Traumatol. 2018;62:105–111.