It is difficult to decide the appropriate treatment for inveterate cervical dislocations because of the difficulty of their reduction, as well as due to the risk of inducing iatrogenic injuries during this reduction. The literature on the most appropriate surgical strategy for their management is also limited as well as controversial.
We report one clinical case treated in the Spine Unit of the Orthopedic Surgery and Trauma Service of the University Hospital of Santiago de Compostela, discussing the currently most used treatment options, the anterior–posterior–anterior and the posterior–anterior–posterior approach.
After analyzing the results, it could be concluded that the surgical approach to these lesions is generally difficult, with any of two techniques described above being suitable, but always with the precaution to remove the entire affected intervertebral disk before axial correction maneuvers, thus avoiding the risk of extrusion into the medullary canal. After the surgical procedure, a proper release and reduction of the joint facets should be performed, sometimes with the need to add osteotomies in them.
Las luxaciones cervicales inveteradas presentan serias dificultades a la hora de plantear su tratamiento adecuado, por un lado, debido la dificultad de su reducción y, por otro, al riesgo de inducir lesiones iatrogénicas durante su reducción. A este hecho hay que añadir la escasa y controvertida bibliografía existente a la hora de establecer la estrategia quirúrgica más apropiada para su manejo.
Presentamos un caso clínico tratado en la Unidad de Raquis del Servicio de Cirugía Ortopédica y Traumatología del Complejo Hospitalario Universitario de Santiago de Compostela, discutiendo las 2 opciones de tratamiento que actualmente se consideran las más utilizadas: el abordaje anterior–posterior–anterior y el posterior–anterior–posterior.
Tras el análisis de los datos obtenidos de la revisión de este caso, podríamos concluir que el abordaje quirúrgico de estas lesiones resulta en general difícil, pudiéndose realizar las 2 técnicas anteriormente descritas, pero con la precaución de extirpar siempre la totalidad del disco intervertebral afectado antes de realizar las maniobras de corrección axial, por el riesgo de extrusión del mismo hacia canal medular. Con posterioridad a este gesto quirúrgico, se procedería a una correcta liberación y reducción de las facetas articulares, siendo necesario, en ocasiones, añadir osteotomías en las mismas.
Inveterate cervical dislocations (over 8 weeks duration) are rare lesions of the cervical spine.1–3 They are often caused by traffic accidents, due to a hyperflexion of the cervical region. The most commonly affected levels are C6/7 and C5/6 in that order.1,2
Anatomically, they are characterized by a displacement of the inferior articular facets of the superior vertebra upwards, through bifacet or unifacet dislocations. Occasionally, they appear associated to fractures of the articular facets. Another typical feature of this type of lesion is the presence of reparative fibrous tissue surrounding them, related to the time elapsed until diagnosis and which further hinders their already difficult reduction.
From the clinical standpoint, rare cases of inveterate dislocations may go unnoticed for long periods of time due to scarce or absent associated neurological symptoms.2,4
A striking feature of this type of lesions is the difficulty of planning and implementing an appropriate treatment. On the one hand, due to the risk of causing iatrogenic lesions during reduction (as this is often associated with significant intracanal disk protrusions) and, on the other, to the limited and controversial literature related to the most adequate surgical strategy.5 Thus, while Hassan defends treatment through traction prior to surgery, and one or another type of approach depending on the level of neurological involvement,3 Payer advocates the use of an anterior–posterior–anterior approach in all cases,1,2 and Bartels and Donk a posterior–anterior–posterior approach.4
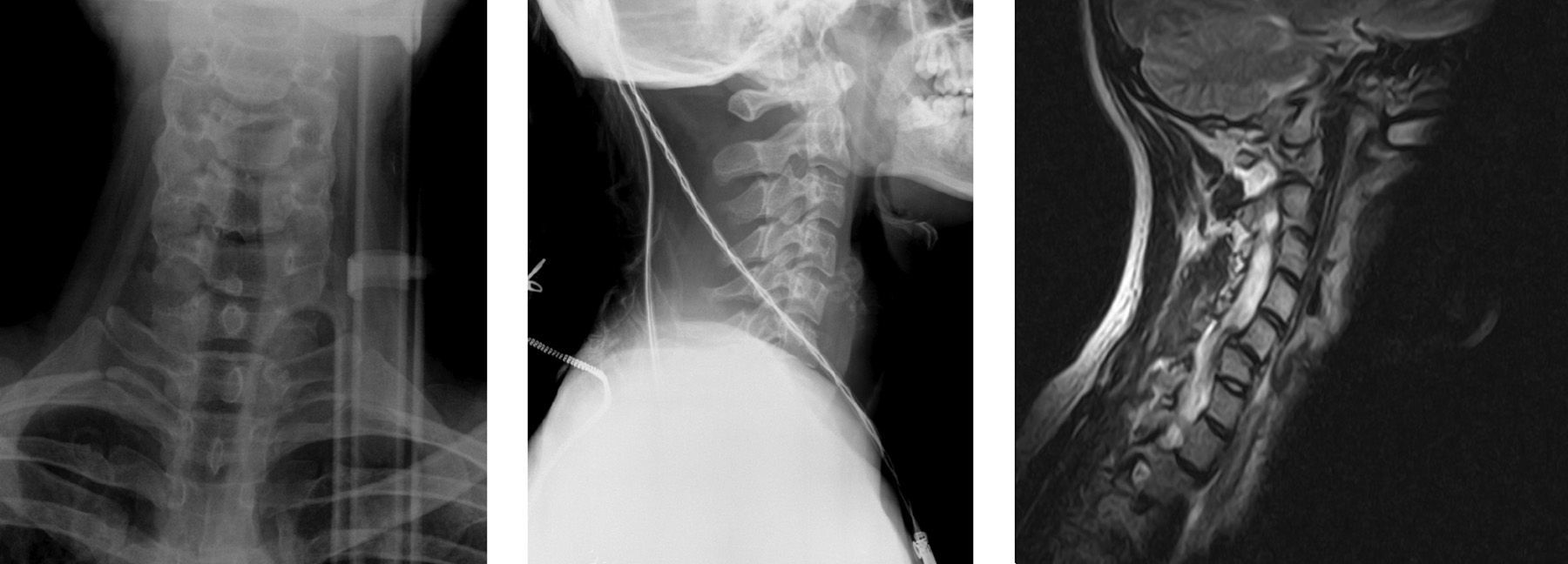
Case ReportWe present the case of a 21-year-old male who was admitted to the emergency department after suffering a traffic accident. Upon admission he only referred mild, right cervicobrachialgia. Radiographic studies of the cervical spine (Fig. 1) led to a diagnosis of cervical sprain which was treated with a soft collar, analgesic drugs and muscle relaxants. Since the lesion was caused by a traffic accident and no dislocation was initially observed, the patient was referred to his private healthcare provider for clinical follow-up.
Anteroposterior and lateral radiographs of the cervical spine on the day of the traffic accident. Magnetic resonance imaging scan obtained subsequently by the private healthcare provider, showing the dislocation of an articular facet and subluxation of the other between C5–C6 and assessment of the disk component.
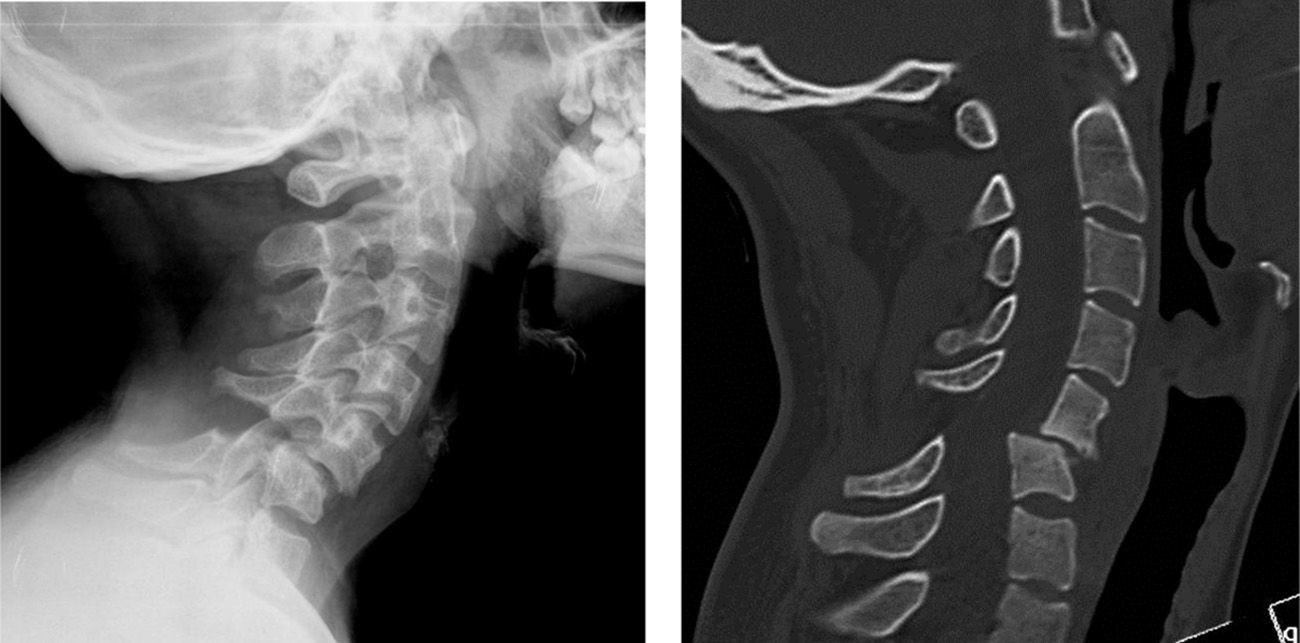
After some rehabilitation sessions, the patient developed a progressive clinical deterioration so he was referred to our Spine Unit 18 weeks after the accident. At the time of assessment, he presented symptoms of right cervicobrachialgia with mixed predominance C6 radiculopathy, ASIA D (American Spinal Injury Association) (normal motor and sensory function), with a score of 62 in the Oswestry functional scale. Once the relevant complementary tests were conducted (computed tomography [CT] and magnetic resonance imaging [MRI]) the patient was diagnosed with a C5–C6 inveterate dislocation (Fig. 2).
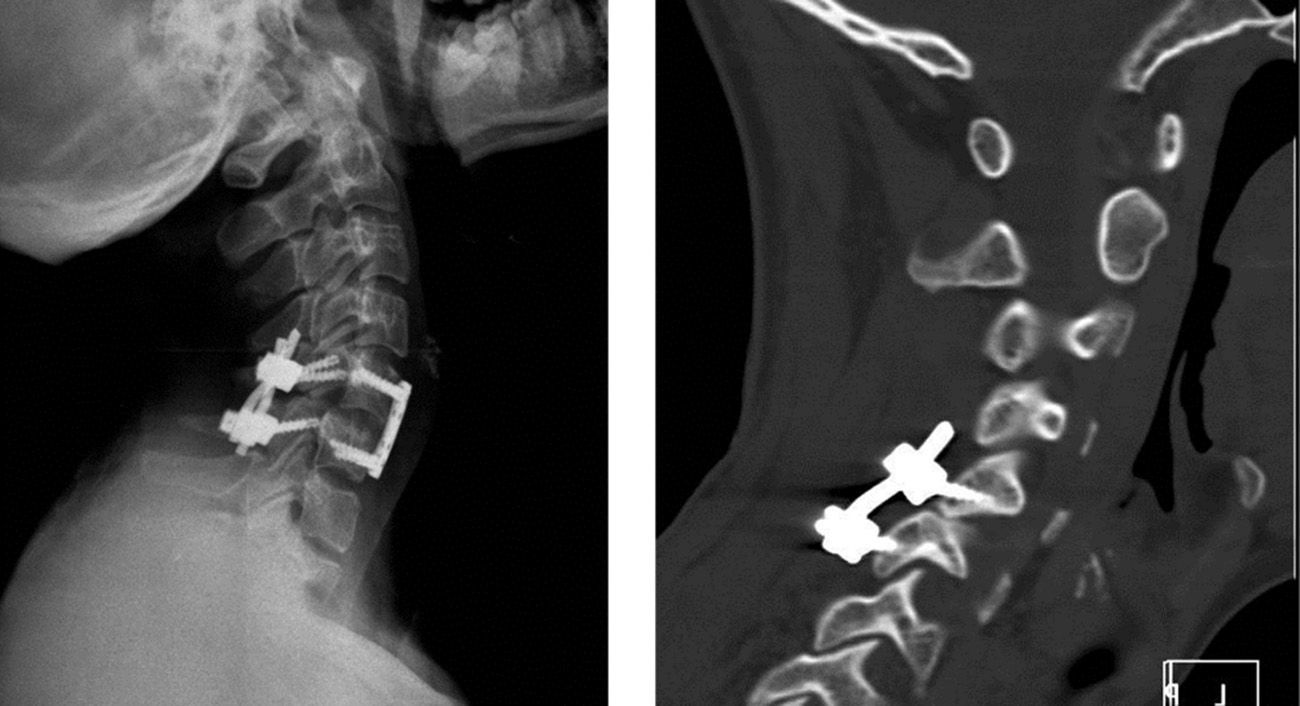
The therapeutic option selected in this case was an anterior approach with disk excision followed by a posterior approach with partial facetectomy and reduction of the dislocation (posterior instrumentation), followed by a new anterior approach to place the intersomatic graft and anterior cervical plate. Evoked potentials were monitored intraoperatively during the entire surgical procedure.
From the surgical point of view, it is worth highlighting the presence of a complete dislocation of a facet joint with subluxation of the other between C5–C6, formation of perifacet fibrous tissue, remodeling of the joint surfaces, herniation of the disk and periarticular calcifications, both in the facets and in the anterior longitudinal ligament, typical anatomical alterations described by Bartels and Donk and responsible for the difficult reduction and stabilization of this type of lesions.4 In spite of them, a correct reduction, fixation and subsequent radiographic arthrodesis of the injured space were achieved.
The clinical evolution after surgery was satisfactory. At 3 months postoperatively, the patient presented minor, residual, ASIA D cervical pain, a slight limitation of mobility (especially rotational), clear functional improvement (score less than 12 in the Oswestry functional scale) and a radiographically stable fixation with arthrodesis of the affected space (Fig. 3).
DiscussionInveterate cervical dislocations are exceptional spinal lesions. In most cases they are caused by high-energy trauma producing a hyperflexion of the cervical spine.1,2
Although in most cases the diagnosis of bilateral dislocation of the cervical facets is usually evident, both by the typical presentation symptoms (severe neck pain with associated neurological deficit) and imaging tests (lateral radiographs of the cervical spine or cervical CT), in some cases (most of them related to incomplete bilateral facet dislocation with mild neurological involvement) diagnosis takes place belatedly, several weeks after the trauma.5 From the clinical standpoint, this fact is normally associated to a spontaneous partial reduction of the lesion following the trauma, with a progressive redislocation of the segment caused by the extension of the lesion toward the posterior soft tissues and intervertebral disk.
This delay in diagnosis and associated segmental instability would justify the onset of the anatomopathological changes described previously due to the healing of soft tissues.4 In turn, these alterations would hinder reduction by closed methods.4–9Thus, regardless of the time of evolution and the level of clinical involvement, open reduction with removal of the affected disk prior to axial correction maneuvers is currently considered to be the treatment of choice for this condition. Nevertheless, it is sometimes difficult to establish the most appropriate therapeutic strategy.1–5 If preoperative traction is used to assess reducibility, this should employ light weights and the patient should remain awake.7
Although a posterior–anterior–posterior approach has the hypothetical advantage of providing the best and simplest reduction of the facets, it also presents the difficulty of requiring 3 positional changes (posterior for facet release, anterior for discectomy and reduction and posterior for instrumentation), as well as increased neurological risk because the dislocation is managed by a posterior approach with a dislocated anterior disk.4,6,9
However, the advantages offered by the anterior–posterior–anterior approach proposed by other authors1–3 include the possibility of removing the disk before performing any other maneuvers and the need for only 2 positional changes. Its disadvantages include greater difficulty to achieve a correct reduction of articular facets,4,6,8 often requiring an osteotomy of the dislocated facets.
Other authors, such as Ahmad,2,10 propose conducting an exclusively anterior–posterior approach in cases in which there is disk herniation.
Performing an isolated posterior approach with dislocation reduction entails the risk of spinal cord compression, especially if the disk is herniated and hyperextension maneuvers are required to reduce the facets. Thus, if attempted, it should always be conducted with gentle movements and close neurological monitoring.11–13 Otherwise, it would be necessary to carry out an anterior approach with removal of the herniated or protruding disk along with anterior arthrodesis.14,15
The results extrapolated from the small experience presented in this work and those obtained from the literature on the subject seem to indicate that both the anterior–posterior–anterior and the posterior–anterior–posterior approaches are adequate surgical options for the treatment of inveterate cervical subaxial dislocations. Each of them presents advantages and disadvantages that must be evaluated individually in each case.
Level of EvidenceLevel of evidence v.
Ethical ResponsibilitiesProtection of people and animals. The authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of data. The authors declare that this work does not reflect any patient data.
Right to privacy and informed consent. The authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Please cite this article as: Gallego-Goyanes A, Caeiro-Rey JR, Díez Ulloa MA, Pino-Mínguez J. Luxación subaxial cervical inveterada. Discusión de cuál es la mejor estrategia terapéutica. Rev Esp Cir Ortop Traumatol. 2013;57:446–449.