Although the correction of knee flexion by lengthening the hamstring musculature is traditionally contemplated in cerebral palsy, literature suggests that treatment of hip flexion also improves knee extension. The aim of the study was to first show the efficacy of the sequence of intrapelvic tenotomy of the psoas followed by intramuscular lengthening of the proximal rectus anterior and, later, that of both surgical soft tissue surgeries separately. For this, a prospective study was carried out in 10 patients with a mean age of 14 years, which presented 16 fixed knee flexes with a mean of deformity of 22°.
The data was analyzed through means of an ANOVA of repeated measures and to determine the effect separately of each one of the techniques, the improvements obtained with respect to the previous level were contrasted.
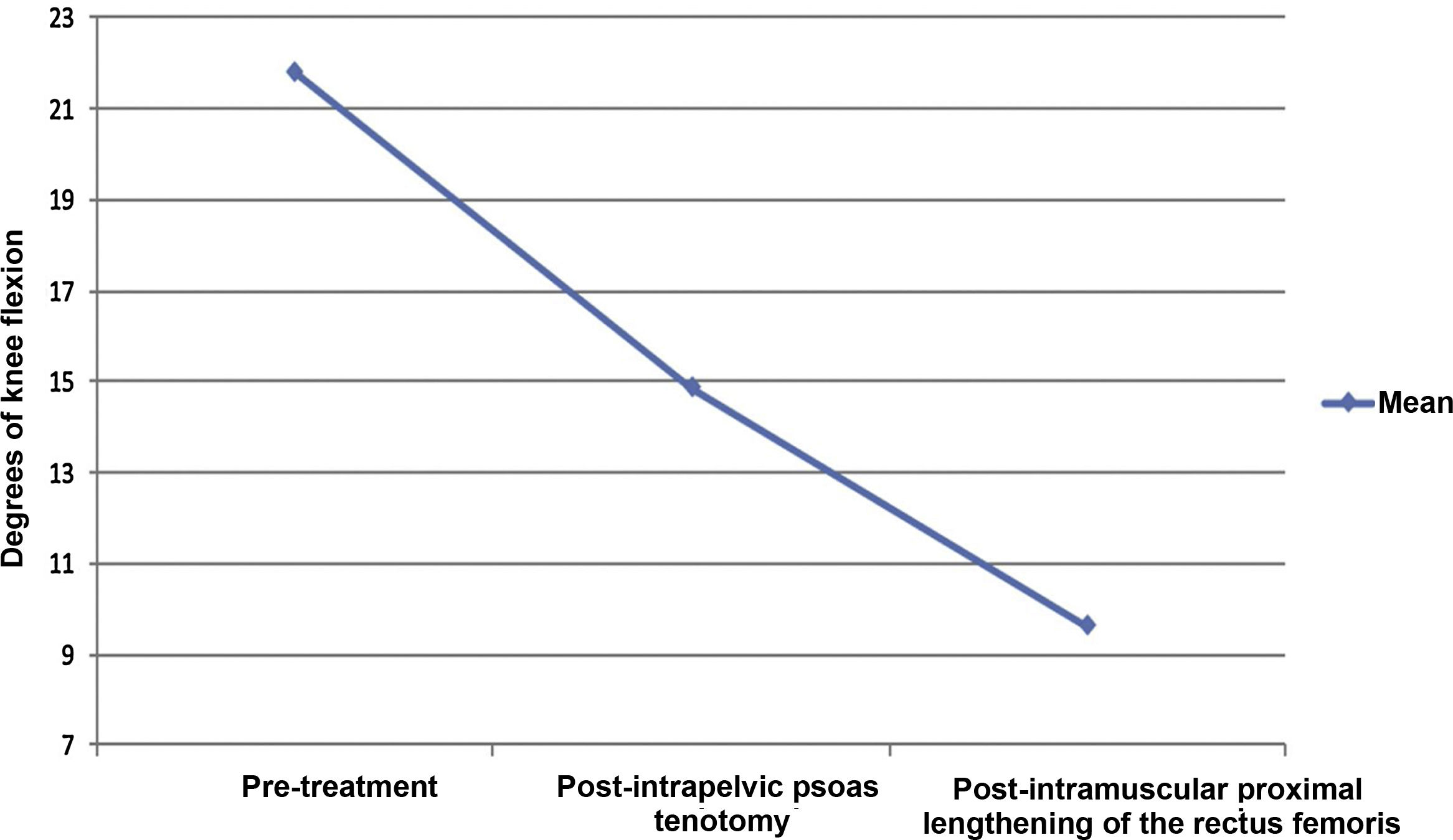
The mean extension achieved was 12°, 7° corresponding to the intrapelvic tenotomy of the psoas and, on the remaining knee flexion, a correction of 5° after intramuscular lengthening of the anterior rectus at the proximal level.
Both the sequence of proposed gestures and those that form separately, showed statistically significant differences (p < 0.001) in the correction of the deformity.
In conclusion, the proposed techniques applied sequentially or separately are effective in reducing knee flexion in predominantly spastic cerebral palsy, facilitating or even being able to avoid the treatment that is directly needed.
Aunque tradicionalmente se contempla en la parálisis cerebral infantil la corrección del flexo de rodilla mediante el alargamiento de la musculatura isquiocrural, la bibliografía sugiere que el tratamiento del flexo de cadera mejora igualmente la extensión de la rodilla. El objetivo del estudio fue mostrar primero la eficacia de la secuencia de la tenotomía intrapélvica del psoas seguida del alargamiento intramuscular del recto anterior y, posteriormente, la de ambos gestos por separado. Para ello se realizó un estudio prospectivo en 10 pacientes con una edad media de 14 años, que presentaban 16 flexos fijos de rodilla con una deformidad media de 22º.
Se analizaron los datos mediante un ANOVA de medidas repetidas y para la determinación del efecto por separado de cada una de las técnicas se contrastaron las mejorías obtenidas con respecto al nivel anterior.
La media de extensión conseguida fue de 12º, correspondiendo 7º a la tenotomía intrapélvica del psoas y, sobre el flexo de rodilla restante, una corrección de 5º tras el alargamiento intramuscular del recto anterior a nivel proximal.
Tanto la secuencia de gestos propuesta como los que la forman por separado, mostraron diferencias estadísticamente significativas (p < 0,001) en la corrección de la deformidad.
Como conclusión, las técnicas propuestas aplicadas de manera secuencial o por separado, son eficaces en la disminución del flexo de rodilla en la parálisis cerebral de predominio espástico, facilitando o incluso pudiendo evitar, el tramiento que de manera directa necesite.
Childhood cerebral palsy (CCP) is the most common paediatric neuromuscular disease, with a prevalence of 1–1.7/1000 live births.1 Considering motor control problems as a criterion, the predominantly spastic form is the most frequent.2
Of the orthopaedic manifestations, knee flexion deformity is the third most common, after ankle equinus and contractures associated with spastic hip dysplasia.3
Its pathogenesis differs according to the patient's ability to walk. On the one hand, it forms part of the natural history of gait disorders in the diplegic population: fixed knee flexion associated with severe lever arm dysfunction conditioned by bone torsion abnormalities and non-flexible deformities of the feet in its final stage.3,4 On the other hand, in non-ambulant patients, permanent sitting causes progressive shortening of the hamstring musculature and retraction of the posterior capsule.5
In both functional groups the consequences are different. During the gait cycle, knee flexion causes instability throughout the stance phase and, in patients who cannot walk, transfers from the wheelchair become difficult. In both cases femoropatellar pain may be associated.
In addition to shortening of the hamstring musculature, soleus insufficiency in unipedal stance and contracture of the hip flexors in the standing position, due to increased anterior pelvic tilt, have been described as causes of knee flexion.4,6 The relationship of the latter to knee flexion is explained by the biarticular behaviour of the hamstring muscles, which, in order to maintain their length when their proximal insertion rises, brings the knee into flexion. Delp and Hoffinger demonstrated this using virtual models that reproduced the crouch gait and showed how knee flexion coexisted with a shortening of the hip flexors, rather than shortening of the hamstrings.7,8 This is corroborated on physical examination with the corrected popliteal angle manoeuvre, in which, after reversing lumbar lordosis, passive knee extension is improved.9
The present study was conducted due to the lack of papers quantifying the impact on reducing fixed knee flexion after correction of ipsilateral hip flexion in patients with CCP.
Intrapelvic tenotomy of the psoas followed by intramuscular proximal lengthening of the rectus femoris were the surgeries of choice due to their proven ability to correct the position of the pelvis position and preserve hip flexor strength.10–12 The latter because it respects the iliac portion of the iliopsoas muscle and the continuity of the rectus anterior muscle.11–13
The aims of the study were twofold: first, to analyse whether the correction of fixed spastic knee flexion was statistically significant after treating hip flexor shortening by intrapelvic tenotomy of the psoas followed by proximal lengthening of the rectus anterior and, second, to analyse separately the efficacy of the abovementioned techniques in reducing knee flexion.
Material and methodA prospective study was conducted, with evaluation of outcomes during 2017–2018, in patients diagnosed with predominantly spastic CCP, selected in the orthopaedic surgery and trauma clinic because they presented orthopaedic deformities with functional impact on walking or standing and showed, supine, fixed knee flexion equal to or greater than 10° with a positive ipsilateral Thomas test.
Exclusion criteria were the absence of functional demand, dystonia as the predominant motor impairment and, in ambulant patients, the presence of hip flexor weakness with a maximum rating of 3 on the Kendall scale, meaning the ability to achieve active hip flexion against gravity without overcoming resistance.14
We quantified the effect that intrapelvic psoas tenotomy followed by proximal lengthening of the rectus femoris had on reduction of knee flexion. We established that, after the psoas surgery, complete correction at the knee as well as a negative Thomas sign were criteria for not performing the procedure on the rectus femoris.
The study was approved by the centre's ethics committee and the families were informed of the reason and purpose for the surgery.
Immediately prior to the surgery and under general anaesthesia, knee flexion was recorded using a sterile rigid goniometer placed on the lateral aspect, making the centre of rotation of the instrument coincide with the femorotibial joint space and placing its proximal arm parallel to the femoral axis and the distal arm parallel to the tibia. The persistence of ipsilateral hip flexion was confirmed in all cases with a positive Thomas sign.
For recording, the mean of 2 measurements taken by 2 observers experienced in the use of the goniometer was taken and 3 different times were recorded: the measurement obtained before surgery, after psoas tenotomy in the pelvis and, finally, after intramuscular lengthening of the rectus femoris.
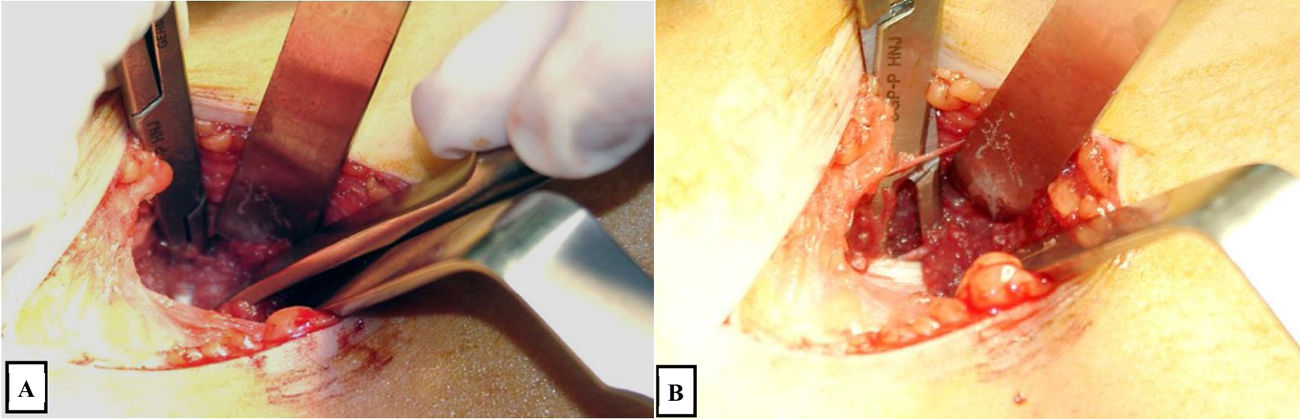
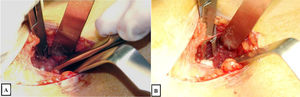
The advantages of the techniques used are preserving strength in hip flexion and using the same surgical approach, taking the description by Novacheck and Matsuo12,13 as the benchmark (Figs. 1 and 2).
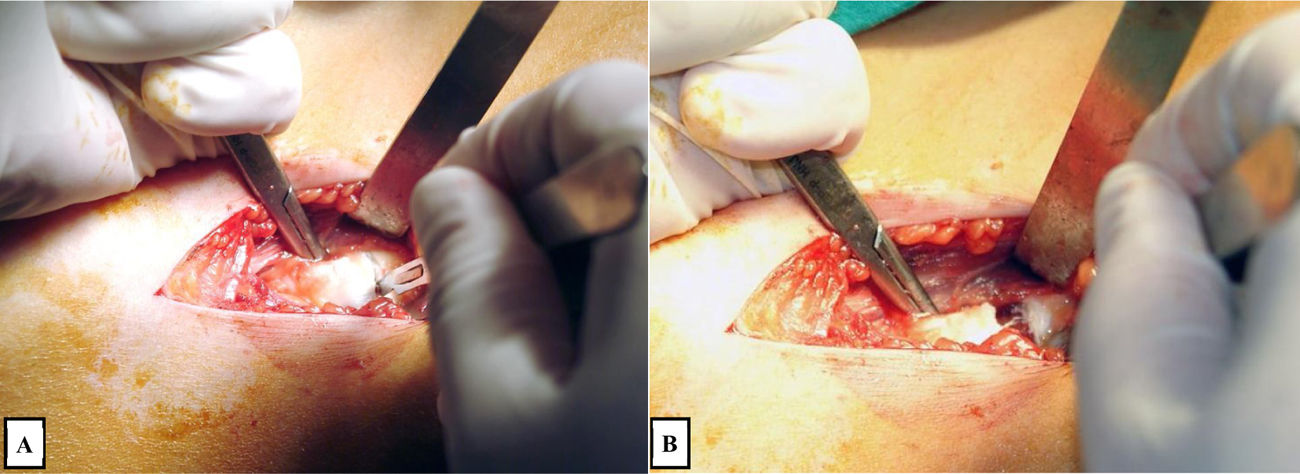
Surgical technique for intramuscular lengthening of the rectus femoris at the proximal level. A) Visualisation and initiation of section of the intramuscular tendon portion of the rectus femoris at the proximal level. B) B) Separation of the ends of the intramuscular portion of the tendon, respecting the continuity of the muscle belly located posteriorly.
The same 5−6 cm long incision is used in the 2 techniques, starting from the anterior superior iliac spine, and following the longitudinal axis of the sartorius muscle. After moving the sartorius laterally, the fascia of the iliacus muscle is identified and, through an eyelet made in it, the surgeon inserts their index finger, holds it firmly to the iliac bone and, in the direction of the symphysis pubis, performs a blunt dissection of the space between bone and muscle. Palpation near the midline of a tight cord that includes the psoas tendon guides us to introduce a curved, blunt dissector with the other hand. By directing the end of this instrument medially and distally while resting it on the inserted finger that locates the tendon, we can make it jump over the cylindrical area under tension. After circling it, the muscle fibres are separated, visualising the tendon fibres to be sectioned with electrocautery.
The intramuscular tendon lengthening of the rectus femoris is performed after identifying it from its origin at the anteroinferior iliac spine. Following it distally, it is encircled medially with a curved and blunt dissector and as distally as possible, the tendon fibres are sectioned while respecting the muscle fibres.
Two working hypotheses were established. The first was that psoas tenotomy at the pelvis followed by lengthening of the rectus femoris at the proximal level statistically significantly corrects structured knee flexion and, secondly, that each of the surgical techniques on its own had an influence on correction of the knee.
Repeated measures ANOVA was used as the statistical study, with a priori contrasts and analysis of effect. Changes were assessed after applying a factor with 3 levels:
- •
Level 1 (pre-intervention degrees of knee flexion).
- •
Level 2 (degrees of knee flexion post intrapelvic psoas tenotomy).
- •
Level 3 (degrees of knee flexion post intramuscular proximal lengthening of the anterior femoris).
To determine the effect separately on knee flexion correction, a priori contrasts of each level with respect to the previous level were performed and the measured effect size was studied.
The SPSS v.23 statistical package was used for the analysis.
ResultsA total of 16 interventions on knee flexion deformity with ipsilateral hip flexion were analysed, corresponding to 10 patients with spastic CCP, 9 were male (90%), with a mean age of 14 years (range: 12–17); 6 required the proposed surgery bilaterally. In terms of GMFCS, 2 were level II, 5 were level III and 3 were level IV.
With the patient under general anaesthesia, mean knee flexion prior to the surgery was 22° (standard deviation 15.8; range 50−7). The minimum value of 7° occurred in 3 cases in which intrapelvic psoas tenotomy achieved complete correction of knee and hip flexion. In the remaining 13 cases, intramuscular proximal lengthening of the rectus femoris was performed as a second surgical procedure.
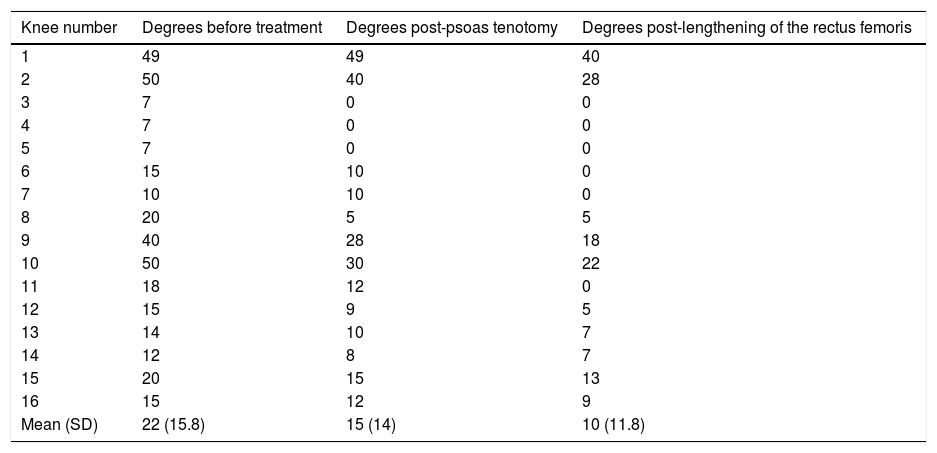
The increased extension obtained in the 16 knees is shown in Table 1.
Increases achieved in knee extension.
| Knee number | Degrees before treatment | Degrees post-psoas tenotomy | Degrees post-lengthening of the rectus femoris |
|---|---|---|---|
| 1 | 49 | 49 | 40 |
| 2 | 50 | 40 | 28 |
| 3 | 7 | 0 | 0 |
| 4 | 7 | 0 | 0 |
| 5 | 7 | 0 | 0 |
| 6 | 15 | 10 | 0 |
| 7 | 10 | 10 | 0 |
| 8 | 20 | 5 | 5 |
| 9 | 40 | 28 | 18 |
| 10 | 50 | 30 | 22 |
| 11 | 18 | 12 | 0 |
| 12 | 15 | 9 | 5 |
| 13 | 14 | 10 | 7 |
| 14 | 12 | 8 | 7 |
| 15 | 20 | 15 | 13 |
| 16 | 15 | 12 | 9 |
| Mean (SD) | 22 (15.8) | 15 (14) | 10 (11.8) |
The first column numbers each of the 16 knee flexions; from left to right, the prior deformity is shown, that achieved after psoas tenotomy and that recorded after proximal lengthening of the rectus femoris. The first 4 flexions correspond to patients who required unilateral surgery.
SD: Standard Deviation.
The last row shows the evolution of flexion deformity, its mean with standard deviation, during the proposed sequence of soft tissue surgery.
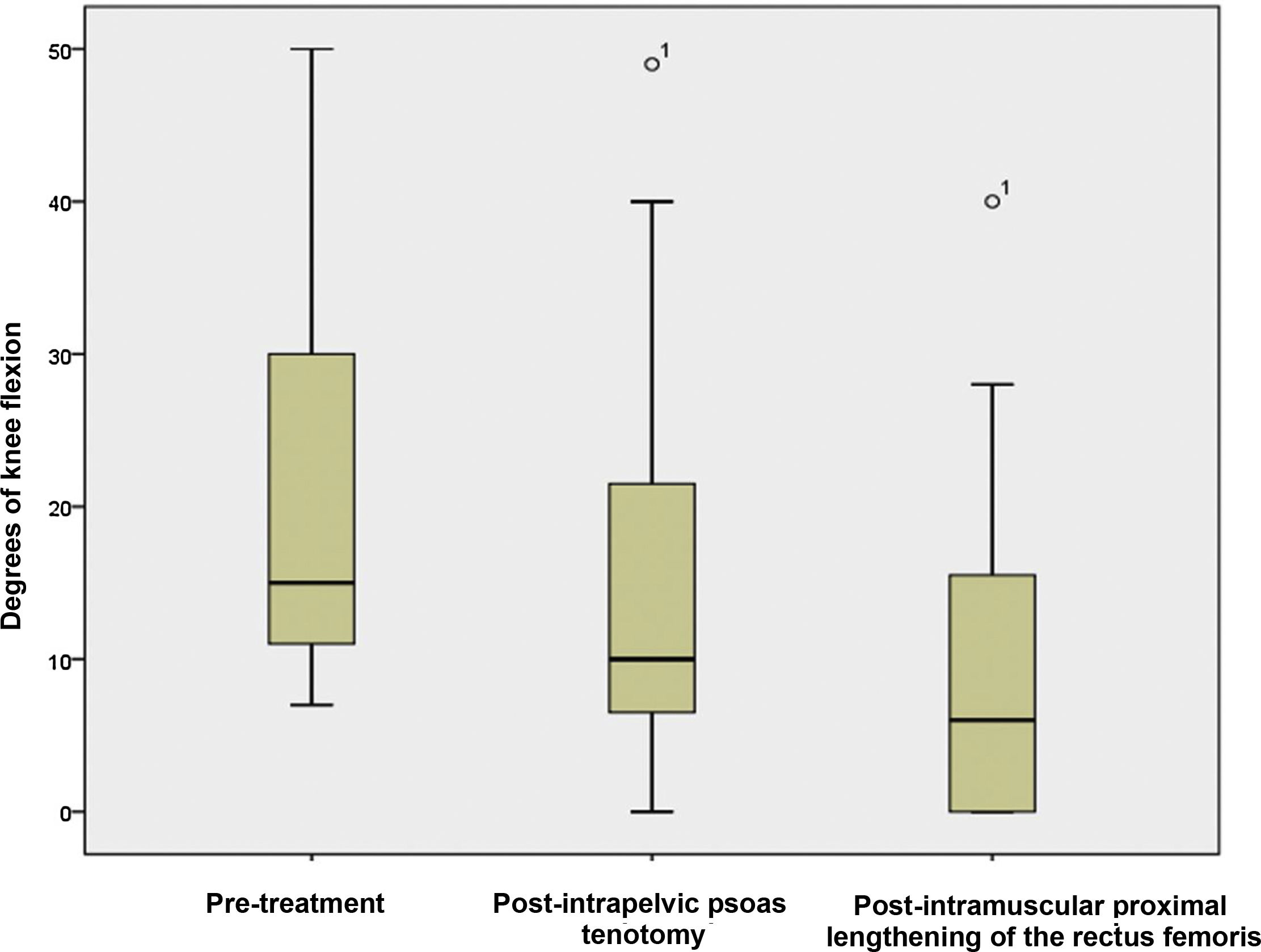
Knee extension after intrapelvic psoas tenotomy improved by a mean of 7° (95% confidence Interval: 3.4–10.5). This difference was statistically significant with a p < .001 and η2 effect size of .66. After lengthening of the rectus femoris at the proximal level, knee extension was achieved by a mean value of 5° (95% confidence interval: 2.1–8.4), a change that was shown to be statistically significant with a p < .001 and η2 effect size of .74.
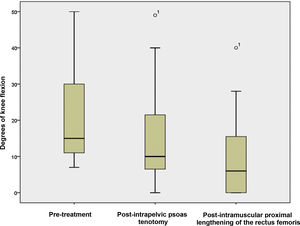
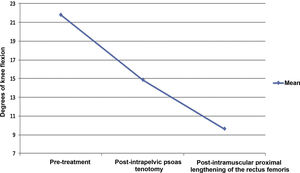
The sequential evolution of knee flexion correction is shown in Figs. 3 and 4. These Figures show how the initial degrees of knee flexion decrease by a mean of 7° after intrapelvic psoas tenotomy and 5° after rectus femoris lengthening. The mean total correction of 12° is a significant improvement prior to directly addressing the knee deformity problem.
Treatment of knee flexion in CCP has traditionally focused on lengthening the hamstring musculature. The musculature includes the hamstring muscles and the long portion of the biceps cruris, the distal insertion of which is at the head of the fibula.15 This surgery weakens the extension of the pelvis and hip, as in the diving syndrome described by Rang, which justifies the search for alternatives.16 One such alternative is offered after acknowledging the importance of pelvic antepulsion related to hip flexor shortening.7,8
Surgical treatment of the hip flexors focuses on shortened biarticular muscles such as the psoas and, less frequently, the rectus femoris.11,12
Pelvic psoas tenotomy has been shown to be effective in reducing lordosis, as it preserves hip flexion strength by respecting the insertion of the iliac portion of the iliopsoas muscle at the lesser trochanter.11,13 The results of Bialik's comparative kinematic analysis questioned whether there was a difference in hip flexion strength, according to where the tendon is sectioned, the lesser trochanter or the intrapelvic portion.17 Their result were explained by the ability of other hip flexor muscles, such as the rectus femoris, to replace the loss of strength caused by sectioning the psoas distally.
This reflects the concern to maintain the strength of the iliopsoas muscle as responsible for 20% of gait propulsion.18,19
The role of the anterior rectus in hip flexion correlates with the attitude in knee extension that appears during the Thomas test and the associated electromyographic activity, as reported by Perry.20 From the surgical perspective, only Matsuo's series reports good outcomes in spastic hips, following lengthening of the psoas and rectus abdominis proximally.12
Following Delp's virtual models, hip surgery improves lordosis, reduces hamstring traction, and therefore improves knee extension.7
The paradox of a weakened knee extensor extending the knee can be explained by relating the greater effect that the site of the surgery has on one of the functions it performs as a biarticular muscle. Thus, the pelvic repositioning effect associated with lengthening of the anterior rectus improves knee extension.7,12,21
The decrease in deformity under general anaesthesia, demonstrated in the change from 10° to 7° present in 3 of the 16 knees, reaffirms the need to consider exploration just prior to surgery as a further pillar in decision-making.22
Analysis of the results shows the high statistical significance (p < .001) in the changes obtained in knee extension acting at a distance. Its statistical significance allows us to vouch for both the surgical sequence used and the role played by each of its steps separately. The efficacy of these surgeries in the correction of hip flexion is described in the literature, but we were not able to find any reference to the role they play in the correction of fixed knee flexion.8,10,23
The final mean correction of 12° achieved after the 2 techniques would, in cases of non-significant deformities, obviate the need for a distal femoral extensor osteotomy.3,5 Savings in morbidity, operating theatre time and costs are factors to be considered for generalising proposed surgical strategy.
Limitations of the study such as follow-up, sample size, lack of a real comparative study between the two techniques or measurement methodology were considered in its design. Firstly, not requiring follow-up is based on the objective of immediate evaluation of intraoperative efficacy. Secondly, in terms of sample size, the statistical study model chosen allows the study of intrasubject changes with 2 advantages: requiring a smaller sample than completely randomised designs and avoiding residual variation due to differences between subjects. As for the lack of comparison of efficacy between the two techniques, this would require a prospective comparative study with 2 homogeneous cohorts in which to apply the 2 surgeries, which presents the difficulty of acceptance by the families and obtaining the approval of the ethics committee. Finally, with respect to the reliability of the intraoperative measurements, to minimise bias related to the sterile goniometer, standardisation of the anatomical references was extreme and was complemented by the agreement of 2 observers with experience in its use. Regarding the results of the surgery in the correction of hip flexion, the difficulty quantifying this in the operating theatre meant that it was assessed by persistence of the Thomas sign after the psoas tenotomy, in order thus to justify the intramuscular lengthening of the rectus femoris.
There are three novel aspects to the present paper. First, it records the direct influence with statistical significance of intrapelvic psoas tenotomy on the reduction of knee flexion. Second, it shows the equally significant efficacy of proximal lengthening of the rectus femoris as a complementary treatment. Finally, it demonstrates that the sum of both surgeries can correct moderate fixed knee flexion deformities.
Three facts reflect the therapeutic significance of the results. First, the possibility of saving bone surgeries of higher cost and risk for morbidity. Second, correction of actual knee flexion, being of lesser magnitude, is associated with a lower risk of neurovascular complications and less need for lengthening of the hamstring musculature. Thus, extensor strength in the hip is preserved. Finally, for the knee, if an extensor osteotomy of the distal femur is required, the size of the anterior base wedge would be smaller, resulting in less metaphyseal deformity.3,6,24 This alteration of the anatomy should be minimised, as it is associated with a decrease in femorotibial joint congruence and loss of knee flexion range of motion similar to the degrees of extension achieved.24,25
Another message of the study is the possibility of evaluating the routine inclusion of intramuscular lengthening of the rectus femoris in hip and knee surgery in CCP. The results demonstrate how this technique can be an alternative to psoas tenotomy in patients with hip flexion weakness.12
ConclusionsIn predominantly spastic CCP, intrapelvic psoas tenotomy followed by intramuscular lengthening of the rectus femoris at the proximal level statistically significantly achieves knee extension with fixed flexion deformity.
Both techniques are effective separately in reducing knee flexion deformity.
Level of evidenceLevel of evidence IV.
FundingWe received no funds or sources of funding for the actual work.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Martínez Caballero I, Chorbadjian Alonso G, Egea-Gámez RM, Ramírez Barragán A, Fraga Collarte M. Tenotomía intrapélvica del psoas y alargamiento proximal del recto anterior como tratamiento del flexo fijo de rodilla en parálisis cerebral infantil. Rev Esp Cir Ortop Traumatol. 2021;65:216–222.