Modern cement implantation techniques during hip arthroplasty rely on high intramedullary pressures which can result in cement extrusion towards femoral nutrient vessels, and thus, the occurrence of a particular image in postoperative radiographs (bone cement arterio-venogram).
We report a case series of 14 patients in whom a bone cement arterio-venogram was observed after undergoing a cemented hip arthroplasty. No local or systemic complications developed after cementing nor during a mean follow-up of three years.
Bone cement arterio-venogram is a radiologic sign that indicates a good cement pressurisation during surgery and is not associated to medical complications or periprosthetic femoral fractures.
Las altas presiones intramedulares que se alcanzan durante la cementación en la artroplastia de cadera pueden producir la extrusión de este cemento hacia los vasos nutricios femorales, generando una imagen radiográfica característica (arteriovenograma de cemento o cementograma).
Presentamos una serie de 14 casos de pacientes intervenidos mediante artroplastia de cadera cementada en los que se observó un cementograma como hallazgo postoperatorio. Ninguno de estos pacientes sufrió complicaciones locales o sistémicas tras la cementación ni durante un seguimiento medio de 3 años.
El cementograma es un hallazgo radiográfico postoperatorio que da cuenta de una buena presurización del cemento durante la cirugía y que no se asocia a complicaciones médicas ni a fracturas alrededor del implante femoral.
The current cement implantation methods for hip arthroplasties require appropriate pressurisation and technique. The aim of cement implantation is to keep the implant in its correct position for as long as possible, achieved through stable cement-bone interaction, by means of close union and interdigitation of the cement with the bone surrounding it.1 The third generation of cements we currently use is to optimise this mechanical cement-trabecular bone interface by using retrograde cement guns and intra-canal pressurisation with restrictor or the surgeon's thumb.2
The pressure peaks that can be reached inside the femoral canal reach up to 1500 KPa in in vitro studies,3 depending on different volumetric and biomechanical parameters, as well as on the viscoelastic properties of the bone that houses it.
This increase in pressure at the time of cement implantation can generate local polymethylmethacrylate leaks.4,5 The leakage of cement through nutrient vessels in the bone generates the presence of radio-opaque images peri-diaphysis, which can be confused with leaks from cortical fissures, but in reality correspond to arterio-venograms, also called cementograms, as they have been described in the few existing publications. Venous valve failure would favour this intravascular extrusion, although we cannot rule out the possibility that some cases are extravascular extrusions through nutrient foramens of the femoral cortex.6,7
To a lesser extent, but with greater risk for the patient, cases of leakage or distal embolism have been described, either of PMMA or fat embolism due to increased intracanal pressure.8,9
We present a series of cases recorded in our centre of migration of cement through a tributary vein or artery of the femoral diaphysis while performing partial and total cemented hip prostheses (Fig. 1).
Our objective is to determine the repercussions of these radiological findings on the results of arthroplasty and to evaluate potential local and remote medical-surgical complications, given that there is insufficient scientific evidence to attach a positive or negative value to these intravascular cement leaks.
Material and methodWe reviewed the database of hip arthroplasties performed in our centre from 2012 to 2018, collecting the patients who had a cement arteriovenogram as a postoperative radiographic finding in the total of 1500 patients operated by means of cement arthroplasty in this period.
In all of them, the surgery was carried out by at least one of our centre’s 4 expert surgeons in prosthetic hip surgery, via a lateral hip approach (Hardinge approach) and using a third generation cementation technique: distal polyethylene restrictor, pressure washing of the canal, drying of the canal by means of an absorbent sponge, vacuum cement centrifuge and cement gun (PALAMIX®), a dose of 75 g high viscosity cement with gentamicin (PALACOS®) and flexible proximal restrictor adapted to the gun (PALAMIX®) or the surgeon's fingers as a proximal restrictor.
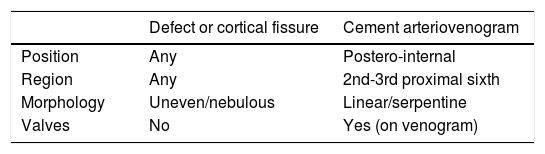
The radiological characteristics of the cement were evaluated with plain X-ray, calibrated with a marker, in anteroposterior projections of the pelvis and axial of the hip, considering cement arteriovenogram to be the radio-opaque images located in the postero-internal face of the proximal femur, with a radiological density close to that of the bone cortex and of linear or serpentine morphology (Table 1). The images suggesting cortical defects were not taken into consideration, and the five cases we found were rejected.
Differences in radiographic characteristics between extrusion of cement into the femoral nutrient vessels (cement arteriovenogram) and extrusion of cement through cortical defects or fissures produced with the fracture or during surgery.
| Defect or cortical fissure | Cement arteriovenogram | |
|---|---|---|
| Position | Any | Postero-internal |
| Region | Any | 2nd-3rd proximal sixth |
| Morphology | Uneven/nebulous | Linear/serpentine |
| Valves | No | Yes (on venogram) |
The patients’ demographic data, the prosthetic models used and possible associated complications (periprosthetic fractures, dislodgement of the femoral stem and cardiovascular or respiratory events) were analysed.
ResultsWe found a total of 14 patients whose postoperative radiography showed a cement arteriovenogram. They were all female, with an average age at surgery of 77.6 years (63–89 years). The mean height was 159 cm and the BMI was 27.3. Of the surgeries, 64.3% (9) were performed for coxarthrosis and 35.7% (5) for intracapsular femoral fractures. Laterality was left in 42.9% of the cases (6) and right in 57.1% (8). The stems used in the arthroplasty were metaphyseal anchoring stems in 71.4% (1 with MBA’s Furlong® model and 9 with Zimmer-Biomet’s F40™ model) and diaphyseal anchoring stems in 28.6% (4 with Stryker’s Exeter™ model).
The average length of the cement arteriovenogram was 26.3 mm, 100% of which was located on the posterior-internal face of the femur, at 154 ± 10 mm distal to the greater trochanter and at 17 ± 10 mm proximal to the tip of the stem. Dividing the femur into sixths, 35.7% (5) showed leakage in the proximal second sixth and 64.3% (9) in the proximal third sixth.
Regarding the short-term results of the arthroplasty, no dislodgement phenomena or postoperative femoral fractures were found. There were 2 cases of intraoperative fracture, both occurred around the trochanteric mass during metaphyseal reaming, which were handled by cerclage wire fixation or with a Dall-Miles®cable system. acetabular wear occurred 2 years after the surgery in one of the hemiarthroplasties and was operated by means of conversion to total hip arthroplasty, without replacement of the femoral component, which was well implanted.
After a mean follow-up of 3 years and 5 months (minimum follow-up of 3 months and maximum follow-up of 7 years and 8 months), no patient presented cardiovascular or respiratory complications. A patient with a history of unstable angina suffered 2 episodes of angina during admission, without elevation of troponins or abnormalities in the electrocardiogram or echocardiogram that would have led to suspicion of morbidity in addition to her basic illness, and was discharged from hospital without precordial pain symptoms. Another patient died during follow-up at the age of 89, 3 months after a hemiarthroplasty, due to a subarachnoid haemorrhage secondary to head trauma after an accidental fall.
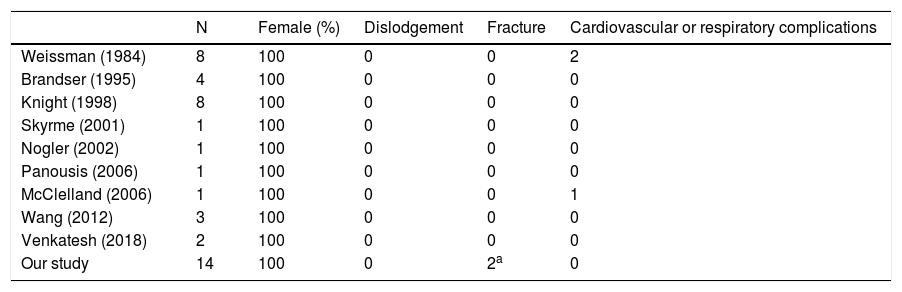
DiscussionWith 14 patients, our case series is now the longest and most time-consuming of those published so far on this characteristic radiographic image of extrusion of bone cement into the femoral nutrient vessels, first described by Weissman in 1984.5 Since then, the literature studying this finding is scarce, but everything published so far, as well as the results of our study, seems to indicate that it is a harmless consequence of the high intramedullary pressures necessary for correct cementation.
The correlation of cement extrusion with women of short stature and a small endosteal canal has been described.7 To date, all of the 29 cases reported in the literature correspond to female patients. The 14 cases that we add are also women, and therefore it could be thought that this phenomenon can only occur in female patients, although there is no exact reason yet to explain this.
The existence of a femoral nutrient bundle anatomically located between 170 ± 25 mm distal to the greater trochanter has been studied in live patients undergoing hip arthroplasties.10 In cadaveric studies, such a vascular bundle has been found around 166 ± 10 mm distal to the greater trochanter.11 All the studies agree that it is a tributary branch of the second perforator of the deep femoral artery, and that it is formed by an artery and one or two veins.12 The shorter average distance in our patients may be due to the shorter stature of the Spanish population compared to the Austrian and German population in the previous studies.
The constancy of the postero-internal location and at a distance that could correspond to the anatomical position of this femoral nutrient bundle should lead us to consider extrusion of the cement towards the veins or arteries that make up the bundle (Fig. 2). Likewise, the linear morphology of the radiographic image suggesting the vessel being occupied by cement, venous valves being observed, differs completely from that produced by a cortical defect or a periprosthetic fracture (Fig. 3), which would result in an irregular image without tubular appearance or the presence of valves.13
Cement syndrome or cement implantation syndrome is defined as “hypoxia, hypotension and/or unexpected loss of consciousness”14 and is an entity with an aetiology and pathophysiology that are not fully established, which can result in right ventricular failure secondary to increased pulmonary blood pressure and, subsequently, systemic hypotension and cardiorespiratory arrest. The presence of micro emboli of bone cement into the systemic circulation has been proposed as a precipitating cause of this syndrome15 and, therefore, the appearance of a cement arteriovenogram could be understood as a possible risk factor.
Of all the cases published in the scientific literature, only 2 presented cardiovascular complications4 and one respiratory complications.16 None of these events had a clear causal or temporal relationship with cement implantation, but they should be taken into consideration as possible complications. However, their low incidence and their dubious correlation with cement implantation, mean we can dismiss the finding of a cement arteriovenogram as a risk factor for cement-implant syndrome.
In terms of implant stability, phenomena of femoral component dislodgment in the presence of a cement arteriovenogram have not yet been described. Although this is not proof that the cement arteriovenogram is always associated with good cement implantation, it is a clear indication of good interdigitation at the cement-bone interface (Table 2). The fractures produced during surgery in 2 of our patients are not attributable to cement implantation since they occurred prior to it and therefore cannot be related to the presence of the cement arteriovenogram.
Comparison of results among cases of cement arteriovenogram published to date.
| N | Female (%) | Dislodgement | Fracture | Cardiovascular or respiratory complications | |
|---|---|---|---|---|---|
| Weissman (1984) | 8 | 100 | 0 | 0 | 2 |
| Brandser (1995) | 4 | 100 | 0 | 0 | 0 |
| Knight (1998) | 8 | 100 | 0 | 0 | 0 |
| Skyrme (2001) | 1 | 100 | 0 | 0 | 0 |
| Nogler (2002) | 1 | 100 | 0 | 0 | 0 |
| Panousis (2006) | 1 | 100 | 0 | 0 | 0 |
| McClelland (2006) | 1 | 100 | 0 | 0 | 1 |
| Wang (2012) | 3 | 100 | 0 | 0 | 0 |
| Venkatesh (2018) | 2 | 100 | 0 | 0 | 0 |
| Our study | 14 | 100 | 0 | 2a | 0 |
The limitations of this study are its observational and retrospective character, and a relatively short follow-up to determine the durability of the stability of the implants.
ConclusionThe finding of a cement arteriovenogram in the postoperative radiographic control after hip arthroplasty is a sign that does not associate local or distant complications and arises as a result of the high intramedullary pressures achieved with modern cement implantation techniques.
Level of evidenceLevel of evidence: IV.
Conflict of interestsThe authors have no conflict of interests to declare. No funding was received to carry out this study.
Please cite this article as: Garríguez-Pérez D, García-Coiradas J, Otero-Otero J, Marco-Martínez F. Arteriovenograma de cemento óseo en artroplastia de cadera. Rev Esp Cir Ortop Traumatol. 2020;64:388–392.