To compare clinical and imaging results and complications between patients treated for femoroacetabular impingement who underwent either open surgery or an arthroscopic approach.
MethodsThis retrospective study included patients who underwent femoroacetabular impingement surgical treatment between June 2009 and January 2018. Patients treated with open surgery were compared with those treated with arthroscopy. Patients were radiographically and clinically assessed by alpha angle, degree of arthritis, Harris Hip Score, hospital stay and complications, as well as progression to total hip arthroplasty.
Results57 patients with FAI were included; 27 (45.6%) underwent open surgery and 31 (54.4%) underwent arthroscopy. Statistically significant differences were observed in hospital stay, where the patients who underwent arthroscopic surgery showed better outcomes. There were no other statistically significant differences, the results were similar in both groups.
ConclusionsArthroscopy and open surgery treatments for femoroacetabular impingement provided comparable clinical and radiographic results. However, the latter surgery provides better results in surgery time, hospital stay and postoperative recovery.
Comparar clínica y radiográficamente los resultados y complicaciones del tratamiento quirúrgico del choque femoroacetabular, mediante cirugía abierta o abordaje artroscópico.
MétodosEstudio retrospectivo en el que se incluye a los pacientes intervenidos entre junio de 2009 y enero de 2018 de choque femoroacetabular mediante abordaje abierto o artroscópico. De dichos pacientes se obtuvieron datos diagnósticos, resultados pre- y postoperatorios del ángulo α, escala Tönnis, valoración clínica mediante Harris Hip Score, estancia hospitalaria y posibles complicaciones así como evolución a prótesis total de cadera.
ResultadosFueron incluidos en el estudio 57 pacientes, de los cuales 27 fueron sometidos a femoroplastia abierta (45,6%) y 31 a cirugía artroscópica de cadera (54,4%). A la hora de comparar los resultados obtenidos en cuanto corrección de ángulo α y de la puntuación del Harris Hip Score, no se obtuvieron diferencias estadísticamente significativas. Donde sí se encontraron diferencias estadísticamente significativas fue en la estancia hospitalaria, siendo aquí superior aquellas femoroplastias realizadas mediante cirugía artroscópica.
ConclusiónAmbas técnicas quirúrgicas para el tratamiento del choque femoroacetabular son válidas y obtienen resultados satisfactorios, si bien es cierto que la artroscopia está demostrando resultados superiores respecto a la cirugía abierta en el acortamiento de los tiempos quirúrgicos, estancia hospitalaria y recuperación postoperatoria.
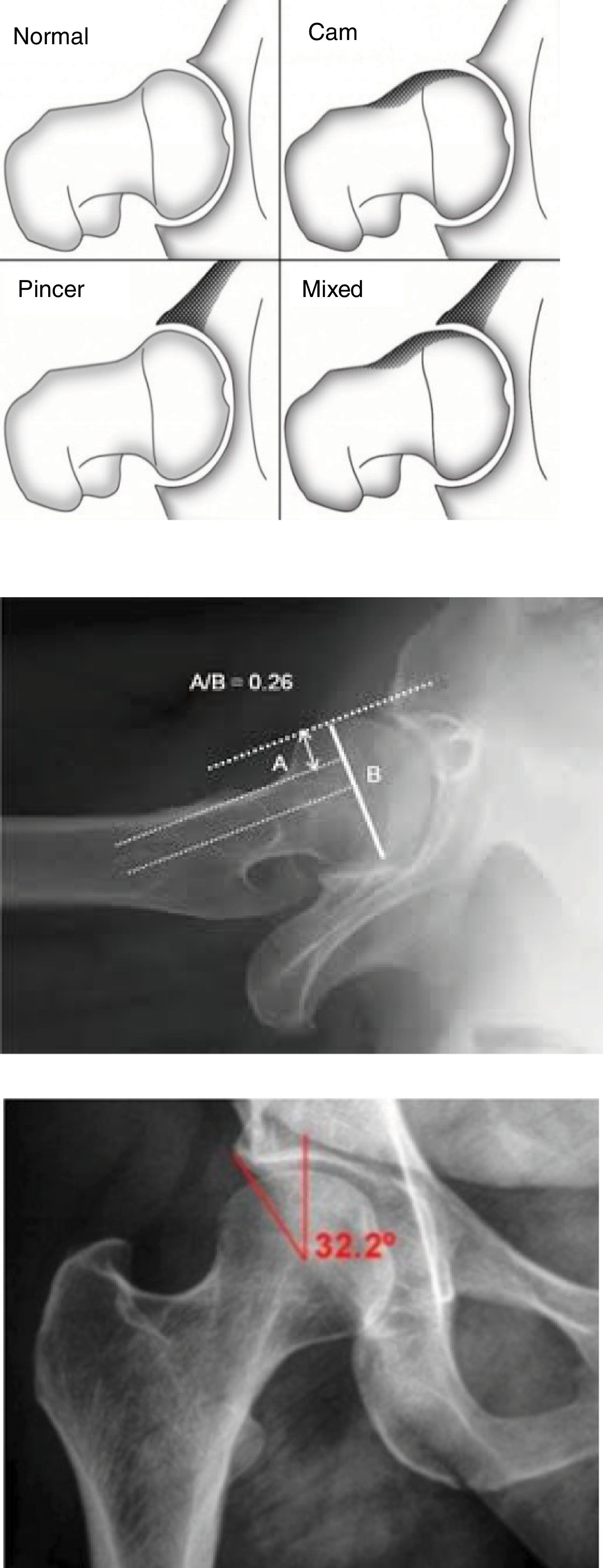
Femoroacetabular impingement or shock (FAI) is a recognised cause of coxalgia resulting from abnormal contact between the femur and the acetabulum, causing pain, limitation of movement and early osteoarthritis in the hip joint.1 Two types of impingement have been described depending on the predominant bone disorder. The cam type, due to femoral head asphericity, and the pincer type, caused by acetabular overcoverage or retroversion;2 mixed forms being the most frequent in terms of presentation (Fig. 1A). The aetiology of this syndrome is not clear, but morphological alterations of the developing femur, caused by the practice of sports or hypermobility of the hip joint, and childhood hip diseases (Legg-Calve-Perthes and subclinical epiphysiolysis) have been described as possible aetiologies.3–5
Medical history and physical examination play an important role in diagnosis, although imaging tests enable anatomical abnormalities to be identified in order to plan surgery, and the diagnosis can be confirmed by magnetic resonance imaging.
Conservative treatment is chosen initially, avoiding exercises that involve overloading and mechanical conflict of the hip. It is also often necessary to combine with anti-inflammatory drugs. If this conservative treatment is not effective and provided that the patient does not have evolved joint damage, correction of the bone deformity by surgical treatment would be indicated.6 Both the open femoroplasty approach and arthroscopic hip surgery (AHS) have shown clinically satisfactory results with similar levels of correction, although there appears to be a trend in favour of arthroscopic surgery due to the lower surgery times and hospital stay.7,8
Among the multiple options for open surgical treatment are Ganz's safe dislocation, periacetabular osteotomies and the direct anterior femoral approach.
Historically, AHS was used for chondral and labral injuries until 2006 when Philippon et al. first reported using this technique to correct the bone deformities that correspond to this type of impingement.
As in the published literature, we have gained experience using both open and arthroscopic techniques in our centre as we have expanded our knowledge of anatomy and pathology. Therefore, the aim of our study was to evaluate and compare the clinical and radiographic outcomes obtained with both techniques.
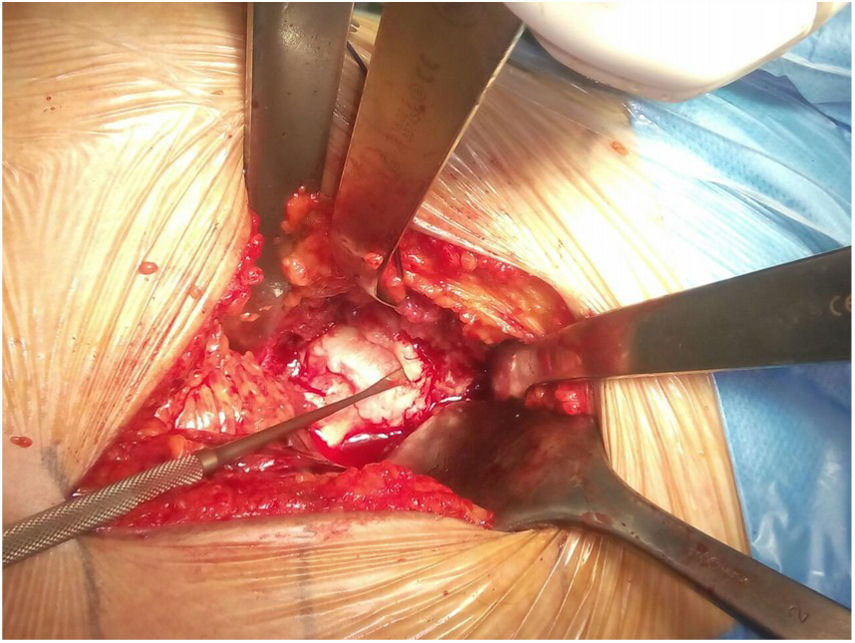
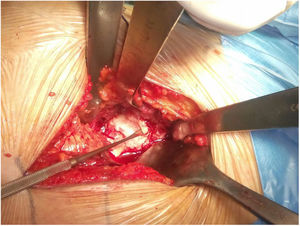
Material and methodsSurgical techniquesThe open surgery technique chosen is the direct anterior femoral approach. Initially described by Ribas et al. with the aim of avoiding damage to the trochanteric mass or the abductor mechanism, it uses an iliofemoral approach to reach the capsule between the sartorius muscle and the tensor fasciae latae, and thus the appropriate osteochondroplasty can be performed.
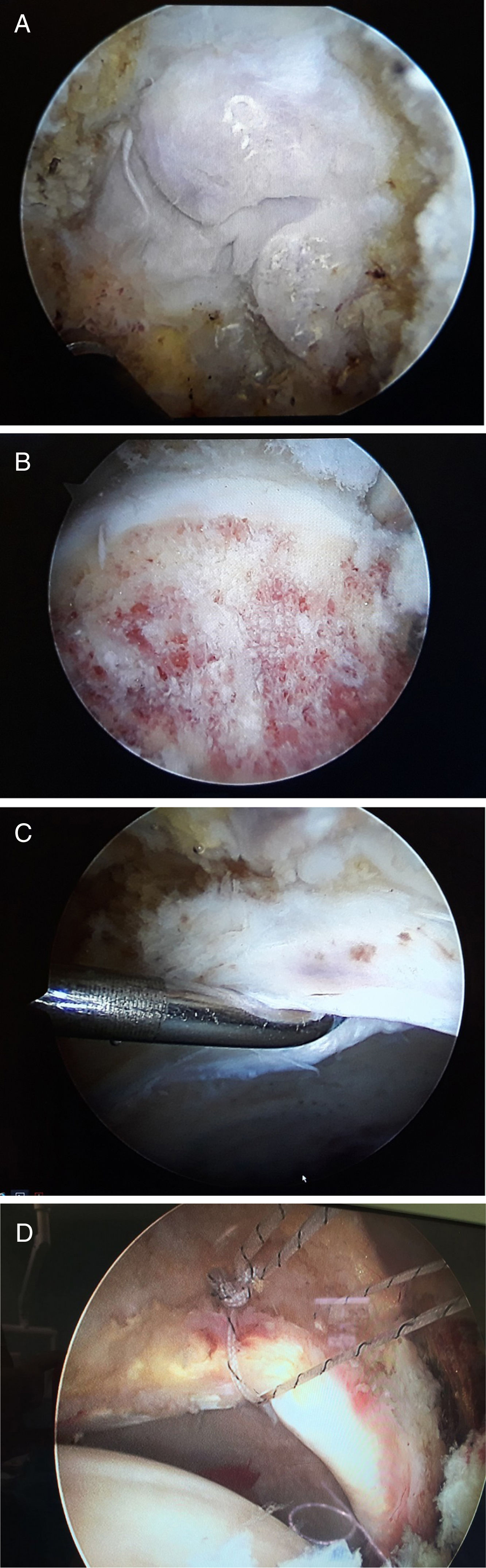
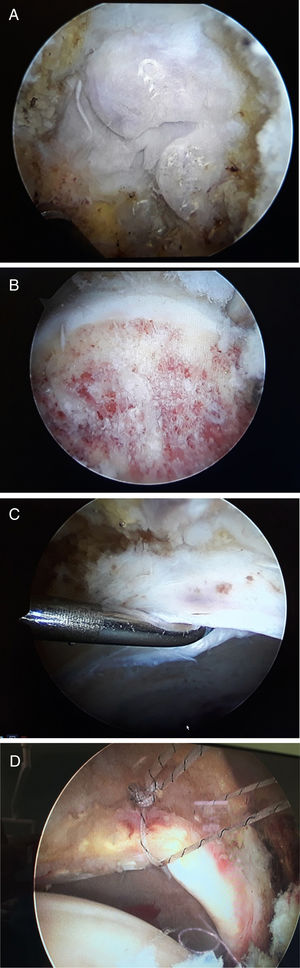
With regard to the arthroscopic technique, multiple patient positioning options and portals can be used to access the central and peripheral compartments. In our case, we place the patient in a supine position on the traction table. The anterolateral and anterior portals are used to assess the central compartment. Once systematic exploration and precise treatment has been carried out (labral lesions, pincer type lesion and chondral lesion) we reach the peripheral compartment where we will check 7 areas: the anterior, middle and lateral area of the femoral head, and the anterior, middle and lateral area of the femoral neck, plus the posterior area, paying special attention to the transition area between head and neck where the osteophytes that give rise to the cam type lesion develop. A generous resection is performed, until it is verified that the convex area becomes a concave and regular surface, and conflict with the acetabular rim disappears.
PatientsFor analysis of the results of the AHS, patients undergoing both open and arthroscopic surgery were reviewed retrospectively, resulting in an observational, comparative and retrospective study.
All the patients were operated by the entire team of the Arthroplasty Unit of the Miguel de Servet University Hospital between June 2009 and January 2018. Each patient underwent a particular surgical intervention according to when they had entered the waiting list. Therefore, patients who entered on even days would undergo the open approach while those who entered on odd days would undergo the arthroscopic technique. During this period, a sample of 53 patients was obtained, to which the following exclusion criteria were applied: age over 55 years, degree of advanced osteoarthritis (Tönnis greater or equal to 3), follow-up of less than 6 months or loss to follow-up.
After applying the exclusion criteria, a final sample of 47 patients was obtained, which was divided into patients undergoing open surgery (group A) and those undergoing arthroscopic surgery (group B).
Group A (open surgery by direct anterior iliofemoral approach) included 26 patients, of which 20 were male (76.9%) and 6 female (23.1%) with a mean age of 37.96 years (SD=7.09 and an age range of 22–50 years). Laterality was left in 16 cases (61.5%) and right in 10 (38.5%).
On the other hand, there were 31 patients in group B, 19 males (61.3%) and 12 females (38.7%) with a mean age of 41.23 years (SD=11.56 and an age range of 19–57 years). Laterality was left in 15 cases (48.4%) and right in 16 (51.6%).
All the patients were assessed prior to the intervention with an interview in which the Harris Hip Score was assessed (excellent 70–80 points, good 60–69 points, fair 50–59 points and poor 49 points or less) and degree of internal rotation.
By means of radiography (anteroposterior projection of the pelvis with both hips and Dunn projection at 45° and 90°) and magnetic resonance imaging, it was possible to evaluate the angle, Tönnis scale score9 and possible associated lesions in the labrum. From a clinical point of view, we analysed the difference in mean hospital stay according to the approach route and complications in both groups.
The AHS was considered cam type if the angle was greater than 50° on the Dunn view at 45° (Fig. 1B) and pincer type if the Wiberg angle was equal to or greater than 40° (Fig. 1C) on the anteroposterior projection.10
All the tests were evaluated by 2 members of the team in order to avoid errors in the measurement of the indicated parameters.
Statistical analysisFor the statistical analysis, the Student's t-test with Pearson's correlation was used. Once the equality of variances was tested with Levene's test, the significance level was established at a p value of less than .5.
ResultsBoth groups were considered homogeneous based on the preoperative statistical analysis.
The diagnoses in the group operated by open hip surgery (Fig. 2) were: 16 cam (61.5%), one pincer (3.8%), 7 cam+labrum (26.9%), one labrum (3.8%), one cam+pincer (3.8%).
On the preoperative X-ray, 9 cases had osteoarthritis classified as Tönnis grade 0 (34.6%), 16 patients had a Tönnis grade 1 (61.5%) and one patient a Tönnis grade 2 (.38%). There were no cases classified as Tönnis grade 3 or 4; these grades are supposed to contraindicate hip preservation surgery.
With regard to the preoperative angle, a mean of 67.08° was observed (SD=5.68, range 57–78). After surgical treatment, a reduction in the angle was achieved, reaching a mean value of 47.7° (SD=2.9; 42°–53°).
The Harris Hip Score showed a preoperative mean of 59.27 points (SD=10.65), with an improvement with a postoperative mean of 69.95 (SD=14.34).
The mean hospital stay of the patients who underwent open femoroplasty was 2.65 days (SD=1.231).
In this group, the complications observed were one case of infection and another of avascular necrosis of the head of femur, assuming 7.69% between the two. A need for conversion to total hip arthroplasty was observed in 3 patients (11.5%). This conversion was carried at 10 months following the open femoroplasty in the first patient, at 47 months in the second and at 14 months in the third patient.
In the group who underwent AHS (Fig. 3), the diagnoses were: 9 cam (29%), 0 pincer, 7 cam+labrum (22.6%), 15 labrum (48.4%), 0 cam+pincer.
In the 22 patients in whom labral tear was found, isolated debridement was performed as a repair in 5 cases (22.73%) and in the remaining 17 (77.27%) anchors were combined with debridement.
With regard to the radiographic Tönnis scale findings, 7 patients were classified as grade 0 Tönnis (22.6%), 13 patients were grade 1 (41.9%), and 11 patients finally obtained a grade 2 Tönnis (35.5%).
The mean preoperative α angle was 64.1° (SD=7.20). After AHS, a reduction in the α angle was obtained, achieving a mean 52.5° (SD=6.76).
The preoperative Harris Hip Score was a mean of 60.6 (SD=11.2). The arthroscopic surgery achieved an improvement, obtaining a mean postoperative score of 70 (SD=10.10).
The mean hospital stay of the patients undergoing arthroscopic surgery was 1.32 days (SD=.59).
Finally, in this group no complications such as avascular necrosis of femoral head, femoral neck fracture or infection were found throughout the follow-up period. On the other hand, conversion to total hip arthroplasty was necessary in 3 patients, with the time periods from arthroscopic surgery to replacement being 23, 15 and 9 months in each of the patients.
Comparative analysis of the results obtained in the groups treated by either open or arthroscopic surgery shows equivalence of the results with both techniques.
The preoperative Harris Hip score was a mean 59.27 (SD=10.65) in the group treated with open surgery and 60.69 (SD=11.23) in the group who underwent AHS (p=.650). The same applies to the postoperative values, which were 69.95 (SD=14.34) in the group treated with open surgery and 70 (SD=10.1) in the group who underwent AHS, (p=.990), which indicates similar clinical improvement with both open and arthroscopic surgery for FAI.
With regard to the pre- and post-operative α angle, the values obtained in the group treated with open surgery were 67.08 (SD=5.68; p=.098) and 47.77 (SD=2.93; p=.02) compared to 64.1 (SD=7.2; p=.098) and 52.52 (SD=6.76; p=.02) in the group treated with AHS, demonstrating a statistically significant greater reduction in α angle with the use of open surgery compared to arthroscopic surgery.
Finally, on attempting to evaluate significant differences between hospital stays according to the type of treatment, not assuming equal variances in the Student's t-test, a bilateral significance was found with p=.000.
DiscussionFAI is the most common indication for hip-sparing surgery. Thorough physical examination and radiographic assessment is fundamental to establish the surgical indications that will benefit with favourable outcomes. Both open and arthroscopic surgery have shown excellent results in the treatment of symptomatic FAI, but there is no evidence of the efficacy of conservative treatment.
The current literature advocates surgical treatment of symptomatic FAI to relieve pain and improve function in active patients without advanced osteoarthritis but does not support prophylactic surgery in asymptomatic individuals in order to prevent degenerative changes of the hip.1,4,11
Historically, the open techniques used for the treatment of this type of condition are Ganz's safe dislocation, periacetabular osteotomies and the direct anterior femoral approach. Ganz's safe dislocation advocates a lateral Gibson approach, followed by a trochanteric osteotomy and an anterior capsulotomy, in order to perform an anterior dislocation without damaging the anterior circumflex femoral artery. Thus, we preserve the vascularisation of the femoral head. For periacetabular osteotomies, a Smith–Petersen approach is used in case the FAI is due to pure retroversion of the acetabulum or combined with another injury. Finally, direct anterior femoral access through an iliofemoral approach allows us to access the anterior capsule between the sartorius muscle and the tensor fasciae latae, and thus perform the necessary osteotomies.12
Despite the advances in arthroscopic surgery, some authors continue to argue that Ganz's open approach is considered the gold standard of treatment for combined or mixed FAI.13,14 In contrast, the open techniques present a greater number of complications: femorocutaneous nerve injury with the anterior approach; femoral osteonecrosis, heterotopic ossification, trochanteric pseudoarthrosis or femoral neck fracture with Ganz's open approach or excessive acetabular anteversion and subsequent acetabular impingement in the case of overcorrection in periacetabular osteotomy techniques.11 In our series we did not observe any of the above-mentioned complications.
Although no results of the long-term impact of the surgery are available, current results indicate that surgical dislocation of the hip as well as acetabular osteoplasty are successful in relieving the symptoms of FAI in most patients.11
Arthroscopic surgery performed by experienced surgeons has demonstrated clinical outcomes equivalent to open surgery but with a lower rate of major complications, better functionality and a return to sports activity rate of about 92%. The results are less favourable when there are other underlying conditions including degenerative osteoarthritis, acetabular dysplasia, extra-articular impingement, significant coxa valga, deep coxa and protrusion, age over 45 years and long-standing symptoms.14
Nwachukwu et al. performed a systematic review of the outcomes published thus far that included medium and long-term outcomes of these interventions, with a minimum follow-up of 3 and 8 years respectively. They found that after open surgery there was a non-significant increase in survival of the coxofemoral joint compared to arthroscopic surgery.15
Along the same lines,16 they highlighted age and previous osteoarthritis as predisposing factors for progression to replacement arthroplasty, as well as poor outcomes following arthroscopic surgery to treat FAI, if these factors are present.
The main risks of hip arthroscopy are femoral neck fracture; pudendal nerve injury; sciatic nerve injury; compartment syndrome of the leg, subsequent hip instability; avascular necrosis of the femoral head and septic arthritis. Minor complications include labral injury, femoral cutaneous nerve neuroapraxia, iatrogenic chondral injury, heterotopic ossification, transient numbness in the foot from traction boots and persistent pain from degenerative arthritis. A recent review of 6962 hip arthroscopies reported a major complication rate of .58% and a minor complication rate of 7.5%.4,11,15 None of the 31 patients undergoing AHS in our study presented complications. By contrast, in the open surgery group we found a complication rate of 7.69% (one case of infection and one case of avascular necrosis of the femoral head).
Although treatment of FAI may improve hip joint function, patient satisfaction is not always positive. Recent studies have reliably demonstrated improvement in hip kinematics (flexion, internal rotation and range of motion) and mean α angle (from 59.8 to 36.4) after surgical correction, which correlated with a significant improvement in mean Harris Hip Score from 65.86±6.66 to 89.1±13.02.6,15
In our series, both patient groups showed an improved Harris Hip Score with results of 69.95 in the open surgery group and 70 in the AHS group without finding significant differences between the two groups.
With regard to the mean α angle, the pre- and post-operative values obtained in the group undergoing open surgery are 67.08 and 47.77 compared to 64.1 and 52.52 in the group treated with AHS, demonstrating a greater α angle reduction with the use of open surgery compared to arthroscopic surgery that is statistically significant.
One of the clear advantages of arthroscopic treatment is the decrease in surgical aggressiveness, which leads to an improvement in patient pain and a shorter hospital stay. In our series we corroborated this reduction in hospital stay with statistically significant results, with a mean 1.32 days of hospitalisation in the patients treated by AHS and 2.62 days in the patients who underwent open surgery (p=.000).15
ConclusionBoth surgical techniques for the treatment of FAI are valid and achieve satisfactory results, although arthroscopy is certainly demonstrating superior results with respect to open surgery in shortening surgical times, hospital stay and post-operative recovery. Studies with large series comparing both groups with longer follow-up times are needed to better understand the evolution of both techniques and to determine guidelines when choosing how to approach this condition.
Level of evidenceLevel of evidence III.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank the arthroplasty team for their constant help and training, both on a personal and a professional level.
Please cite this article as: Campoamor González M, Martínez Aznar C, Martín Martínez A, Martín Hernández C, Mateo Agudo JJ, Panisello Sebastiá JJ. Comparación del abordaje abierto frente al artroscópico en el tratamiento del choque femoroacetabular Abordaje abierto frente al artroscópico como tratamiento para el CFA. Rev Esp Cir Ortop Traumatol. 2020;64:185–190.