To determine if the thickness of the transverse carpal ligament measured by T2 axial magnetic resonance imaging actually influences the onset of carpal tunnel syndrome.
Material and method94 patients between January 2015 and June 2016, of whom 28 had carpal tunnel syndrome, underwent magnetic resonance imaging, 37 with discomfort in different carpus regions without symptoms of carpal tunnel and 29 healthy subjects. Two observers performed 3 measurements in 3 different levels, and in the 3 groups of patients.
ResultsNo statistically significant differences in transverse carpal ligament thickness measurements between the carpal tunnel syndrome group and the group without carpal tunnel involvement became apparent, but statistical differences between the control group and the carpal tunnel syndrome group, and between the control group and the group without involvement of the carpal tunnel were observed. In both these groups, the thickness of the transverse ligament was higher than in the control group.
DiscussionAn increase in the thickness of the transverse ligament in was found in this study in subjects with involvement of carpal tunnel syndrome as evidenced by numerous studies in the literature. There is no certain causative factor, but rather a set of facts that make onset of the syndrome possible in a specific group of patients.
ConclusionCarpal tunnel syndrome is multifactorial. The thickness of the transverse ligament does not directly affect the onset of symptoms.
Determinar si el espesor del ligamento transverso del carpo medido en el corte axial T2 en resonancia magnética influye realmente en la aparición del síndrome del túnel carpiano.
Material y métodoSe realizó resonancia magnética de la región de la muñeca a 94 pacientes entre enero del 2015 y junio del 2016, de los cuales 28 presentaban síndrome del túnel carpiano, 37 con molestias en diferentes regiones del carpo, sin síntomas de túnel carpiano y 29 sujetos sanos. Dos observadores realizaron 3 medidas en 3 niveles diferentes y en los 3 grupos de pacientes.
ResultadosNo se evidenciaron diferencias estadísticamente significativas en las medidas del espesor del ligamento transverso del carpo entre el grupo de síndrome del túnel carpiano y el grupo sin afectación del túnel, pero sí hubo diferencias estadísticas entre el grupo control y el grupo afecto de síndrome del túnel carpiano y entre grupo control y grupo sin afectación del túnel carpiano. En estos dos grupos, el espesor del ligamento transverso fue mayor al grupo control.
DiscusiónEn este estudio se evidencia un aumento del ligamento transverso en sujetos con afectación de síndrome del túnel carpiano como demuestran numerosos estudios de la literatura, pero no existe un factor causal determinado sino un conjunto de hechos que hacen posible la aparición de dicho síndrome en un determinado grupo de pacientes.
ConclusiónEl síndrome del túnel carpiano es multifactorial, sin intervenir directamente el espesor del ligamento trasverso en la aparición de los síntomas.
The carpal tunnel is a fibre-bone channel in the volar part of the carpal bone. It is composed of the carpal bones, while the bottom of the tunnel consists of the transverse ligament. This ligament band is 3–4cm wide1 and from 0.8 to 2.5mm thick,2 in a range from 1.3 to 3mm depending on the point at which it is measured.
The carpal tunnel syndrome (CTS) is the most frequent neuropathy of the peripheral nerve. It is caused by compression of the median nerve in the wrist3 against the carpal transverse ligament, which swells.4 It is particularly common in middle-aged women3 and in people who are in work, although a clear cause in its etiopathology has yet to be ascertained.
In the majority of cases it is idiopathic, although it may occur in cases of systemic disease or conditions (rheumatoid arthritis, diabetes, pregnancy, etc.). It may also be secondary to lesions that occupy space: ganglions, fibromas, lipomas, osteophytes and gout tophi.3 On other occasions it is secondary to injury, and it is associated with hard manual labour.5
The most significant symptom is tingling in the area of the carpus and fingers.6
There is a lack of agreement in the different publications on the definition of the transverse carpal ligament (TCL) and the flexor retinaculum, as both terms refer to the same thing. We have chosen the description by the authors Paceck and Manley7,8 for our work. According to them the flexor retinaculum refers to a volar fascial plane that is under the palm fascia and which is comprised of 3 parts: (a) proximal, the continuation of the antebrachial fascia; (b) medial, corresponding to the TCL itself, which is thicker than the first part with 4 connections to bones, the trapezium, scaphoid tubercle, the pisiform bone and the hook of the hamate bone, and (c) distal, corresponding to the aponeurosis between the thenar and hypothenar musculature.7,8
The aim of this study is to evaluate the influence of the thickness of the transverse ligament in the appearance of carpal tunnel syndrome. This is due to the existence of certain disagreements that have arisen between the traumatologists and radiologists in our hospital.
Material and methodStudy design: a prospective and descriptive study of a series of patients undertaken from January 2015 to June 2016. It was approved by the Ethics Committee of the institution.
Patients: 94 patients were included and classified in three groups. 28 had the typical clinical symptoms of CTS (group A), 37 had discomfort in different parts of the carpus without carpal tunnel syndrome symptoms (group B) and 29 were healthy subjects (group C). All of the patients in the study signed their informed consent so that they could be included in it.
Patients who had been operated for any reason in the carpus were excluded, as were those with a history of distal radiocubital joint fracture or carpus fracture, patients with rheumatoid arthritis, diabetes mellitus, those who were pregnant and those who due to movement or lack of cooperation could not give reliable ligament measurements.
Imaging studies: all studies took place using magnetic resonance imaging technique (MRI) with a Toshiba 0.35 T with a specific antenna for the carpus. Patients were supine and with their hand parallel to the body in a neutral position, according to the following protocol: coronal T2*, coronal T1 3D spin echo, axial spin echo T1, axial spin echo T2* and sagital spin echo T1, although measurements were taken in the axial spin echo T2* sequence, according to the following protocol: TR 777; TE 20; FA 30; FOV 10; ST 4; Mx 208×256; NA 2.
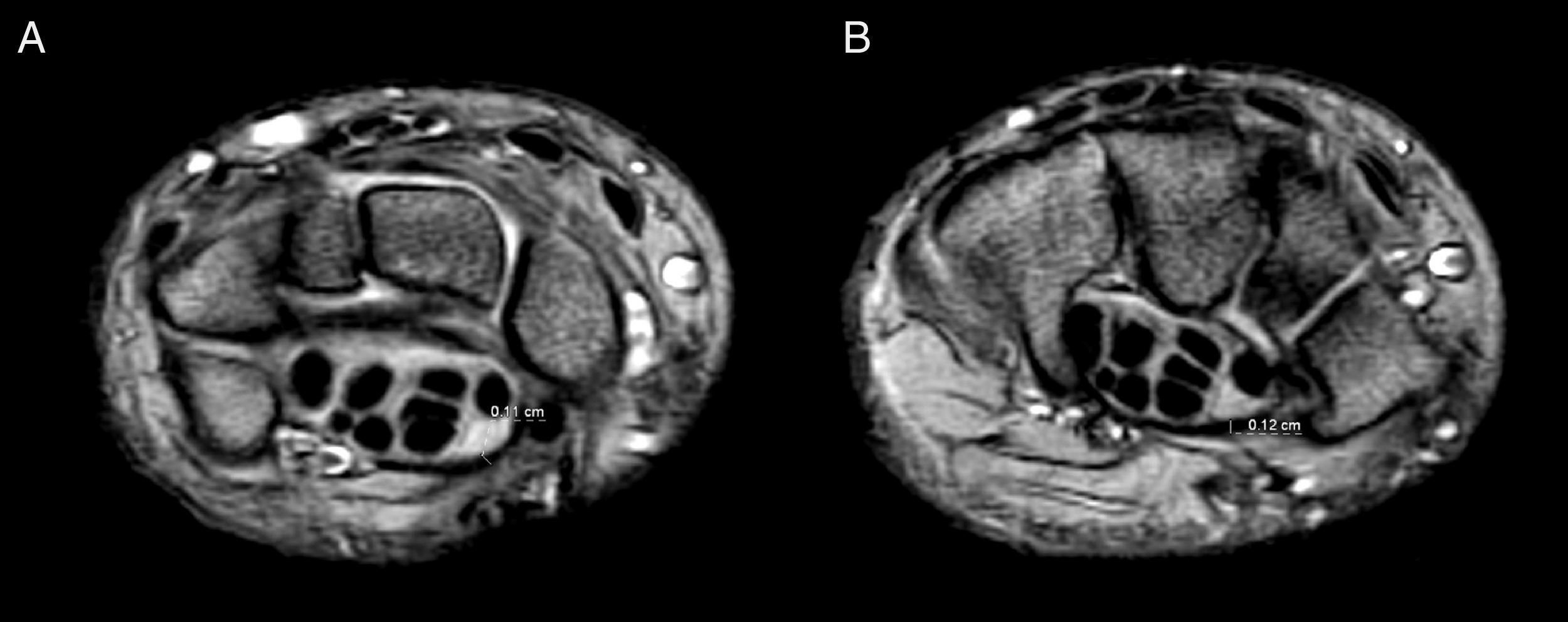
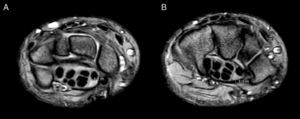
Imaging studies analysis: two radiologists with broad experience in the musculoskeletal system measured the TCL using MRI in the axial T2* sequence, at 3 preset levels:
- -
At the level of the first line of the carpus where the pisiform bone appears and as close as possible to the median nerve.
- -
At the level of the second line of the carpus at the height of the hamate bone and also as close as possible to the nerve.
- -
At the level of the base of the metacarpal bones, in the closest area to the median nerve (Fig. 1).
Data analysis: V20.0 of the SPSS® (SPSS Inc., Chicago, IL, USA) program for Windows was used for the statistical study. Quantitative variables were described as averages with their typical variation, while qualitative variables were described in terms of frequency and percentage. Distribution normality analysis was undertaken using the Kolmogorov–Smirnov test, and the Kruskal–Wallis and Mann–Whitney U tests were used for comparisons due to a non-normal distribution of study variables. The reliability of measurements by both observers was measured using the intraclass correlation index (ICC).
Statistically significant results were defined as those with a value of P<.05.
ResultsA total of 94 patients were divided into 3 groups according to their symptoms: 28 in group A (29.8%), 37 in group B (39.4%) and 29 in group C (30.9%).
42 patients were men (44.7%) and 52 were women (55.3%): in group A there were 8 men (28.6%) and 20 women (71.4%), in group B there were 24 men (64.9%) and 13 women (35.1%), while in group C there were 10 men (34.5%) and 19 women (65.5%).
The average age of the subjects in the study was 39.91 years old (±9.137 years old), ranging from 36 years old (22–58 years old). In group A the average age was 41.36 years old (±7.737 years old), in group B it was 38.11 years old (±8.959 years old) and in control group C it was 40.86 years old (±10.491).
71 right hands were studied (75.5%) together with 23 left hands (24.5%). In group A there were 21 right hands (75%) and 7 left hands (25%), in group B there were 25 right hands (67.6%) and 12 left hands (32.4%) while in group C there were 26 right hands (89.6%) and 3 left hands (10.4%).
The dominant hand was studied in 71 cases (75.5%) vs 23 (24.5%) non-dominant hands. The ratio in each group was as follows; in group A there were 20 dominant hands (71.4%) and 8 (28.6%) non-dominant ones, in group B there were 22 (59.5%) dominant hands and 15 (40.5%) non-dominant ones, and in group C the dominant hand of all of the subjects was studied (100%).
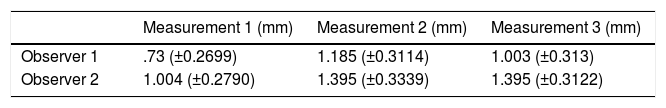
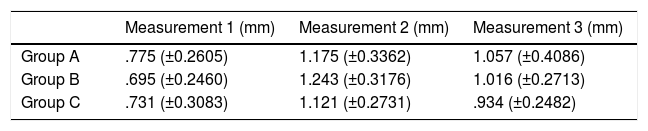
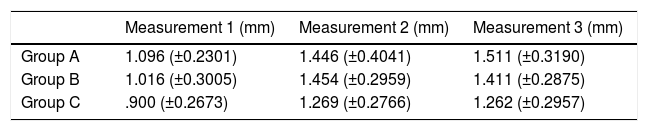
The 3 measurements of ligament thickness by observer 1 and observer 2 are shown in Table 1. The differences between the average thicknesses measured by both observers in all 3 study groups (A, B and C) and at the 3 different levels are shown in Tables 2 and 3.
Average size of the ligament in millimetres (mm) in the three measurements carried out by both observers in the set of all of the patients in the study.
| Measurement 1 (mm) | Measurement 2 (mm) | Measurement 3 (mm) | |
|---|---|---|---|
| Observer 1 | .73 (±0.2699) | 1.185 (±0.3114) | 1.003 (±0.313) |
| Observer 2 | 1.004 (±0.2790) | 1.395 (±0.3339) | 1.395 (±0.3122) |
Average size of the ligament (mm) in the measurements by observer 1 of the three groups studied.
| Measurement 1 (mm) | Measurement 2 (mm) | Measurement 3 (mm) | |
|---|---|---|---|
| Group A | .775 (±0.2605) | 1.175 (±0.3362) | 1.057 (±0.4086) |
| Group B | .695 (±0.2460) | 1.243 (±0.3176) | 1.016 (±0.2713) |
| Group C | .731 (±0.3083) | 1.121 (±0.2731) | .934 (±0.2482) |
Average size of the ligament (mm) in the measurements by observer 2 of the three groups studied.
| Measurement 1 (mm) | Measurement 2 (mm) | Measurement 3 (mm) | |
|---|---|---|---|
| Group A | 1.096 (±0.2301) | 1.446 (±0.4041) | 1.511 (±0.3190) |
| Group B | 1.016 (±0.3005) | 1.454 (±0.2959) | 1.411 (±0.2875) |
| Group C | .900 (±0.2673) | 1.269 (±0.2766) | 1.262 (±0.2957) |
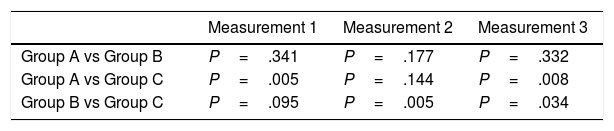
The Kruskal–Wallis test was used to study the differences between the 3 groups studied and at the 3 levels measured by both observers. Statistically significant results were found for the 3 measurements in the 3 groups, in the 1st (P=.027), the 2nd (P=.017) and the 3rd (P=.018) measurements only for observer 2. The comparison between the groups and the 3 measurements by this observer was undertaken using the Mann–Whitney U test (Table 4).
It was found that the 2nd and 3rd measurements by observer 2 are clearly higher than the 1st measurement in all of the groups studied.
For observer 2 in the statistical comparison between the groups it was found that measurement 1 in group A compared to group C (at the first line of the carpus) and measurement 3 (at the base of the metacarpals) were higher and statistically significant (P=.005 and P=.008, respectively).
For groups B and C and for observer 2 a significant increase in ligament size was found in measurements 2 and 3 (P=.005 and P=.034, respectively).
The differences between the measurements of the observers in dominant hands were studied using the Mann–Whitney U test, and no statistically significant results were found.
When checking the differences between measurements, their reliability was studied using the ICC between the observers. The resulting values were 0.285 for measurement 1, 0.478 for measurement 2 and 0.183 for measurement 3.
DiscussionThis study attempted to detect whether the thickness of the TCL is greater in the group of subjects with carpal tunnel syndrome than it is in the other two groups, and to find which one of the 3 measurements has the greatest influence on the appearance of the clinical symptoms.
It was confirmed that transverse carpal ligament thickness has no direct influence on the appearance of CTS symptoms, as in group A the TCL was found to be thicker in the 2nd and 3rd measurements than it was in the healthy subjects, while in group B it was thicker in measurements 2 and 3 compared to the group of healthy subjects.
Thus in both groups, A and B, the TCL is thicker while it is not in the healthy subjects, so that it can be deduced that this is not the cause of this important syndrome.
MRI studies were performed of the carpal tunnel in the 1980s. These evaluated the thickening of the flexors tendons, the area and thickening of the median nerve, the anatomical variations within the tunnel with persistence of the median artery, and the presence of accessory muscles, in an attempt to discover the cause of the CTS.5 John et al. observed hypertrophy of the transverse carpal ligament and suggested that this may contribute to the CTS, but no subsequent studies have supported this theory.9
In 2006 Bower et al. used MRI to study the carpal tunnel in a group of CTS patients and a control group. They found an increase in pressure within the tunnel as the carpus had increased in length, with a reduction in tunnel area in women.10 In 2015 Liao et al. continued this line of research and also found an increase in tunnel pressure and a more than 30% increase in the length of the carpus.5
In 2012 Shen et al.,11 studied the thickness of the TCL using ultrasound scan in cadavers and a control group. They found higher values in the cadavers, and it is interesting that they found ultrasound scan to be a valid diagnostic technique for measuring ligament thickness. The ICC among the 3 observers who took part in this study is far higher than emerged in our series, and this is so even when three are major difficulties when using ultrasound scan in differentiating the transverse carpal ligament itself from the surrounding structures.
As is shown in the literature and in our series of cases, in spite of all of the variables studied over recent years to seek a relationship with the CTS, no single causal factor has been found. Rather than this, a set of factors have been found that make the appearance of the said syndrome possible in a certain group of patients.
The thickness of the transverse ligament did not influence the appearance of CTS in our study. It only influenced the appearance of painful symptoms in the carpus, and this was more frequent in women and was always in the dominant hand.
The limitations of this study may be clearly associated with several causes; firstly there is the difficulty of establishing a specific point for measurement. This is because the ligament is approximately 4cm wide, while the closest zone to the median nerve may measure about 2cm. Due to this the possibility of having measured at the same point and at the different levels is remote. Secondly, the measurements were made using different monitors, although the PACS system was the same. There is a dispersion bias that is not inconsiderable in the data obtained.
It is probable that greater agreement between the observers could have been attained regarding our hypothesis of the influence of the transverse carpal ligament on the genesis of CTS if the measurements had used the same monitors, and if they had been in a more specific location.
ConclusionsThis work shows that although the thickness of the transverse carpal ligament does not directly influence the symptoms of the CTS, it does influence the appearance of painful symptoms in the carpus. CTS is probably a multifactorial syndrome in which the repetitive movements involved in certain everyday life activities may contribute to its emergence.
Level of evidenceLevel of evidence IV.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank Lorena López Bofill and Elena Martínez Arribas for their help in searching for data in clinical histories, together with Ana Leiva Aguilera, the document manager in our hospital, for her help in searching the bibliography, and Andrea Peris Bartolomé for the transcription and supervision of the article.
Please cite this article as: Bartolomé-Villar A, Pastor-Valero T, Fuentes-Sanz A, Varillas-Delgado D, García-de Lucas F. Influencia del espesor del ligamento transverso del carpo en el síndrome del túnel carpiano. Rev Esp Cir Ortop Traumatol. 2018;62:100–104.