Femoroacetabular impingement (FAI) is a clinical syndrome relatively recently recognised as source of hip mechanic pain and early osteoarthritis. Two types of FAI have been described, based on the bone morphology and pattern of chondral and labral damage; the cam type is frequently associated with chondral delamination; and the pincer type is associated with a contre-coup injury of the posteroinferior acetabulum. A close relationship between the zone of acetabular overcoverage or retroversion and the area of acetabular chondral delamination has been observed.
ObjectiveTo evaluate the relationship between the acetabular overcoverage or retroversion zone, and the cartilage delamination area; and whether by treating the overcoverage zone, the cartilage delamination area itself is also treated.
MethodsA prospective evaluation was conducted for 16 patients (17 hips) with FAI and chondral delamination treated with acetabular trimming and labral reinsertion, and femoral bump resection.
ResultsAll the cases had chondral delamination in the anterosuperior acetabular area, corresponding to the overcoverage or retroversion zone. In the 16 patients (94% of the hips) after the acetabular overcoverage bone resection, the remaining cartilage was stable and without delamination. Only one case (6%) required microfractures to treat the exposed subchondral bone after delaminated cartilage debridement.
ConclusionThe acetabular chondral delamination area has a very close relationship with the acetabular overcoverage zone, meaning that the delamination area can be treated by trimming the overcoverage zone.
El pinzamiento femoroacetabular es un síndrome reconocido como fuente de coxalgia y artrosis temprana de cadera. Están descritos 2 tipos de pinzamiento según la alteración ósea predominante, que se asocia a daños condrales característicos. El tipo cam (o leva) frecuentemente se asocia a delaminación condral; el tipo pincer (o pinza) se asocia a lesión por contragolpe en el aspecto posteroinferior del acetábulo. Nosotros hemos observado una estrecha asociación entre la zona de sobrecobertura o retroversión acetabular (alteración tipo pincer) y el área de delaminación condral (típicamente asociada con el pinzamiento tipo cam).
ObjetivoEvaluar la correlación entre la zona de sobrecobertura o retroversión acetabular y el área de delaminación condral, y si al tratar la alteración tipo pincer, se elimina el área de delaminación.
MétodosEstudio prospectivo de 16 pacientes (17 caderas) con pinzamiento y delaminación condral, tratadas con fresado acetabular y reinserción labral, además de osteoplastia femoral en los casos necesarios.
ResultadosTodos los casos presentaban la delaminación condral en el área acetabular anterosuperior, correspondiente a la zona de sobrecobertura o retroversión. En 16 caderas (94%) después de resecar la sobrecobertura acetabular se eliminó la zona delaminado dejando el cartílago remanente estable. Solo un caso (6%) requirió microfracturas para tratar el hueso subcondral expuesto después de resecar la sobrecobertura acetabular y el cartílago delaminado.
ConclusiónLa delaminación condral acetabular tiene una fuerte asociación con la zona de sobrecobertura o retroversión, lo que permitiría tratar la delaminación condral al eliminar el pincer.
Femoroacetabular impingement (FAI) is a clinical syndrome recognised as a source of mechanical hip pain and a cause of early coxarthrosis.1 Subtle morphological changes in the acetabulum and/or femoral head–neck union result in an abnormal contact throughout the range of motion of the hip, thus leading to the development of labral and chondral lesions.2
There are 2 types of FAI, as described by Ganz et al.1 based on bone morphology patterns. The “cam” type is characterised by an alteration at the level of the femoral head–neck junction, which increases the radius of the head and forces this aspherical head into the acetabulum, thus causing labral lesions and chondral delamination more frequently in the anterosuperior region of the acetabular cup.1,2 The “pincer” type is characterised by an acetabular alteration, which leads to an abnormal overcoverage of the femoral head, either by coxa profunda or acetabular retroversion, causing labral tear and chondral lesions due to a “contrecoup” or counterblow in the posteroinferior aspect of the acetabulum.1,2 However, in most of the cases we face a combination of both conditions, determining a mixed-type FAI.2
Classically, chondral delamination has been associated with cam-type impingement.2 However, relatively recent studies3 suggest that the linear contact of pincer-type FAI could, in theory, be even protective for chondral delamination (although, this has not yet been demonstrated).
In contrast, we have observed a strong association between the area of overcoverage or acetabular retroversion (anterolateral) and the area of chondral delamination (anterosuperior).
The purpose of this study is to prospectively evaluate the association between the area of overcoverage and that of chondral delamination, as well as to assess whether treatment and elimination of the acetabular overcoverage area also eliminates the area of delaminated cartilage.
MethodsThis was a prospective study in patients suffering from FAI and chondral delamination who were treated at our institution between June and October 2008. We recorded the preoperative clinical condition of patients, findings on preoperative arthro-magnetic resonance imaging (arthro-MRI) scan, intraoperative findings and short-term clinical condition (minimum of 6 months postoperatively).
The inclusion criteria for the study were: (1) diagnosis of FAI; (2) complete preoperative study including radiographic images, hip arthro-MRI informed by a specialist osteoarticular radiologist and positive lidocaine test (we considered as positive those lidocaine tests in which pain decreased over 50% through intraarticular injection of 5cm3 of lidocaine); (3) no previous history of hip surgery; and (4) presence of chondral delamination detected intraoperatively (with or without labral lesion).
We excluded from the study those patients with: (1) radiological signs of osteoarthritis (Tönnis II or III); (2) loss of monitoring; and (3) chondral lesions other than delamination (Outerbridge I–IV).4
The preoperative and postoperative clinical condition was assessed using the modified Harris hip score (MHHS).
The preoperative evaluation included plain radiographs of the pelvis (well-centred anteroposterior [AP] projection) and hip (AP and true axial or cross-table), as well as arthro-MRI with positive lidocaine test. We considered as pincer-type cases those with presence of overcoverage with a Wiberg angle (centre-edge angle)5 greater than 35° (Fig. 1) and/or acetabular retroversion (signs of crossover; all retroversions were partial or focal, with no patients in our sample presenting overall retroversion) (Fig. 2), both in well-centred AP pelvis radiographs.
Measurement of the Wiberg angle (centre-edge), defined by 2 lines: the first is perpendicular to the horizontal of the pelvis and passes through the centre of the femoral head, whilst the second line connects the centre of the femoral head with the most supero-lateral point of the acetabular roof.
All the procedures were performed by the same surgical team and recorded in our specific form for hip arthroscopy.6
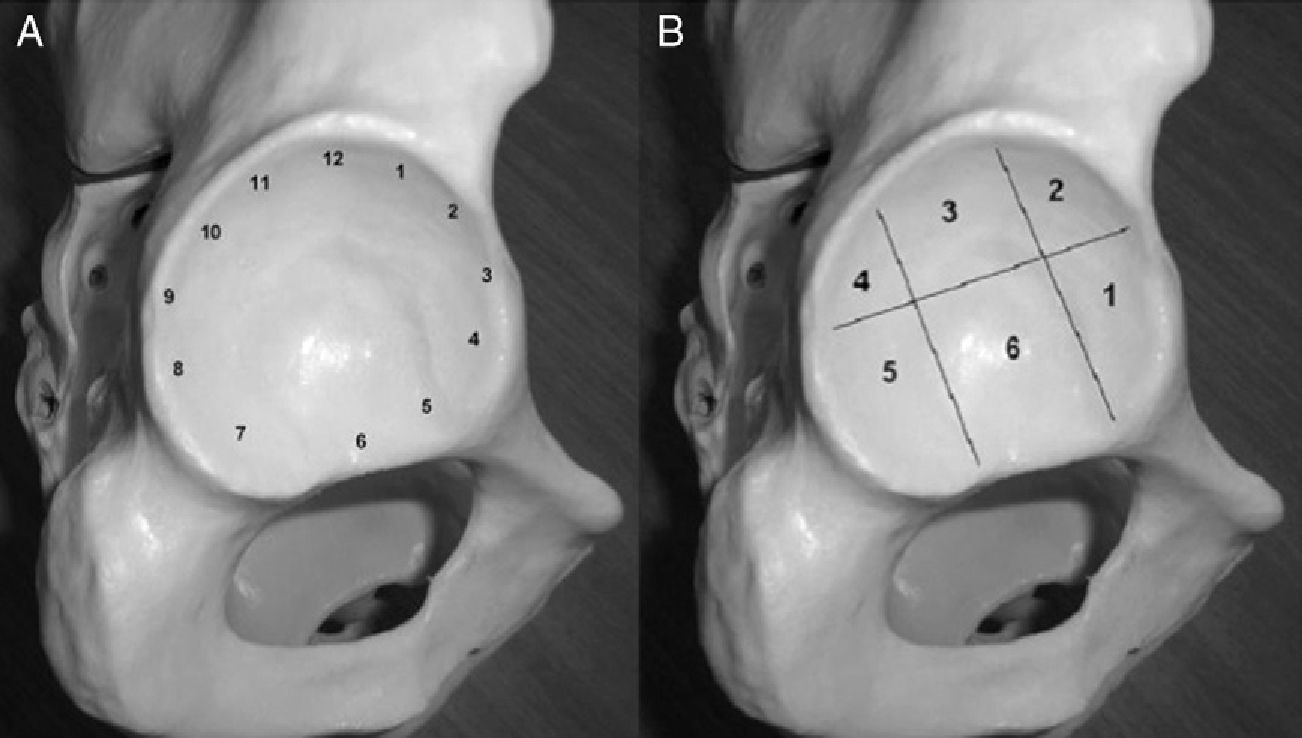
We evaluated the presence of chondral delamination with and without labral lesion, and noted its location according to geographical and time (clockwise) description methods (Fig. 3).7
A total of 49 hip arthroscopies were performed for FAI at our centre between June and October 2008. Of these, 17 met the inclusion criteria (15 females and 2 males). The mean age was 32.7 years (age range between 16 and 52 years). There were 4 cases of pincer-type FAI, 1 case of cam-type FAI and 12 mixed cases.
Surgical techniqueAll the patients had received combined anaesthesia for lumbar plexus blockage plus general anaesthesia.
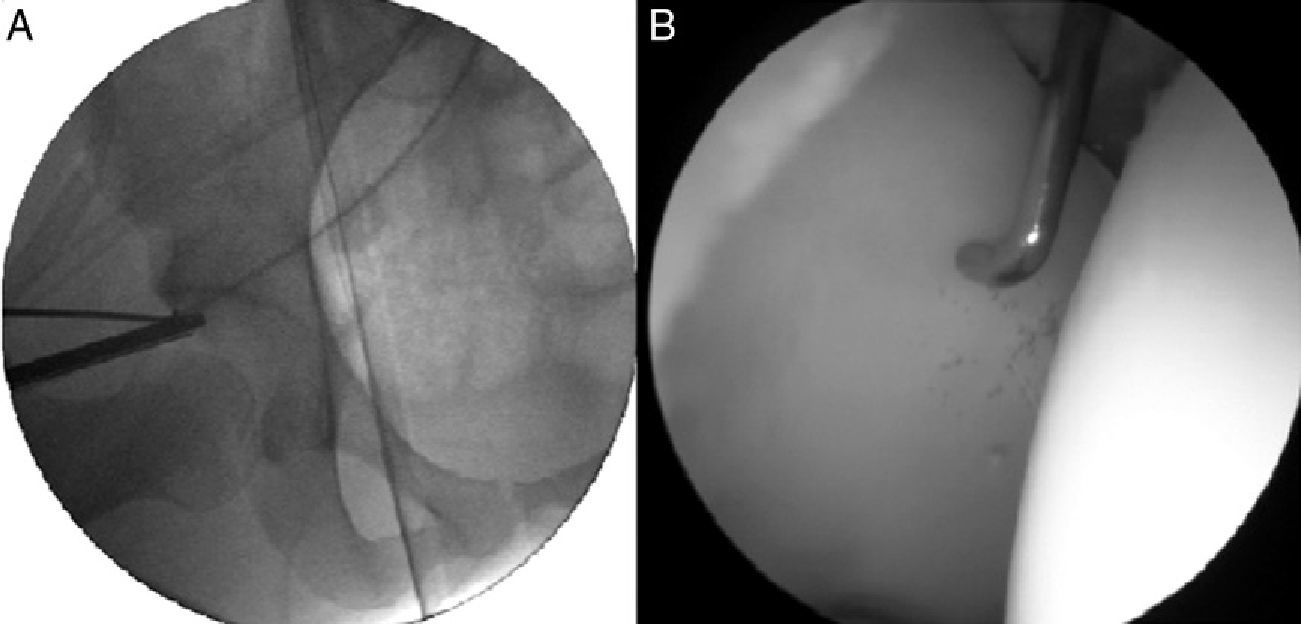
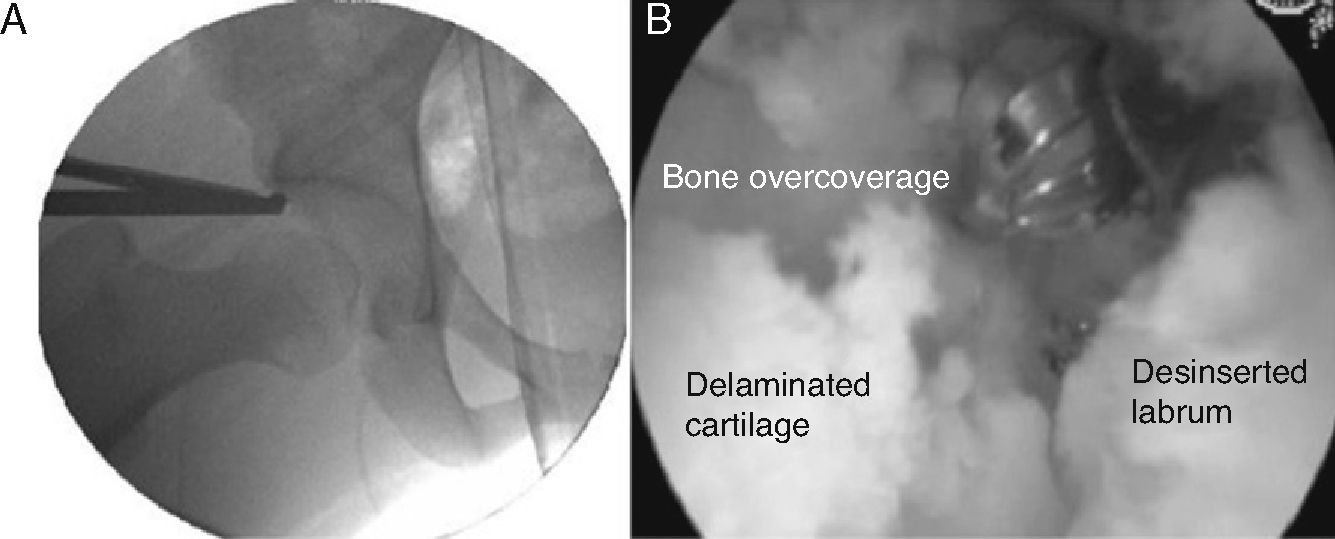
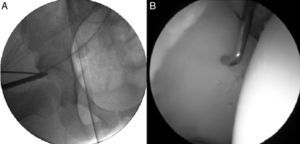
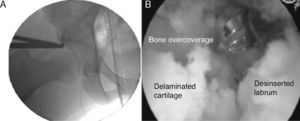
Arthroscopy was conducted through the anterolateral (ALP) and anterior accessory (AAP) portals, identifying the chondral delamination area, the area of acetabular overcoverage and the femoral hump. We correlated the overcoverage area (under radiographic vision) and the chondral delamination area (under direct vision) and evaluated this correlation (Fig. 4).
After achieving an adequate exposure of the acetabular edge overcoverage, this was normalised with a high-speed 4.5 drill under radiographic control, in order to remove the area of crosslinking or achieve a Wiberg angle between 25° and 35° (Fig. 5) (the Wiberg angle to be obtained was established during preoperative planning, defining the number of millimetres to be resected). We removed redundant soft tissue and delaminated chondral fragments with a synoviotome and radiofrequency, and subsequently reinserted the labrum into the acetabular neo-edge and stabilised the labrum–cartilage joint with radiofrequency (Fig. 6).
Resection of the femoral hump was conducted without traction, seeking to recover the head–neck offset. The final step was to verify the absence of residual impingement throughout the full range of the hip under arthroscopic view.
ResultsA total of 49 hip arthroscopies were conducted at our centre between June and October 2008. Of these, 17 (16 patients) met the inclusion criteria for the study.
The preoperative arthro-MRI showed 14 cases of labral lesion (all true positives) and 3 cases with intact labrum (2 true negatives and 1 false negative). However, none of the arthro-MRI scans revealed the chondral delamination found in the arthroscopies (17 false negatives).
Regarding intraoperative findings, all the cases (17 hips) presented chondral delamination located in the anterosuperior acetabular region: 1 case in zone 3 (12:00), and 16 cases in zones 2–4 (between 9:00 and 3:00) (1 case presented a lesion extending to zone 5).
A total of 15 cases (88.2%) presented labral lesion, whilst 2 cases (11.8%) presented an intact labrum–cartilage junction.
In all the patients, the overcoverage zone correlated with the delamination area.
The mean preoperative Wiberg value was 37° (range between 32° and 47°), whilst the mean postoperative value was 29.5° (range between 25° and 34°). All the acetabular retroversions were corrected (the crosslinking signs were removed on the intraoperative radiographs). Out of the 17 patients, a total of 13 cases required osteoplasty of the femoral hump, with 4 cases of pure pincer-type FAI.
In 16 (94%) patients, resection of the acetabular overcoverage or retroversion area left a stable cartilage remnant without delamination. Only in 1 case (6%) did the delamination area extend into the load area, thus requiring microfractures. This was a mixed case, with a preoperative Wiberg value of 38° and postoperative Wiberg value of 25°.
The mean preoperative MHHS score was 77pts, with a range between 52 and 91pts.
The mean postoperative follow-up period was 6 months (range between 4 and 9 months). The mean postoperative MHHS score was 94pts, with a range between 86 and 100pts.
DiscussionDespite the absence of studies with long-term follow-up periods showing that hip impingement stops the progression of early hip osteoarthritis, there is evidence in the medium term (4.7 years) of non-progression of degenerative joint changes following FAI treatment.8
FAI treatment should not only be directed at relieving symptoms by treating their consequences, but instead, the goal of treatment should also include the correction of the anatomical causes of impingement, in other words, restoring the normal anatomy and biomechanics of the hip.
One of the great challenges of this condition is the treatment of lesions of the labrum–cartilage complex, especially chondral delamination, from a simple debridement of small focal lesions to microfractures in larger lesions.9
In pincer-type cases, acetabular drilling is the basis of treatment, either through resection or reinsertion of the labrum. Espinosa et al.10 have compared labral reintegration with resection in 52 patients with follow-up periods of 1 and 2 years, and found better clinical outcomes among patients with labral reinsertion.
Philippon et al.11 have reported the results of hip arthroscopy in FAI among 112 patients with a minimum of 2 years follow-up. The findings of the work suggested that 3 factors were associated with better postoperative outcomes (assessed through MHHS): preoperative MHSS, joint space (>2mm) and labral reinsertion.
In another study, Anderson et al.3 have studied the relationship between cam-type impingement and chondral delamination and reported finding no relationship between them. They suggested that, in theory, the linear contact of pincer-type FAI could represent a protection for chondral delamination, although this theory is currently unproven. The treatment used in that study was very similar to the one used in the present work.
In works which are currently under review for publication, and in agreement with the available literature,12,13 our group has shown that chondral delamination is a common finding in FAI, which may be underdiagnosed by arthro-MRI and other preoperative imaging studies,12–14 and that it may take place even without involvement of the labrum–cartilage junction.
In this study we found a close relationship between the most frequent region of acetabular overcoverage (anterior) and the area of acetabular chondral delamination (anterosuperior). In 94% of cases, resection of the region of acetabular overcoverage served as sufficient treatment to remove the area of chondral delamination, leaving only the stable cartilage. Only in 1 (6%) case was the delamination area more extensive than resection of bone overcoverage, thus requiring debridement of the chondral flap and microfractures.
These findings demonstrate that treating acetabular overcoverage (through high-speed drilling) would not only eliminate the pincer-type component of FAI, but also the flap of delaminated and unstable cartilage.
An important detail to consider is that our parameter to define the extent of acetabular bone resection was the elimination of the overcoverage or retroversion area under radiographic guidance, unlike the chondral delamination area. This consideration is very important since a bone resection based on the area of chondral delamination may lead to an excessive resection and a dysplastic acetabulum remnant.
ConclusionsThe area of chondral delamination is closely related to the acetabular overcoverage/retroversion area. This coincidence enables the chondral delamination area to be eliminated by treating the area of acetabular overcoverage, thus eliminating the pincer-type component of FAI and leaving a stable and firm cartilage remnant. We recommend labral reinsertion after treating overcoverage.
Level of evidenceLevel of evidence II.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Camacho-Alvarez D, Mardones-Peterman R. Pinzamiento femoroacetabular: asociación entre el área de sobrecobertura y la zona de delaminación condral acetabular. Rev Esp Cir Ortop Traumatol. 2013;57:111-6.