The use of plate fixation to treat displaced midshaft clavicular fractures in adults reduces complications and residual shoulder disability. New features of the precontoured locking plates have been shown to reduce the need for hardware removal in adults. There is a lack of studies evaluating surgical fixation of displaced clavicular fractures with precontoured plates in adolescents. We evaluate outcomes and complications of adolescents with displaced midshaft clavicular fractures treated with precontoured locking plates.
Materials and Methods40 adolescents with displaced midshaft clavicular fractures were surgically treated from January 2010 to May 2017. Outcomes were evaluated using the Constant score, the 11- item version of the Disabilities of Arm, Shoulder and Hand (QuickDASH) questionnaires, and radiographs, and a visual analog scale. Return-to-sport rate, level achieved and complications were recorded.
ResultsMean follow-up was 50 months (18–108 months). Constant, Quick-DASH, and visual analog scale scores were 95.6, 2.8 and 0.5 points, respectively. 100 % of adolescents returned to sports at the same level they had before injury. Mean time to return was 69 days and 95 % of patients were able to return before 12 weeks. Complication rate was 12.5 %, 3 patients (7.5 %) required hardware removal.
ConclusionsAdolescents with displaced midshaft clavicular fractures treated with precontoured locking plates exhibited satisfactory outcomes and low complication rate. Compared to other reports, this study had lower rates, anatomic plates might reduce hardware-related complications.
La fijación con placas de fracturas claviculares desplazadas mediodiafisarias en adultos reduce complicaciones y discapacidad residual. Además, las características de las placas bloqueadas precontorneadas reducen la necesidad de retirar el implante en adultos. Faltan estudios de fijación quirúrgica de las fracturas claviculares desplazadas con placas precontorneadas en adolescentes. Evaluamos los resultados de adolescentes con fracturas claviculares desplazadas mediodiafisarias tratadas con placas bloqueadas precontorneadas.
Materiales y métodosTratamos 40 adolescentes con fracturas claviculares desplazadas mediodiafisarias de enero de 2010 a mayo de 2017. Se realizó el score de Constant, la versión de 11 ítems del score de Discapacidad de brazo, hombro y mano (QuickDASH), radiografías, y escala visual analógica. Evaluamos la tasa de retorno al deporte, el nivel alcanzado después de la cirugía y las complicaciones.
ResultadosEl seguimiento medio fue 50 meses (18-108 meses). Los score de Constant, Quick-DASH y escala visual analógica fueron 95.6, 2.8 y 0.5 puntos, respectivamente. Al último seguimiento, 100 % de los adolescentes volvieron al deporte al mismo nivel previo a la lesión. El tiempo de retorno fue 69 días y 95 % volvieron al deporte antes de las 12 semanas. La tasa de complicaciones fue 12,5 % y 3 pacientes (7,5 %) requirieron extracción del implante.
ConclusionesLos adolescentes con fracturas claviculares desplazadas mediodiafisarias tratados con placas bloqueadas precontorneadas exhibieron resultados satisfactorios y bajas complicaciones. Comparado con otros estudios tuvimos tasas de extracción de implante más bajas. Las placas anatómicas podrían reducir complicaciones con el implante.
Clavicular fractures are common injuries that occur in all age groups, but are most commonly seen in the young and active population.1–3 Non-surgical treatment has traditionally been considered the treatment of choice for most clavicular fractures.4,5 However, recent evidence suggests that surgery has lower rates of nonunion, better functional outcomes, better cosmetic outcome and greater patient satisfaction compared to conservative treatment in the adult population.1,5,6 This shift has led many paediatric orthopaedic surgeons to seek and refine indications for clavicular fracture fixation in skeletally immature patients, particularly in high-functioning and active adolescents.3,7,8
Although children have great potential for fracture healing and remodelling, as they enter adolescence, they become more active than adult patients, lose the ability to remodel and may have greater functional impairment as a result of residual disability.3,7,9 Although there is abundant Level I evidence on adult management, the literature on adolescent patients remains limited.8,10–12 In addition, various problems associated with plate fixation have been reported, including hardware-related complications such as irritation, protrusion or loosening, and wound complications (infection, dehiscence).13
The development of precontoured locking plates and the introduction of angular stability have paved the way for a new perspective on the surgical treatment of these fractures. The aim of this study was to analyse clinical outcomes and hardware-related complications in a group of adolescents with displaced midshaft clavicular fractures treated with precontoured locking plates.
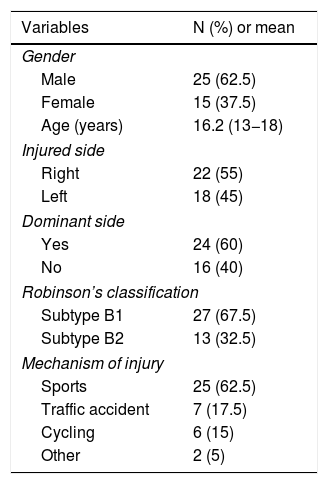
Material and methodsBetween January 2010 and May 2017, 42 patients with midshaft clavicular fractures (Table 1) were surgically treated in our centre with open reduction and fixation with precontoured angular stability plates. The inclusion criteria were a) patients aged between 14 and 18 years; b) type 2 B fractures according to Robinson's classification; and c) displacement (more than 2 cm). Exclusion criteria were a) exposed fracture; b) neurovascular injury; c) associated upper limb injury; d) pathological fracture; e) previous fracture in the same shoulder; and f) lack of informed consent. The analysis comprised 40 fractures in 40 patients; two patients were lost to follow-up.
Demographic characteristics and characteristics related to fracture.
| Variables | N (%) or mean |
|---|---|
| Gender | |
| Male | 25 (62.5) |
| Female | 15 (37.5) |
| Age (years) | 16.2 (13−18) |
| Injured side | |
| Right | 22 (55) |
| Left | 18 (45) |
| Dominant side | |
| Yes | 24 (60) |
| No | 16 (40) |
| Robinson’s classification | |
| Subtype B1 | 27 (67.5) |
| Subtype B2 | 13 (32.5) |
| Mechanism of injury | |
| Sports | 25 (62.5) |
| Traffic accident | 7 (17.5) |
| Cycling | 6 (15) |
| Other | 2 (5) |
Demographic and fracture characteristics were recorded. The patients were seen postoperatively at one week, two weeks and monthly until fracture healing, and then once a year. Radiological assessment was obtained on the immediate postoperative day and monthly until fracture healing. Fracture healing was defined as complete periosteal and endosteal bridging visible between medial and lateral fragments on at least two different radiographs and the absence of pain and instability at the fracture site.
The patients were assessed at last follow-up by two of the authors (L.A.R and GM) using the Constant score and the 11-item version of the Disabilities of the Arm, Shoulder and Hand (Quick-DASH) questionnaire. Residual pain was assessed with the visual analogue scale (VAS), 0 being "no pain" and 10 being "maximum pain". All complications and reoperations related to the surgery were documented. The patients were also asked whether they had been able to return to sports and whether return was at the same level as before the accident (Table 1).
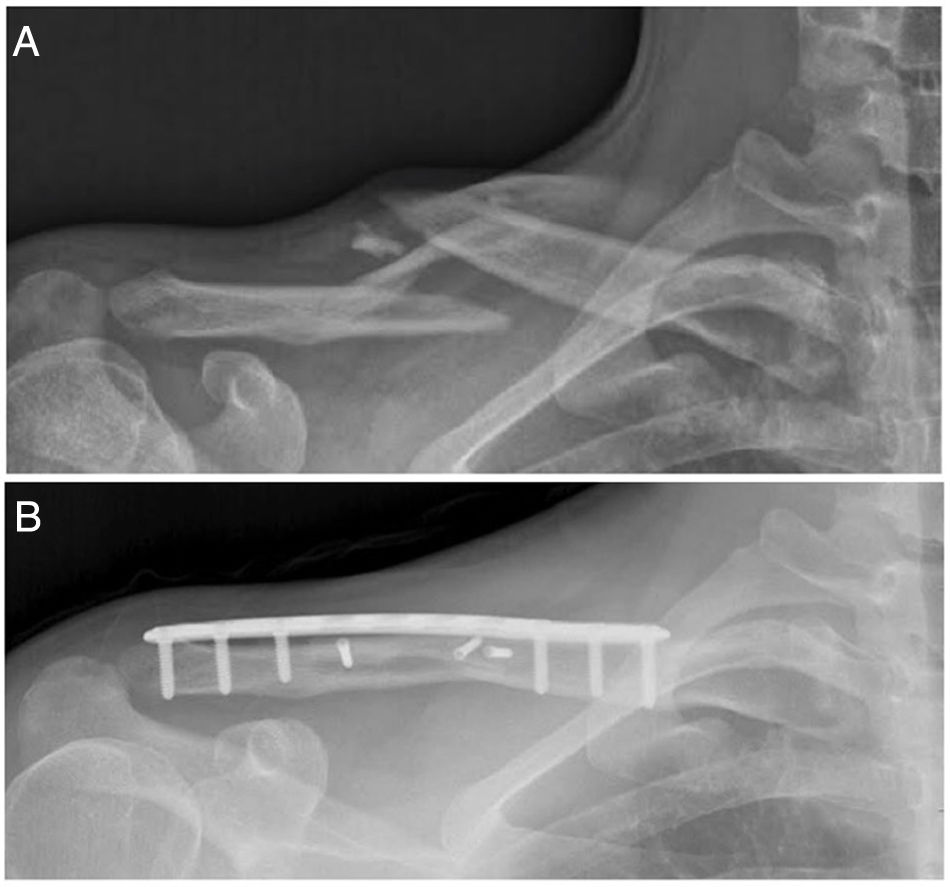
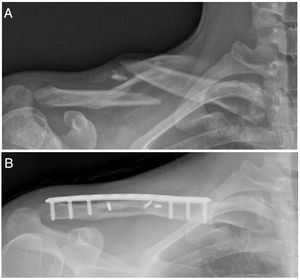
The patients underwent combined anaesthesia (regional block and general anaesthesia) and were placed in the beach chair position with padding behind the ipsilateral scapula. An anterior-inferior approach centred on the fracture site was used. Once the fracture was anatomically reduced, fixation was performed. A precontoured locking plate (Acumed, Hillsboro, OR, USA) was placed on the superior side of the clavicle (Fig. 1B). Interfragmentary screws were used for fragment fixation when a third fragment was present. At each plate fixation site, we used a minimum of three screws on each side of the fracture at each plating site.
A) Preoperative clavicle radiograph with 45° cephalic tilt showing a Robinson 2B2 fracture (displaced, comminuted and segmental) in a 17-year-old rugby player. B) Postoperative radiograph showing bone healing of the clavicular fracture three months after surgical fixation with a precontoured locking plate and three interfragmentary screws.
The postoperative rehabilitation protocol comprised wearing a sling for the first two weeks postoperatively. Pendular movements were allowed for the first three weeks, followed by active abduction and flexion to the horizontal plane from the third to the sixth week. Full active range of motion in the shoulder was allowed after six weeks, and full return to activities was allowed after three months.
Statistical methodologyContinuous variables are expressed as means ± standard deviations and categorical variables as absolute and relative frequencies. STATA 12 software (StataCorp LP, College Station, TX, USA) was used for the statistical analysis. A p-value <.05 was considered statistically significant.
ResultsThe series comprised 25 males (62.5%) and 15 females (37.5%) with a mean age of 16.2 years (range 13−18 years), with 18 left-sided and 22 right-sided fractures; 24 fractures (60%) were on the dominant side. All fractures were classified as 2B according to Robinson's classification; specifically, 27 B1 and 13 B2 subtypes of fractures were identified. Sports-related trauma was the main cause of fracture, present in 25 patients (62.5%); traffic accidents were the second most frequent cause, in seven patients (17.5%; Table 1). The average time to surgery was five days (range, 2–11 days). The average surgery time was 66 min (range, 55−80 min). There were no major intraoperative complications.
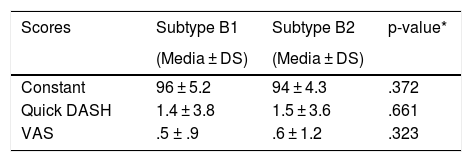
Mean follow-up was 50 months (range, 18–108 months). All fractures healed. The mean Constant score was 95.6 points (range, 76–100 points). The mean QuickDASH score was 2.8 points (range, 0–15 points). Mean pain during follow-up was 0.5 points (range, 0–2 points) according to the VAS. In terms of fracture type, according to Robinson's classification, there were no significant differences with respect to functional outcomes (Table 2). Thirty-five of the forty patients played sports before the injury. All patients were able to return to their pre-injury sports and level. At the last follow-up, 32 of the 35 patients who played sports were still competing. Three patients had given up sports, but their reasons were independent of the shoulder injury.
Summary of functional outcomes according to Robinson’s classification.
| Scores | Subtype B1 | Subtype B2 | p-value* |
|---|---|---|---|
| (Media ± DS) | (Media ± DS) | ||
| Constant | 96 ± 5.2 | 94 ± 4.3 | .372 |
| Quick DASH | 1.4 ± 3.8 | 1.5 ± 3.6 | .661 |
| VAS | .5 ± .9 | .6 ± 1.2 | .323 |
QuickDASH: 11-item version of the Disabilities of the Arm, Shoulder and Hand Questionnaire.
SD: standard deviation; VAS: visual analogue scale.
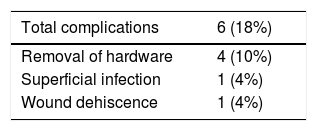
Six complications occurred in 40 patients (18%); all were considered minor complications (Table 3). Plate removal was necessary after fracture healing in four patients (10%). The hardware was removed due to protrusion and discomfort in all patients. None of these patients had refracture 18 months after plate removal. One patient had a partial wound dehiscence that was closed with 4.0 nylon and one patient had a superficial wound infection that resolved with oral antibiotics. The reoperation rate was 10%. Excluding the patients who underwent hardware removal, there were no reoperations.
DiscussionThe main finding of this study was that surgical fixation of midshaft clavicular fractures with precontoured locked plates in adolescent patients had excellent functional outcomes, with most patients returning to sports and at the same level as before their injury. In addition, the rate of implant-related complications was significantly lower than reported in previous studies with other plate designs.
Recent meta-analyses of randomised controlled trials comparing surgical with non-surgical treatment of displaced clavicular fractures in adults favour open reduction and plate fixation for significantly displaced or shortened midshaft clavicular fractures, although whether this applies to adolescents remains controversial.1,14 Although specific evidence in adolescents evaluating clinical outcomes after surgical fixation of midshaft clavicular fractures is limited, many studies show an increasing trend towards fixation in adolescents; the outcomes in the literature on adults most influence treatment options among paediatric surgeons.15,16
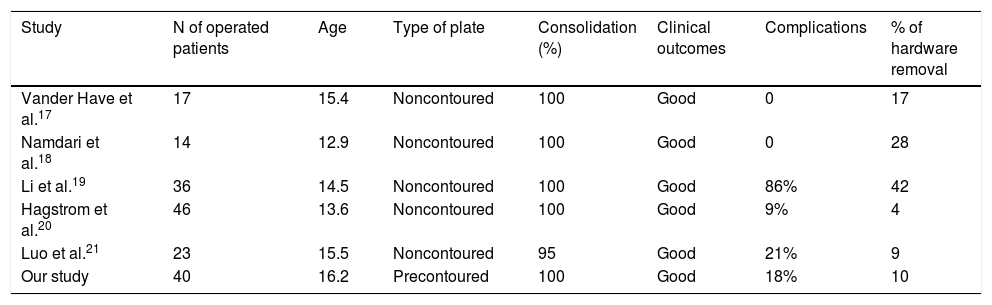
Favourable results have been reported with plates,17–21 but several problems have been associated with these implants (Table 4). The most frequent reports are irritation, protrusion or loosening of the implant, and wound complications (infection, dehiscence).17–21
Published series.
| Study | N of operated patients | Age | Type of plate | Consolidation (%) | Clinical outcomes | Complications | % of hardware removal |
|---|---|---|---|---|---|---|---|
| Vander Have et al.17 | 17 | 15.4 | Noncontoured | 100 | Good | 0 | 17 |
| Namdari et al.18 | 14 | 12.9 | Noncontoured | 100 | Good | 0 | 28 |
| Li et al.19 | 36 | 14.5 | Noncontoured | 100 | Good | 86% | 42 |
| Hagstrom et al.20 | 46 | 13.6 | Noncontoured | 100 | Good | 9% | 4 |
| Luo et al.21 | 23 | 15.5 | Noncontoured | 95 | Good | 21% | 9 |
| Our study | 40 | 16.2 | Precontoured | 100 | Good | 18% | 10 |
The design features of precontoured plates could offer potential benefits. Firstly, they have the anatomical shape of the natural clavicle and high modularity with the available right and left clavicle fittings. This allows all types of diaphyseal fractures to be treated and may facilitate surgical technique. Secondly, the low profile and rounded edges may reduce the risk of postoperative hardware intolerance. Finally, the lower modulus elasticity of titanium compared to stainless steel in other plates may result in lower mechanical stress.22
Biomechanical and clinical studies in adults support the use of precontoured plates.22–26
However, the evidence in the literature is limited on clinical outcomes with precontoured plates in adolescents. In our study, satisfactory clinical outcomes were obtained, like those previously reported with non-contoured plating (Table 4). In addition, all patients who played sports prior to injury were able to return to sports and at the same level as before injury. The benefits of precontoured plates with respect to the need for hardware removal have also been previously demonstrated in adults.23,26
Our overall complication rate was 18%, with a total reoperation rate of 10%. These results were consistent with previously published figures (Table 4).
However, an interesting finding of our study is that our hardware removal rate was 10%, compared with previously published rates of 4% to 42% with the use of non-contoured plates17–21 (Table 4). This is an important advantage of precontoured plates, as it avoids the patient having to undergo further surgery and anaesthesia.
LimitationsOur study has several limitations. First, this was a retrospective study, and all data were collected from patient records. Second, there was no control group, and therefore we could not compare our results with other treatments. Finally, all plates were placed in the upper clavicle; therefore, our findings cannot be generalised to clavicular plating in other sites.
ConclusionThis study showed satisfactory clinical outcomes and a low complication rate in adolescents with displaced midshaft clavicular fractures treated with precontoured locking plates. The rate of hardware removal was lower than that reported with non-contoured plating, suggesting that a decrease in implant-related complications might be expected with the use of anatomical plates.
Level of evidenceLevel of evidence IV, case series.
FundingThis paper received no funding.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Rossi LA, Magno G, Tanoira I, Puigdevall MH, Bosio S, Ranalletta M. Tratamiento de fracturas mediodiafisarias de clavícula con placas precontorneadas en adolescentes. Rev Esp Cir Ortop Traumatol. 2021;65:223–228.