To determine, through a systematic review, the effects of halo gravity traction in spinal deformity.
MethodsProspective studies or case series of patients with scoliosis or kyphosis treated with cranial halo gravity traction (HGT) were included. Radiological outcomes were measured in the sagittal and/or coronal planes. Pulmonary function was also assessed. Perioperative complications were also collected.
ResultsThirteen studies were included. Congenital etiology was the most frequent etiology observed. Most studies provided clinically relevant curve correction values in the sagittal and coronal planes. Pulmonary values improved significantly after the use of HGT. Finally, there were a pool of 83 complications in 356 patients (23.3%). The most frequent complications were screw infection (38 cases).
ConclusionsPreoperative HGT appears to be a safe and effective intervention for deformity that allows correction prior to surgery. However, there is a lack of homogeneity in the published studies.
Determinar, mediante una revisión sistemática, los efectos de la tracción de halo-gravedad (HGT) en las deformidades de columna.
MétodosSe incluyeron estudios prospectivos o series de casos de pacientes con escoliosis o cifosis tratados con HGT. Los resultados radiológicos se midieron en los planos sagital y/o coronal. También se evaluó la función pulmonar. Finalmente, se recogieron las complicaciones perioperatorias.
ResultadosSe incluyeron 13 estudios. La etiología congénita fue la más frecuente. La mayoría de los estudios proporcionaron valores de corrección de la curva clínicamente relevantes en los planos sagital y coronal. Los valores pulmonares mejoraron significativamente tras el uso de HGT. Por último, existieron 83 complicaciones en 356 pacientes, siendo la infección la más frecuente (38 casos).
ConclusionesLa HGT mostró ser una intervención segura y eficaz para la deformidad, que permite la corrección antes de la cirugía. Sin embargo, existe una falta de homogeneidad en los estudios publicados.
In 1959, Perry and Nickel introduced the basis for the development of the halo, an aid for traction and stabilization of the cervical spine.1–3 The halo has been used for stabilizing cervical pathology caused by heterogeneous etiology, including trauma pathology, deformities, neoplasms, rheumatoid arthritis, or infections.4,5 Initially, the halo was used to reduce further surgery risks by providing safety and gradually correcting spinal curvature.6 Likewise, halo gravity traction has been recommended to mitigate the curve of severe scoliosis and improve pulmonary function prior to surgery.7,8
The correction of severe and rigid scoliosis and kyphoscoliosis is a challenging surgical procedure; in addition, there is significant pulmonary compromise. The goal of surgery in these patients is to detain the progression of deformity, decrease the size of the curve, and restore trunk balance while improving the patient's quality of life, providing cardiopulmonary stability, and avoiding long-term sequelae of restrictive lung disease.7
One of the most dramatic complications associated with the correction of severe scoliosis is a significant incidence of perioperative pulmonary insufficiency. The deformation of the rib cage, as well as the weakness of the inspiratory and expiratory muscles, causes restrictive lung disease in addition to obstructive lung disease due to compression of the upper respiratory tract.9 Therefore, patients with scoliosis may present preoperative alterations, such as hypoxia, alveolar hypoventilation, and hypercapnia. After surgery, these modifications could drastically complicate the prognosis of the patients and therefore hinder an effective and satisfactory correction.10 Respiratory function has an impact on both physical function and mortality.11 In patients with severe curves greater than 100°, the pulmonary compliance decreases to levels comparable to those of adult respiratory distress syndrome.12
The neurological consequences of stiff kyphoscoliosis are caused by the strain on the spinal cord placed at the kyphotic or scoliotic apex. Enhancement of progressive neurologic deficits may occur during halo gravity traction in selective cases with non-compensated curves.6,13 The progressive reduction of the curve and neurological and pulmonary improvement may allow the spine surgeon to achieve a pre-operative risk reduction.6
The complications of halo gravity traction (HGT) differ widely in the literature, ranging from 11 to 92% in different studies, although most of these are classified as “minor” complications.14 The following are absolute contraindications to halo placement: cranial fracture, bone deficit, sepsis, or severe soft tissue injury. Relative contraindications include severe chest trauma, obesity, and barrel chest.7,15
In the present study, the existence of meta-analyses on the topic of interest,16–18 was considered, but a systematic review was chosen instead. The decision was based on the broad nature of the research question, which encompassed multiple topics and approaches. Furthermore, the data from the included studies exhibited significant heterogeneity, which made it challenging to combine the results in a meta-analysis. In addition, the available data were inadequate to perform a meta-analysis, and various study types, including qualitative and quantitative, were included. Consequently, a systematic review was preferred to offer a narrative synthesis of the literature and to identify areas that require further research.
Therefore, the objective of this study was to determine, through a systematic review, the efficacy and safety of Halo Gravity Traction on spinal deformity.
MethodsEligibility criteriaWe followed the PICO strategy: Participants: patients were younger than 30 years old, most of them were pediatric patients with spine deformity due to idiopathic, congenital, neuromuscular or syndromes among others etiology. Due to the heterogeneity of the studies this cut-off point of 30 years was established by the senior surgeons in pediatric spine deformity. Intervention: Series or prospective cohort studies that analyzed the efficacy or safety of HGT in the treatment of spine deformities. Comparation: These studies compare the efficacy and complications of HGT procedure measuring the magnitude of the curve, the pulmonary function and the adverse events. Outcomes: Primary outcome measures were the Cobb angle in the sagittal and coronal plane. Secondary outcome were the pulmonary function measured through forced vital capacity FVC, forced expired volume in the first second FEV1, FEV1/VC or Tiffenau index, and peak expiratory flow PEF. Finally, we recorded the adverse events found during the follow up.
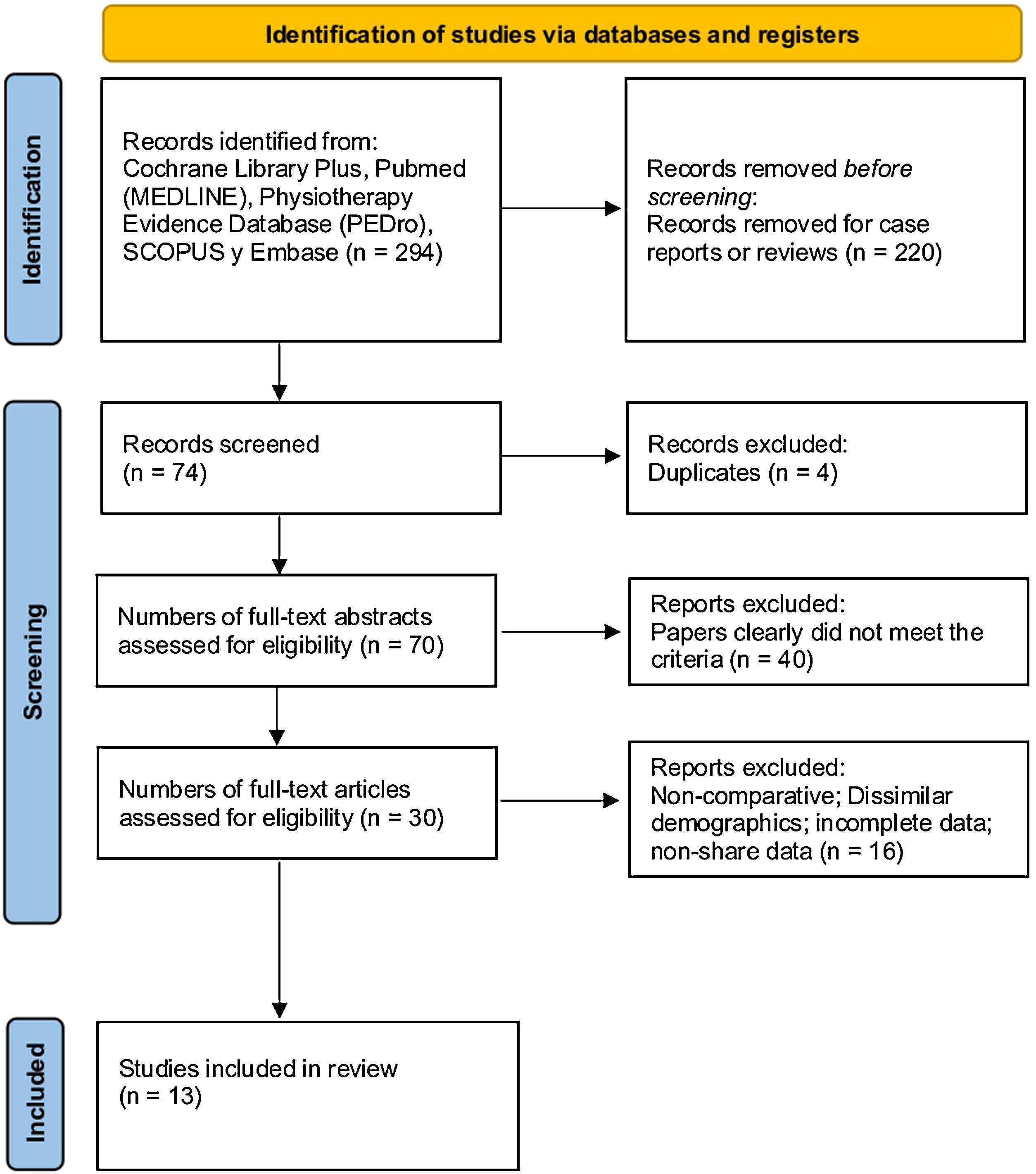
Information sourcesThis systematic review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria (Fig. 1).19 We search for studies in the following databases recognized by the scientific community: The Cochrane Library Plus, Pubmed (MEDLINE), Physiotherapy Evidence Database (PEDro), SCOPUS and EMBASE.
Search strategy and selection of studiesThe publication cut-off date was the last 20 years. The following Medical Subject Headings (MeSH) were used: “Halo AND spine”, “Halo AND spine deformity”, “Halo AND scoliosis”, and “Halo AND kyphosis”. The search was limited to the English language. Inclusion criteria were as follows: prospective studies or series of patients treated with cranial HGT; studies that included at least any of the following outcomes: etiology of scoliosis or kyphosis, radiological outcomes measured by Cobb angle before and at the end of follow-up in the sagittal and/or coronal planes, and pulmonary function. Exclusion criteria were studies that used traction after surgery, studies that focused on a single etiology, patients older than 30 years, studies that did not treat humans, studies that were the same, studies that used femoral traction or another surgical or orthopedic procedure, and studies that did not share variables (Fig. 1).
Data extraction and data itemsWe extracted the following baseline data from each study: number of patients, gender, mean age, height, weight, follow-up, and maximum/mean halo weight. The variables related to the efficacy of the use of halo gravity traction were radiological outcomes and pulmonary function outcomes. The most frequent etiologies of each study were collected. The radiological results included the Cobb angle in a sagittal plane (kyphosis) and in a coronal plane (scoliosis). From the radiological results, the mean difference between the Cobb angle before halo and at the end of follow-up was obtained. In addition, the standard deviation and range of the articles as well as the statistical significance were obtained. Respiratory function was assessed by forced vital capacity FVC, forced expired volume in the first second FEV1, FEV1/VC or Tiffenau index, and peak expiratory flow PEF. The statistical significance provided by the studies was also obtained.
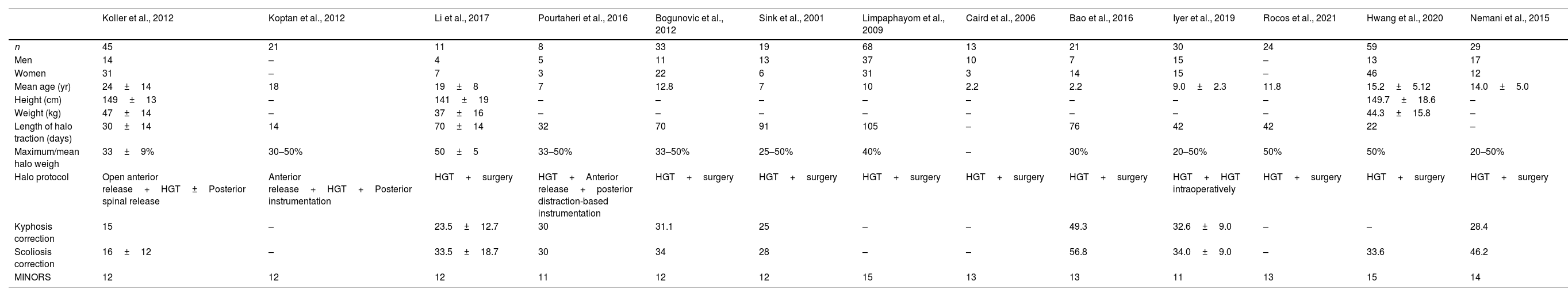
Risk of bias of individual studiesThe quality of the included studies was assessed independently by two authors using the Methodological Index for Non-Randomized Studies (MINORS) criteria (Table 1). It was established to assess the quality of comparative and noncomparative studies; the maximum score is 24 for comparative studies and 16 for noncomparative studies. For noncomparative studies, scores of 0–4 corresponded to very low quality, 5–7 corresponded to low quality, 8–12 corresponded to fair quality, and ≥13 corresponded to high quality. For comparative studies, scores of 0–6 corresponded to very low quality, 7–10 corresponded to low quality, 11–15 corresponded to fair quality, and ≥16 corresponded to high quality.
Demographic characteristics of the included studies and mean scoliosis/kyphosis correction.
| Koller et al., 2012 | Koptan et al., 2012 | Li et al., 2017 | Pourtaheri et al., 2016 | Bogunovic et al., 2012 | Sink et al., 2001 | Limpaphayom et al., 2009 | Caird et al., 2006 | Bao et al., 2016 | Iyer et al., 2019 | Rocos et al., 2021 | Hwang et al., 2020 | Nemani et al., 2015 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | 45 | 21 | 11 | 8 | 33 | 19 | 68 | 13 | 21 | 30 | 24 | 59 | 29 |
| Men | 14 | – | 4 | 5 | 11 | 13 | 37 | 10 | 7 | 15 | – | 13 | 17 |
| Women | 31 | – | 7 | 3 | 22 | 6 | 31 | 3 | 14 | 15 | – | 46 | 12 |
| Mean age (yr) | 24±14 | 18 | 19±8 | 7 | 12.8 | 7 | 10 | 2.2 | 2.2 | 9.0±2.3 | 11.8 | 15.2±5.12 | 14.0±5.0 |
| Height (cm) | 149±13 | – | 141±19 | – | – | – | – | – | – | – | – | 149.7±18.6 | – |
| Weight (kg) | 47±14 | – | 37±16 | – | – | – | – | – | – | – | – | 44.3±15.8 | – |
| Length of halo traction (days) | 30±14 | 14 | 70±14 | 32 | 70 | 91 | 105 | – | 76 | 42 | 42 | 22 | – |
| Maximum/mean halo weigh | 33±9% | 30–50% | 50±5 | 33–50% | 33–50% | 25–50% | 40% | – | 30% | 20–50% | 50% | 50% | 20–50% |
| Halo protocol | Open anterior release+HGT±Posterior spinal release | Anterior release+HGT+Posterior instrumentation | HGT+surgery | HGT+Anterior release+posterior distraction-based instrumentation | HGT+surgery | HGT+surgery | HGT+surgery | HGT+surgery | HGT+surgery | HGT+HGT intraoperatively | HGT+surgery | HGT+surgery | HGT+surgery |
| Kyphosis correction | 15 | – | 23.5±12.7 | 30 | 31.1 | 25 | – | – | 49.3 | 32.6±9.0 | – | – | 28.4 |
| Scoliosis correction | 16±12 | – | 33.5±18.7 | 30 | 34 | 28 | – | – | 56.8 | 34.0±9.0 | – | 33.6 | 46.2 |
| MINORS | 12 | 12 | 12 | 11 | 12 | 12 | 15 | 13 | 13 | 11 | 13 | 15 | 14 |
MINORS: Methodological Index for Non-Randomized Studies.
This systematic review was carried out using an Excel spreadsheet (v.16.52 for IOS). For quantitative variables, the mean, standard deviation, range, and statistical significance of each study were used. A statistical comparison or meta-analysis of the studies could not be made since the studies did not measure the variables in the same way and most of them did not provide the standard deviations, confidence interval, or statistical significance of their results. P-values less than 0.05 were considered statistically significant.
ResultsCharacteristics of the studiesTable 1 reflects the characteristics of the included studies.4,6,20–27 Thirteen studies were included between 2001 and 2020. The number of patients varied between 8 and 68. The mean age varied between studies, and most included pediatric patients, although three articles included adult patients. Maximum/mean halo weight varied between 25 and 50% of patient weight. Follow-up ranged from 14 days to 105 days from study with shorter to longer follow-up periods respectively.
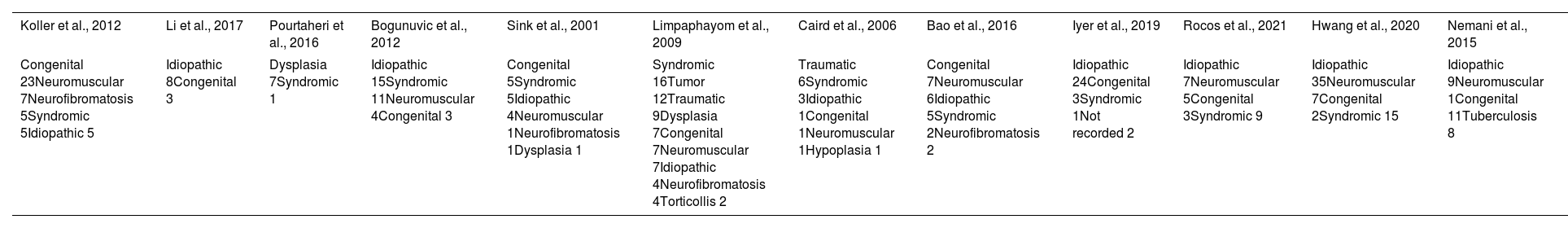
EtiologyThirteen studies analyzed the etiology of the patients carefully. The etiology included in the articles is shown in Table 2. Idiopathic (24.6%) was the most frequently observed, followed by congenital (19.4%), syndromic (16.6%), traumatic (14.8%) and neuromuscular (9.7%) etiology.
Etiology presented by the included studies.
| Koller et al., 2012 | Li et al., 2017 | Pourtaheri et al., 2016 | Bogunuvic et al., 2012 | Sink et al., 2001 | Limpaphayom et al., 2009 | Caird et al., 2006 | Bao et al., 2016 | Iyer et al., 2019 | Rocos et al., 2021 | Hwang et al., 2020 | Nemani et al., 2015 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Congenital 23Neuromuscular 7Neurofibromatosis 5Syndromic 5Idiopathic 5 | Idiopathic 8Congenital 3 | Dysplasia 7Syndromic 1 | Idiopathic 15Syndromic 11Neuromuscular 4Congenital 3 | Congenital 5Syndromic 5Idiopathic 4Neuromuscular 1Neurofibromatosis 1Dysplasia 1 | Syndromic 16Tumor 12Traumatic 9Dysplasia 7Congenital 7Neuromuscular 7Idiopathic 4Neurofibromatosis 4Torticollis 2 | Traumatic 6Syndromic 3Idiopathic 1Congenital 1Neuromuscular 1Hypoplasia 1 | Congenital 7Neuromuscular 6Idiopathic 5Syndromic 2Neurofibromatosis 2 | Idiopathic 24Congenital 3Syndromic 1Not recorded 2 | Idiopathic 7Neuromuscular 5Congenital 3Syndromic 9 | Idiopathic 35Neuromuscular 7Congenital 2Syndromic 15 | Idiopathic 9Neuromuscular 1Congenital 11Tuberculosis 8 |
Nine studies provided the difference between the initial Cobb angle and the one after follow-up when using HGT. This difference ranged from 16° in the study with the least correction (Koller 2012) to 56.83° (Bao 2016). Seven studies gave the difference between the sagittal plane Cobb angle at baseline and at the end of follow-up when using halo. This difference ranged from 15° in the study with the least correction (Koller 2012) to 49.27° (Bao 2016).
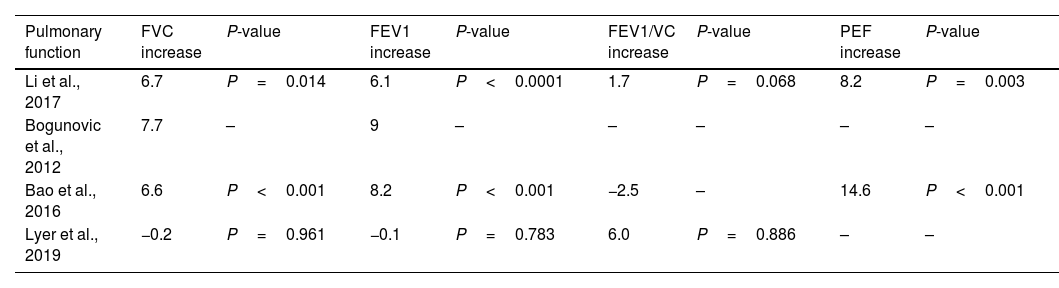
Pulmonary functionPulmonary function is shown in Table 3. Four studies included pulmonary function outcomes. Regarding FVC, three studies demonstrated an increase in FVC after follow-up with halo, two of which provided a significant P value. Regarding FEV1, two studies showed a significant increase in FEV1 at the end of follow-up. Regarding FEV1/FVC evaluated in three studies, none showed a significant increase. Finally, PEG showed a significant improvement in two studies.
Pulmonary outcomes after follow-up.
| Pulmonary function | FVC increase | P-value | FEV1 increase | P-value | FEV1/VC increase | P-value | PEF increase | P-value |
|---|---|---|---|---|---|---|---|---|
| Li et al., 2017 | 6.7 | P=0.014 | 6.1 | P<0.0001 | 1.7 | P=0.068 | 8.2 | P=0.003 |
| Bogunovic et al., 2012 | 7.7 | – | 9 | – | – | – | – | – |
| Bao et al., 2016 | 6.6 | P<0.001 | 8.2 | P<0.001 | −2.5 | – | 14.6 | P<0.001 |
| Lyer et al., 2019 | −0.2 | P=0.961 | −0.1 | P=0.783 | 6.0 | P=0.886 | – | – |
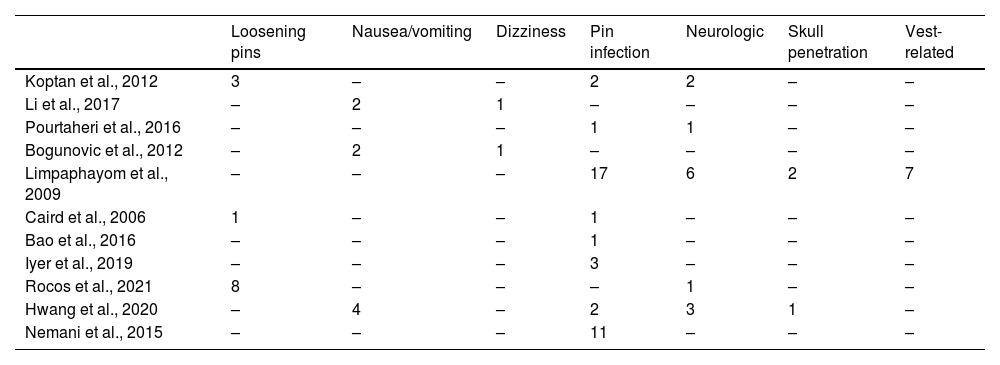
The complications are shown in Table 4. Eleven studies were included. There were 83 complications in 356 patients. The most frequent complication was screw infection (38), followed by neurological complications (13), screw loss or loosening (12), nausea and vomiting (8), vest-related complications (7), skull penetration (3), and dizziness (2).
Complications during HGT period.
| Loosening pins | Nausea/vomiting | Dizziness | Pin infection | Neurologic | Skull penetration | Vest-related | |
|---|---|---|---|---|---|---|---|
| Koptan et al., 2012 | 3 | – | – | 2 | 2 | – | – |
| Li et al., 2017 | – | 2 | 1 | – | – | – | – |
| Pourtaheri et al., 2016 | – | – | – | 1 | 1 | – | – |
| Bogunovic et al., 2012 | – | 2 | 1 | – | – | – | – |
| Limpaphayom et al., 2009 | – | – | – | 17 | 6 | 2 | 7 |
| Caird et al., 2006 | 1 | – | – | 1 | – | – | – |
| Bao et al., 2016 | – | – | – | 1 | – | – | – |
| Iyer et al., 2019 | – | – | – | 3 | – | – | – |
| Rocos et al., 2021 | 8 | – | – | – | 1 | – | – |
| Hwang et al., 2020 | – | 4 | – | 2 | 3 | 1 | – |
| Nemani et al., 2015 | – | – | – | 11 | – | – | – |
Based on the findings of this review, we can report that HGT is an effective procedure that corrects deformity prior to surgery and improves pulmonary function. Complications are not rare, although most are mild and vary greatly among different studies. Regarding neurological complications, many of the studies did not specify the type of complication found. Those studies that reported the exact type of complication found mostly reported mild complications, including paresthesia or weakness that were recovered over time in the majority of cases. Less frequently, cranial nerve injuries, Horner's syndrome, and bradycardia in one patient were found.
The included studies were based on case series and prospective cohort studies, so the evidence is not conclusive; however, it is difficult to find randomized clinical trials (RCTs) of the use of HGT given the ethical implications.
Regarding the studies included in the last 20 years, there was considerable heterogeneity as well as a lack of data. This heterogeneity was observed in the number of patients included. The use of HGT is not widespread, and it is difficult to create large series. Age also varied in the different studies, and this is related to the etiology included by each of the studies. Not all studies included all etiologies. For example, traumatic or tumor etiology was included in very few studies, and this is logical since these causes are not frequent at pediatric age. Furthermore, there was no consistency in the measurement of the results and each study provided the results in different units. Regarding the weight used in traction, there was homogeneity among the studies, varying approximately between 30 and 50% of the total weight. Regarding the lack of data, only two series included the weight and height of the patients. However, traction must be individualized for each patient.
Correction of the kyphoscoliotic deformity was evident in all studies. Moreover, this correction is sufficiently large to be explained by a failure to measure the Cobb angle. There were no differences between studies in terms of deformity correction and time of HGT or weight used (although some articles did not include these measures). Table 1 shows the correction results in the sagittal and coronal planes along with demographic variables. Although there were no differences in the patient's age.
HGT has demonstrated clear preoperative benefits in the treatment of severe spinal deformities, reaching corrections in some series of 35% of the coronal and 35% of the sagittal Cobb angle and also optimizing pulmonary function by 9%. This causes a release of the apical tethering in the spinal cord. With a partial curve correction, the stress on the spinal cord is reduced.6,13 Koller et al. observed neurological improvement in five patients with progressive spasticity preoperatively at the onset of halo-gravity traction.6 Despite these results, there is no consensus on an optimal protocol for traction and use of halo in clinical practice.4,6 Childhood development could condition the results of the HGT and the presence of complications.7
Problems with HGT during sleep and during different daily activities also need to be addressed. Studies have shown that the distraction forces on the neck are much greater in a supine position relative to a standing or sitting position during rest.28
The results obtained regarding pulmonary function were analyzed by few studies in a comparative way. In this case it is important to individualize the patients and to give clinically relevant results, such as how many patients had an obstructive pattern and how many stopped having it after the use of HGT.
In terms of complications, only complications after HGT surgery were collected. There was heterogeneity when classifying complications, so in this study we included fewer complications from each study, since some studies included screw penetration after a fall when wearing the HGT as a complication. Some complications such as erythema were included under infection. Some studies included reoperations as complications, so the number of complications increased in these studies. Reoperations should be given separately so as not to skew the percentage of complications. We were also unable to analyze reoperations because few studies included these variables, and some studies did not include the reason for the reoperation. No correlation was found between the rate of complications and time of HGT use.
Since most of the complications were related to pin infection, some of the measures proposed by the literature to decrease pin complications were a greater number of pins, meticulous care of the pin placement site, frequent follow-up, and limited ambulation, since young children are more likely to fall than older age groups. The following measures should be considered to decrease the number of pin-related complications.26,29–31
This study has several limitations. The patient sample in some studies was limited; however, the use of HGT is not common and some etiologies of scoliosis are not frequent. It would also be important to include measures of patients’ quality of life during the traction period. There was a lack and heterogeneity of statistical data that did not allow for an adequate comparison. In addition to the heterogeneity inherent to the age and etiology of scoliosis, there were differences in the number of patients included in each etiology and even etiologies that were not included in other studies. Also, the heterogeneity in age and the cut-off point of 30 years should lead us to consider these results carefully. We add the intra- and inter-observer variability when measuring scoliosis and kyphosis using the Cobb angle. In some cases, it was not separated when measuring scoliosis and kyphosis. Preoperative and postoperative frontal and sagittal Cobb angles could not be obtained according to etiology. Among the idiopathic etiology, the type of deformity according to Lenke's classification could not be determined. In most studies there was no definition of kyphosis. Also, it was not feasible to evaluate the rate of correction per day or week with HGT. Additionally, the uncertainty or level of evidence of the results was low due to the design of the included studies, which were clinical series or cohort studies, and the heterogeneity in the inclusion criteria and measurement processes, such as the period with HGT. Finally, it was not possible to quantitatively assess publication bias through a funnel plot, so the results should be interpreted with caution. Failure to take these considerations into account could result in an overestimation of the effect of the results.
In conclusion, this systematic review shows that the use of HGT in spinal deformities is effective in reducing scoliotic and kyphotic curves prior to surgery and thus predictably reduces the number of complications in subsequent fusion surgery. The use of HGT has an impact on pulmonary function; however, it would be necessary to determine whether this impact has clinical relevance. As for complications, pin infection was the most frequent. Finally, more homogeneity between studies is needed, as well as a wider provision of data.
Level of evidenceLevel of evidence iii.
FundingNo funding was received.
Conflict of interestsThe author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.