the main purpose of this study is to determine the agreement between two radiological tests, ultrasonography and magnetic resonance, in the diagnosis of distal brachial biceps tendon injury.
Material and methodA retrospective study was made of patients over 3 years who underwent distal brachial biceps tendon reattachment open surgery, and whose preoperative diagnosis was complemented either by ultrasonography, by magnetic resonance or both. The agreement was calculated by Cohen’s kappa coefficient (k).
Resultsinformation of 79 patients was analyzed. The concordance was excellent between resonance and surgical findings (k=.950), and a good Cohen´s kappa coefficient was also achieved between both ultrasonography and surgery (k=.706) and between information of sonography and magnetic resonance (k=0.667).
ConclusionsResonance and ultrasonography could be considered reliable diagnostic tests to determine the acute rupture of the distal brachial biceps tendon in patients with consistent aetiology and physical examination.
el objetivo fundamental de este estudio es determinar la concordancia entre dos pruebas radiológicas, la ecografía y la resonancia magnética, para el diagnóstico de rotura del tendón distal del bíceps braquial.
Material y métodose realizó un estudio retrospectivo de pacientes a lo largo de 3 años a los que se realizó cirugía abierta de reanclaje de tendón distal de bíceps y cuyo diagnóstico preoperatorio se complementó con ecografía, con resonancia magnética o bien con ambas. Se calculó la concordancia mediante el coeficiente kappa de Cohen (k).
Resultadosse analizaron datos de 79 pacientes. La concordancia fue excelente entre resonancia y hallazgos quirúrgicos k=0,950, y se obtuvo un índice de concordancia bueno tanto entre ecografía y cirugía k=0,706 como entre ecografía y resonancia magnética k=0,667.
Conclusionestanto resonancia como ecografía se podrían considerar técnicas diagnósticas fiables para la determinación preoperatoria de rotura aguda del tendón distal del bíceps braquial en pacientes con mecanismo y clínica congruentes.
Partial or total rupture of the distal brachial biceps tendon (DBT) does not lead to severe inability to carry out basic daily life activities but it does lead to functional impairment with regards to strength for flexion and supination of the forearm, which are necessary for performing demanding manual tasks and certain sports that require a fully functioning of the affected upper limb.1
The rate of DBT injuries is low, and it has been estimated that there are 1.2–2.5/100,000 inhabitants/year.2,3 They usually occur in two types of different population groups: in young sportspeople who carry out eccentric forced contraction of the biceps, generally due to overburdening the forearm in flexion and supination and in middle-aged patients, who are sportspeople and blue collar workers where repetitive force is used with the elbow in flexion that leads to progressive tendon degeneration in the insertion of the bicipital tuberosity of the radius,3,4 that finally leads to its rupture, normally after sudden contraction.
Until a few years ago there were scarcely any publications on the diagnosis and treatment of these injuries, but greater attention has been paid lately to the development and improvement of diagnostic methods such as ultrasonography (USG) and magnetic resonance (MR),5–10 and new surgical and conservative treatment options.11–14
MR has traditionally been considered the gold standard in radiologic diagnosis of tendon pathology in other anatomical locations. However, several studies equate MR and USG with regard to its reliability for the detection of findings suggestive of tendon injuries.15,16
It is important to be able to make a fast, accurate diagnosis for scheduling surgery and for prognosis, to improve treatment results and minimize the financial loss of sick leave and disability for the patient who wishes to retrieve their previous level of activity in the shortest possible time.17
USG is largely available in hospital emergency services but access to MR is more expensive and complicated in many centres, and if diagnosis depends on this test, the procedure becomes more expensive whilst treatment and clinical recovery is delayed.
The main aim of this study is to determine the (kappa) index of agreement between two radiologic tests, the USG and MR, for the diagnosis of DBT rupture. The possibility of the USG being a reliable preoperative test would mean that the diagnosis and treatment of these injuries could be carried out earlier.
Material and methodA descriptive retrospective study of agreement between USG and MR was conducted in the preoperative diagnosis of patients attended in our centre for 3 consecutive years for DBT injuries.
Following compatible anamnesis and physical examination, the study was complemented by performing USG or MR or both radiological examinations, depending on the case. Patients with a previous pathological process in the antecubital fossa were excluded from the study.
Information was collected by a single researcher, registering the diagnostic impression of the reports from imaging tests and the events described in the surgical protocol of each patient.
All the MR performed included images in axial, coronal and sagittal sectioning, and the report was made by the hospital radiology department where partial lesion, complete avulsion or whole distal insertion of the biceps brachii was reported.
Ultrasonographic examinations obtained images both in the short and long axis, and also dynamic exploration of the tendon during muscle contraction.
To consider the level of tendon compromise in the radiological tests, the classification proposed by Fuente et al.6 was taken, based in turn on the standard classification by Festa et al.18 and Le Huec et al.19 for MR findings:
Complete rupture: defined as the avulsion of the tendon of its tuberosity, total or partial of high grade (compromise >50% of insertion).
Partial rupture: defined as rupture of <50% of tendon thickness.
An expression of the agreement (kappa index) is proposed between:
- 1)
The surgical findings and those of the USG.
- 2)
The surgical findings and those of the MR.
- 3)
The interpretation of USG and MR images.
For each event the kappa index was calculated according to the following formula developed by Cohen20 to eliminate the possibility of agreement attributable to chance:
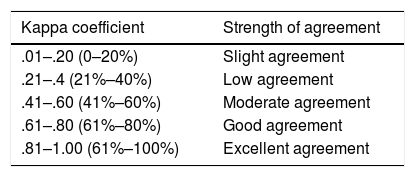
For the interpretation of the result, the kappa index obtained was classified, following the grading made by Landis and Koch (1977)21 contained in Table 1.
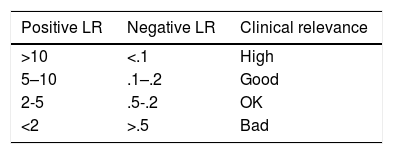
For greater external validity to the study and to increase reliability and the possibilities of reproducibility to extrapolate the obtained data to the rest of the population with suspected DBT rupture, the likelihood ratio was calculated (LR)22 (positive and negative) and the result was interpreted according to the scale described in Table 2.
According to this statistic, a test would be useful to confirm the injury the larger its positive LR, and on the other hand, the lower its negative LR, the higher its ability to detect healthy subjects, i.e. to rule out pathology.
As a general rule, it was considered that a positive LR higher than 10 and a negative LR below .1 would indicate a raised clinical relevance to bear in mind in the diagnosis for taking therapeutic decisions. For example, a positive LR of 10 means that it is 10 times more probable that a patient with a (partial or total) ruptured tendon would receive diagnosis of rupture (partial or total, whichever corresponds) than a patient who does not have it.
Assessment of the internal validity of the diagnostic tests studied were calculated using the corresponding creation of 2×2 contingency tables, for each case, the sensitive (S) values, specificity (SP), predictive positive value (PPV) and predictive negative value (PNV).
Statistical analysis was made with the support of free software from vassarstats.net, for the calculation of Cohen’s kappa agreement index, the exact Fisher test for measuring the degree of association between variables (p<.05 is considered statistically significant), the LR and the internal validity assessment measurements of the study.
ResultsThe sample obtained in this study comprised 79 patients who were operated on between 1st January 2015 and 31st December 2018 for DBT injury. Surgical findings determined that 13 of the total patients had partial ruptures and 66 had total ruptures. Preoperative diagnosis was made with USG on 58 of them, with MR on 68 and both preoperative tests were performed on 47 patients.
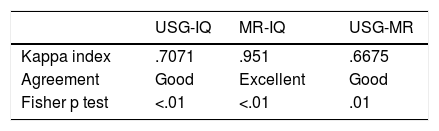
The kappa index was calculated for each case, obtaining an excellent agreement between the information described by the MR and the surgical findings (k=.950). The agreement index between the ultrasound and surgery was good (k=.706) and also between the USG and MR data (k=.667).
As may be noted in Table 3, in all compared assumptions, a high level of statistical significance was found (p≤.01).
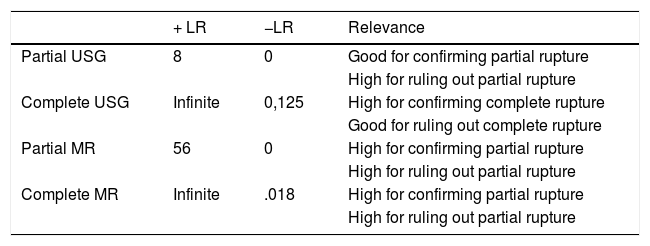
With regard to LR (positive and negative) calculated to extrapolate data obtained from the rest of the population, the results contained in Table 4 were obtained.
Calculation of likelihood ratios (LR).
| + LR | −LR | Relevance | |
|---|---|---|---|
| Partial USG | 8 | 0 | Good for confirming partial rupture |
| High for ruling out partial rupture | |||
| Complete USG | Infinite | 0,125 | High for confirming complete rupture |
| Good for ruling out complete rupture | |||
| Partial MR | 56 | 0 | High for confirming partial rupture |
| High for ruling out partial rupture | |||
| Complete MR | Infinite | .018 | High for confirming partial rupture |
| High for ruling out partial rupture |
Regarding partial rupture of the DBT, the USG (positive LR=8) is 8 times more probable to correctly inform of this lesion presented by the patient than not presented, whilst the MR (positive LR=55) is 55 times more probable than when it reports of partial rupture really being there, which implies a high clinical relevance to be very much taken into account for preoperative diagnosis.
When a patient has USG or MR, and either of these two tests report complete rupture of DBT, there is a very high clinical relevance, as both obtain a positive LR much higher than 10 (positive LR=infinite), and both also have a very low negative LR, which indicate their high ability to detect intact tendons when they really are. Both tests therefore offer great diagnostic security for ruling out complete rupture.
Both radiological tests have a high success rate when compared with the diagnostic impression described in the radiologist’s report with intraoperative findings, to the extent that the USG is in line with surgery in 89.7% of cases, whilst MR is in line with surgery in 98.5% of cases, both for partial and complete ruptures.
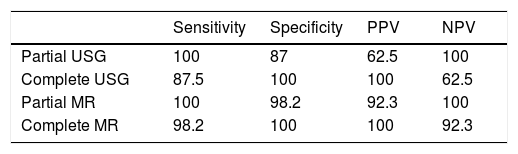
Regarding the detection of partial DBT lesion in our sample (Table 5), the USG was able to offer the right diagnosis in 10/16 patients, whilst the MR did this in 12/13 cases. Both the USG and the MR have a 100% sensitivity, but with greater specificity in the case of MR (SP=98.2%) than in the USG (SP=87.5%). Both have a negative predictive value of 100%, but the positive predictive value was higher in the case of the MR (PPV=92.3%) than in the USG (PPV=62.5%).
Results for the calculation of values both for ultrasound (partial or complete tendon lesions) and for magnetic resonance (partial or complete tendon lesions) expressed in percentage.
| Sensitivity | Specificity | PPV | NPV | |
|---|---|---|---|---|
| Partial USG | 100 | 87 | 62.5 | 100 |
| Complete USG | 87.5 | 100 | 100 | 62.5 |
| Partial MR | 100 | 98.2 | 92.3 | 100 |
| Complete MR | 98.2 | 100 | 100 | 92.3 |
Regarding the detection of the complete DBT lesion in our sample (Table 5), the USG was able to offer the right diagnosis in all cases that reported complete rupture, 42/42 cases, similarly to the MR which did this in 55/55 patients.
Both USG and MR have 100% specificity, but there is higher sensitivity for MR (S=98.2%) than for the USG (S=87.5%). Both have a positive predictive value of 100%, but with regard to the negative predictive value, the MR (NPV=92.3%) it is higher than that of USG (NPV=62.5%).
DiscussionIt is considered that the MR is an imaging test with a high correspondence to the true surgical findings for tendon injury in several anatomical locations,15,16 and also for lesions of the distal biceps tendon18,19 with the technological development and improvement in imaging acquisition, the USG is increasingly more popular for the diagnosis of this type of lesions,7,9 due to its easy access, high availability of emergency services and hospital consultations, the speed of examination, the possibility of establishing comparison with healthy limbs and dynamic exploratory manoeuvres and all of this at a low financial cost.
The aim of this study is to validate the USG and the MR as diagnostic methods of DBT rupture.
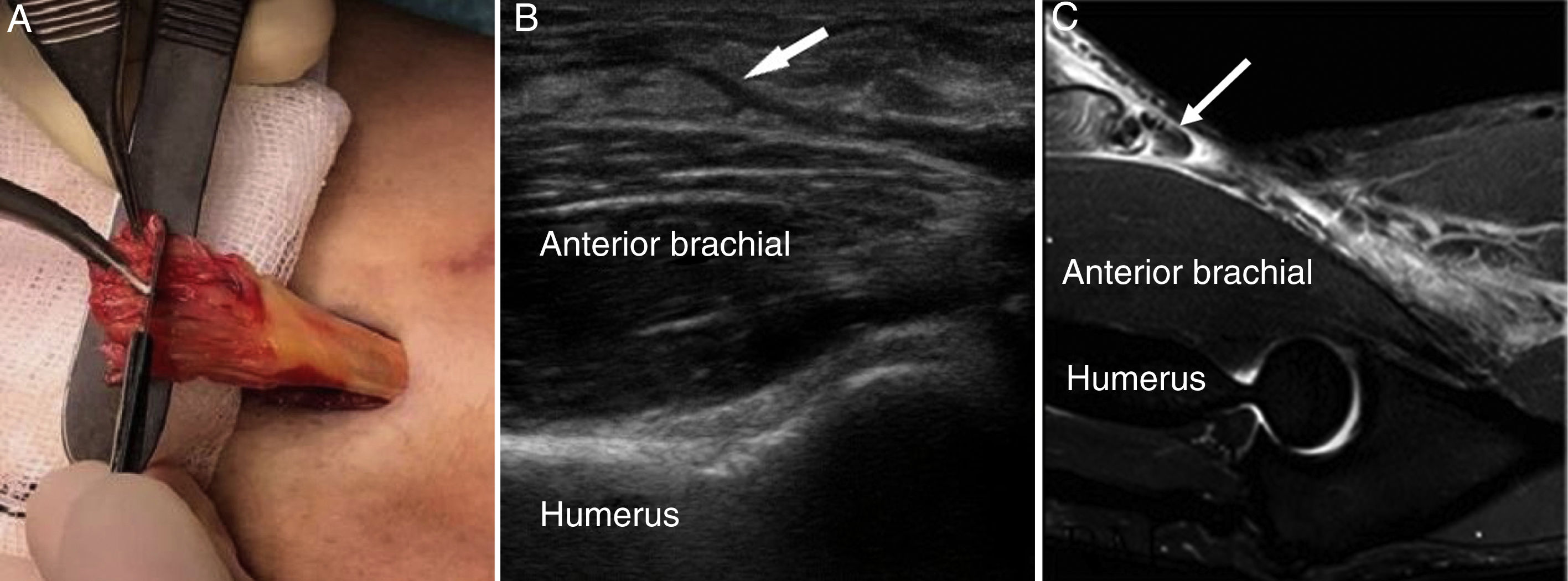
Fig. 1 shows the appearance of the complete rupture of the DBT. It may be observed that the tendon stump is located in both imaging tests.
The results obtained by the MR in this study coincide with those of the reviewed literature, showing an excellent agreement (k=.950) with the intraoperastive findings, describing the same type of tendon rupture in 95% of cases, whilst the USG does this in somewhat more than 70% of cases, which means there is good agreement, close to excellence (k=.706), and similar to the results published in the last 5 years.
Between both radiological tests there is also good correlation (k=.667), coinciding with the diagnosis of 41/47 cases. It is of note that 2 out of the 5 patients in whom there were discrepancies among them, the USG identified as partial a rupture which both the MR and intervention showed to be complete, without retraction and with maintenance of the peritenon intact. All the assumptions compared to calculate the kappa index showed a statistical significance level of p<.01, which implies a very raised association between the analysed variables.
From the results of our study it was found that the USG and MR have very high sensitivity and specificity for the diagnosis of DBT ruptures (partial and complete), and in all cases above 85% for the USG and above 98% for the MR, as described in the recent literature.6,7
If we look at the results obtained for partial ruptures, both USG and MR have a negative predictive value of 100%, which suggests that when any of these tests report that there is not a partial rupture, at least in our sample, this has always been confirmed as complete in surgery. When MR, with higher positive predictive value than USG reports partial rupture, this is confirmed during surgery in 92.3% cases, whilst with USG this is the case for 62.5%.
For complete ruptures, both tests have a positive predictive value of 100%, i.e. that in our sample when any of the two tests reported that the rupture was complete, it was always confirmed by surgery, but MR, with a higher predictive negative value (PNVC=92.3%), was able to better discriminate than USG (PNV=62.5%), similarly to what had occurred in the partial ruptures.
In our study, the USG obtained good clinical relevance for the detection of partial lesions (positive LR=8), and a much higher relevance (positive LR >10) for the detection of complete ruptures, equitable in this case to MR, where LR is much higher than 10 for both partial and complete ruptures. This implies great clinical relevance for the detection of these lesions of distal biceps. In this way, both diagnostic tests are considered reliable and will help with decision making for the treatment of patients with suspected DBT trauma injury.
One of the limitations of this study is that in some patients it is possible the same radiologist who had completed and reported the USG, without having taken the precaution to hide the result obtained in this preoperative test, had already performed MR as well. Since no data masking had taken place it is possible that interpretation of the results was biased. To resolve this in the future a prospective study could be designed with double blind masking for all the medical staff involved in the preoperative diagnoses of the patients.
Also, only data on operated cases was analysed, and there was therefore no availability of data relating to patients who had an elbow USG and/or MR and who did not undergo surgery, which would be relevant if we attend patients with inserional tendionpathy and partial ruptures or total rupture which evolve favourably with conservative treatment or who simply do not wish to undergo surgery.
ConclusionsBoth USG and MR are appropriate tests for the preoperative diagnosis of DBT ruptures. In our series the results of the MR are superior to those of the USG, as reflected in the reviewed literature.6,7,9,15,16
In view of the results obtained, since USG is a reliable diagnostic measurement and is more accessible and cheaper than MT, this could be the initial method of choice for the study of partial and complete rupture of the distal tendon of the biceps, in patients with compatible causes and symptoms.
Level of evidenceLevel of evidence II.
Conflict of interestsThe authors have no conflict of interest to declare nor have they received any grants or financial support of any type for this study.
Please cite this article as: García Rodríguez C, et al. Rotura del tendón distal del bíceps: potencia diagnóstica de la ecografía y la resonancia magnética. Rev Esp Cir Ortop Traumatol. 2020;64:77–82.