Low-back pain remains a common pathological entity in the Western population. We have found no data in the literature that assess whether, with correct physical examination and evaluation of simple X-rays of the spine, it is possible to diagnose patients who are highly likely to be candidates for lumbar spine surgery and thus reduce the care burden and resource consumption that this disorder entails.
The aim of the study was to develop a user-friendly calculator that allows only patients who are strong candidates for surgical treatment to be referred for spinal surgery consultation.
Material and methodsAn observational and retrospective study that included all adult patients from the healthcare area of Talavera de la Reina (Toledo, Spain) with a clinical and/or radiological diagnosis of degenerative lumbar spine disease referred by other specialists over one calendar year to the spinal surgery unit to assess whether surgery was indicated after unsuccessful conservative treatment. All the patients were assessed under the same protocol with a follow-up of 6years, at the end of which we performed a check of those who had undergone lumber spine surgery.
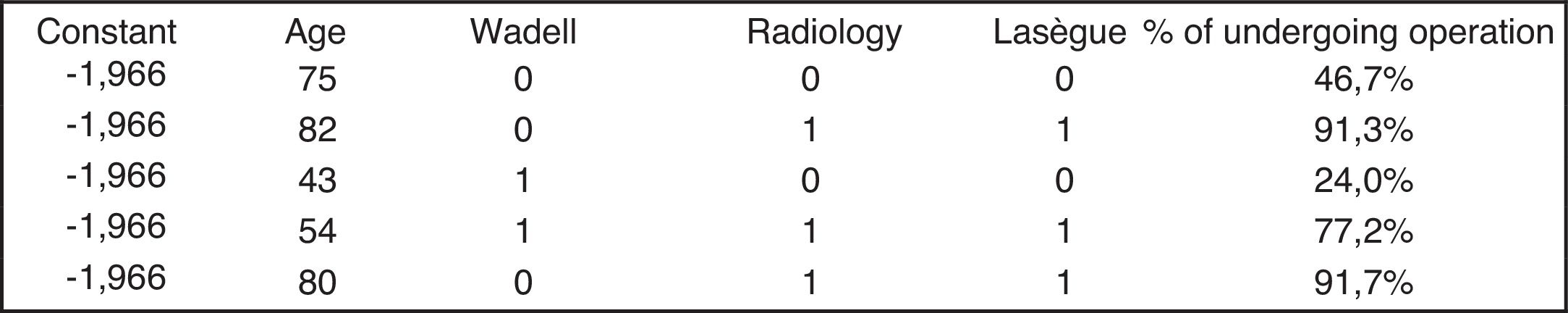
ResultsA total of 201 patients were studied and at the end of the 6-year follow-up, a total of 77 patients had been operated. Concordance of 70% was found between the indication for surgical treatment and the treatment received at the end of the follow-up. Therefore a logistic regression was performed in an attempt to predict the patients that could be referred to the spinal surgery units and from that a calculator was generated, which included the plain X-ray variable as an essential item, and which showed as statistically significant (p<.05): age, Waddell's non-organic signs, Lasegue's sign and plain X-ray assessment. Once this tool had been obtained, the likelihood of undergoing surgery was calculated for all patients who were proposed surgical treatment, obtaining results above 62% as the cut-off point when using the calculator.
ConclusionsThe use of the calculator predicts the possibility of being a candidate for surgical treatment with 70% reliability. Therefore, patients with a result in the calculator of above 62% should be referred for spinal surgery consultation for assessment by a specialist.
Hoy por hoy el dolor lumbar sigue constituyendo una entidad patológica de alta incidencia en la población occidental. No hemos encontrado en la literatura datos que evalúen si con una exploración física correcta y una valoración de las radiologías simples de la columna vertebral se puede diagnosticar a los pacientes con una alta probabilidad de ser candidatos a cirugía de columna lumbar, disminuyendo así la carga asistencial y el consumo de recursos que esta patología supone.
El objetivo del estudio es desarrollar una calculadora de fácil manejo que permita derivar a las consultas de Cirugía del Raquis solo a los pacientes con elevada probabilidad de recibir tratamiento quirúrgico.
Materiales y métodosEstudio observacional y retrospectivo que incluyó a todos los pacientes mayores de edad del Área Sanitaria de Talavera de la Reina (Toledo) con diagnóstico clínico y/o radiológico de patología lumbar degenerativa derivados, por otros especialistas durante un año natural, a la unidad de Cirugía de Columna para valorar la indicación de cirugía tras tratamiento conservador infructuoso. Todos los pacientes fueron evaluados bajo un mismo protocolo con un seguimiento de 6años, al final de los cuales se controló quiénes fueron intervenidos sobre la columna lumbar.
ResultadosSe estudiaron un total de 201 pacientes, y al final de los 6años de seguimiento se intervinieron un total de 77 pacientes. Se encontró una concordancia del 70% entre la indicación de tratamiento quirúrgico y el tratamiento recibido al final del seguimiento, por lo que se realizó una regresión logística tratando de hacer una predicción de los pacientes que se pueden derivar a las unidades de Cirugía del Raquis, y a partir de ahí se generó una calculadora, que incluía la variable radiología simple como ítem imprescindible, y que mostró como estadísticamente significativo (p<0,05): la edad, los signos de no organicidad de Waddell, el signo de Lassegue y la valoración de la radiología simple. A partir de la obtención de esta herramienta, se realizó el cálculo de probabilidad de ser intervenido a todos los pacientes a los que se propuso tratamiento quirúrgico, obteniéndose como punto de corte, al emplear la calculadora, unos resultados por encima del 62%.
ConclusionesEl empleo de la calculadora diseñada predice la posibilidad de ser candidato a tratamiento quirúrgico con un 70% de fiabilidad, así que los pacientes con un resultado en la calculadora superior al 62% deben ser derivados a consultas de Cirugía del Raquis para valoración por un especialista.
Non-specific chronic low back pain (NSLBP) remains a highly prevalent pathological entity in the Western population. Although the majority of episodes of low back pain are limited and have a good prognosis with conservative treatment (analgesia, injections, physiotherapy and rehabilitation, etc.), it has been estimated that between 44% and 78% will present with increasingly more intense and long-lasting relapses and episodes.1,2
Several authors calculate that 95% of patients who go to the primary care services with low back pain will present with a NSLBP.3 Of the remaining 5% (who will present with a pathology which requires more complex diagnostic methods for possible treatment), 4% will correspond to a disease which may be called organic (herniated disc or stenosis), and 1% with a systemic disease (tumour or infection). It is this group of the previously mentioned 5% which will present with a non-specific cause of pain and correspond to those patients who will become candidates for surgical treatment.4
Despite the advances in the diagnosis of the different possible aetiologies, the percentage of patients referred to spinal surgery specialists continues to be tremendously high.
We did not find any protocol in the literature which would enable us to standardise the patients who were candidates for surgical treatment based on accurate physical examination and an evaluation of plain X-rays of the spine.
The aim of this study was to develop a user-friendly calculator that allows only patients who are strong candidates for surgical treatment to be referred to spinal surgery consultation, thus allowing for rationalisation of resources and a reduction of the care burden which this disorder entails.
Material and methodsThis was an observational and retrospective study. The sample was random, simple and consecutive. Data analysis was performed using the SPSS 15.0 and Epidat 3.0 statistical programmes.
To calculate sample size, as a result of not knowing the prevalence of the clinical characteristics and patient profile, nor probability of surgery, the maximum degree of uncertainty which was a prevalence of 50% was considered. Taking a precision of 5%, with a confidence level of 95% (p<.05), a minimal sample size of 198 patients was obtained.
All patients of legal age were included from the health area of Talavera de la Reina (Toledo) with a clinical and/or radiological diagnosis of degenerative lumbar spine disease referred by hospital specialists (trauma specialists, rheumatologists, neurologists, physiotherapists, etc.), for one natural year, to the spinal surgery unit to assess whether surgery was indicated after unsuccessful conservative treatment (pharmacological, rehabilitation and injections by the pain unit) for an approximate period of 6 months. Patients with low back pain of non-degenerative origin (trauma, tumour, metabolic, etc.) were excluded from the study.
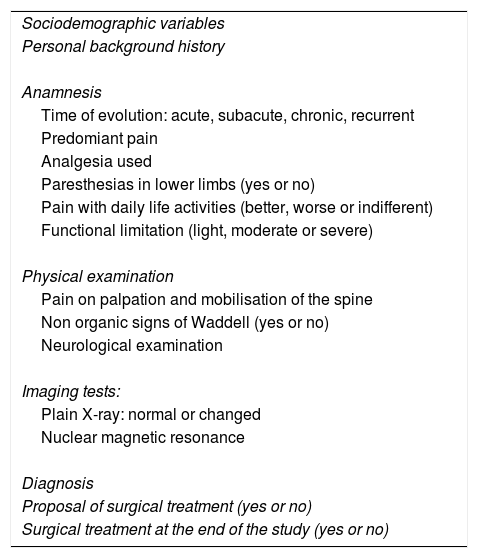
All patients were assessed in the outpatients departments under the same protocol (Table 1) and by a single observer, with a follow-up of 6 years, after which those who were operated on in the lower back were controlled, both in the hospital of reference and in other centres.
Protocol used in outpatient departments.
| Sociodemographic variables |
| Personal background history |
| Anamnesis |
| Time of evolution: acute, subacute, chronic, recurrent |
| Predomiant pain |
| Analgesia used |
| Paresthesias in lower limbs (yes or no) |
| Pain with daily life activities (better, worse or indifferent) |
| Functional limitation (light, moderate or severe) |
| Physical examination |
| Pain on palpation and mobilisation of the spine |
| Non organic signs of Waddell (yes or no) |
| Neurological examination |
| Imaging tests: |
| Plain X-ray: normal or changed |
| Nuclear magnetic resonance |
| Diagnosis |
| Proposal of surgical treatment (yes or no) |
| Surgical treatment at the end of the study (yes or no) |
This study was carried out with the consent from patients and a favourable report from the Ethics Committee of Clinical Research in the Area of Integrated health Management of Talavera de la Reina.
Since the aim of the study was to obtain a user-friendly calculator for the different specialists and above all, for primary care physicians, they decided to reduce the visible changes in plain X-rays into 2 groups: normal and pathological (this included pinched discs, facet joint osteoarthritis degenerative scoliosis, isthmic and degenerative listhesis).
ResultsA total of 201 patients (51.7% men and 48.3% women) were studied, with a mean age of 51 years (SD: 15).
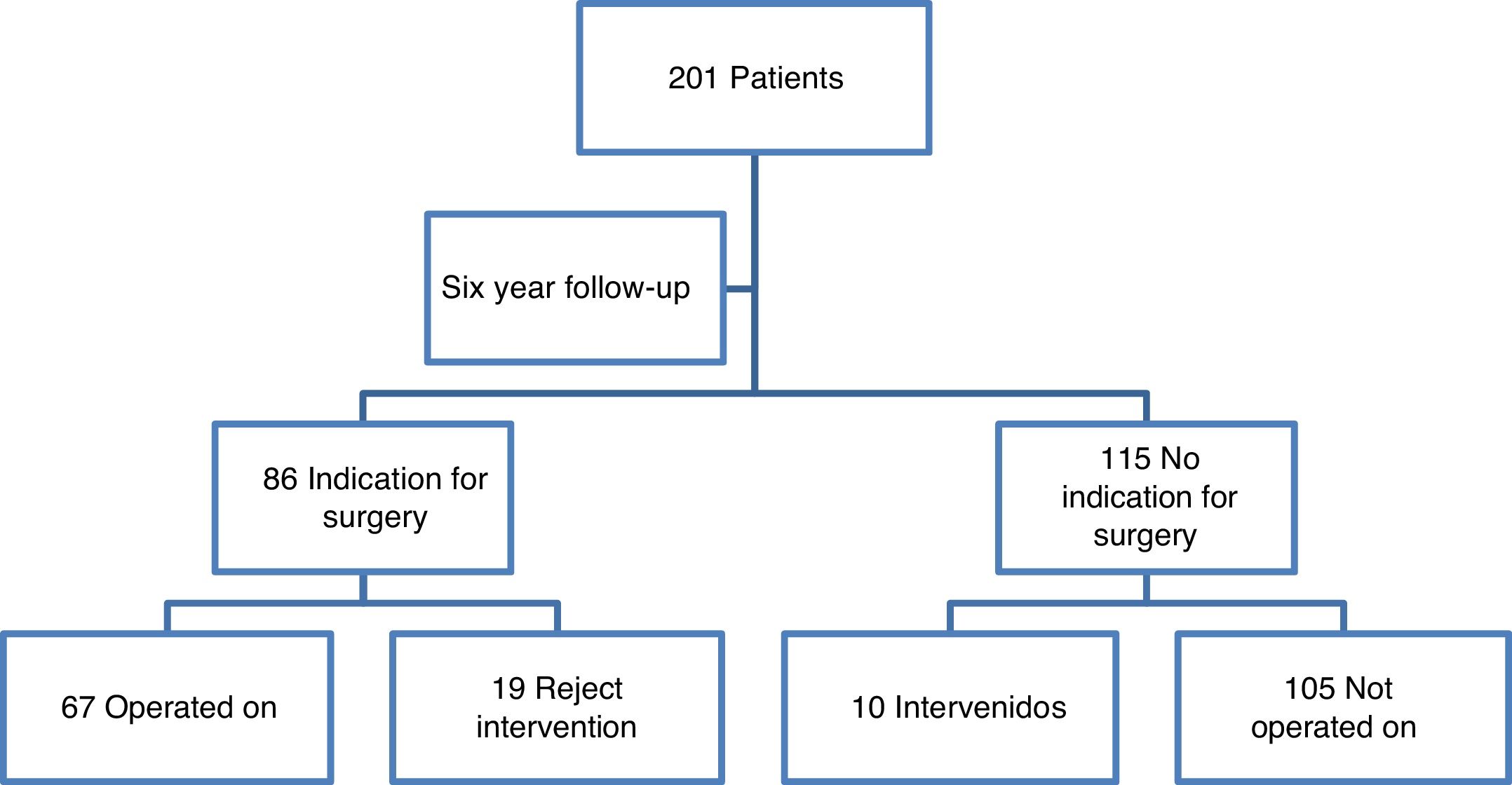
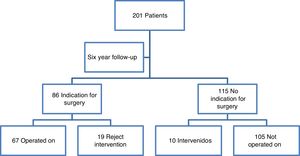
Protocol items were crossed over with the proposal or non-proposal of surgical treatment and surgical intervention was proposed in 86 patients according to observer criteria (67 accepted treatments). At the end of the 6 year follow-up a total of 77 patients were operated on (10 of them in other hospitals) (Fig. 1).
No statistically significant differences were observed regarding sex (40 men compared to 37 women), personal histories (with a tendency to operate more on those patients who were not smokers or obese), and those who had no previous history of surgery on the spine.
Ninety one percent (p>.05) of patients who were operated on presented with a history of chronic or recurrent low back pain (acute pain with asymptomatic periods of 3 months during a period over 3 years) with pain being predominantly low back in 29 cases, radicular in 16 cases, lumbar-sciatica in 8 cases and neurogenic claudication type when walking in 24 cases (p<.05).
Seventy eight point one percent of patients who were operated on were taking minimum analgesics of the second WHO scale, combining this treatment in 18.2% of cases with neuromodulator drugs, such as pregabalin, and finding statistically significant differences to the group of patients who had not been operated on (p<.05).
A total of 68 patients out of the 77 who underwent surgery presented with moderate or severe functional limitation for carrying out basic daily life activities (p<.05), with a worsening of symptoms when walking (p<.05), when moving from sitting to a standing position (p<.05), at rest (p>.05) and when recumbent (p>.05).
Ninety four point eight percent of patients who were operated on at the end of the study did not present with Waddell's non-organic signs (p<.05), and there was altered neurological examination in 28 of cases (p>.05), with the positive Lasègue sign being the most frequently observed sign (85.7% of cases).
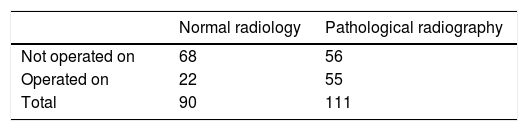
Regarding imaging tests performed during the study (Table 2), 55 patients who had been operated on presented with some kind of change in the plain X-ray of the lumbar spine, with facet joint osteoarthritis and pinched disc being the most observed changes in up to 42.9% of cases (p<.05).
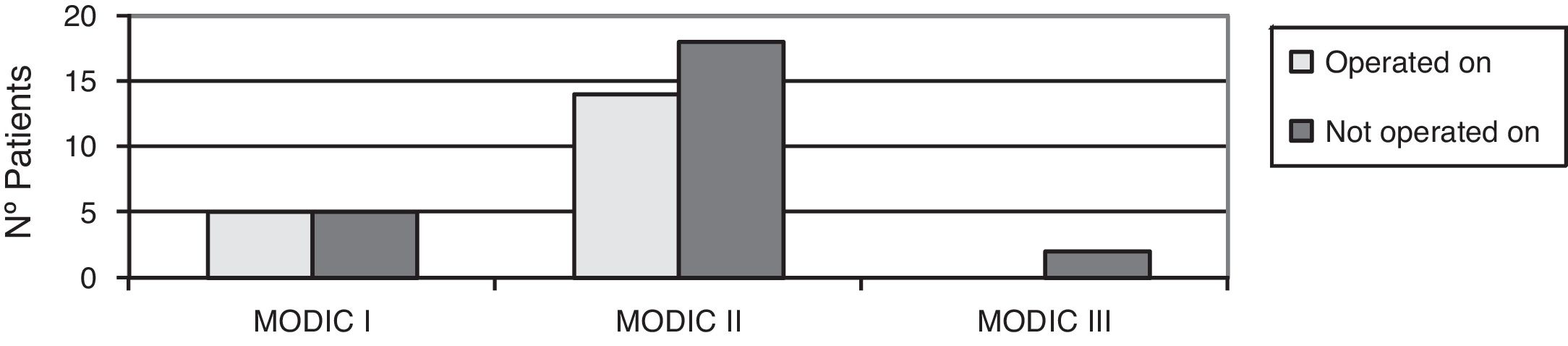
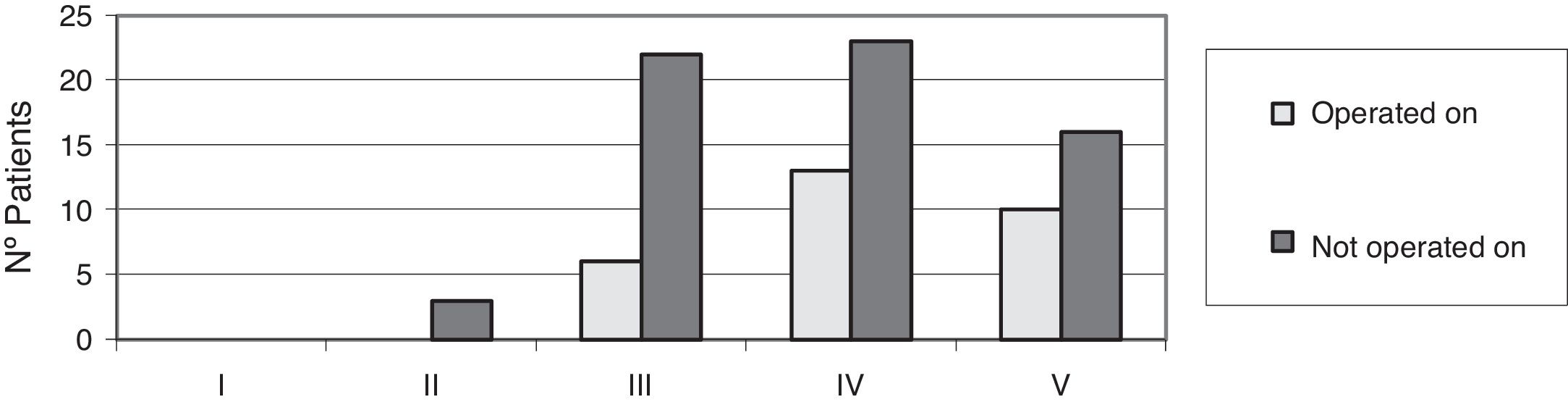
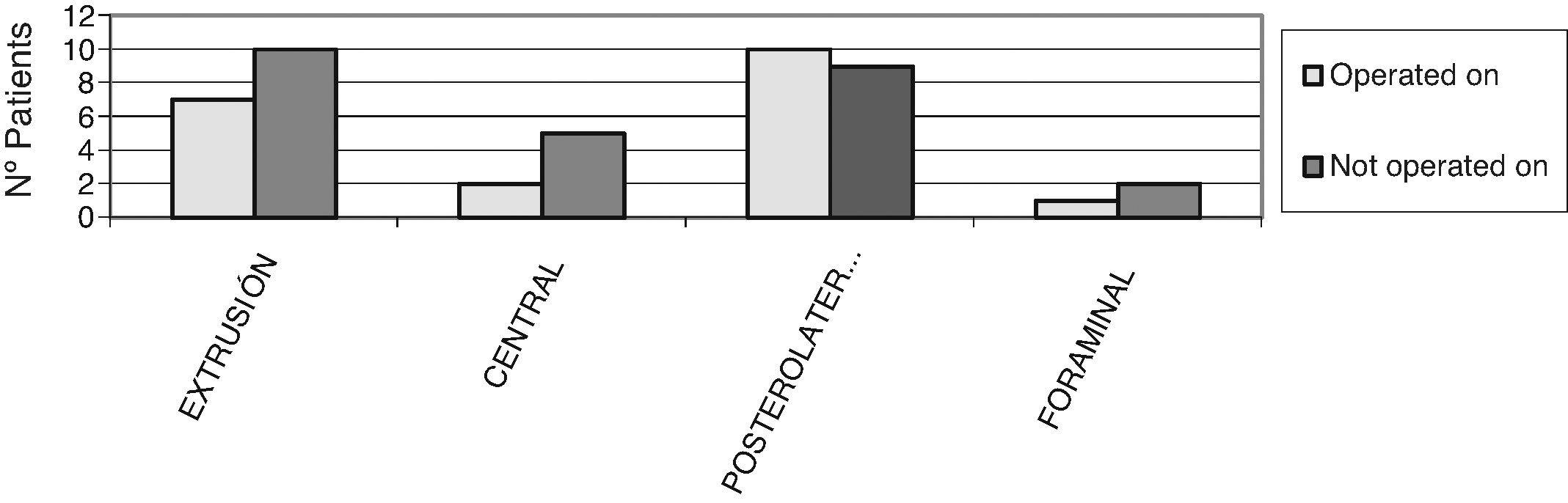
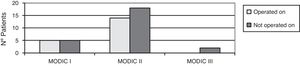
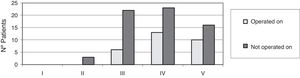
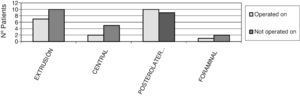
No patient was operated on who had not presented with changes in magnetic resonance tests, with degenerative disc disease (DDD) grade IV and V of DDD according to Pfirmann,5 Modic type II,6 changes, with posterolateral disc hernia and canal stenosis (p<.05) being the most frequent diagnoses (Figs. 2–4).
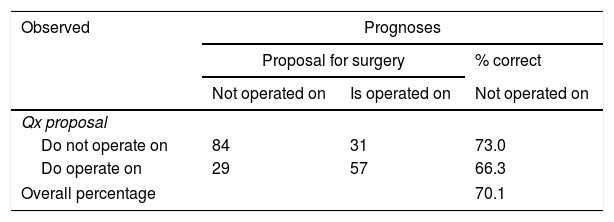
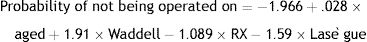
With all the protocol data analysed we assessed if there was any concordance between referral for surgical treatment by our observer and the treatment received at the end of follow-up, obtaining a 70% degree of concordance as a result. Logistic regression was then incorporated into the plain X-ray variable (normal or pathological) as a necessary item for the development of the calculator, as this was a test which could be requested by any specialist, obtaining them as variables which were of the greatest influence when surgical treatment was suggested (Fig. 5):
- •
Age: in years.
- •
The Waddell non organic signs:
- a)
Negative=0.
- b)
Positive=1.
- a)
- •
The Lasègue sign:
- a)
Normal=0.
- b)
Pathological=1.
- a)
- •
Assessment of plain X-ray:
- a)
Normal=0.
- b)
Pathological=1.
- a)
Assessment of the regression model adjustment revealed that 70.1% of cases had been currently classified (Table 3) and that all the variables studied, both constant (operation or no operation) and variables that were not in the equation, were statistically significant (p<.05).
The logistic regression equation was constructed, which in our centre was reflected as follows:
Once the equation had been obtained, and in order to facilitate calculation of the probability of being operated on, a user-friendly calculator was designed in which only age and values of 0 and 1 in the different variables were inserted, to obtain the probability of being operated on (Fig. 5).
To establish a value to determine which patients were to be referred for consultation in the spine unit the calculator was used with those patients who were candidates for surgical treatment and who were operated on at the end of the study (a total of 77 patients), obtaining a result above 62%.
DiscussionThis study sought to develop an objective tool which could lead to the rationalisation of healthcare resources, and has traced lines of research on the importance of carrying out accurate anamnesis and physical examination associated with an initial assessment of the possible visible changes in plain X-ray of the lumbar spine. As a result it is particularly useful in primary care.
No treatment has been shown to have significant and constant benefits in non-specific low back pain,7 and indication for surgical treatment is therefore reserved for selected patients where the combination of clinical and radiological tests was appropriate. Our study maintains this premise, since 100% of patients to whom surgical treatment was proposed presented with specific low back pain with neurological involvement in physical examination in 36.4% of cases (p<.05).
On consideration of all of the above, it seems clear to accept, as stated by Chou et al.,8 that surgical treatment in the case of NSLBP should be reserved for those patients who present with major functional limitation and who have not responded satisfactorily to conservative treatment for an approximate period of 6 months. This was confirmed by data obtained in our study, where at the end of the same 88.31% of patients who were operated on presented with moderate or severe functional limitations for their daily life (p<.05), with worsening of symptoms with physical activity (83.1% pain on walking, 72.7% on changing from a sitting to a standing position) and with rest (p>.05).
Equally important as anamnesis is the performing of an accurate physical examination which in many cases and based on the examiner's experience may guide us to possible diagnosis. The problem, as stated by Muñoyerro and Castell9 is that both inspection and mobility and palpation are based on subjective data (pain) and have a relative value, since they depend on the age of the patient and on the involvement of other joints, which means that exploratory findings are low in reproducibility. In keeping with the data obtained at the end of our study, patients who underwent surgery did not present with pain on palpation in 35% of cases (p<.05). This may be explained because most of them had pathologies related to radiculer compromise or claudication on walking and presented with a worsening in pain with movement of the spine and/or ambulation and in particular with flexion (62.35%).
In accordance with that reported by Dagenais et al.10 in 2010 regarding neurological examination, the latter should also be performed systematically, and include Lasègue's sign and strength assessment, reflexes and nerve root sensitivity of L4, L5 and S1. In our case, at the end of the study 64% of patients presented with a normal neurological examination. Although this result could be considered high, we should recall that a negative test does not rule out nerve compromise, and as the age of the patient increases, the proportion of positive results falls.11 Of the patients who were operated on, 37% presented with changed neurological examination, with Lasègue's sign and hypoesthesia in the L5 or S1 region being the most common pathological data (p<.05). No statistically significant differences were observed regarding the loss of strength, alteration of osteotendinous reflexes or sensitivity in lower limbs.
It is essential to stress the importance which Wadell's non-organic signs12 have acquired. In our study this became an essential variable, since with their presence, the rate of success in surgery13 dropped and this was considered a negative factor when considering surgical treatment for these patients, despite the fact that in the written literature its assessment is not commonly referred to.
With regard to assessment of plain X-rays, the indications given by the North American Agency for Health Care Policy and Research are generally accepted. According to these, there is no need to perform plain x-rays in the case of acute low back pain where there are no warning signs or for symptoms which have been present for under 4weeks because, as published by Magora and Schwartz14 regarding visible changes in plain X-rays, there may be degenerative changes in asymptomatic patients. At the end of our study 45.16% of the patients who had not undergone surgery presented with some type of radiologic change, a pinched disc and facet joint osteoarthritis being the most common (p<.05). This implied that, despite visible changes in imaging tests, only patients with good clinical and radiological correlation should be operated on, since there are many asymptomatic patients who present with visible changes in plain X-rays.
Even so, with our study we have demonstrated that, in the case of low back pains lasting over 4–6weeks, plain X-rays may provide much information. Also 71.43% of patients who underwent surgical treatment presented with some type of radiologic change (p<.05), with the most frequent pathological events being, like those of non-operated patients, pinched disc and facet joint osteoarthritis.
In our study out of the 201 patients, 30 presented with pinched discs. The fact that this entity was one of the most common findings in the X-rays of patients who had undergone intervention may be explained by the clinical significance which this entity represents, since after finding this change, the possibility that the patient would present with DDD combined with Modic type changes was very high. After performing NMR it was observed that approximately 47% of patients with pinched discs presented with DDD or Modic type changes.
In the case of facet joint osteoarthritis similar events occurred, since imaging studies were able to detect facet joint degenerative changes, although this does not imply the presence of a facet syndrome or lumbar pain, since many of these changes appear in asymptomatic individuals.15 In contrast, it may be stated that in patients with good clinical and radiological correlation this could be an indirect sign of canal stenosis. In our case, 22% of patients who underwent surgery presented with facet joint osteoarthritis in the plain X-rays. If to this we add that 35% of the patients who underwent surgery presented with canal stenosis in the NMR, it may be considered that facet joint osteoarthritis could be an indirect sign of this condition.
Despite the fact that according to Rosenberg,16 the incidence of a spondilolistesis is approximately 4% and the most frequent location of it is L4–L5, our findings were different, with a listhesis incidence of 13%, and the most affected level being L5–S1, with no justification for these events. The difference in percentages and level of location is probably due to the fact that in the Rosenberg study they were analysing the general or asymptomatic population and in our study the sample was selected from patients with a background of low back pain (with greater involvement of level L5–S1), and for this reason they were referred to a spine surgery unit. Another bias in this case is that sometimes an “automatic” referral takes place to a specialised unit when some specialists detect listhesis, even when it is asymptomatic.
Regarding the grouping of radiologic changes, it is true that only dividing them into two groups (pathological X-rays or non-pathological) without specifying what type of change they present, could be considered very simple analysis of them and a study limitation, but the aim of this study was to develop a user-friendly tool for primary care physicians and/or specialists who are not dedicated to spine surgery. We may also add that in the results obtained no statistically significant differences were obtained when proposing surgical treatment based on a more detailed description of the X-rays (levels affected, grading of listhesis, etc.), and the grouping used appears to be sufficient.
At the end of the study confirmation was made that the patients who underwent surgery were most commonly diagnosed with a herniated disc (17%), with DDD (21%) and with canal stenosis (35%) (p<.05), and these patients were the ones who, apart from presenting with low back pain, presented more frequently with radicular symptoms. We must therefore again state the need for appropriate clinical and radiological correlation prior to proposing more aggressive therapeutic measures.
Since all patients included in the study belonged to the same health area and were assessed by the same observer, this could entail a study limitation due to low reproducibility (it is assumed that the surgical criteria of the observer were correct). However, the sample was therefore more homogeneous, bringing greater force to the study.
Once data analysis had terminated and after successfully developing a calculator which was able to predict the probability of undergoing surgery based on age, the presence of radiologic changes, positive Lasègue signs and Waddell non organic signs, the problem of coming up with a value to determine which patients should be referred to spine units as highly probable candidates for surgical treatment. To solve this problem, we decided to analyse what percentage was obtained after using the calculator on patients who were operated on at the end of the study, and we obtained a result above 62%. Whilst waiting to extent the study to other health areas to corroborate the usefulness of the tool, we would therefore recommend that patients who were above the previously mentioned 62% be sent to the spine unit.
In addition to the calculation in patients who had undergone surgery, we analysed what results the calculator provided on all patients who had not undergone surgery. In this case, the result obtained was a 47% probability of being operated on, but, according to the Bayer's theorem, also called pretest probability,17 any patient has a 50% chance of being operated on when they present for consultation at a Spine Surgery. To solve this bias, the calculator has to be designed to assess the prevalence of non-operation, since knowing that they will not be operated on means the pretest probability is different. In our study, this calculation obtained a result of a 56.4% chance of not being operated on.
Despite the promising performance of the calculator, we agree with Chou et al.8 and with Jacobs et al.18 and we reserve surgical treatment for the patients who have been referred to Spine Surgery units who present with chronic pain, major functional limitation during a period of approximately 6 months or progression of neurological involvement, who have not responded satisfactorily to appropriate conservative treatment for 6–12weeks and who present with good radiological and clinical correlation.
ConclusionsUsing the calculator enables a prediction to be made with 70% reliability about the possibility of surgical intervention at lumbar spine level based on age, changes in plain X-ray, Lasègue's sign and Waddells's non-organic signs. Consequently, patients with a result from the calculator equal to or above 62% should be referred for consultation in the Spine Surgery unit for assessment by a specialist.
Level of evidenceLevel of scientific evidence III.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Puerto-Vázquez MG, Vicario-Espinosa C, Criado-Álvarez JJ, Marco-Martínez F. Desarrollo de una calculadora para establecer indicación de derivación a consulta de cirugía del raquis en patología degenerativa lumbar. Rev Esp Cir Ortop Traumatol. 2020;64:177–184.