Femoroacetabular impingement is probably the most common mechanism that leads to the development of early cartilage and labral damage in the non-dysplastic hip. The objective was to evaluate the outcomes of hip arthroscopy as a treatment for femoroacetabular impingement in patients with high level of function.
Material and methodsA prospective study was performed on 41 patients younger than 40 years old undergoing hip arthroscopy for femoroacetabular impingement. Modified Harris Hip Score and HOS and IHOT questionnaires were used for clinical assessment. Radiological evaluation was made for joint space and alpha angle.
ResultsThe mean age of patients was 32.7 years. Labrum injury was detected in 78%, and acetabular cartilage injury in 56% of cases. The average follow-up was 31.3 months. There was a significantly improvement in the mean score in the clinical questionnaires. Radiologically there was no change in the mean joint space, with significantly reduction to normal values of the alpha angle. All patients returned to sports at their pre-injury level of function.
DiscussionHip arthroscopy resulted in improvement in hip functional outcomes with correction of the underlying osseous deformity and treatment of the associated labral and cartilage pathology, with the return of patients to their pre-injury sports. Further follow-up is essential to confirm the stability of the clinical and radiological outcomes.
El choque femoroacetabular es el mecanismo más común descrito en la literatura que conduce a la lesión del labrum y del cartílago articular en la cadera no displásica. Nuestro objetivo fue determinar los resultados clínicos y radiológicos de la cirugía artroscópica de cadera como tratamiento del choque femoroacetabular en pacientes jóvenes con alta demanda funcional.
Material y métodosEstudio prospectivo de 41 pacientes menores de 40 años tratados mediante cirugía artroscópica de cadera por choque femoroacetabular. Para valoración clínica se utilizaron la escala modificada de Harris, cuestionarios de valoración HOS e IHOT12. Se realizó una valoración radiológica para determinar altura articular y ángulo alfa.
ResultadosLa edad media de los pacientes fue de 32,7 años. Se detectó lesión del labrum en el 78% y del cartílago acetabular en el 56% de los casos. El seguimiento medio de los pacientes fue de 31,3 meses. Hubo una mejora significativa en la puntuación media en los cuestionarios de valoración clínica. Radiológicamente no se modificó la altura media del espacio articular, con reducción significativa a valores normales del ángulo alfa. Todos los pacientes se reincorporaron a su actividad deportiva habitual previa.
DiscusiónLa cirugía artroscópica de cadera ha permitido la mejoría clínica de los pacientes con corrección de la deformidad ósea, lesión labral y cartilaginosa, y reincorporación de los pacientes a sus actividades deportivas previas a la cirugía. Es fundamental un mayor seguimiento para confirmar la estabilidad de los resultados clínicos y radiológicos obtenidos.
The effectiveness of arthroscopic procedures in the knee, shoulder and ankle has been well-established and their extensive use by Traumatology and Orthopedic Surgery Services has enabled the development of the corresponding instrumentation in recent decades. This experience has been extrapolated to the hip joint; however, the hip presents specific characteristics. It is an enarthrosis enveloped in a capsule, ligaments and muscles in a deep anatomical location, which requires specific, longer and more flexible instrumentation. The technical complexity and long learning curve associated lead to an initial rejection of the incorporation of arthroscopy hip surgery (AHS) into the range of services provided at our hospitals. Initially, AHS was indicated as a diagnostic procedure, but a better understanding of hip pathology and improvement of the instrumentation have led to an increase in the number of therapeutic procedures.1,2
According to the literature, femoroacetabular impingement (FAI) is the most common mechanism of injury of the labrum and joint cartilage of non-dysplastic hips of young patients. The relation with sports activities involving flexion-adduction-internal rotation and combined movements is progressively increasing. Different surgical techniques to correct the deformity and treat lesions of the labrum and joint cartilage have been reported, including safe dislocation with ample exposure of the joint, minimally invasive anterior approaches and AHS.3–5 Safe dislocation is the benchmark technique for the treatment of FAI, although recent systematic reviews comparing it to AHS have questioned its superiority.6,7
Our working hypothesis was that AHS is an effective technique for the treatment of FAI in young male athletes with high, short-term functional demands. In order to verify this hypothesis, our main objective was to assess the clinical and radiographic results obtained with AHS following FAI among male athletes aged under 40 years. The secondary objective was to determine whether AHS was able to correct the characteristic anatomical alterations of FAI.
Materials and methodsSince 2009, our prospective database registered all patients intervened through AHS. From this database we selected patients who fulfilled the following criteria: age under 40 years, male gender, high-intensity sports physical activity, diagnosis of FAI (Cam, Pincer or mixed type) and Tönnis stage 0–2. The diagnosis of FAI was established based on the anamnesis, positive pincer maneuver in exploration and pathognomic radiographic signs. The assessment of AHS results in this study required a minimum postoperative follow-up period of 12 months.
We excluded patients with hip dysplasia determined by a centre-edge angle less than 25°, Legg-Calve-Perthes disease, prior hip surgery and age under 18 years. All the patients gave their informed consent for inclusion in the study and the study was approved by the clinical research ethics committee of our centre.
Surgical protocolAll interventions were carried out by a surgeon experienced in AHS (JM), in a room with laminal flow and under spinal anesthesia. Patients were placed in the supine position on a traction table with perineal and foot protection. The anterolateral, medial-anterior and distal anterior portals were used. When combined, these offer an excellent view of the entire coxofemoral joint. The central compartment was systematically explored at the outset in order to detect any excess of acetabular coverage and lesions of the labrum, round ligament and joint cartilage.
Labral8 and joint cartilage9 lesions were assessed in the 6 areas described by Ilizariturri.10 Acetabular and femoral osteoplasty were carried out under direct view and radioscopic control with a high-speed 5.5mm drill. None of the cases in the series underwent capsular repair.
All patients underwent an intraoperative infiltration of platelet-rich plasma. Two additional infiltrations were added in all cases requiring microfractures, the first 1 month after surgery and the second 2 months after the surgery.
Postoperative managementAll patients followed the same postoperative pain and rehabilitation protocol. Patients were discharged after 24h and partial load with crutches was allowed on the intervened hip. Passive mobility was initiated in the immediate postoperative period, with restriction of rotations for 4 weeks and thereafter initiating the specific rehabilitation protocol. No orthesis which restricted hip mobility were used.
AssessmentsThe preoperative and postoperative clinical assessments were carried out with the modified Harris Hip Score (mHHS),11 the Hip Outcome Score with the sections for Activities of Daily Living (HOS-ADL) and Sports-Specific Subscale (HOS-SSS),12 and the International Hip Outcome Tool (IHOT12) questionnaire measuring quality of life.13 Patients also responded to 2 questions during each assessment: “How would you define your function in activities of daily living and sports activities, assigning a score between 0 and 100; with 100 being your level prior to the onset of the hip problem and 0 a total inability to carry out such activities?” and “Do you consider that your level of activity is normal, near to normal, abnormal or severely abnormal?”. Patients were postoperatively assessed after 3, 6 and 12 months, and annually thereafter.
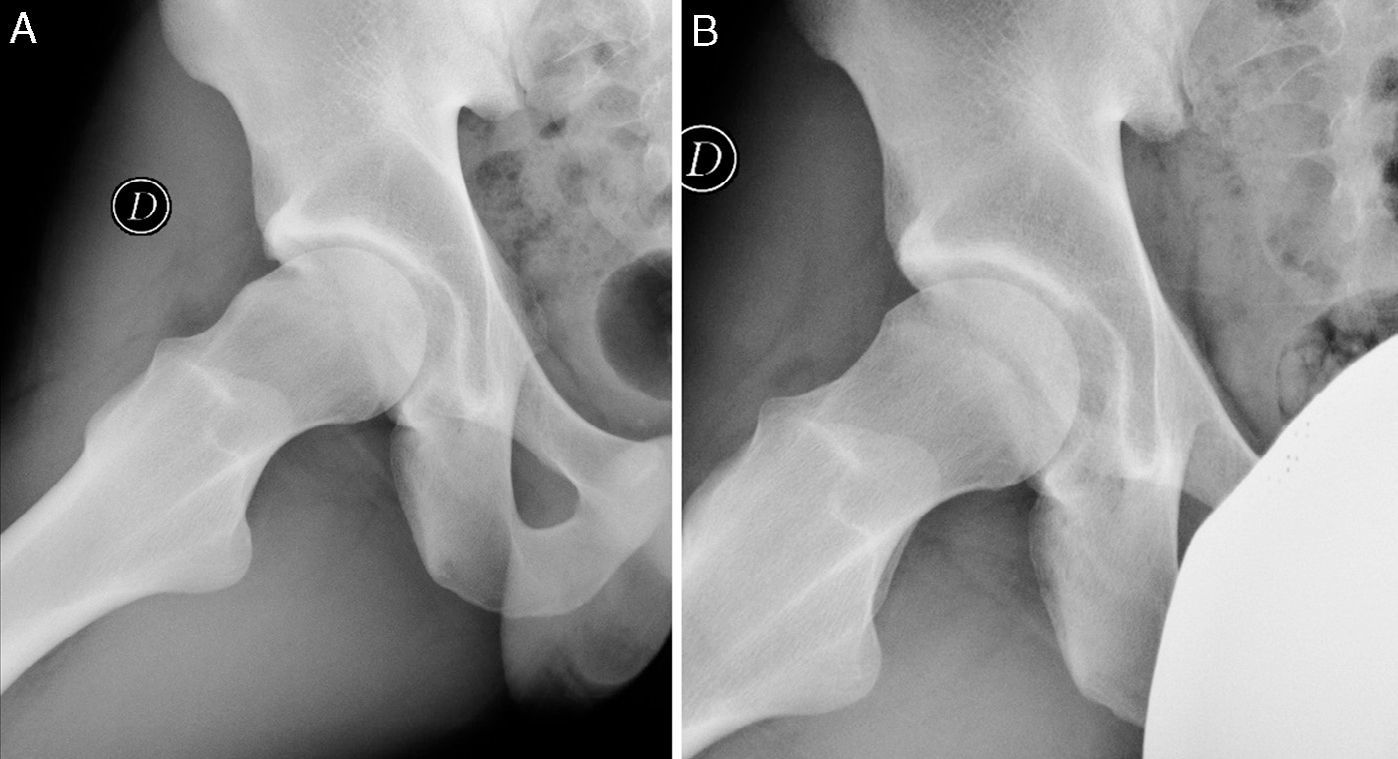
We obtained anteroposterior radiographs of the pelvis whilst standing and Dunn axial projections preoperatively in a digital format. Pincer-type lesions were determined by the presence of cross-over sign or superposition of both the anterior and posterior walls, and by the prominence of the ischiatic spine in the pelvic radiograph whilst standing. Cam-type lesions were established by the presence of the pistol grip sign in the anterosuperior femoral head-neck union (Fig. 1A).5 The height of the joint interline was measured in the load area of the pelvic anteroposterior projection.14 In addition, the alpha angle in the Dunn axial projection was also measured.5 Degeneration of the coxofemoral joint was determined according to the Tönnis scale.15 A preoperative magnetic resonance imaging (MRI) scan was requested in all cases in order to detect the presence of avascular necrosis and lesions of the labrum and joint cartilage. An anteroposterior radiographic study whist standing was requested during postoperative assessments in order to determine the height of the joint interline and the level of joint degeneration according to the Tönnis scale, as well as a Dunn axial projection to determine the alpha angle.
Statistical analysisThe statistical analysis was performed using the software package SPSS, version 15.0 (SPSS Inc., Chicago, US). We considered as significant values of P≤0.05. We used the Kolmogorov–Smirnov test to determine normal distributions. To establish comparisons we carried out univariate analysis for categorical variables through the Chi-square test for variables with a normal distribution and the Mantel–Haenszel test for non-parametric data, whilst in continuous variables we used the Student t test and the Mann–Whitney U test.
ResultsGeneral preoperative dataA total of 162 hips were intervened by AHS at our service between January 2009 and December 2013. Of these, 41 fulfilled the criteria for inclusion in the study. All were males, with a mean age of 32.7 years (range: 18–40 years; SD: 6.7 years). The right hip was affected in 21 patients and the left in 20, whilst 7 arthroscopies were bilateral (34.1%). A total of 18 patients (52.9%) attended consultation with a prior diagnosis, with tendinitis of the hip abductor muscles, pubic osteopathy and lumbar discopathy being the most frequent. All patients practiced high-intensity sports activity: long distance running (11 patients), football (7 patients), paddle tennis (7 patients), basketball (5 patients), swimming (2 patients) and martial arts (2 patients).
The mean period elapsed from the start of symptoms until surgery was 19.6 months (range: 3 to 60 months; SD: 15.0 months).
Preoperatively, all patients presented radiographic signs of Cam-type lesion. The radiographic signs of Pincer-type lesion were detected in 16 hips (39.1%). In total, 25 hips presented Cam-type FAI mechanism (60.9%), whilst 16 cases (39.1%) presented a combined FAI mechanism (Cam+Pincer). The mean height of the joint space of the hip in the anteroposterior pelvic projection was 4.8mm (range: 3.2 to 6.5mm; SD: 0.8mm). The mean value of the alpha angle in the Dunn axial projection was 64.6° (range: 57°–77°; SD: 7.6°). According to the Tönnis classification there were 25 hips with Tönnis O (61%), 13 with Tönnis 1 (31.7%) and 3 with Tönnis 2 (7.3%). The level of preoperative radiographic joint degeneration according to the Tönnis classification was significantly related to the time of evolution of symptoms until surgery (P=0.002).
The preoperative MRI showed a labral lesion in 13 hips (31.7%) and a cartilage lesion in 1 hip (2.7%).
Findings and arthroscopic treatmentArthroscopically, Cam-type lesions were present in all hips and Pincer-type lesions in 16 hips (39.1%). Acetabular overgrowth or Pincer-type lesions were determined by the presence of diffuse ecchymosis of the labrum, labral ossification, intralabral cystic degeneration and/or by the extension of the acetabular edge beyond the chondrolabral junction.16
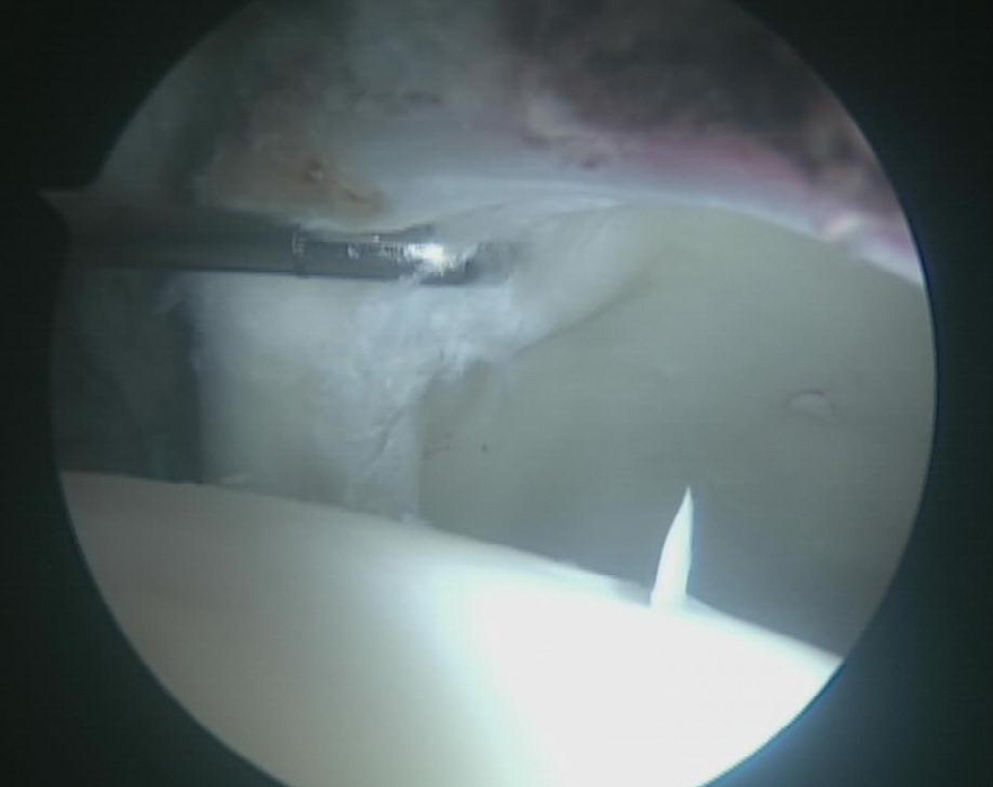
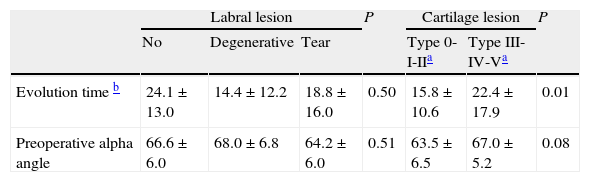
We detected labral tears (Fig. 2) with loss of the sealing function of the femoral head in 28 hips (68.3%), labral degeneration without loss of the sealing function in 5 hips (12.2%), and 8 hips (19.5%) with no labral lesion. Labral lesions were located in areas 2 and 3 in 81.8% of cases. There was no correlation between labral tear and the time of evolution of the symptoms (P=0.50) or with the preoperative value of the alpha angle (P=0.51) (Table 1).
Arthroscopic findings.
| Labral lesion | P | Cartilage lesion | P | ||||
| No | Degenerative | Tear | Type 0-I-IIa | Type III-IV-Va | |||
| Evolution time b | 24.1±13.0 | 14.4±12.2 | 18.8±16.0 | 0.50 | 15.8±10.6 | 22.4±17.9 | 0.01 |
| Preoperative alpha angle | 66.6±6.0 | 68.0±6.8 | 64.2±6.0 | 0.51 | 63.5±6.5 | 67.0±5.2 | 0.08 |
Scores shown as mean±standard deviation.
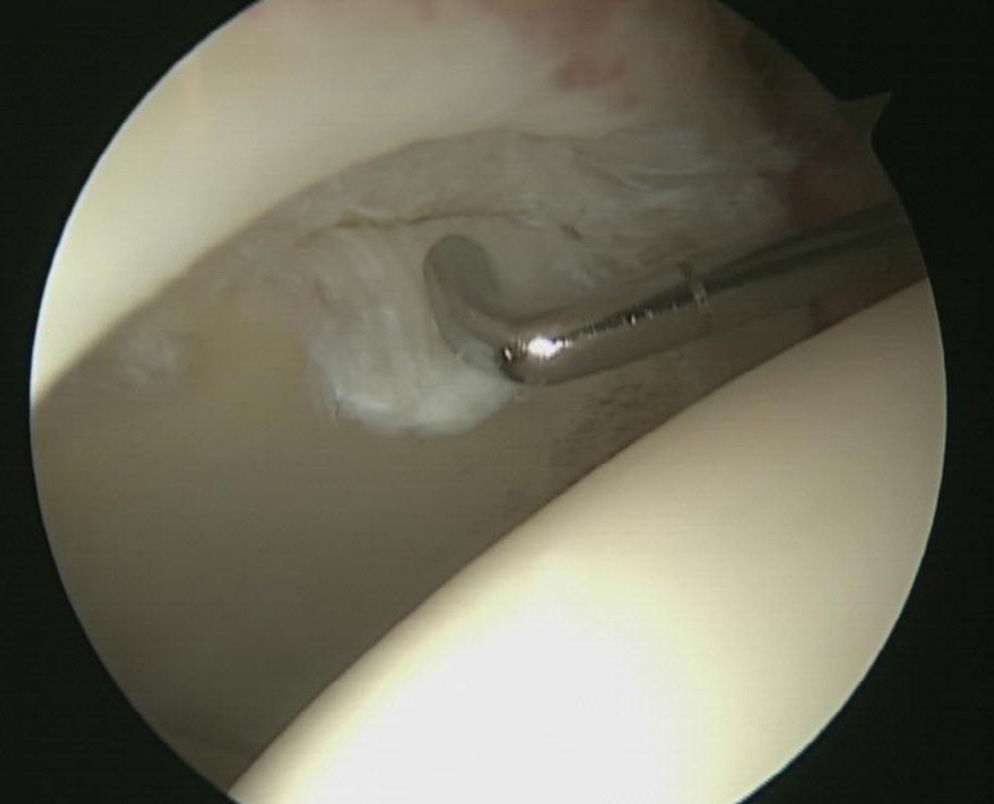
Lesions of the joint cartilage were observed in 23 hips (56.1%), classified according to the Mahorn system into 2 type II, 2 type III, 8 type IV (Fig. 3) and 11 type V. In total, 9.5% of the joint cartilage lesions were located in areas 2 and 3. No cartilage lesions were detected in the femoral head. The grade of cartilage lesion was significantly related to the time of evolution of the symptoms until surgery (P=0.01) although not to the preoperative value of the alpha angle (P=0.08) (Table 1).
Inflammatory alterations located in the anterior labrum (area 1), indicating impingement of the iliopsoas tendon,17 were detected in 2 hips.
Pincer resection was carried out in 16 hips (39.1%) and femoral osteochondrodysplasia in all cases (Fig. 1B).
In labral tears with loss of the sealing function of the femoral head, the labrum was stabilized with a mean 2.1 harpoons (range: 1-3 harpoons) (Pushlock® 2.9mm, Arthrex inc. Naples, FL, US). In cases suffering labral degeneration, the lesion was resected with an oscillating saw, preserving the labrum insofar as possible without affecting the sealing function of the femoral head.
Full-thickness cartilage lesions were treated through microfractures, whereas the rest underwent debridement with an oscillating saw.
Hips presenting signs of impingement of the iliopsoas tendon underwent transcapsular tenotomy in the central compartment, at the level of anterior acetabular bone ridge, only sectioning the tendinous part of the psoas muscle.17
Functional assessment and quality of lifeA total of 6 hips (5 patients) with a follow-up period under 12 months were excluded from the assessment of results.
The mean follow-up period of the patients was 31.3 months (range: 12–57 months; SD: 12.21 months).
The mean score in the mHHS went from 77.17 points (range: 51.70–90 points; SD: 9.1 points) points preoperatively to 97.1 points (range: 83.7–100 points; SD: 5.1 points) at the end of the follow-up period (P<0.001). In the HOS-AVD scale, the mean score increased from 65.1 points (range: 32.8–91.6 points; SD: 14.9 points) to 97.7 points (range: 90.0–100 points; SD: 3.5 points) (P<0.001), whilst in the HOS-SSS scale it went from 28.6 points (range: 0–66.7 points; SD: 18.4 points) to 95.4 points (range: 84.3 to 100 points; SD: 5.9 points) (P<0.001). In the IHOT12 questionnaire, the score increased from 34.3 points (range: 12.5–65.6 points; SD: 34.3 points) to 96.0 points (range: 75.0–100 points; SD: 7.4 points) (P<0.001).
The score assigned by patients to their function in the scale from 0 to 100 in activities of daily life increased from 52.7 points (range: 30 to 90 points; SD: 14.0 points) to 99.1 points (range: 90–100 points; SD: 2.5 points) (P<0.001); and with respect to their function for sports activities from 18.8 points (range: 0–40 points; SD: 15.1 points) to 95.2 points (range: 75–100 points; SD: 6.9 points) (P<0.001).
The question about how patients described their level of activity received a preoperative response of severely abnormal by 80% of patients and abnormal by 20%; whilst, at the end of the follow-up period, 83.3% of patients described it as normal and 16.7% as close to normal.
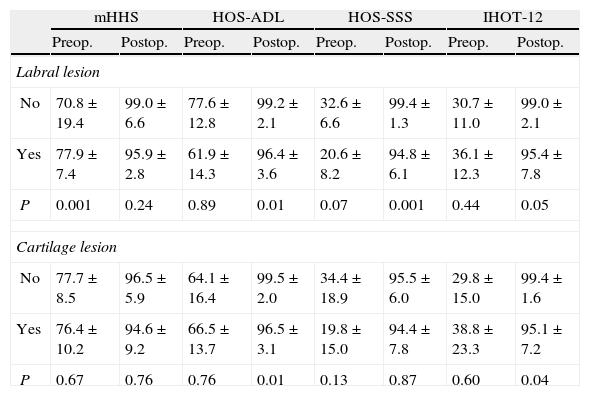
There were no significant differences in the clinical result between patients with combined FAI mechanism versus patients with a Cam-type mechanism (P>0.05). However, patients who did not present lesions of the labrum or the joint cartilage had a higher score in the clinical assessment questionnaires. Statistical significance was not observed in mHHS, but was observed in the HOS-AVD, HOS-SSS (only in cases without labral lesion) and IHOT12 tools (Table 2).
Functional results.
| mHHS | HOS-ADL | HOS-SSS | IHOT-12 | |||||
| Preop. | Postop. | Preop. | Postop. | Preop. | Postop. | Preop. | Postop. | |
| Labral lesion | ||||||||
| No | 70.8±19.4 | 99.0±6.6 | 77.6±12.8 | 99.2±2.1 | 32.6±6.6 | 99.4±1.3 | 30.7±11.0 | 99.0±2.1 |
| Yes | 77.9±7.4 | 95.9±2.8 | 61.9±14.3 | 96.4±3.6 | 20.6±8.2 | 94.8±6.1 | 36.1±12.3 | 95.4±7.8 |
| P | 0.001 | 0.24 | 0.89 | 0.01 | 0.07 | 0.001 | 0.44 | 0.05 |
| Cartilage lesion | ||||||||
| No | 77.7±8.5 | 96.5±5.9 | 64.1±16.4 | 99.5±2.0 | 34.4±18.9 | 95.5±6.0 | 29.8±15.0 | 99.4±1.6 |
| Yes | 76.4±10.2 | 94.6±9.2 | 66.5±13.7 | 96.5±3.1 | 19.8±15.0 | 94.4±7.8 | 38.8±23.3 | 95.1±7.2 |
| P | 0.67 | 0.76 | 0.76 | 0.01 | 0.13 | 0.87 | 0.60 | 0.04 |
HOS-ADL: Hip Outcome Score with sections for Activities of Daily Living; HOS-SSS: Hip Outcome Score with Sports-Specific Subscale; IHOT12: International Hip Outcome Tool; mHHS: modified Harris Hip Score; Preop.: preoperative value; Postop.: postoperative value.
Scores shown as mean±standard deviation.
The mean height of the joint space of the hip in the anteroposterior pelvic projection was of 4.9mm (range: 3.0–5.9mm; SD: 0.7mm) at the end of the follow-up period, similar to the preoperative value (P=0.88). The mean value of the alpha angle was 43.0° (range: 25°–49°; SD: 5.9°) in the Dunn axial projection at the end of the follow-up period, with a significant difference with respect to the value prior to AHS (P<0.001). One hip presented progression to joint degeneration, going from a preoperative Tönnis 2 to Tönnis 3, 2 years after the intervention.
Complications and surgical revisionsComplications included 3 patients with postoperative paresthesias (2 of the pudendal nerve and 1 of the femorocutaneous nerve), and 1 patient with erectile dysfunction. All were resolved spontaneously 3 months after the operation.
None of the patients required surgical revision through arthroscopic surgery or total hip arthroplasty at the end of the follow-up period.
DiscussionThe effectiveness of AHS in the treatment of FAI has been demonstrated and the results obtained are comparable to those of open surgery.1,2 The minimally invasive approach to soft tissues and bone structures enables a rapid recovery with immediate mobilization and load, avoiding muscle atrophy and prolonged bed rest. Young patients with a high level of sports activity are more sensitive to these changes and could benefit from AHS.
FAI is an increasingly well-known pathology in our specialty. The symptoms and exploration allow a high level of suspicion of FAI. The radiographic study reveals the typical cross-over and pistol grip signs and must constitute the initial imaging test. Nevertheless, MRI with and without contrast presents higher sensitivity and specificity for the diagnosis of intraarticular pathology associated to labral and cartilage lesions. In our study, low percentages of detection of labral and joint cartilage lesions are explained by the lack of routine use of MRI with contrast.2–5Various reports in the literature2–5,18 have related labral tears and joint cartilage lesions to Cam and Pincer-type deformities.
The sealing effect of the labrum on the femoral head is essential to maintain hip stability and protect the joint cartilage.19 Repair of the labrum has been associated with better short and medium term results than resection of the labral lesion.8 More recent studies conducted on cadavers have shown a recovery of the normal values of intraarticular pressure20 and greater resistance of the joint to distraction forces when conducting sutures or reconstructions of the labrum, compared to total or partial resection.21 On the other hand, Farjo22 and Santori23 reported favorable results after 3.5 years, Mehtaf24 after 8.4 years and Byrd25 after 10 years of the resection of the labral lesion in patients with no associated arthritis. Most labral lesions are found in an anterior position.26 In our study, we detected lesions of the labrum in 80.5% of cases, the location of the lesions was also anterior, there was no significant relationship with the time of evolution of the symptoms and patients who did not require treatment for labral lesions presented better functional results.
A high percentage of patients intervened through AHS presented associated lesions in the joint cartilage, even without degenerative signs in the preoperative radiographic study. Lesions of the joint cartilage at the chondrolabral level are considered part of early coxofemoral joint degeneration. The treatment of full-thickness cartilage lesions is controversial, given the limited capacity for regeneration of the joint cartilage. The good results obtained through microfractures for the treatment of these lesions in other joints have promoted their use in the hip joint, with favorable results in terms of reincorporation of patients to their prior sports activity.27–29 Philippon30 carried out revision AHS in 9 patients after 20.7 months from the previous AHS, involving microfractures in the lesion of the joint cartilage, and observed coverage of the lesion between 95 and 100% in 8 cases. Karthikeyan31 reported similar results in 19 out of 20 patients at 17 months of the AHS with lesion of the joint cartilage treated through microfractures. In our study, 56.1% of patients presented joint cartilage lesions at the level of the acetabulum, in most cases in an anterior location, with a severe grade in 91.3% of cartilage lesions and with significant relationship with the mean time of onset of the symptoms. The presence of joint cartilage lesions has been associated to a lower increase of the improvement reflected in assessment questionnaires. However, the subgroups of patients with cartilage lesions, and even patients with full-thickness cartilage lesions, presented better results compared with the preoperative situation, and the microfractures enabled patients to return to their previous functional situation.
The literature contains several descriptions of functional assessment questionnaires for patients with hip pathology. However, not all have proven to be valid for use in patients intervened through AHS. The questionnaire by Harris was modified and adapted (mHHS) for the functional assessment of patients intervened through AHS,11 but it does not contemplate data about sports activities. Thus, given the characteristics of our series, we considered it convenient to use the HOS questionnaire which includes data about activities of daily living (HOS-ADL) and a sports-specific subscale (HOS-SSS).12 In order to determine the impact of this pathology and the results in terms of quality of life of patients, we added the IHOT-12 questionnaire,13 validated with respect to the initial IHOT-33 questionnaire.32 We used the version translated into Spanish by the International Society for Hip Arthroscopy (www.isha.net). The functional results in our study were satisfactory in the assessment questionnaires employed. Our patients performed sports activities with high functional demands, so they presented the lowest scores in the sports activity assessment scale, with a clear effect on the assessment of quality of life. The AHS increased the score in all the assessment questionnaires, and particularly in those referring to sports activities and quality of life. Up to 83.3% of patients reported a normal activity after the AHS. These results are comparable to other studies published in the literature with series and function and quality of life questionnaires which were similar to ours.33–35 The height of the joint space was a poor prognosis factor for the final results when it presented preoperative values under 2–3mm.24 Philippon36 measured the joint space in 3 areas; however, since the lowest value was in the middle or load area, in our study we only carried out the measurement in that area. All the patients in our series presented a joint space height over 3mm in the preoperative radiographic study. There was no significant decrease of the joint space between the preoperative period and the last review. The anteroposterior pelvic radiograph whilst standing presented a limitation for the measurement of the joint space due to the need for a correct radiographic technique to adequately assess the joint space and acetabular cover. The axial or false profile projection shows a reduced joint space, but also eliminates the effect of the load on the joint narrowing.
The alpha angle defines the concavity in the head-neck union.2,5 Higher alpha angle values have been related to the presence of labral and joint cartilage lesion,36 which is not reproduced in our series. The AHS enabled a correction of the alpha angle by a mean 21° and in all patients the postoperative value was below 50°.
Joint degeneration is another factor for poor prognosis for the final result, as reported in the literature.24 The presence of advanced degenerative signs is associated to worse functional results and should be discussed with patients prior to conducting AHS. In our series, 3 patients presented Tönnis grade 2 joint degeneration and 1 of them showed progression of the degeneration to Tönnis 3 during the follow-up period. The grade of preoperative joint degeneration was significantly related to the time of evolution of the symptoms.
An MRI scan can show changes in the cartilage, labrum, capsule and joint space.37 This requires MRI devices with a minimum field of 1.5 Tesla, although field strengths of 3 Tesla have recently been used. Moreover, arthro-MRI improves the contrast resolution and makes intraarticular pathology more evident, with a sensitivity of 90% and a specificity of 91%; which can be increased when conducted under traction.38
Despite being a minimally invasive procedure, AHS is not without complications. In a review article on AHS, Griffiths1 indicated a rate of complications of 1.4%, in most cases related to traction. Harris39 carried out a systematic review of 92 studies which included 6,134 patients and established a rate of 0.58% for major complications and 7.5% for minor complications. Most complications were minor and were related to traction, nerve neuropraxia (femoral, sciatic or pudendal), and to the experience of the surgeon. Nevertheless, this fact should be commented with patients and requires an informed consent form to be signed. In our series there were 4 minor complications (9.7%) which were resolved spontaneously.
The main objective of the study was to assess the results of AHS in male athletes aged under 40 years and with high functional demands, with a diagnosis of FAI. The study has shown satisfactory short-term results. The strengths of this study were its prospective design, the homogeneity of the series and the fact that all surgical procedures were carried out by the same surgeon. It greatest weaknesses are the short follow-up period and the lack of a control group. AHS has enabled a clinical improvement of patients with correction of the bone deformity, labral and cartilage lesion, and the reincorporation of patients to their sports activities prior to the surgery. A longer follow-up period is essential to confirm the stability of the clinical and radiographic results obtained.
Evidence levelEvidence level IV.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThe authors declare that they have not received financing for this work.
Conflicts of interestThe authors have no conflict of interests to declare.
Please cite this article as: Más Martínez J, Morales-Santías M, Bustamante Suarez Suarez de Puga D, Sanz-Reig J. La cirugía artroscópica de cadera en deportistas varones menores de 40 años con choque femoroacetabular: resultado a corto plazo. Rev Esp Cir Ortop Traumatol. 2014;58:343–350.