The aim of this study is to value whether patients who have suffered a hip fracture have a higher mortality than expected.
Material and methodsA prospective, observational study was carried out where patients with hip fracture were collected as a sample over a year. The study included 284 patients and a minimum follow-up was two years. The mean age of these patients was 84.26 years, with 21.48% (61/284) males and 78.5% (223/284) females. Survival and previous diseases that affect mortality, as risk factors, were collected and analyzed using the Kaplan-Meier Method and the Cox regression model. Actual mortality was compared with that expected according to the Charlson Comorbidity Index (CCI), adjusted for age.
ResultsPrevious pathology was the main mortality factor, with heart disease being the most significant (OR 1,817: 1,048; 3,149). The real mortality at one year of the sample was 22.5%, while the estimated annual mortality according to the ICC was 29.68% (IC95%:44,36−15).
ConclusionsHip fracture does not cause an increase in mortality according to the CCI estimate.
El objetivo de este estudio es valorar si los pacientes que han sufrido una fractura de cadera tienen una mortalidad más alta de la esperada.
Material y métodosSe realizó un estudio prospectivo, observacional donde se toma como muestra los pacientes con fractura de cadera a lo largo de un año, cuya cifra fue de 284 y el seguimiento mínimo fue de dos años. La edad media de estos pacientes fue de 84,26 años, siendo el 21,48%(61/284) varones y el 78,5%(223/284) mujeres. La supervivencia y las enfermedades previas que afectan a la mortalidad como factores de riesgo se recogieron y se analizaron mediante el método de Kaplan-Meier y mediante la regresión de Cox. Se comparó la mortalidad real con la esperada según el Índice de Comorbilidad de Charlson (ICC), ajustado por la edad.
ResultadosLa patología previa fue el principal factor de mortalidad, siendo la cardiopatía la más significativa (HR: 1,817, IC95%: 1,048; 3,149). La mortalidad real al año de la muestra fue del 22,5%, mientras que la mortalidad anual estimada según el ICC, era de un 29,68% (IC95%:44,36-15).
ConclusionesLa fractura de cadera no provoca un aumento de mortalidad según la estimación del ICC.
Of the different osteoporotic fractures, hip fracture is the one that causes the highest rate of mortality.1 This leads to an increase in the workload of the emergency department, overcrowding in hospitalisation and increased medical costs. The major incidence of this fracture is a problem which affects three levels: the epidemiological, medical care and economic fields.
One of every 3 women and one of every 5 men over the age of 50 years will suffer a hip fracture. It is estimated that 35% of them will suffer intrahospital complications, and that from 20% to 24% will die in the first year.2–7
The presence of concomitant diseases and poor state of health are negative predictors for survival after a hip fracture.8–11 An increase in early mortality is observed in those patients with a worse clinical, functional and mental situation.
The most important diseases associated the most often in patients with hip fracture ae chronic ones that correspond to the cardiovascular area, chronic obstructive pulmonary disease, dementia, anaemia and even malnutrition.
Less severe diseases or health problems are even more common, and an average of 4 of these have been detected per patient. Cardiovascular apparatus pathology affects 63% of patients, digestive pathologies 48% or mental disorders, which affect 39% of them.12
In 2003 Wehren13 stated that the previous pathology of these patients is the chief factor in their risk of mortality. Mortality depends more on their previous general state of health than it does on the fracture itself. If we take into account different medical diagnoses to evaluate their general chronic state of health we will find that mortality will amount to 0% in those without previous diseases, 14% in those with 1 or 2 diseases and 24% in those with 3 diseases or more.
Several indexes can be used to estimate mortality according to patients’ previous diseases, including the Charlson comorbidity index (CCI). This index was designed by Charlson in 1987, and it gives a weighted score that takes into account the number and severity of the previous pathologies in a cohort of 559 patients. The comorbidity classification technique offer a method that is simple, applicable and valid to estimate the risk of death due to previous diseases, for use in longitudinal studies.
Given the high prevalence of disease and the acute and intense stress which arises from the fracture and subsequent surgical operation, these may trigger aggravation of previous diseases as well as the emergence of complications.
Although it may be deduced from all of the above considerations that mortality occurs more often and earlier in less healthy individuals, the hip fracture itself must have some negative influence in itself on survival.14
The aim of this study is to evaluate whether patients who have suffered hip fracture suffer a higher than expected rate of mortality.
Material and methodsAn observational, longitudinal and prospective study was performed. Our inclusion criteria were patients admitted to our department from 1 November 2011 to 31 October 2012 with hip fracture (cervical, trochanter or subtrochanter) diagnosed by simple X-ray imaging and caused by a low energy mechanism, aged above 65 years and treated surgically. Patients under 65 years old were excluded, as were those with a fracture caused by tumoral pathology or a high energy event, those with concomitant fracture of the pelvis or femoral diaphysis, and those who could not be treated surgically due to their personal characteristics or their refusal to undergo surgery. A total number of 284 patients were included in the study.
The average patient age was 84.26 years (range 65–103 years and a SD of 6.8 years). 21.48% (61/284) were men and 78.5% (223/284) were women.
All of the patients were subjected to a haemotherapy protocol consisting of the administration of 3 200 mg intravenous doses of iron (Venofer®) every 48 h. and erythropoietin (Binocrit®) was administered to all of the patients with a haemoglobin level on admission lower than 12 g/dl.
From admission all of the patients were treated with prophylactic doses of low molecular weight heparin (enoxaparin 40 mg sc/24 h. or bemiparin 3500 units sc/24 h.).
The treatment that was applied, depending on age and functionality criteria, was partial bipolar or total cemented hip arthroplasty in the transcervical fractures and osteosynthesis by means of cephalomedular nailing in trochanter and subtrochanter fractures.
1 g cefazolin was administered in anaesthesia induction in all of the patients with a subcapital femur fracture to be treated by hip prosthesis, and 1500 mg cefuroxime was given in anaesthesia induction in all of the patients with a trochanter fracture, except in case of allergy to penicillin, in which case 600 mg clindamycin was administered (according to the hospital protocol).15
The minimum follow-up period was 2 years after the fracture or until exitus, if this occurred before the end of this period.
Mortality data were obtained in the regular check-ups in outpatient surgeries or otherwise in the clinical area of the hospital internet where the date of exitus is specified together with its cause, or even by interviewing the family when the patient failed to attend our surgery.
The biological and clinical parameters of all of the patients included in the study were recorded, as well as their previous illnesses such as arterial hypertension, diabetes mellitus, psychiatric pathology, cerebrovascular accidents, kidney failure, heart disease, chronic pulmonary pathology, Parkinson’s and oncological diseases.
Statistical analysis using version 3.0.1 of the R program (R. Core Team, 2013) and Kaplan-Meier survival tables were used to analyse the survival of the sample and which previous diseases of the hip fracture patients affected mortality. Multivariate analysis was also performed using Cox’s regression model.
Results were considered to be statistically significant when the resulting hypothesis comparison P value was less than .05.
Expected mortality was calculated by applying the CCI16 adjusted by sample age, without taking the hip fracture into account. These data were entered in a web page17 that supplied an annual estimate of survival.
ResultsPrevious comorbidity corresponding to arterial hypertension amounted to 75% in the series, and the corresponding figures for diabetes mellitus were 23.59%, dementia 22.18%, psychiatric pathology 23.24% (depression and other disorders), cerebrovascular accident 12.68%, heart disease 38.73%, tumoral processes 16.90%, chronic obstructive pulmonary disease 16.90%, chronic kidney failure 12.68% and Parkinson’s disease 5.28%.
44.01% of the sample had 3 or more previous pathologies, while 5.63% of patients had more than 5 pathologies.
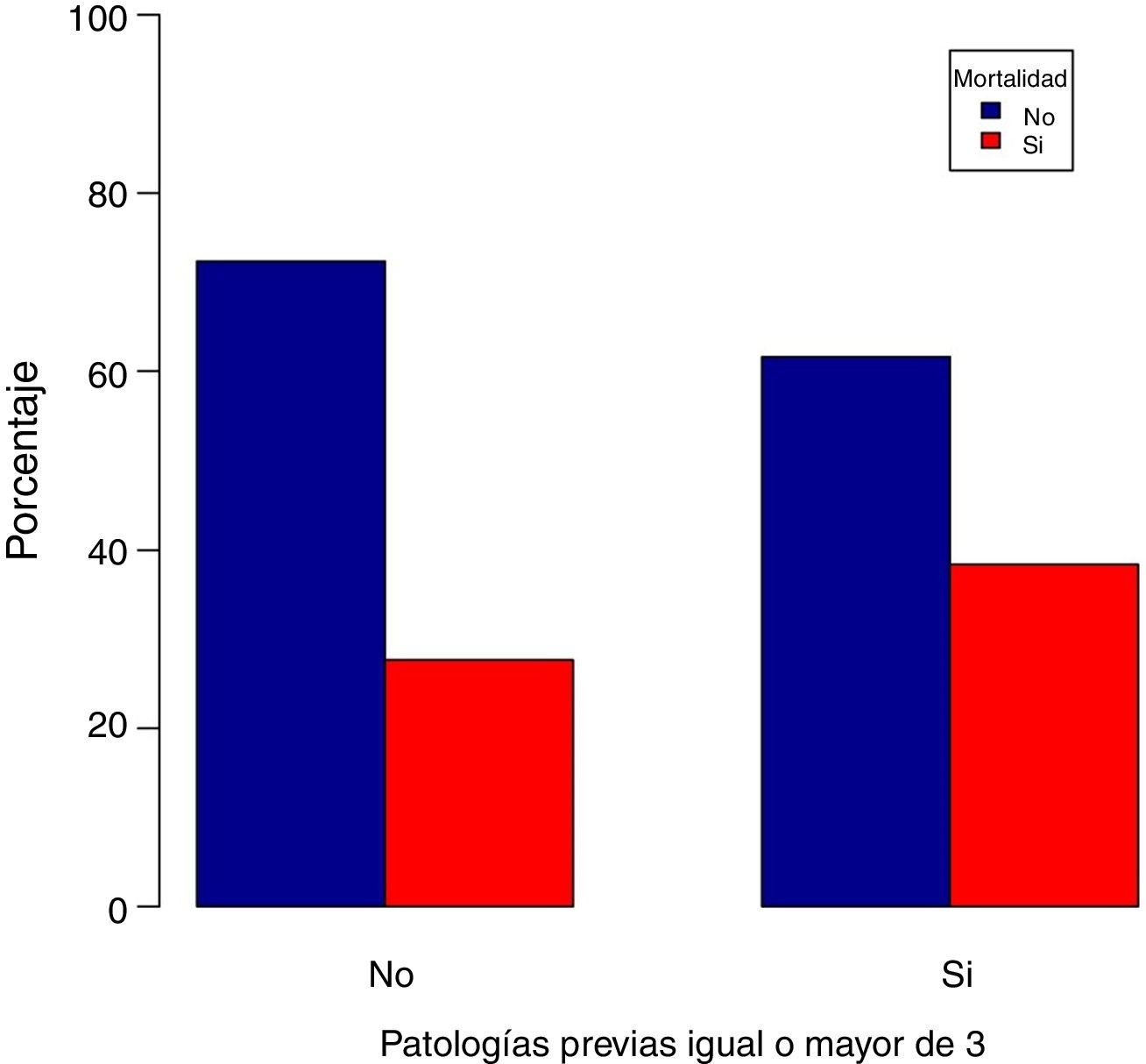
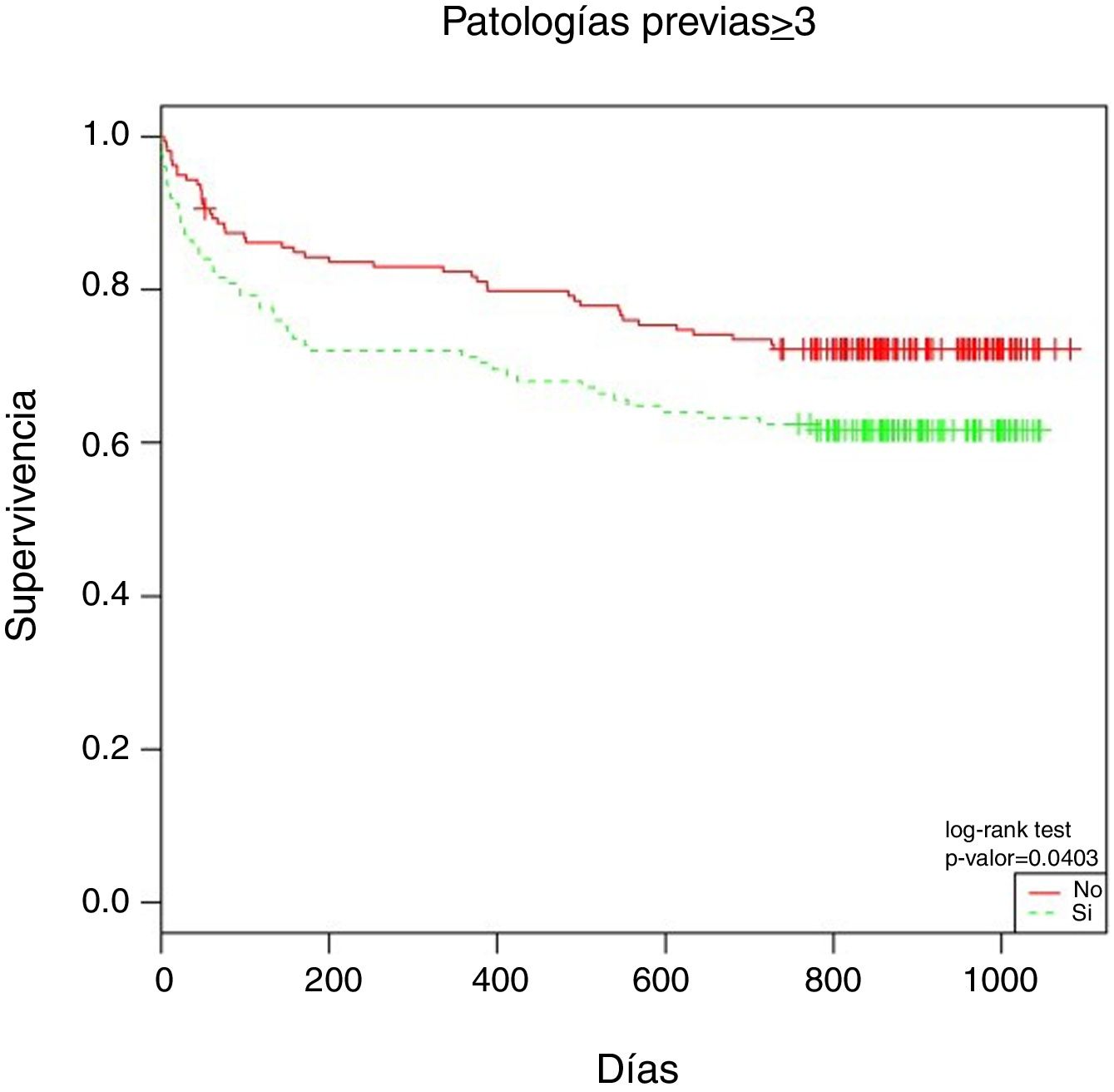
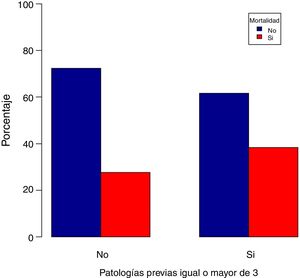
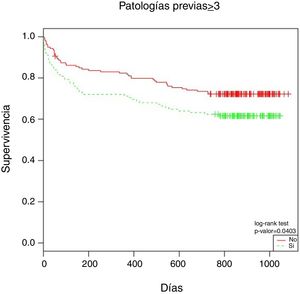
The patients with 3 or more pathologies had a higher rate of mortality (P = .007) (Fig. 1). The Kaplan-Meier survival table showed a fall in survival of 10.6% at the end of the study in those patients with more than 3 pathologies (P = .0403) (Fig. 2).
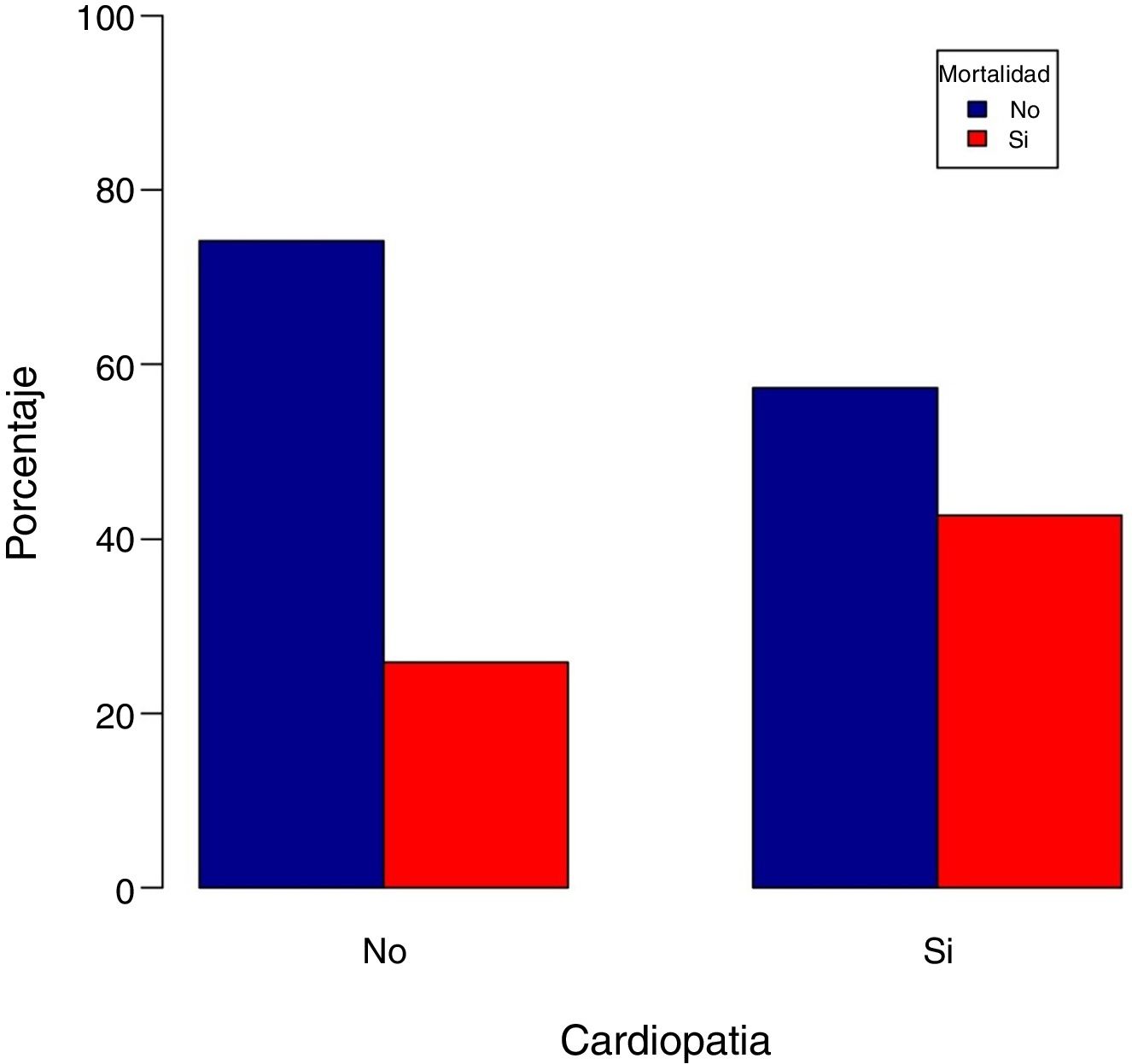
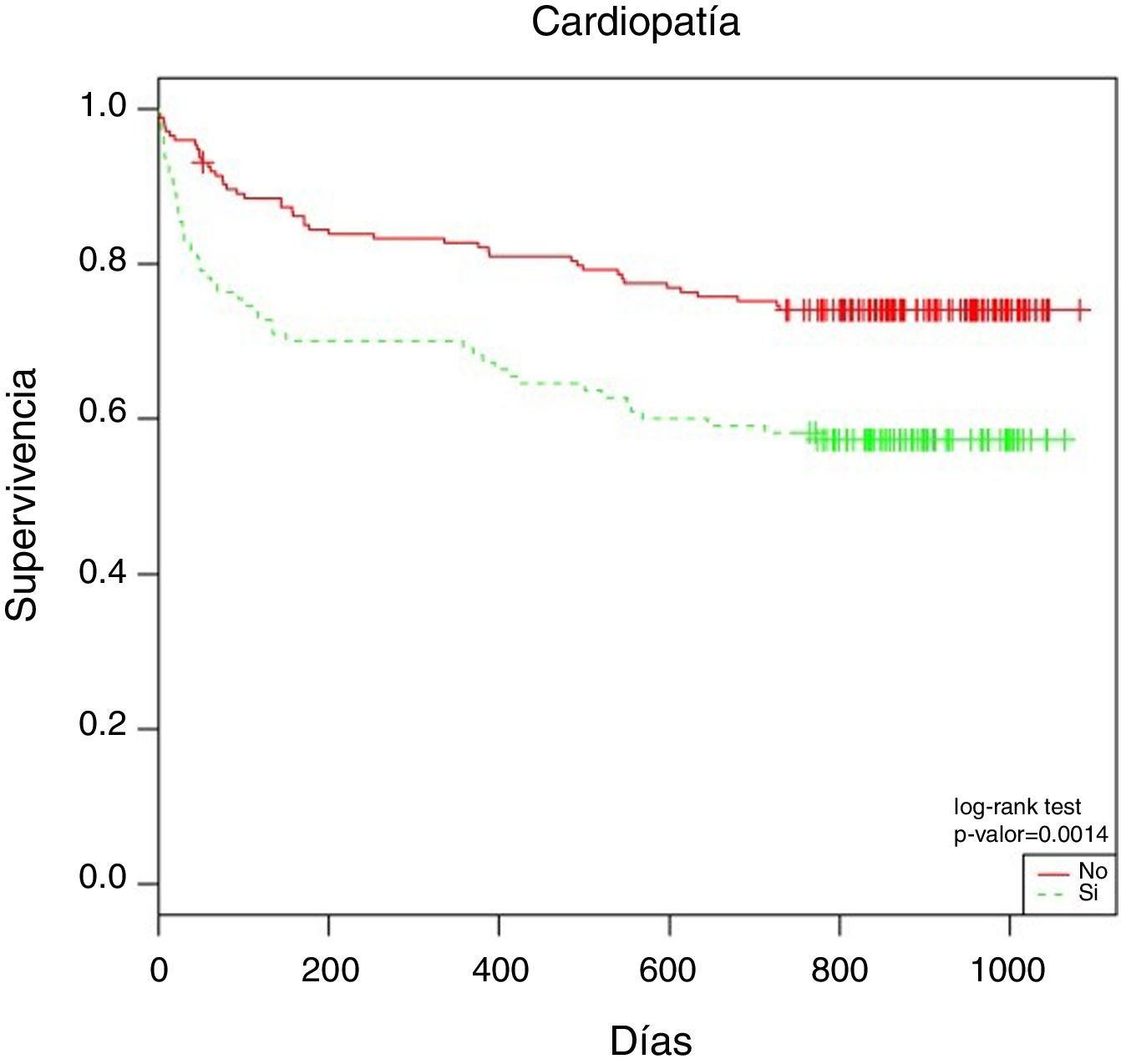
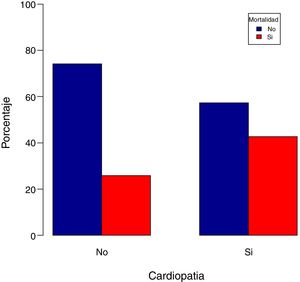
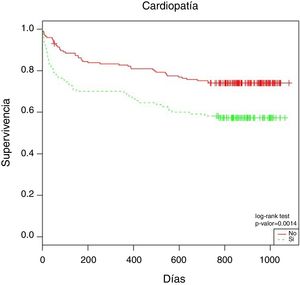
Of all the previous pathologies, the presence of heart disease influenced the mortality of these patients with hip fracture (P = .0047) (Fig. 3).
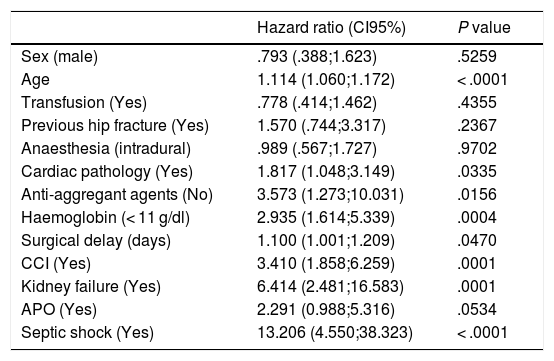
According to the Cox regression model for the study of survival at one year, having heart disease was found to increase the risk of death at one year by 81% (OR: 1.817; CI95%: 1.048; 3.149) and it is one of the most influential risk factors for mortality (Table 1).
Results of Cox’s regression models for survival at one year.
| Hazard ratio (CI95%) | P value | |
|---|---|---|
| Sex (male) | .793 (.388;1.623) | .5259 |
| Age | 1.114 (1.060;1.172) | < .0001 |
| Transfusion (Yes) | .778 (.414;1.462) | .4355 |
| Previous hip fracture (Yes) | 1.570 (.744;3.317) | .2367 |
| Anaesthesia (intradural) | .989 (.567;1.727) | .9702 |
| Cardiac pathology (Yes) | 1.817 (1.048;3.149) | .0335 |
| Anti-aggregant agents (No) | 3.573 (1.273;10.031) | .0156 |
| Haemoglobin (< 11 g/dl) | 2.935 (1.614;5.339) | .0004 |
| Surgical delay (days) | 1.100 (1.001;1.209) | .0470 |
| CCI (Yes) | 3.410 (1.858;6.259) | .0001 |
| Kidney failure (Yes) | 6.414 (2.481;16.583) | .0001 |
| APO (Yes) | 2.291 (0.988;5.316) | .0534 |
| Septic shock (Yes) | 13.206 (4.550;38.323) | < .0001 |
At 2 years after the fracture 74% of the patients without heart disease were still alive, while this was the case for only 57.2% of those who did have this form of pathology (Fig. 4).
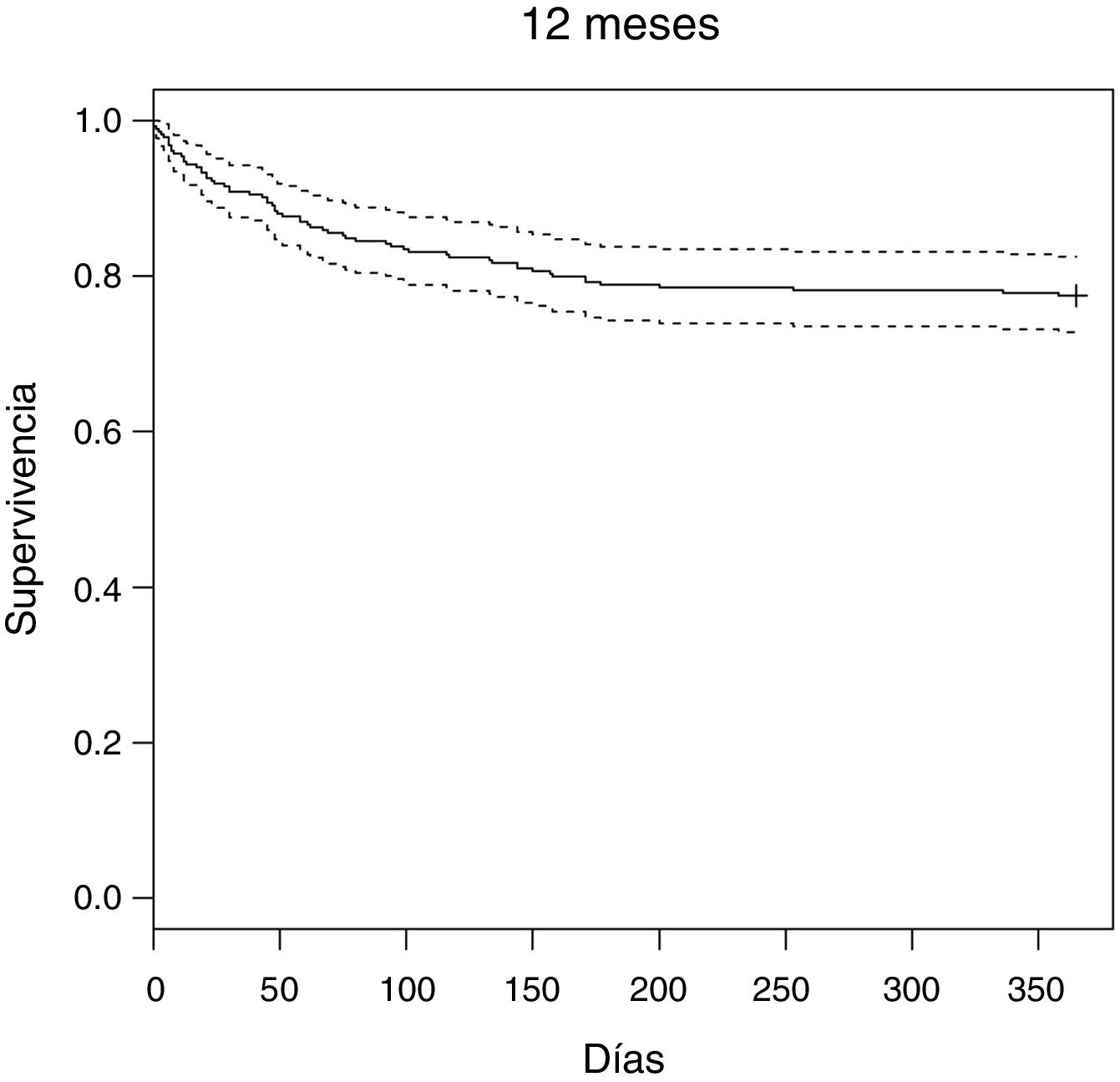
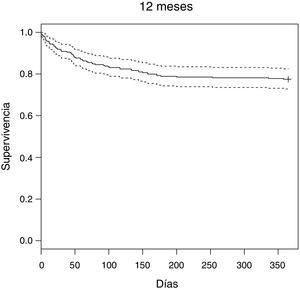
Survival analysis using Kaplan-Meier tables showed 84.5% survival of hip fracture patients after 3 months, 77.5% after one year (Fig. 5) and 67.5% at the end of the study.
The highest rates of mortality occurred during the 6 months after the hip fracture (59 patients died during this period of the total of 92 deaths; 64.13%) and this stabilised in the following months (Fig. 5). The probability of dying was 24.8% higher during the first 6 months than it was during the first year (OR:24.88; CI95%:13.12–47.20).
Estimated annual mortality (according to data entered in the web page using the CCI) was 29.68%. The actual mortality in our sample amounted to 22.5%. This real rate of mortality of 22.5% would be included within the 95% of the average range of mortality as estimated by the CCI (CI95%: 44.36−15).
DiscussionPatient mortality in the sample at the end of the study was 32.39%, with mortality of 15.1% at 3 months and 22.5% after a year. This datum is similar to those given in the majority of current studies, which record percentages that vary from 17% to 33% one year after the fracture.3,5,18,19
The highest rates of mortality in this study occur in the first 6 months after hip fracture, before stabilising in the following months. This agrees with reports by other authors such as Tosteson et al.20 and Rapp et al.,21 who state that the increase in mortality is maximum during the first 6 months, which is when almost half of the deaths of patients with hip fracture occur. However, it is hard to state how long hip fracture influences mortality, given that the bibliography shows that this question is somewhat controversial. Alffram22 stated that the highest rate of mortality occurs in the first 3 months, while Holmberg et al.23 and Larsson et al.24 state that this corresponds to the first year, and Jensen y Töndewold25 describe survival stabilisation as occurring 19 months after the fracture.
In this study we found that previous and concomitant diseases of patients with a hip fracture are a strong mortality predictor. This agrees with numerous series8–10 that report that the presence of previous diseases and a poor state of health have a negative influence on survival after hip fracture.
44% of our sample had 3 or more pathologies, and these patients were found to suffer a significantly higher rate of mortality. Survival analysis shows that at the end of the study 38.4% of the patients with 3 or more pathologies had died. This is similar to the report by Pitto26 that half of the patients with 3 or more previous pathologies died.
Of all the severe diseases included in this study, the one most strongly associated with mortality was cardiovascular disease. In the Cox regression multivariate model the risk of a patient with heart disease dying amounts to 81% in one year. This coincides with the finding by Stavrou et al.,27 who state that heart-respiratory disease increases mortality by a very significant amount.
Nevertheless, we did not find any higher rate of mortality in association with other major pathologies, such as dementia, cerebrovascular accident, psychiatric pathology, kidney failure, Parkinson’s disease, tumoral pathology or chronic pulmonary pathology, among others.
Determining which mortalities are due to hip fracture and which are due to previous diseases is a common problem. In this study the CCI allowed us to approximately evaluate this question.
Hip fracture is unable to modify the estimation of survival obtained according to the CCI, so that it does not cause an increase in mortality at one year for these patients. Nevertheless, it probably is an influential factor in early mortality, given that 64.13% of total mortality at 2 years occurs in the first 6 months. This fact may be explained by the fact that these patients would have died due to another cause (pneumonia, heart disease…) if they had not suffered hip fracture, so that hip fracture in itself does not lead to higher mortality.
We therefore agree with Wehren and Magaziner13 that previous pathology in these patients is the main risk factor for mortality, and that mortality depends more on their general previous state than it does the fracture. We differ from other authors3,14,28,29 who state mortality occurs more often and earlier in the least healthy individuals, although the fracture itself leads to higher mortality.
This study has certain weaknesses as it has no control group. This hinder comparison with a population of the same age and pathology, so that we compare actual mortality with the mortality that would be expected according to the CCI. In spite of its limitations, we accept this expected rate of mortality because the CCI is described in the literature as a good mortality predictor.30
To conclude, the previous existence of diseases is the most important predictive factor for mortality in these patients. Although hip fracture does not cause an increase in annual mortality according to the estimation of the CCI, it does do so in the first 6 months after the fracture, acting as a factor which accelerates the said rate.
FinancingThis study received no external financing.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Blanco-Rubio N, Gómez-Vallejo J, Torres-Campos A, Redondo-Trasobares B, Albareda-Albareda J. ¿Es mayor la mortalidad en los pacientes que han sufrido una fractura de cadera? Rev Esp Cir Ortop Traumatol. 2021;65:85–90.