Tibial plafond fractures are one of the most challenging injuries in orthopaedic surgery. Their results could be improved by following the new guidelines for the management, and modern plating techniques. The results and complication rate between anteromedial and anterolateral approach for open reduction and internal fixation of these fractures were compared.
Material and methodsA study was conducted on 40 patients treated by open reduction an internal fixation between 2007 and 2008. The surgical approach was selected by the surgeon in charge, depending on fracture pattern and skin situation. Patients were evaluated clinically and radiographically by an independent orthopaedic surgeon, who was not involved in the surgical procedure, using clinical (American Orthopaedic Foot and Ankle Society score) and radiological criteria at a minimum of 2 years. The appearance of complications after both approaches was recorded.
ResultsForty patients were included. The mean age was 53 years, with 24 males and 16 females. Seventeen of the injuries were of high energy, and there were 8 open fractures (3 of type i, 4 type ii and one type iii), and 12 of the closed injuries were grade ii or iii in the Tscherne classification. Six patients (15%) had associated injuries. At final follow-up there were 33 (82%) excellent or good results. No statistical differences were found between either surgical approach regarding time to bone union, rate of delayed union and infection rate. Three plates of the anteromedial group and none of the anterolateral group needed to be removed.
ConclusionOpen reduction and internal fixation of distal tibia fractures produced reliable results, with no statistical differences found between anteromedial and anterolateral surgical approaches. Clinical and radiological results and complication rate were mainly related to the fracture type.
Las fracturas de pilón tibial constituyen una de las lesiones más difíciles de tratar en cirugía ortopédica. Los nuevos protocolos y las modernas placas pueden mejorar los resultados. Comparamos los resultados y la tasa de complicaciones entre el abordaje anteromedial y anterolateral para la reducción abierta y fijación interna.
Material y métodosSe estudiaron de forma prospectiva 40 pacientes tratados mediante reducción abierta y fijación interna entre 2007 y 2008. El abordaje fue seleccionado por el cirujano, dependiendo del patrón de fractura y de la situación de la piel. Los pacientes fueron evaluados clínica y radiológicamente por un cirujano independiente, utilizando criterios clínicos (puntuación de la Sociedad Americana de Ortopedia de Pie y Tobillo) y radiológicos a un mínimo de 2 años. Se registró la aparición de complicaciones de ambos abordajes.
ResultadosCuarenta pacientes fueron incluidos. La media de edad fue de 53 años, había 24 hombres y 16 mujeres, 17 fracturas fueron de alta energía y hubo 8 abiertas (3 de tipo i, 4 de tipo iiI y una de tipo iii), y 12 de las lesiones cerradas eran de grado ii o iii de la clasificación de Tscherne. Seis pacientes (15%) presentaron lesiones asociadas. Al final del seguimiento hubo 33 (82%) resultados excelentes o buenos. No se encontraron diferencias estadísticas entre ambos abordajes con respecto al tiempo de consolidación, tasa de retardo de consolidación y tasa de infección. Fueron extraídas tres placas anteromediales y ninguna anterolateral.
ConclusiónLa reducción abierta y fijación interna de la fractura de pilón tibial proporciona buenos resultados; no se pudo encontrar diferencias estadísticas entre los abordajes anteromedial y anterolateral. Los resultados clínicos y radiológicos y la tasa de complicaciones se relacionan principalmente con el tipo de fractura.
Treatment of tibial plafond/pilon fractures is challenging due to the difficulty of achieving an anatomical reduction without complications.1 New plates with an anatomically preformed low profile and angular stability are promising elements for this procedure. However, there is controversy in the literature regarding the best approach for the management of these fractures.
The anteromedial approach enables a good visualisation of the central and medial thirds of the tibial pilon, but provides poor soft tissue coverage and the rate of wound complications is high.2 Minimally invasive techniques can be used for the indirect reduction of the fracture, thus preserving the anatomy and avoiding problems with soft tissues.2–4 However, this method is technically demanding, especially in complex fractures.4–6
The anterolateral approach is preferred in cases of fractures of the lateral column of the tibial plafond associated with fibular fractures and syndesmosis injury. The lateral surface of the distal tibia has a better soft tissue cover, and the fibular Chaput tubercle may be displaced to allow reduction of the posterior fragments.7 The Bohler modification of the anterolateral approach allows exposure of the entire Chaput fragment.8 Some complex fractures require conducting an extended approach in order to reduce and fix both columns.9
The aim of this study is to compare the results and complication rates between the anteromedial and anterolateral approaches for open reduction and internal fixation of tibial plafond fractures.
Material and methodsWe prospectively evaluated 40 consecutive patients with tibial plafond fractures between January 2007 and December 2008. The inclusion criteria for the study covered all the tibial plafond fractures treated in our hospital during the study period. Tibial plafond fracture was defined as a fracture with a line within 4cm of the joint. All the patients were treated by open reduction and plate fixation. In each case, the primary surgeon decided which approach and plate design to use.
The postoperative protocol consisted of immobilisation with a sural-foot splint at 90° dorsiflexion until healing of the soft tissues took place. Load was not permitted for a period of 8–12 weeks. Thromboprophylaxis with low molecular weight heparin was used for 4 weeks, as well as antibiotic prophylaxis with cefazolin (vancomycin if the patient was allergic) for 48h.
Open fractures were classified according to the Gustilo and Anderson classification and treated with early debridement and irrigation.10 Soft tissue damage in closed fractures was classified according to the Tscherne classification.11 We used a temporary external fixator for those patients with soft tissue problems. Definitive treatment with open reduction and plate fixation was delayed until the healing of soft tissues.
Patients were evaluated clinically and radiologically by an independent orthopaedic surgeon who was not involved in the operation at 1, 3 and 6 months and 1 and 2 years after surgery. The American Orthopaedic Foot and Ankle Society (AOFAS) scale12 was used for clinical assessment. We also collected information on the presence of soft tissue necrosis and infection. Wound or soft tissue complications were considered as major complications if their treatment required surgery. Removal of material was considered after fracture consolidation if it caused symptoms.
We used anteroposterior and lateral ankle radiographs with a standard technique at the time of fracture to evaluate their patterns. Fractures were classified according to the AO/OTA classification.13 During follow-up we used the anteroposterior and lateral ankle radiographs to assess the quality of the reduction, secondary displacement, consolidation and presence of degenerative changes in the ankle joint.
Fractures were considered consolidated when radiographs showed 3 bone bridge corticals and weight load without significant pain was possible. Consolidation was considered delayed if the time exceeded 6 months from the injury. Pseudoarthrosis or nonunion was considered if no bone consolidation had taken place 9 months after the injury. Septic nonunions were managed by removal of the plate and use of an external fixator. Aseptic nonunions were treated with iliac crest autografts and fixation of the fracture using new plates. Fracture malunion was defined as a joint step of more than 1mm, an angulation greater than 5° in any plane or shortening of over 1cm.14,15 The presence of ankle osteoarthritis was evaluated according to the Kellgren and Lawrence criteria.16
We used the Statistical Package for Social Sciences (SPSS 12.0, Chicago, IL, USA) software program for the statistical analysis. The level of statistical significance was set at P<.05.
ResultsThe mean age at the time of fracture was 53 years (range: 22.9–92.1 years). There were 24 males and 16 females; 17 right leg fractures and 23 left leg fractures, and 17 high-energy fractures and 23 low-energy fractures. A total of 6 (15%) patients presented associated injuries (1 fracture of the lumbar spine, 2 contralateral tibial shaft fractures, 1 contralateral calcaneal fracture, 1 ankle fracture and 1 fracture of the humerus).
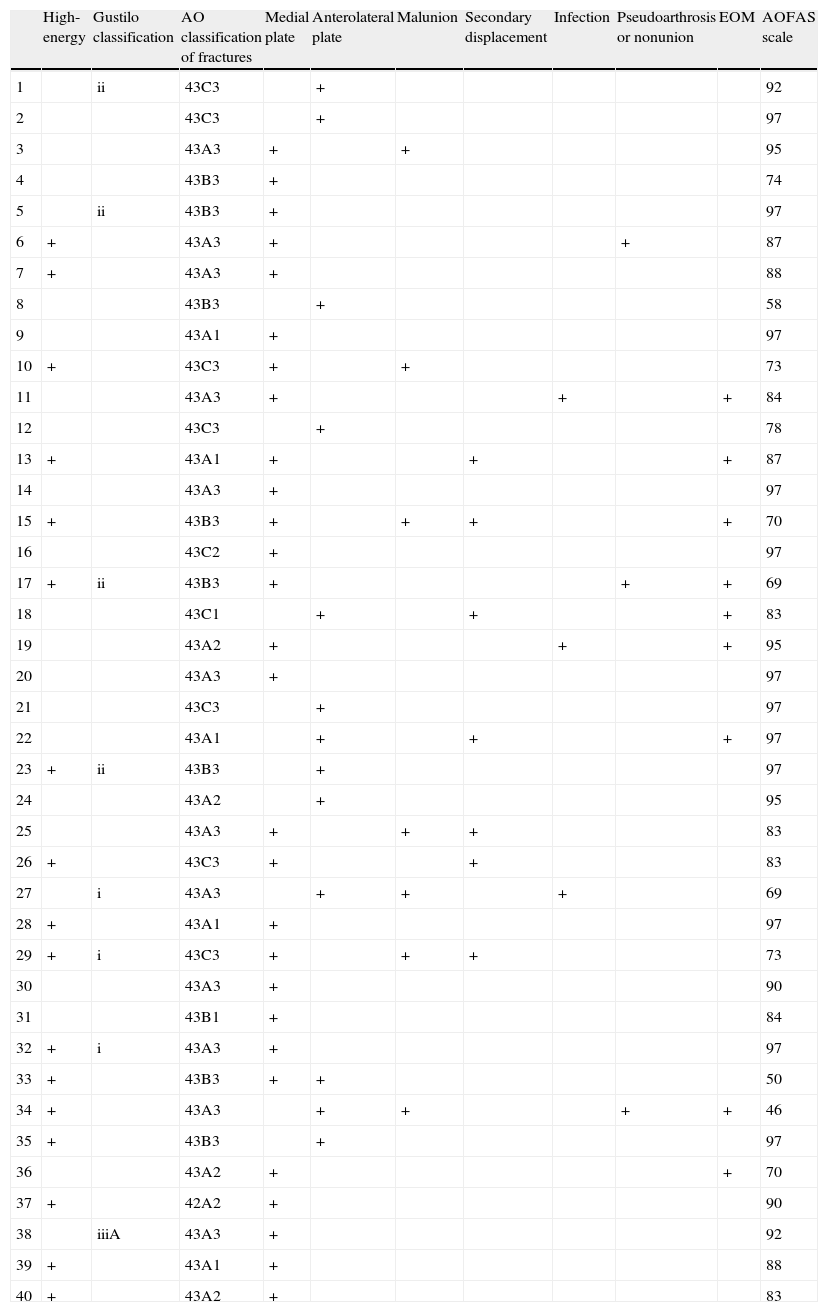
The radiographic classification included: 22 type A fractures (5 A1, 5 A2 and 12 A3), 9 type B fractures (1 B1 and 8 B3) and 9 type C fractures (1 C1, 1 C2 and 7 C3). A total of 33 (82.5%) cases suffered associated fibular fracture. There were 8 open fractures which were classified according to the Gustilo classification: 3 as type I, 4 as type II and 1 as type III.10 In closed fractures, soft tissue damage was present in 12 patients (grade II or III of the Tscherne classification)11 (Table 1).
Results.
| High-energy | Gustilo classification | AO classification of fractures | Medial plate | Anterolateral plate | Malunion | Secondary displacement | Infection | Pseudoarthrosis or nonunion | EOM | AOFAS scale | |
| 1 | ii | 43C3 | + | 92 | |||||||
| 2 | 43C3 | + | 97 | ||||||||
| 3 | 43A3 | + | + | 95 | |||||||
| 4 | 43B3 | + | 74 | ||||||||
| 5 | ii | 43B3 | + | 97 | |||||||
| 6 | + | 43A3 | + | + | 87 | ||||||
| 7 | + | 43A3 | + | 88 | |||||||
| 8 | 43B3 | + | 58 | ||||||||
| 9 | 43A1 | + | 97 | ||||||||
| 10 | + | 43C3 | + | + | 73 | ||||||
| 11 | 43A3 | + | + | + | 84 | ||||||
| 12 | 43C3 | + | 78 | ||||||||
| 13 | + | 43A1 | + | + | + | 87 | |||||
| 14 | 43A3 | + | 97 | ||||||||
| 15 | + | 43B3 | + | + | + | + | 70 | ||||
| 16 | 43C2 | + | 97 | ||||||||
| 17 | + | ii | 43B3 | + | + | + | 69 | ||||
| 18 | 43C1 | + | + | + | 83 | ||||||
| 19 | 43A2 | + | + | + | 95 | ||||||
| 20 | 43A3 | + | 97 | ||||||||
| 21 | 43C3 | + | 97 | ||||||||
| 22 | 43A1 | + | + | + | 97 | ||||||
| 23 | + | ii | 43B3 | + | 97 | ||||||
| 24 | 43A2 | + | 95 | ||||||||
| 25 | 43A3 | + | + | + | 83 | ||||||
| 26 | + | 43C3 | + | + | 83 | ||||||
| 27 | i | 43A3 | + | + | + | 69 | |||||
| 28 | + | 43A1 | + | 97 | |||||||
| 29 | + | i | 43C3 | + | + | + | 73 | ||||
| 30 | 43A3 | + | 90 | ||||||||
| 31 | 43B1 | + | 84 | ||||||||
| 32 | + | i | 43A3 | + | 97 | ||||||
| 33 | + | 43B3 | + | + | 50 | ||||||
| 34 | + | 43A3 | + | + | + | + | 46 | ||||
| 35 | + | 43B3 | + | 97 | |||||||
| 36 | 43A2 | + | + | 70 | |||||||
| 37 | + | 42A2 | + | 90 | |||||||
| 38 | iiiA | 43A3 | + | 92 | |||||||
| 39 | + | 43A1 | + | 88 | |||||||
| 40 | + | 43A2 | + | 83 |
AOFAS: American Orthopaedic Foot and Ankle Society scale score; EOM: extraction of osteosynthesis material.
The mean time from the accident until surgery was 7.5 days (range: 0–40 days). In 9 (22.5%) patients without significant soft tissue injury, surgery was performed within the first 24h. In total, 11 fractures were initially managed with external fixation due to soft tissue problems. The external fixator was maintained for a mean period of 13.45 days (range: 8–40 days). A total of 27 patients were treated with a distal tibial locking compression plates (LCP) (Synthes, Paoli, PA, USA) through an anteromedial approach (in 6 cases without intraarticular involvement, the plates were placed percutaneously). A total of 12 fractures were treated with anterolateral plates (Synthes) (Figs. 1 and 2).
One fracture with significant comminution required plates in both columns through an extended approach. Bone grafts were used in 8 fractures. There were no statistically significant differences regarding the types of fracture (type, mechanism, associated injuries) or regarding patients between the anterolateral and anteromedial groups.
At the end of the follow-up period there were 33 (82%) excellent and good results. The mean AOFAS score was 84.9 points (range: 46–97 points). Anatomical reduction was achieved in 33 (82.5%) cases. We found a higher rate of anatomical reductions among type A (81.8%) and type B (88.9%) fractures than among type C fractures (77.8%).
There were 7 (17.5%) losses of secondary reduction during follow-up (5 with anteromedial plates and 2 with anterolateral plates). We could not find statistically significant differences between the anteromedial and anterolateral plates regarding the quality of the reduction (P=.88) or the secondary displacement of the fracture (P=.88). At the end of the follow-up period, 5 (12%) ankles presented mild degenerative changes without clinical symptoms which made it necessary to conduct additional procedures.
The mean consolidation time was 18.1 weeks (range: 8–32 weeks). Delayed union was observed in 5 (12%) cases; 3 cases had been treated with an anteromedial plate and the other 2 with an anterolateral plate. No statistically significant differences were found regarding the rate of delayed union between both groups (P=.63). In total, 4 cases were high-energy fractures, but we could not find statistically significant differences regarding the mechanism of fracture. A total of 3 cases suffered infection and required external fixation until fracture consolidation. The cases of aseptic nonunion were treated with iliac crest autografts and new plates.
Deep infection appeared in 3 (7.5%) fractures (2 were open fractures and 1 was a closed fracture), 2 after an anteromedial plate and 1 after an anterolateral plate. There were no statistically significant differences in infection rates between both methods (P=.92) or between open and closed fractures (P=.54), which is probably not significant due to the small sample size. All the infections were successfully treated with surgical debridement, implant removal, external fixation and antibiotic therapy.
Five (12.5%) patients required a graft; 4 patients due to skin necrosis with wound dehiscence and exposure of material and 1 patient due to the development of compartment syndrome which required surgery to close the medial fasciotomy. A total of 3 anteromedial plates generated discomfort and were withdrawn after fracture consolidation.
DiscussionPatients suffering tibial plafond fractures present poorer scores on functional and overall health scales compared to control subjects.17,18 In our series, the functional outcomes for the ankle joint were good in most of the patients, with a mean AOFAS score of 85 points, similar to other series of patients treated with modern plates.5,6 Patients treated with external fixation suffered more pain and less range of motion than patients treated with open reduction and internal fixation.18 Complications were more common after fractures of type C3.19 Anatomical reduction could only be achieved in 78% of type C fractures and these patients presented a worse clinical outcome. The quality of the reduction was more related to the type of fracture than to the approach employed.
Depending on the fixation method, it is difficult to achieve and maintain an adequate reduction and alignment following tibial plafond fractures. Fractures treated by intramedullary nailing suffer alignment problems in 7–35% of cases,15,20 whilst fractures treated with external fixation suffer them in 19–25% of cases.21,22 Distal tibial plates enable a more accurate reduction of fractures. Blocked plates provide greater rigidity and load than standard plates.23 However, there are have been reports of high rates of malunion and a long learning curve when using percutaneous plates.4,6,24,25 Modern plates provide good axial stability, although Collinge et al. report secondary displacement in 7% of cases.5
Nonunion and delayed union are common complications following distal tibial fractures treated with traditional approaches.26 Minimally invasive techniques offer excellent consolidation rates, with lower bone graft requirements.27 However, 35% of high-energy fractures treated by minimally invasive plate osteosynthesis (MIPO) require a second surgical procedure to achieve consolidation.5 Our series, as most other studies, included both low- and high-energy fractures. We found no differences in the consolidation rates between medial and lateral plates. This supports the idea that the consolidation rate depends more on the mechanism of injury than on the surgical approach employed.
The rate of soft tissue complications has decreased after the establishment of a treatment protocol in 2 stages.1,28 In our study, the rate of soft tissue problems was 12.5%, which seems to be more related to the injury itself than to the technique employed. Despite using minimally invasive techniques, Collinge et al. found soft tissue complications in 19% of patients with high-energy trauma. We found a similar rate of wound problems with both approaches. Chen et al. reported a wound complication rate of 8% using a medial or lateral approach.29 The mean age of our series was high. Thus, although external fixation was used extensively, the occurrence of complications was frequent. The low rate of complications was similar to other series and could be attributed to the use of external fixation until the recovery of soft tissues, as well as to the rate of low-energy fractures. There were 3 (7.5%) cases of infection. The onset of infection was similar with both methods and similar to that in other published series.30
Some of the limitations of this study included the small number of patients and the involvement of several different surgeons. The type of method employed was decided by the surgeon depending on the fracture pattern, rather than randomised. The study included low- and high-energy fractures in all age groups. The strengths of this work include it being a prospective study, not losing any patients during follow-up and a monitoring period of over 2 years.
In short, open reduction and internal fixation of distal tibial fractures provide reliable results. No differences were found between the 2 approaches regarding the clinical and radiographic results. The onset of complications appeared to depend more on the injury itself that on the type of approach employed to manage the fractures.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Encinas-Ullán CA, et al. Placas mediales versus laterales para las fracturas de pilón tibial: estudio prospectivo de 40 fracturas. Rev Esp Cir Ortop Traumatol. 2013;57:117-22.