SCIWORA has a low incidence but a high functional repercussion. The aim of the present study was to characterize the epidemiology of this clinical–radiological condition and evaluate functional outcome with a mean of 10-years follow-up.
Material and methodsObservational, longitudinal ambispective cohort study. Thirteen SCIWORA patients were admitted in the study period. Demographics, mechanism of injury, spinal cord MRI findings, neurological level of injury, time to SCI, neurological status (AIS) at admission/discharge/5 years, spinal cord independence measure (SCIM III) scale at admission and discharge, hospital length of stay and mean follow-up were recorded. On October 2022 patients were re-evaluated using NDI, Oswestry, and SV-QLI/SCI.
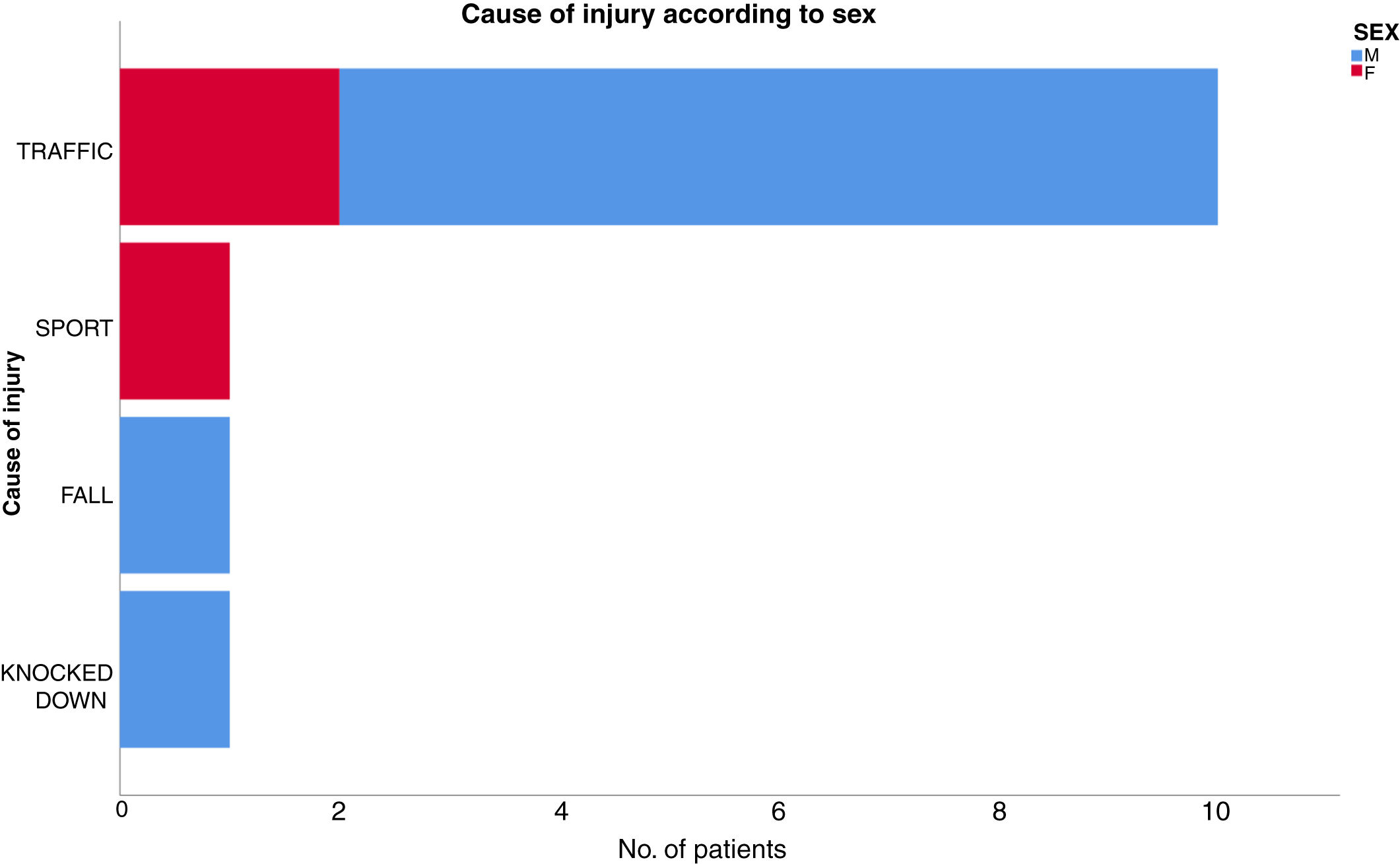
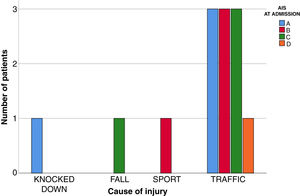
ResultsMedian age was 4 years. The study population for this investigation was mostly men (77%). 54% of level of injury correspond to cervical spine. AIS at admission was A (31%) and C (31%). Neurological level of injury was C2 (22%) and T10 (15%). Motor vehicle-related injury was the most prevalent mechanism of injury (77%), SCIM III scale at admission and discharge: 28.5/42, hospital length of stay was 115 days. The NDI was 11.6, Oswestry: 15.3 and SV-QLI/SCI: 17.
ConclusionsSeventy-seven percent of SCIWORA patients was detected under 8 years-old. At 1 year follow-up after discharge 31% patients were AIS grade D and with 5 years follow-up the percentage remain constant. No statistically significant differences in the mechanism of injury and MRI findings (P=0.872), age and MRI spinal cord findings (P=0.149) were found in SCIWORA patients.
La lesión medular tipo SCIWORA es una entidad clínica con baja incidencia y alta repercusión funcional. El objetivo del estudio es la descripción epidemiológica de esta lesión y su evolución funcional con un seguimiento medio de 10 años.
Material y métodosEstudio analítico, longitudinal, de cohortes ambispectivo. Fueron evaluados 13 pacientes con el diagnóstico de SCIWORA en el periodo de estudio 2001-2022. Variables evaluadas: edad, sexo, días hasta la lesión medular, causa de la lesión, imagen medular en la RM postraumatismo, nivel neurológico de la lesión, ASIA ingreso/alta/5 años, SCIM III ingreso/alta/3 años, tipo de tratamiento empleado, empleo de terapia NASCIS III ingreso, tiempo de hospitalización, seguimiento medio. En octubre de 2022 fueron nuevamente evaluados en consultas externas mediante: cuestionario de discapacidad cervical (NDI)/Oswestry y cuestionario de calidad de vida validado en castellano para lesionados medulares (SV-QLI/SCI).
ResultadosLa mediana de edad fue de 4 años, 77% varones. El 54% de las lesiones corresponden a nivel cervical. El ASIA al ingreso fue del 31% A y del 31% C, nivel neurológico: C2 (22%) y T10 (15%), tráfico como causa de lesión (77%), SCIM III ingreso/alta: 28,5/42. La estancia media hospitalaria fue de 115 días. NDI: 11,6 y Oswestry: 15,3.
ConclusiónEl 77% de los SCIWORA se producen en menores de 8 años. Al año del alta hospitalaria el 31% de los pacientes fueron catalogados como ASIA D y a los 5 años el porcentaje se mantiene constante. No se encontraron diferencias significativas entre la causa de la lesión y el tipo de alteración en RM (p=0,872), ni entre la edad y el tipo de lesión medular objetivada en RM (p=0,149).
SCIWORA (spinal cord injury without radiographic abnormality) is a clinical entity whose name was coined by Pang and Wilberger in 1982.1 It has a low incidence and high functional repercussion in paediatric age.2 It consists of a spinal cord injury without radiographic abnormalities following vertebral trauma. It fundamentally affects paediatric ages and the cervical region, with traffic accidents and sports injuries as its chief causes.3 Its high level of incidence in the paediatric population can be attributed to the greater elasticity of ligamentous structures in comparison with the spinal cord, the presence of a more wedge-shaped form in the anterior region of the cervical vertebra and a more horizontal alignment of the articular facets. All of these factors favour an increased likelihood of spinal cord injury in the case of a sudden flexor-extension mechanism.
In the majority of cases SCIWORA is treated conservatively during a 12-week period, with the aim of preventing recurring SCIWORA.4
Nevertheless, although the causes of this injury in paediatric age and its treatment are known, few studies have been undertaken that define the functional status of these patients over more than 10 years’ follow-up time.5,6
The objectives of this study are therefore: to describe the epidemiological characteristics of this type of injury in the paediatric population and evaluate the functional status of the patients with a SCIWORA over an average follow-up time of 10 years.
Material and methodsAn analytical, longitudinal and ambispective cohort study was designed of a population of patients affect by a SCIWORA-type lesion in the study period 2001–2022. This study was wholly undertaken in a national referral hospital for the comprehensive treatment of spinal cord injury patients. The inclusion criteria set for this study were: (1) an age below 18 years at the moment of the spinal cord injury; (2) spinal cord injury after trauma at cervical or thoracic level; (3) the absence of vertebral fracture in imaging tests, and (4) patients hospitalised in our centre following their spinal cord injury and who subsequently attended our centre annually to date for follow-up in the out-patient departments. The following exclusion criteria were set: (1) age higher than 18 years at the moment the injury occurred; (2) the presence of ligamentous lesions, cervical luxation or fractures in imaging tests; (3) epidural haematoma; (4) traumatic disc hernia, or (5) those patients who decided not to participate in the study.
The variables of interest evaluated for the study were: demographic variables, days from the trauma until the commencement of neurological symptoms, cause of injury, post-traumatic spinal MR image, neurological level of the lesion, AIS at admission/discharge/5 years, SCIM III at admission/discharge/3 years, type of treatment used, the use of NASCIS III therapy at admission, hospitalization time, and average follow-up. In October 2022 the patients were evaluated again in out-patient facilities by: a cervical disability questionnaire (NDI) in the case of cervical lesion or the Oswestry disability scale in the case of thoracic level lesion, and a quality of life questionnaire validated in Spanish for spinal cord injury patients (SV-QLI/SCI).
All of the patients gave their informed consent to be included in the study. The study was approved by the ethics committee of our hospital.
The data obtained were entered in an Excel database (Microsoft Office for Macintosh [Washington, U.S.A.]). Statistical analysis was performed using the IBM SPSS Statistics 25 programme for health sciences (SPSS Inc., Chicago, IL, U.S.A.). The following qualitative variables were recorded: sex (1: female; 2: male), cause of injury (1: traffic; 2: sport; 3: fall), type of treatment used (1: conservative; 2: surgical), use of NASCIS III therapy (1: yes; 2: no). The ordinal qualitative variable obtained was: the AIS scale. The continuous quantitative variables were: days after the trauma to the start of neurological symptoms, average follow-up time, hospitalization time, and SCIM III score. The discrete quantitative variables were: Oswestry, NDI, and SV-QLI/SCI.
All of the study data were recorded by the same individual (the chief researcher), as was the evaluation of all of the patients assessed in October 2022, thereby preventing any probable distortions. The chief researcher is an independent researcher. To limit interviewer bias structured questionnaires that had been validated in Spanish were used, Oswestry, NDI and SV-QLI/SCI.
Categorical variables were described in terms of absolute frequencies and percentages. Continuous variables were described using the median and interquartile range. For inferential analysis the Chi-squared test (categorical variables) and the Mann–Whitney U test were used to compare a quantitative variable with another qualitative one were applied, and the Kruskal–Wallis test was used when a categorical variable had more than 2 categories. The level of statistical significance was defined as P<0.05.
Shapiro–Wilks analysis was performed using the SPSS statistical package to find whether the variables evaluated in the study followed a normal distribution.
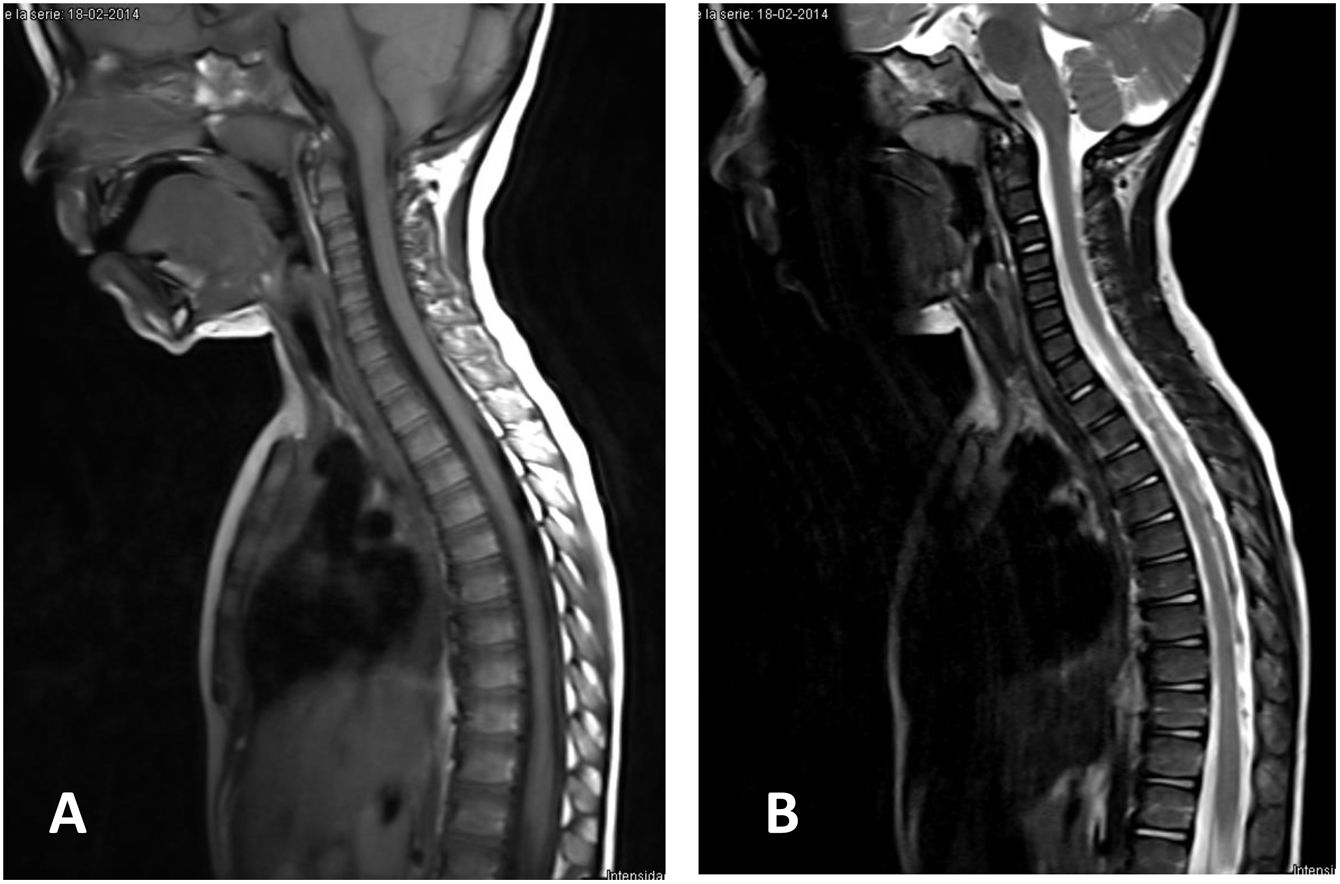
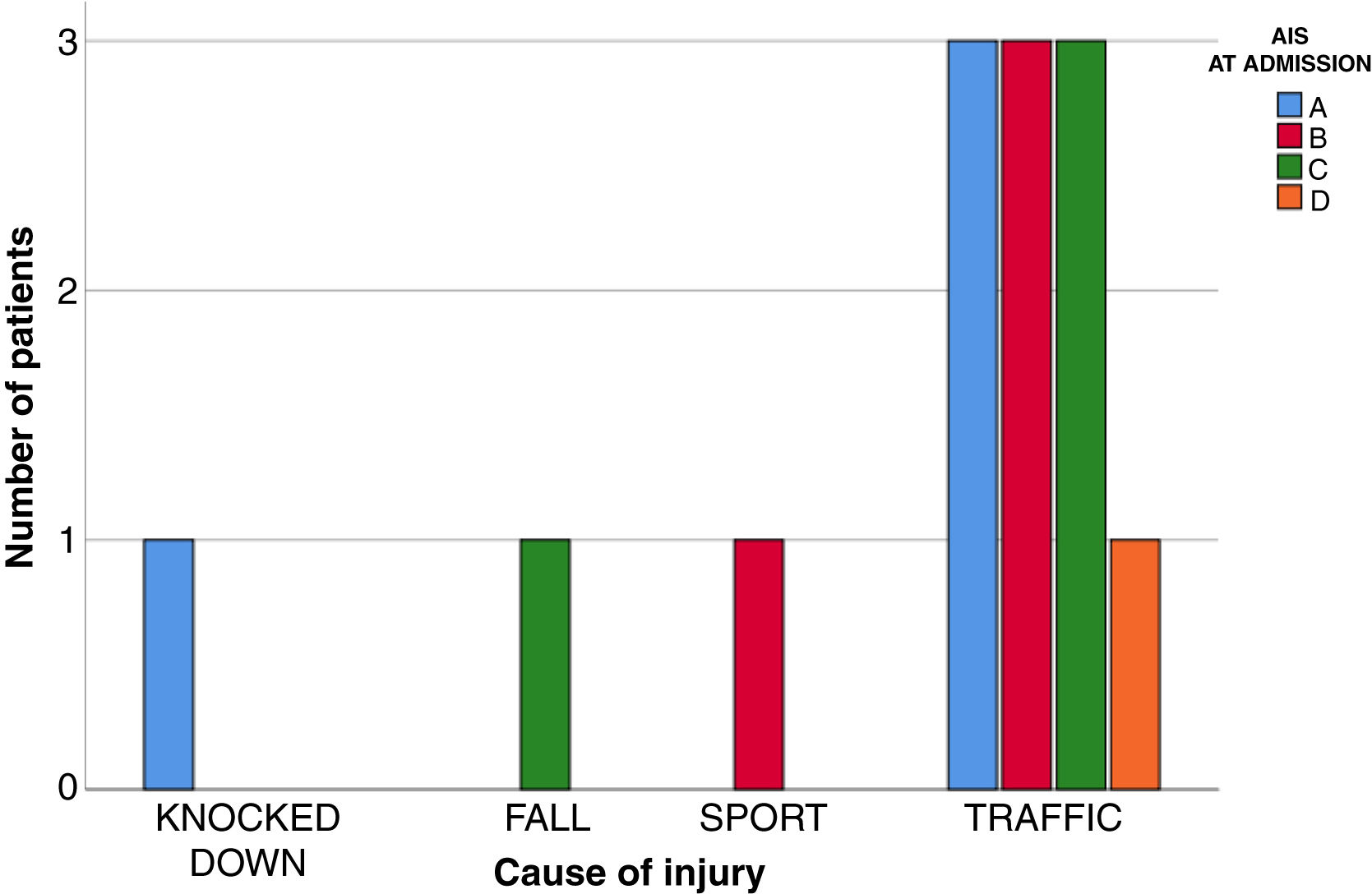
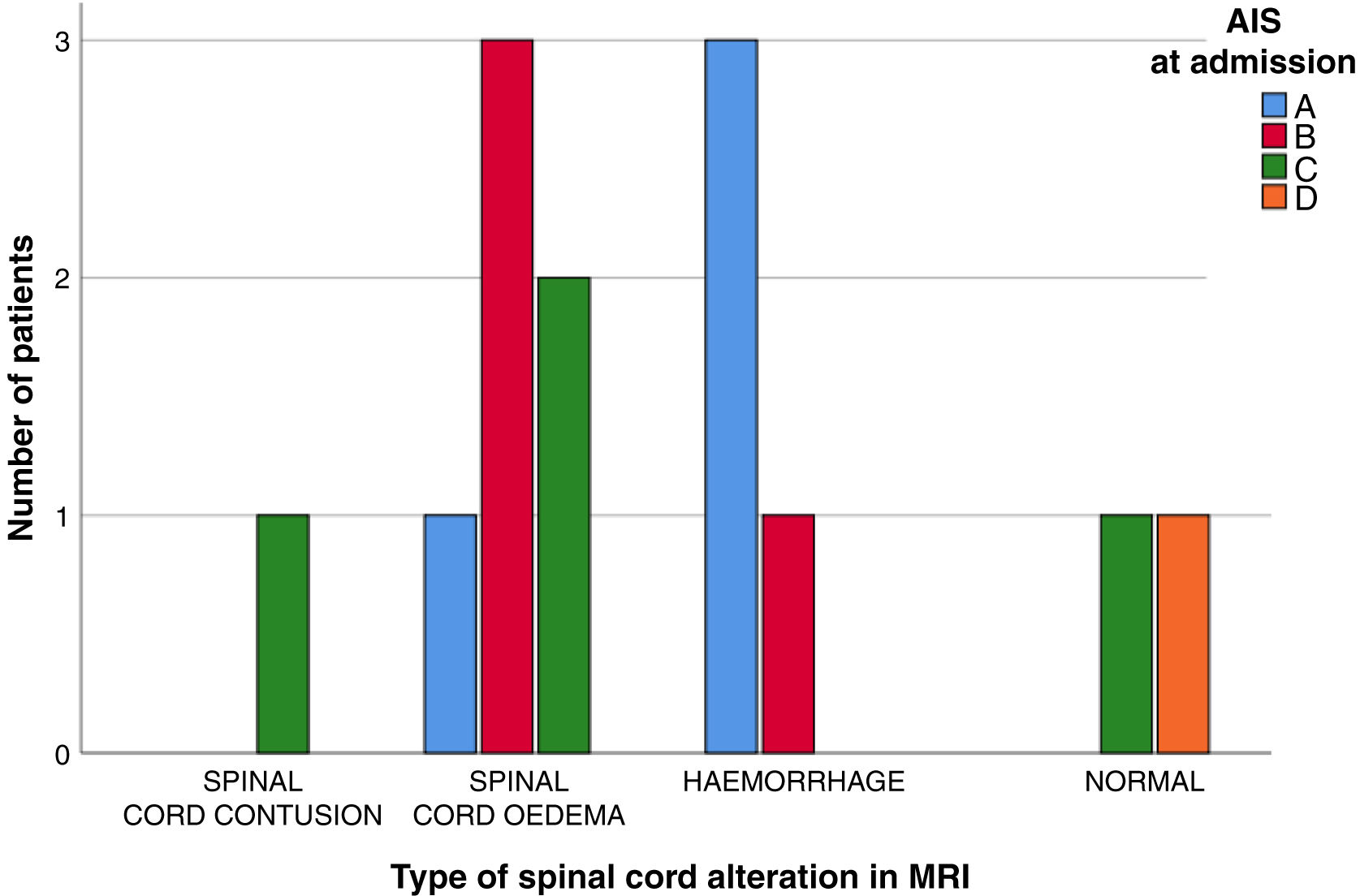
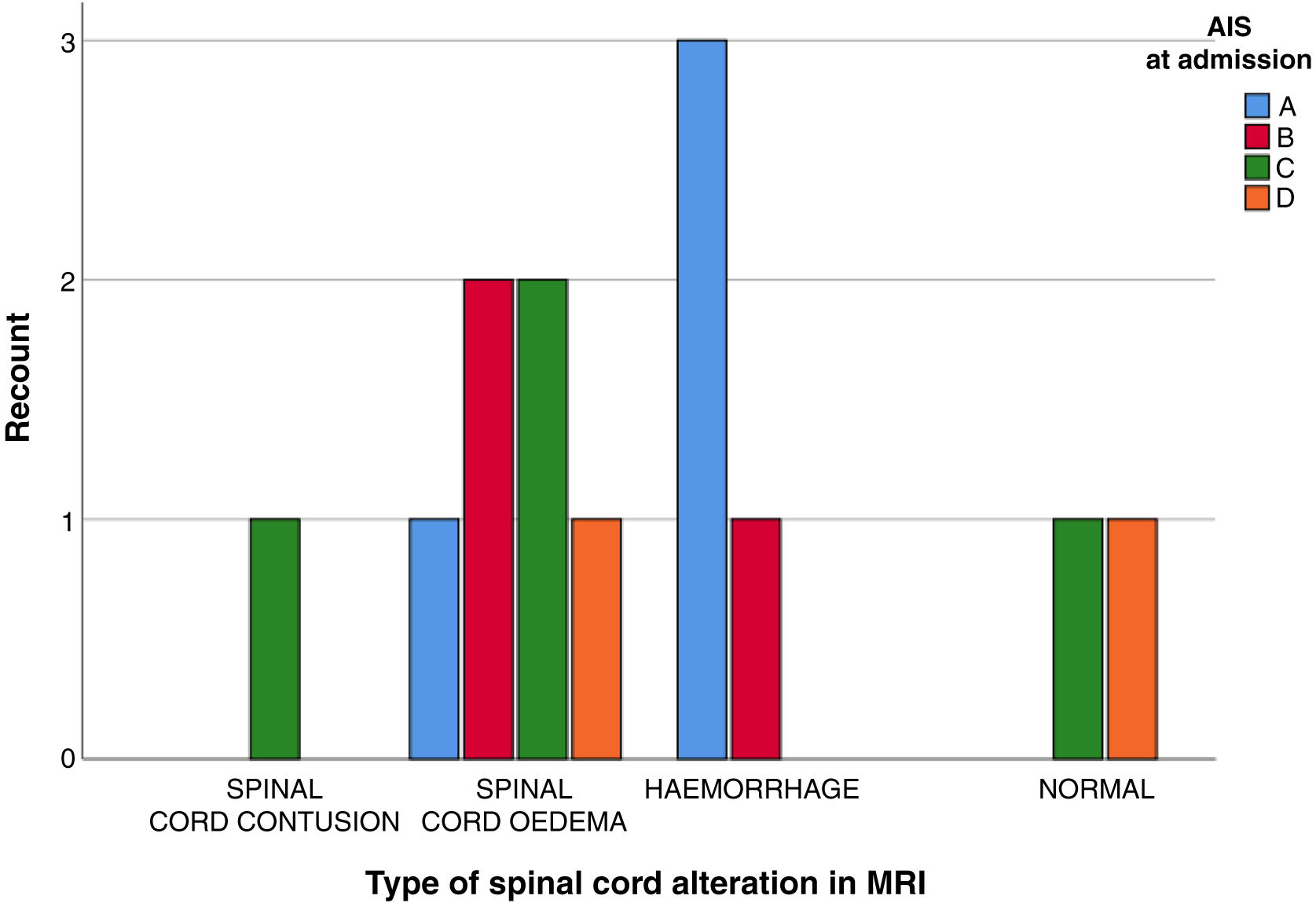
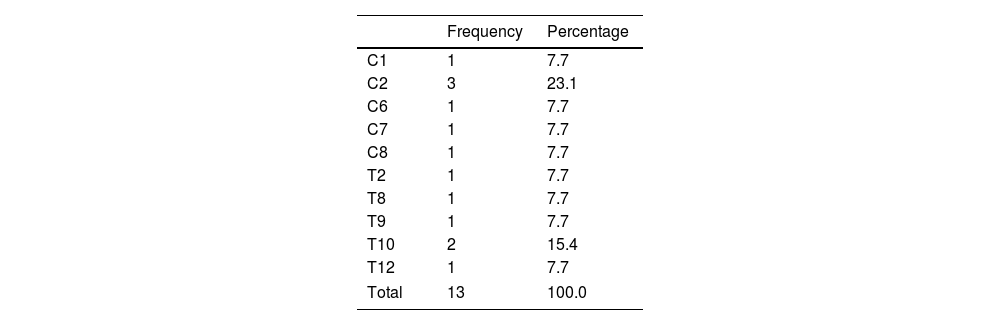
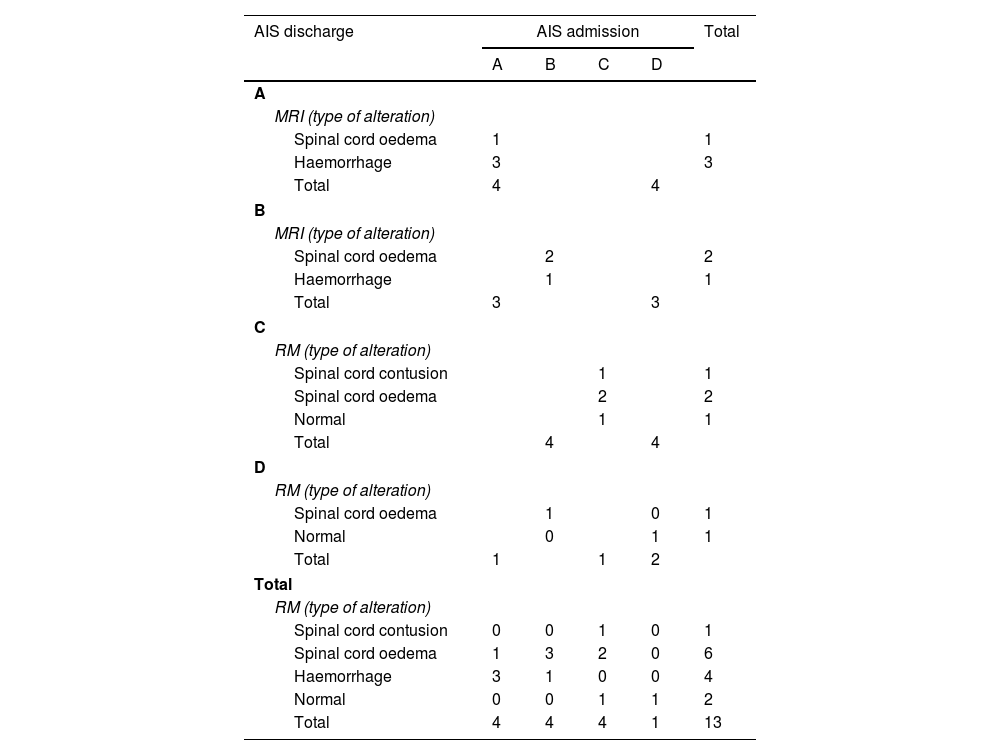
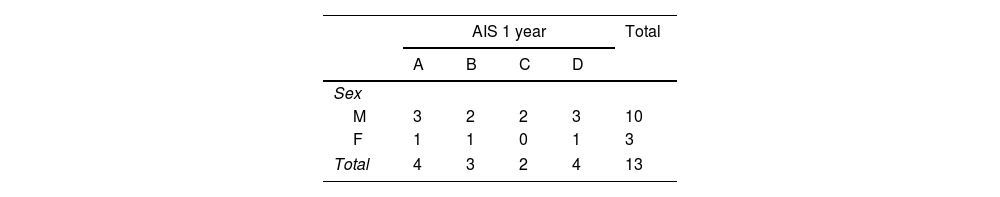
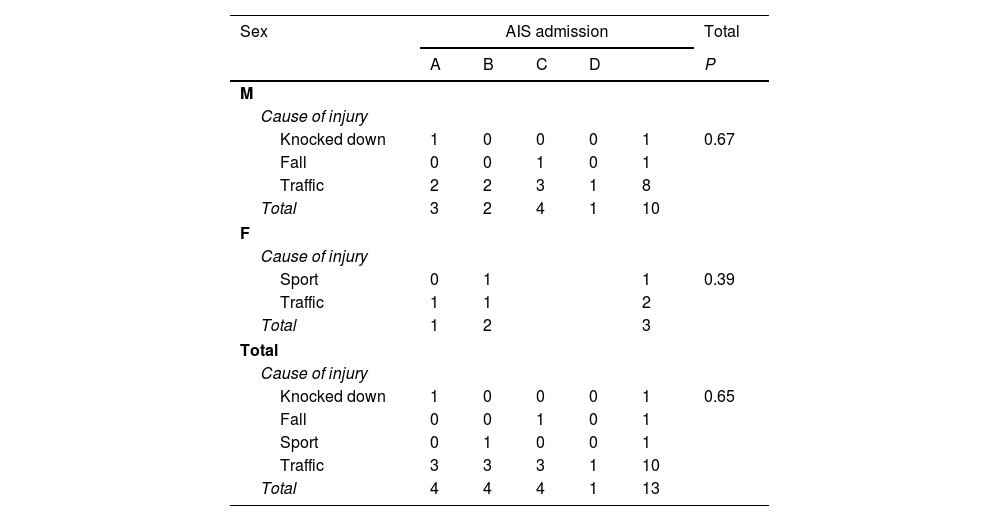
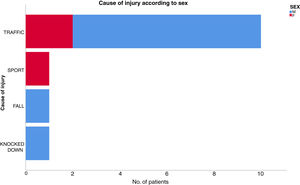
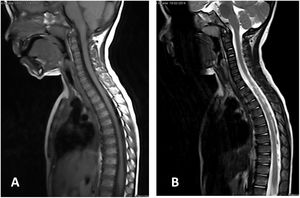
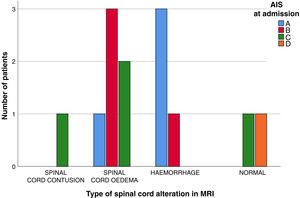
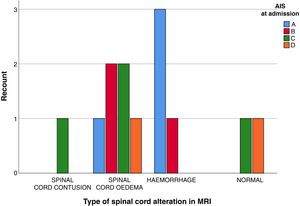
ResultsThirteen patients fulfilled the study inclusion criteria. Their median age was 4 years, with an interquartile range (IQR) of 16. The study population was composed of 3 females (23%) and 10 males (77%). 54% of the patients with SCIWORA corresponded to a cervical level, and C2 was the most frequent neurological level (22%), while T10 was the most common thoracic level (15%) (Table 1). A traffic accident was the main cause of the injury, in 77% of the cases (Fig. 1). In 12 patients the neurological symptoms commenced within the first 24h after the trauma, and in one patient they commenced 11 days after the trauma. The magnetic resonance image at the acute moment of the SCIWORA-type lesion was in 4 cases compatible with spinal bleeding (31%), while in 2 cases the images were compatible with normality (classic SCIWORA) (Fig. 2). The neurological presentation evaluated in our hospital on admission using the AIS scale was: complete sensory and motor deficit (AIS A) in 4 patients (31%), while 4 patients had complete motor deficit (AIS B), 4 patients were AIS C (31%) and one patient was AIS D (8%) (Fig. 3). The MRI scan of the spine and the AIS at admission showed that AIS A-type injuries corresponded to images compatible with spinal bleeding, while AIS B injuries corresponded to images that were compatible with spinal oedema (Fig. 4; Table 2). The proportions of AIS A and B-type lesions at one year are shown in Fig. 5. However, no statistically significant differences were found between the type of signal in MRI and the AIS scale at admission (P=0.11) or at discharge (P=0.33). Neurological evolution as expressed on the AIS at one year is shown in Table 3. 30% of the cases evaluated were found to have been subjected to NASCIS III-type therapy in the Emergency Department. Twelve patients in the series were treated conservatively, while one patient required surgical treatment in the form of decompressive laminectomy.
Cervical–dorsal MR image of a 3 year-old boy with a SCIWORA-type spinal cord injury after a traffic accident. Neurological level of the injury T9 AIS C, the weighted image of the spinal cord in T1 (A) and in T2 (B) is compatible with normality (classic SCIWORA). The patient had evolved favourably to AIS D one year after the injury.
Descriptive analysis of the type of signal found in MRI at admission and correlation of the same with the AIS scale at admission and discharge.
| AIS discharge | AIS admission | Total | |||
|---|---|---|---|---|---|
| A | B | C | D | ||
| A | |||||
| MRI (type of alteration) | |||||
| Spinal cord oedema | 1 | 1 | |||
| Haemorrhage | 3 | 3 | |||
| Total | 4 | 4 | |||
| B | |||||
| MRI (type of alteration) | |||||
| Spinal cord oedema | 2 | 2 | |||
| Haemorrhage | 1 | 1 | |||
| Total | 3 | 3 | |||
| C | |||||
| RM (type of alteration) | |||||
| Spinal cord contusion | 1 | 1 | |||
| Spinal cord oedema | 2 | 2 | |||
| Normal | 1 | 1 | |||
| Total | 4 | 4 | |||
| D | |||||
| RM (type of alteration) | |||||
| Spinal cord oedema | 1 | 0 | 1 | ||
| Normal | 0 | 1 | 1 | ||
| Total | 1 | 1 | 2 | ||
| Total | |||||
| RM (type of alteration) | |||||
| Spinal cord contusion | 0 | 0 | 1 | 0 | 1 |
| Spinal cord oedema | 1 | 3 | 2 | 0 | 6 |
| Haemorrhage | 3 | 1 | 0 | 0 | 4 |
| Normal | 0 | 0 | 1 | 1 | 2 |
| Total | 4 | 4 | 4 | 1 | 13 |
The SCIM III at admission was 28.5 points, and at discharge it was 42 points. The median duration of hospitalization was 62 days (2–270 days).
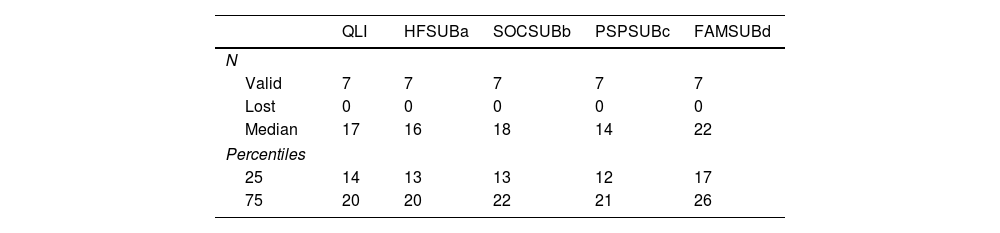
The NDI evaluated for the patients with SCIWORA at cervical level after an average follow-up of 10 years was 12, and the Oswestry score for those with a dorsal location was 15. The quality of life score for patients with spinal cord injury SV-QLI/SCI found a 25 and 75 median and percentile of 17 (14;20). The SV/QLI/SCI index contains scores corresponding to sub-scales associated with health and functionality (HFSUB), social and economic aspects (SOCSUB), psychological and spiritual factors (PSPSUB) and lastly ones in connection with family questions (FAMSUB). The results obtained were described in terms of the median and percentiles 25 and 75 (Table 4).
Result of the spinal cord injury patient quality of life questionnaire (SV-QLI/SCI).
| QLI | HFSUBa | SOCSUBb | PSPSUBc | FAMSUBd | |
|---|---|---|---|---|---|
| N | |||||
| Valid | 7 | 7 | 7 | 7 | 7 |
| Lost | 0 | 0 | 0 | 0 | 0 |
| Median | 17 | 16 | 18 | 14 | 22 |
| Percentiles | |||||
| 25 | 14 | 13 | 13 | 12 | 17 |
| 75 | 20 | 20 | 22 | 21 | 26 |
Subscales on health and functionality (HFSUB), social and economic aspects (SOCSUB), psychological and spiritual aspects (PSPSUB) and lastly in connection with family matters (FAMSUB). Results expressed as the median and 25–75 percentile.
No significant differences were found between the cause of the injury and the type of alteration detected by MRI (P=0.87). No statistically significant differences were found between the cause of the injury and the AIS at admission when stratified according to sex (P=0.65) (Table 5). This was also the case for age at the time of the injury and the AIS score at 5 years (P=0.65) or between age and the type of spinal cord injury detected by MRI (P=0.15). One death occurred during the study period, corresponding to a patient with SCIWORA at a neurological level corresponding to C1.
Descriptive analysis of the cause of injury with AIS scale associated with admission stratified according to sex.
| Sex | AIS admission | Total | ||||
|---|---|---|---|---|---|---|
| A | B | C | D | P | ||
| M | ||||||
| Cause of injury | ||||||
| Knocked down | 1 | 0 | 0 | 0 | 1 | 0.67 |
| Fall | 0 | 0 | 1 | 0 | 1 | |
| Traffic | 2 | 2 | 3 | 1 | 8 | |
| Total | 3 | 2 | 4 | 1 | 10 | |
| F | ||||||
| Cause of injury | ||||||
| Sport | 0 | 1 | 1 | 0.39 | ||
| Traffic | 1 | 1 | 2 | |||
| Total | 1 | 2 | 3 | |||
| Total | ||||||
| Cause of injury | ||||||
| Knocked down | 1 | 0 | 0 | 0 | 1 | 0.65 |
| Fall | 0 | 0 | 1 | 0 | 1 | |
| Sport | 0 | 1 | 0 | 0 | 1 | |
| Traffic | 3 | 3 | 3 | 1 | 10 | |
| Total | 4 | 4 | 4 | 1 | 13 | |
Given the functional repercussion of SCIWORA in the affected paediatric population, knowledge of main causes of this injury and how it evolves in functional terms is highly relevant and interesting.
Depending on the series in question, SCIWORA-type spinal injuries have an incidence of from 19% to 34% in paediatric age. The series analyzed show incidences of 87% with a cervical location and 13% at thoracic level.1,2,5 Although the thoracic region is more susceptible to more severe injuries, due to its more precarious nature of its vascularization and the distribution of outgoing roots, in this study we did not find that dorsal-level lesions were more severe than cervical-level ones.
The special anatomical characteristics of the spine during paediatric age mean that the highest concentration of patients affected by SCIWORA-type lesions varies from 0 to 6 years. Their age in our study was from 0 to 4 years, and this finding is very similar to another one described in the literature.3,5 The main causes of injury found in this study were traffic accidents followed by sports accidents. Nevertheless, several authors3–5 describe sport as the main cause of SCIWORA (41% of cases), followed by traffic accidents (26%) and falls (14%).
Neurological symptoms of a complete or incomplete spinal cord injury were found in our series during the first day in 92% of cases. Latency times were measured in hours (8h) and neurological symptoms commenced in one case after 11 days. Other authors such as Eleraky et al.,7 did not record latency times after the lesion and the appearance of neurological problems. Other papers in the literature recorded a delay in the appearance of SCIWORA in children at percentages of up to 27% of cases up to 4 days after the injury.1,2 In the same way as other authors, such as Rozzelle et al.,8 we consider that a child who has shown signs or symptoms of transitory neurological deficit without an objective neurological deficit identified by a radiographic imaging study may subsequently go on to develop a SCIWORA syndrome.
In our series, the presentation at admission was 8% AIS A and D in 8% at cervical level, and 23% AIS A, without finding any patient to be AIS D at a dorsal level at admission. Carroll et al.,5 in their systematic review, described how at admission 70% of the patients were classified as AIS D, and 17% as AIS A. Boese and Lechler9 show data that at admission 28% of the patients were AIS A and 17%, B, while 31% were C and 25% were D. In the AIS D cases the degree of complete recovery amounted to 97%. As was the case in our series, the neurological presentation correlated with the long-term functional state.1,2,5
In the same way as Bosch et al.,10 we found no deterioration in neurological function during hospitalization or during the evolution of the cases over years.
No patients were found who had achieved complete recovery (AIS E) at discharge or during follow-up in the case of the patients with incomplete paraplegia at admission. Nevertheless, neurological improvements were detected in patients classified as AIS B and who at discharge were classified as AIS D (one case of cervical SCIWORA) and in patients classified as AIS C who were classified as AIS D one year after discharge, in 2 cases (one cervical and the other thoracic).
The phenomenon of recurring SCIWORA is described in medical literature, defined as the occurrence of neurological symptoms days or weeks after the first episode.4 The incidence of this stands at 17% according to the series, and it has been observed that the incidence of this recurring phenomenon is lower in the group of patients who were immobilized during 12 weeks, in comparison with the group immobilized for 8 weeks. Recurrent SCIWORA generally leads to a more severe deficit than the original condition. No patient with recurrent SCIWORA was found in this study, and this may be due to the use of a 12 week period of immobilization.
Patients with a suspected spinal cord injury require radiographic imaging studies using X-rays and CT. In the same way as other authors, we consider MR imaging to be the gold standard for patients with a spinal cord injury.11,12
Boese and Lechler differentiate the findings of MRI studies in the spine into four types. Type I: no detectable pathology, and type II: abnormalities detected by MRI, subclassified as IIa: extraneural findings, IIb: intraneural findings, and IIc: intra and extraneural findings.9 The absence of MRI signal changes is associated with an excellent evolution. Changes in the MRI signal consistent with oedema or micro-haemorrhages are associated with a significant improvement over time.13 The presence of a massive haemorrhage is associated with a severe and permanent neurological lesion.14,15
To treat patients of this type the recommendation is to use external immobilization during a 12-week period, followed by restricted activities during 6 months.16–18 Rigid immobilization was used in our series regardless of the level of the neurological lesion. A rigid collar was used to immobilize the neck in the cervical region, while a shaped corset was used in the thoracic region. Both of these systems were used for the maximum possible number of hours, and they were only removed for personal hygiene during 12 weeks. Immboilization during 12 weeks has been proven to be more effective in preventing recurrent SCIWORA than immobilization for 8 weeks.19 However, some authors who found no recurrent SCIWORA when applying orthosis for 12 weeks therefore recommend an individualized approach in each case, especially in those where there is no cervical instability.8,10 Imaging tests should be performed every 3 months or before the removal of the immobilization. X-ray imaging studies in flexo-extension should be used to ensure that there is no associated cervical instability. Immobilization with a thoracolumbar orthosis is used in the majority of thoracic lesions.20,21 Traction or laminectomy are not indicated as treatment for thoracic SCIWORA.
Our study found an 8% mortality rate, corresponding to the patient with a neurological lesion at level C1, with the respiratory complications that this involves. Knox cites figures close to 2%.3
The most outstanding limitation of this study is that one of its parts is retrospective, so that some findings are restricted by the data contained in each clinical history. Nevertheless, the loss of data was minimum because of the prospective recording of the same by the research team. We also believe that our study may have a severe distortion due to the referral of patients to our centre from other hospitals. This is because they will predominantly have referred the cases with the most severe symptoms. The small size of the sample is another limitation, as this may reduce the power of the study and influence the non-detection of significant associations in the comparisons made between groups. However, one of the strengths of this study that we underline is that its sample is representative of the population, and that its data may be extrapolated to the paediatric population. The patients affected by SCIWORA were followed-up for an average of 10 years, one of the longest periods in the literature that was reviewed. There are very few scientific studies of this subject, so that this work helps to broaden the data on the epidemiology and functional status of these patients.
Studies with a prospective methodology are required that are able to evaluate different lengths of time of conservative treatment or restricted physical activity, above all for those patients without ligament injuries within the context of SCIWORA.
ConclusionSeventy-seven percent of the patients affected by a SCIWORA-type spinal cord injury are under the age of 8 years. One year after discharge from hospital 31% of these patients are classified as AIS D, and this percentage remains constant after 5 years. Orthopaedic treatment using immobilization of the affected segment during 12 weeks is effective in the treatment of SCIWORA and in the prevention of recurrent SCIWORA. No statistically significant differences were found between the cause of the injury and the type of alteration found by MRI technique (P=0.872), between the age at the time of injury and the AIS at 5 years (P=0.647) or age and the type of spinal cord injury found by MRI (P=0.149).
Level of evidenceLevel of evidence ii.
Conflict of interestsThe authors have no conflict of interests to declare.
FundingThe authors declare that they have received no funding for the conduct of the present research, the preparation of the article, or its publication.
Right to privacy and informed consentThe authors have obtained informed consent from the patients and/or subjects referred to in the article. This document is held by the corresponding author.
Ethics committee approvalEthics Committee Hospital Universitario de Toledo.