The concept that small incisions lead to a better outcome in many procedures has extended into most surgical areas, orthopaedic surgery among them. However, in some cases there is not enough scientific evidence to recommend these procedures. This article attempts to provide an updated review of the works published with sufficient scientific evidence on the advantages of minimally invasive surgery (MIS) compared to conventional access approaches. The published articles, meta-analyses and systematic literature reviews with level I or II evidence are reviewed in topographic order. Wherever possible, the information available on the costs-benefits of this type of surgery is also reviewed.
En los últimos años se ha extendido en las áreas quirúrgicas, entre ellas la cirugía ortopédica, el concepto de que las incisiones pequeñas facilitan una mejor evolución en múltiples procesos. Sin embargo, no existe en algunos casos una evidencia científica (EC) suficiente para recomendar estos procedimientos. Este artículo pretende realizar una revisión actualizada de los trabajos publicados con EC suficiente sobre las ventajas de la cirugía de mínima invasión (MIS) en comparación con las vías de acceso convencionales. A través de un orden topográfico se revisan los trabajos publicados con nivel de evidencia i o ii y los meta-análisis y revisiones sistemáticas de la literatura médica. Cuando ha sido posible también se ha revisado la información disponible sobre el coste-beneficio de este tipo de cirugía.
When surgeons consider a surgical technique they seek the maximum benefit for the patient and consequently the minimum local and general aggression. Therefore, “minimal invasion” is not a new and revolutionary concept, but rather one which is implicit in surgery since its inception. So-called “minimal invasion” is not an antonym of “open approach” nor is it determined by the size of an incision. As will be reviewed in this work, there are open approaches which involve minimal invasion to correctly and successfully treat a particular process, and there are supposedly minimally invasive techniques which are far more aggressive than the conventional alternatives. By using the term “minimal” we refer to the extent of tissue damage and, as a general rule, this is not proportional to the size of the approach. Before continuing, we should make an observation for readers: despite knowing its inaccurate meaning in Spanish, we have used the word “invasion” in this work, for it seemed easier to understand by readers, who will surely be accustomed to Anglo-Saxon literature and the term MIS (minimally invasive surgery).
The title of this work evokes the existing debate between a supposedly modern technique, minimally invasive surgery, and other, supposedly older ones, such as conventional techniques. Some authors believe that advances in the size of the incision have been encouraged and promoted in order to enable different, more “natural” and even “greener” techniques, as opposed to the aggressive, derogatory and “obsolete” concept of conventional techniques. This debate, loaded with fundamentalism by some surgeons and schools, distorts the true concept of minimal invasion, considering as such the least aggression possible for bones and soft tissues.
A certain level of simple-mindedness, marketing and especially lack of scientific basis and rigor are present in this issue. Justified by supposed advantages with regard to minimal tissue alteration, faster healing and better local and general recovery, patients are oriented towards new processes without sufficient support of scientific evidence (SE) and recommendation degrees. We must bear in mind that the manner and time in which a particular soft tissue lesion heals and scars is the product of its own idiosyncrasy, as well as the adequacy of its treatment. Most often, it is completely independent of the size of the route by which it was generated. Neither do the wishes of patients follow the same pattern as those of minimal invasion enthusiasts. The main desire of patients is a complete recovery with minimal discomfort and pain, secondarily to achieving it in the shortest possible time (and this is determined more by the nature of the lesion itself and by the delays inherent in the repair process), all this with the least aesthetic disruption and with results that last as long as possible. In professional practice, patients rarely ask questions about the size of the resulting scar in preoperative consultation. Instead, they always ask about the elimination of pain and any resulting functional limitations. Thus, it seems that the objective of minimal invasion is more a purpose for surgeons than for patients.
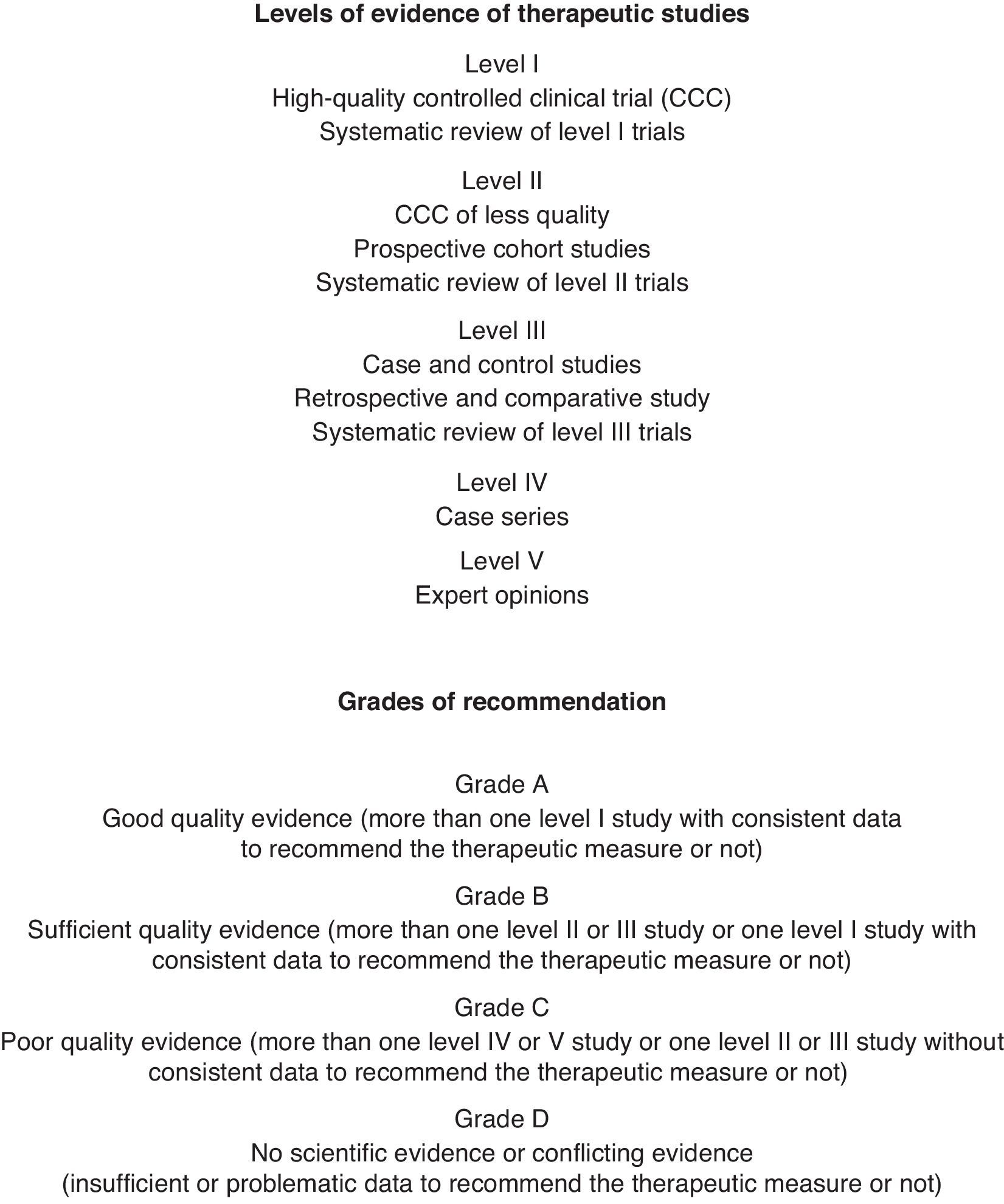
Our obligation is to maintain a critical attitude and analyse the potential advantages and disadvantages of some methods over others in the light of available SE. Only then can we offer patients the best treatment option with a rational basis on which to rely upon. We will review the different existing and proposed “minimally invasive” techniques, including arthroscopic and endoscopic techniques,1,2 which despite their universal and enthusiastic acceptance should, like other procedures, be used rationally and according to SE.3 In order to make the article more cohesive, we will follow a topographical order. The comparison of the different methods analysed has been performed in the light of works with levels I and II of SE (Fig. 1), meta-analyses and systematic literature reviews, capable of detecting real differences between them. Whenever relevant literature was available, we also addressed the cost-effectiveness of different procedures. Often, all this process leads to recommendations on what to do, or not do, in each individual case.
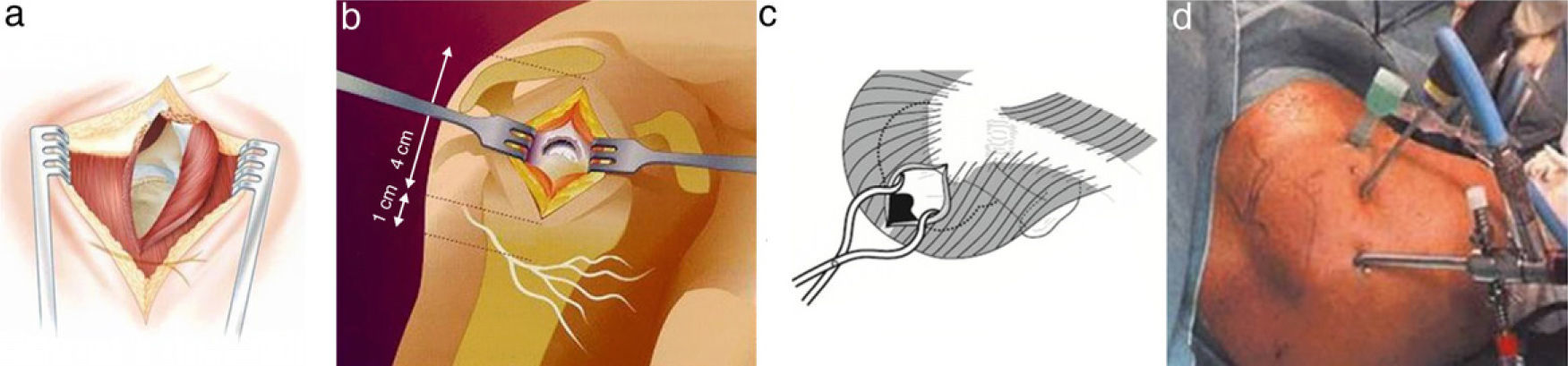
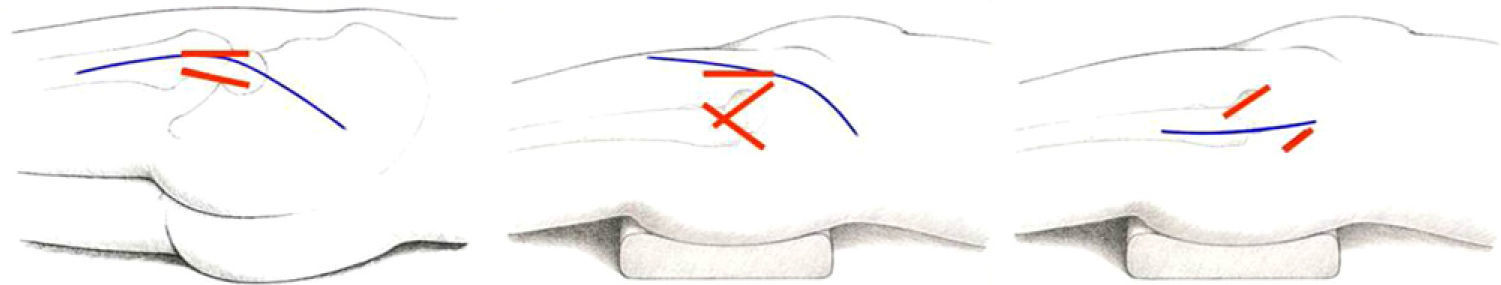
ShoulderSubacromial and rotator cuff pathologySubacromial space and rotator cuff surgery can be performed through various approaches (Fig. 2). From largest to smallest size, we must first mention the conventional subacromial route. This is about 5cm in length, accompanied by disinsertion of the deltoid fibres from the acromion, 1cm on each side of the longitudinal branch of the incision, forming a “T” shape, accessing the subacromial space through dissociation of the deltoid muscle fibres without disinserting them. The second option is known as “mini-open” and follows the same principles as the aforementioned transdeltoid route, but shortening its length by 3–4cm and without disinserting the deltoid. It can be used to resolve most cases and can always be expanded into a conventional open approach, thus following the usual practice of any surgeon to resolve the problem of poor visualisation: modulating and widening the access route to the required size. Finally, the third possibility is the most “minimally invasive” of the 3: arthroscopy through 2 or 3 portals. It also can be transformed into an open route by longitudinally extending the lateral portal.4
The hypothetical advantages of open surgery cited in the literature include better visualisation, better mobilisation of the tendons, less operative time, a less demanding technique and less necessary instrumentation. On the other hand, regarding arthroscopy, it has been reported to free the surgeon from spatial limitations, enable inspection of the joint (very important), preserve the deltoid muscle (like the mini-open approach without disinsertion of the deltoid), supposedly reduce morbidity and hospital stay, shorten recovery and produce better cosmetic results which, as mentioned previously, are a minor concern for the vast majority of patients. Reported drawbacks include less accuracy to assess structures and their level of repair, longer duration of surgery, greater technical difficulty and more necessary infrastructure, with the added cost entailed.
This raises several questions. Does arthroscopy represent an improvement over open surgery in the treatment of these processes? What is its level of safety? Does it work in all cases? Can it be used by everyone? Is it predictable, reliable, reproducible and durable in terms of results? Preference for one technique over the other is linked to the response to these questions.
With respect to acromioplasty as a treatment for Neer grade II subacromial syndrome and comparing open surgery with arthroscopy, there is 1 work with level I SE which did not any find any significant difference between them.5 This was also confirmed in a systematic review with level II SE, including 4 level I studies and 1 level II study.6 In a recent meta-analysis,7 the clinical outcomes, operative time and complication rates were similar for open and arthroscopic acromioplasty. However, hospital stay was less and return to work was faster with arthroscopic acromioplasty, in a statistically significant manner for both parameters. The latest Cochrane review on the different forms of surgical treatment for rotator cuff pathology concluded that, in view of the known publications, no definitive conclusions could be reached about the efficacy or safety of these procedures.8 There is “silver standard” evidence (www.cochranemsk.org) stemming from 6 studies which did not detect any differences in the results of open or arthroscopic acromioplasties, although 4 of them reported a faster recovery with the latter technique. Finally, there is 1 study with level I SE showing that, despite there being no differences regarding postoperative improvement in patient satisfaction, UCLA scale score or force, open acromioplasty was significantly superior in terms of both pain and function.9
When comparing rotator cuff repair with mini-open or open techniques, we noticed a faster improvement, with significantly better results and quality of life at 3 months, after surgery with the mini-open repair. Nevertheless, in 1 work with level I SE this difference with open repair became cancelled after 1 and 2 years of surgery.10 We can therefore report the equivalence of these 2 rotator cuff repair techniques after the time periods mentioned. A systematic review of 32 studies, including 5 controlled and randomised studies, 4 comparative studies with a control group, 6 prospective cohort studies and 17 retrospective cohort studies, observed that functional outcomes were similar for open versus mini-open repairs, open versus arthroscopic repairs, and mini-open versus arthroscopic repairs, with a moderate level of evidence. The only significant difference observed was in return to work or sports activities (1 month sooner after mini-open compared with open repairs).11
There have been 2 reviews regarding rotator cuff repair by arthroscopic or mini-open approaches. Although there are no works with level I or II SE on this issue, no significant differences were found by any of the other existing studies, which do not exceed level III SE.12,13 More recently, a study with level II SE14 reported a reduced use of analgesics during the first postoperative week in the group of patients treated arthroscopically. Conversely, the study also reported less pain between the fourth and eighth postoperative weeks in the mini-open repair group. Clinical results, range of motion and magnetic resonance imaging (MRI) findings were similar at 6 months after surgery, thus supporting the idea that both techniques have equivalent outcomes after that period of time.
The mini-open repair technique is significantly faster, with 10min less operating time and lower cost than the arthroscopic technique.15 Cost-effectiveness analysis of rotator cuff repair favours the open method, with a cost/Oxford improvement unit of $14.50 for the open technique versus $63.18 for the arthroscopic option. The mean operating time was 14min less in the first technique compared to the second.16
Judging from the serum levels of C-reactive protein (CRP), haemoglobin and interleukin 6 (IL-6), the degree of surgical aggression in arthroscopic rotator cuff repair compared to the open technique showed no differences regarding the first 2 parameters. However, there was a significantly lower postoperative serum level of IL-6 in the arthroscopic group.17 Thus, the authors of this study concluded that arthroscopic repair was less invasive than open repair.
Regarding the recommendations and precautions after surgery (aimed at repairing and healing damaged tissues), we should bear in mind that the ability of damaged tissues for repair and healing is independent of the size of the access route. Therefore, the measures to be taken in order to successfully complete this process should be similar, and more conditioned by the type and size of the primary lesion, retraction of the edges, quality of the tendon, muscle atrophy and effectiveness of the repair technique. It takes between 6 and 9 weeks to obtain a strong rotator cuff scar. Thus, even the 5 or 6 weeks required to obtain a solid deltoid reinsertion, if necessary, will be included within that time frame. Therefore, the basic conditions will still be the same: the key point is to obtain a good repair, rather than the route employed to achieve it.
Shoulder instabilityAccording to a meta-analysis of the medical literature published between 1966 and 2003, open stabilisation provides better results than arthroscopic repair in terms of recurrence and return to activity for patients with recurrent, anterior shoulder instability.18 In another meta-analysis,19 randomised controlled studies revealed that arthroscopic techniques resulted in better function than open techniques, although they also entailed a higher risk of recurrence, redislocation and reoperations, thus being less effective in terms of reintegration of patients to their work and/or sports. In 1 study20 with level I SE, no differences in clinical outcomes were found between arthroscopic or traditional open repairs. Neither were any differences observed in the Cochrane review of this issue21 or other equivalent reviews.22 Arthroscopic methods are very sensitive to the technique employed in the repair19 and the most effective once achieve failure rates equivalent to open techniques.23
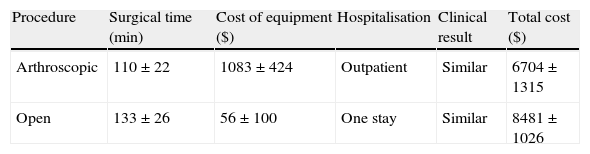
The cost of arthroscopic repair is less (Table 1), since it does not require hospitalisation and surgical time is reduced compared to the traditional Bankart technique, with similar clinical results.24 However, this shorter surgical time is directly related to the experience of the surgeon and his team.
Cost of arthroscopic stabilisation compared to open surgery in the shoulder.
| Procedure | Surgical time (min) | Cost of equipment ($) | Hospitalisation | Clinical result | Total cost ($) |
| Arthroscopic | 110±22 | 1083±424 | Outpatient | Similar | 6704±1315 |
| Open | 133±26 | 56±100 | One stay | Similar | 8481±1026 |
A recent literature review on the indications and results of minimally invasive arthroscopic elbow surgery attempted to determine the SE supporting its use and the recommendations which can be established thereof.25 The quality of existing work ranged between SE levels II and IV. There was reasonable evidence favouring the use of arthroscopy in the treatment of rheumatoid arthritis of the elbow and epicondylitis (grade B recommendation). However, there was little evidence favouring arthroscopic treatment of osteoarthritis, osteochondritis dissecans, removal of loose bodies, post-traumatic arthrofibrosis, posteromedial shock, excision of a plica, fractures of the condyle, coronoid and radial head, and arthroscopic resection of the radial head (grade C recommendation). There was insufficient evidence to recommend or contraindicate arthroscopic treatment in posterolateral rotatory instability and septic arthritis (grade I recommendation). It has not been demonstrated that the arthroscopic technique offers better, or at least similar, results than conventional treatment with open surgery in these elbow processes.
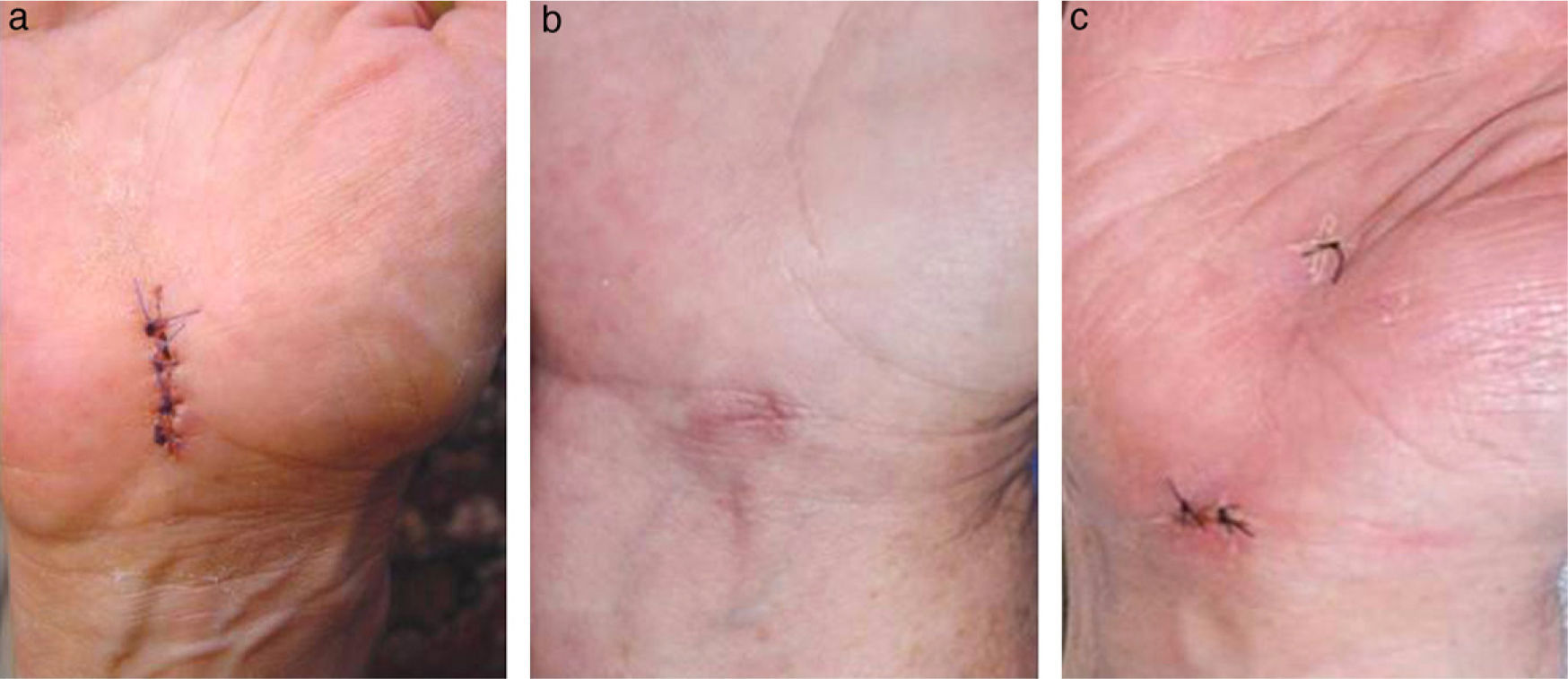
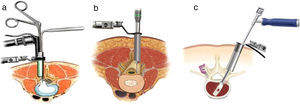
WristCarpal tunnel openingThis intervention is one of the most common procedures in orthopaedic surgery. It can be performed through a more or less large, conventional incision in the palmar side of the wrist or endoscopically with 1 or 2 portals (Fig. 3).
A comparison between open and endoscopic surgery showed no difference in results, except for a faster return to work activity, increased grip strength and reduced residual scar sensitivity with endoscopic treatment, as reported by 2 reviews with level II SE.26,27 On the other hand, the open technique was technically less demanding, entailed less risk of complications and had a lower cost.27
Comparing open surgery with the single portal endoscopic technique, 3 works with level II SE reported a lack of advantages of the former over the latter in relieving symptoms, postoperative period and recovery of muscle strength, hand function, grip strength, manual dexterity and sensitivity.28,29 The complication rate was similar for both alternatives.28 Operating time was shorter with the open procedure,28 while return to work was faster with the endoscopic technique,29,30 representing an economic benefit between $19030 and $947.29
As for the conventional, open technique31–33 or reduced mini-invasive procedure,34,35 no differences were observed compared to endoscopy with 2 portals regarding outcomes, symptom relief, complications or return to work activity in studies with level II SE.31,33–35 Subjective evaluation by patients was higher in the open technique,35 with a satisfaction rate of 93% versus 85% for endoscopy.31 At 5 years after surgery, there were no significant differences between both procedures according to a study with level I SE.32 Given the small size of the effect obtained by endoscopic intervention and only less postoperative pain until the third month, its cost-effectiveness advantage is doubtful.32
A meta-analysis of randomised controlled trials with level I or II SE, which analysed the effectiveness of different procedures for carpal tunnel opening, with long or short incision, through 1 or 2 portals, intrabursal or extrabursal, concluded that there was no difference in relief of symptoms associated with the technique employed. Neither were there any differences in residual, permanent, neurological damage, although endoscopy produced more neurological damage, albeit reversible. Nevertheless, it was also superior in grip strength and caused less scar sensitivity alterations. When analysing function and return to work, the evidence was contradictory, since different definitions were used and several collateral factors that could cause bias were included in the works examined.36
A cost-utility analysis performed by the same authors,37 adhering to the specific conditions of their institution, showed that endoscopic release required the use of a major operating room and general anaesthesia for 60min, whereas the open method took place in 30min, with local anaesthesia, in an outpatient surgery unit and with the aid of a single nurse. The mean cost of arthroscopy was $1015 and that of the open procedure was $356. The increase in cost-utility was $124,311 per unit of quality-adjusted life years (QALY) gained, thus providing strong evidence for rejecting endoscopic release performed in a major operating room, whereas open release can be performed in an ambulatory surgery unit. If both techniques took place in the same unit, the cost-effectiveness ratio would favour arthroscopic release.
In view of this evidence, the Cochrane review38 concluded that there was insufficient quality evidence to support the need to replace open carpal tunnel release with an alternative technique, such as endoscopic release. The use of one or the other is determined by the wishes of patients and surgeons. In its clinical guideline on the treatment of carpal tunnel syndrome,39 the American Academy of Orthopaedic Surgeons proposed the release of the median nerve through section of the flexor retinaculum as the preferred treatment of carpal tunnel syndrome, based on studies with levels I and II SE and recommendation grade A, regardless of the route and technique employed. The comment by Szabo40 on this subject is relevant: “The advantages of endoscopic carpal tunnel release are in no way equivalent to those of arthroscopic joint procedures. The scarce benefit obtained is substantially outweighed by disadvantages like poor or no visibility, inability to identify anatomical variants involved in the pathology and the risk of damaging neurovascular structures. The safety, efficacy and cost of endoscopic release are still disputed points. Cadaver studies have shown incomplete releases in over 50% of the specimens. Regardless of the technique employed, pain in the edges has not been reduced and dysesthetic palm hypersensitivity has not been eliminated. Grip strength returns to preoperative levels by the third month after the release and pinch strength by the sixth week. Endoscopic release has only shortened these periods minimally. Summing up, simple, open carpal tunnel release is still the preferred method of treating carpal tunnel syndrome”.
AnkleAchilles tendon repairPercutaneous repair of the Achilles tendon has represented a significant improvement in a field full of complications when using open surgery. Surgical repair is indicated because it significantly reduces the risk of iterative breakage entailed by conservative treatments. In addition, open surgery carries a high rate of complications, which can be reduced by percutaneous repair (Fig. 4), according to studies with level I and II SE.41–44 Patient satisfaction is 3 times higher with this technique.45
Ankle arthroscopyA review of published works regarding the indications and uses of ankle arthroscopy produced a series of recommendations in favour or against its use in certain cases.46 There is sufficient evidence to establish a grade B recommendation regarding the use of arthroscopy to treat ankle impingement syndrome, osteochondral lesions and arthrodesis in this joint. The evidence supporting arthroscopy in the treatment of ankle instability, septic arthritis and arthrofibrosis and removal of loose bodies is poor (grade C recommendation). Arthroscopy would not be indicated in the treatment of ankle osteoarthritis, excluding isolated bone shock and, therefore, would not be recommended in this indication (grade C recommendation, against). Finally, there is insufficient evidence to support or refute the benefit of arthroscopy in the treatment of ankle fractures and synovitis (grade I recommendation). As in the case of the elbow joint, it is necessary to pursue the subject with more quality studies, in order to consider arthroscopy as an alternative to open surgery.
SpineThe serum level of creatine phosphokinase (CPK) is a good marker of tissue damage. Thoracolumbar surgery, posterior approaches, duration of surgery, review surgery and preoperative CPK values are all factors which influence those levels.47 Comparing levels of circulating tissue damage markers, such as creatine phosphokinase, aldolase, proinflammatory cytokines, IL-6 and IL-8 and anti-inflammatory cytokines (IL-10 and IL-1 receptor antagonist), we can see that levels are higher after conventional open surgery than after performing minimally invasive surgery. Most of these markers return to normal levels 3 days after minimally invasive surgery, whereas it takes 7 days for normalisation after conventional surgery.48
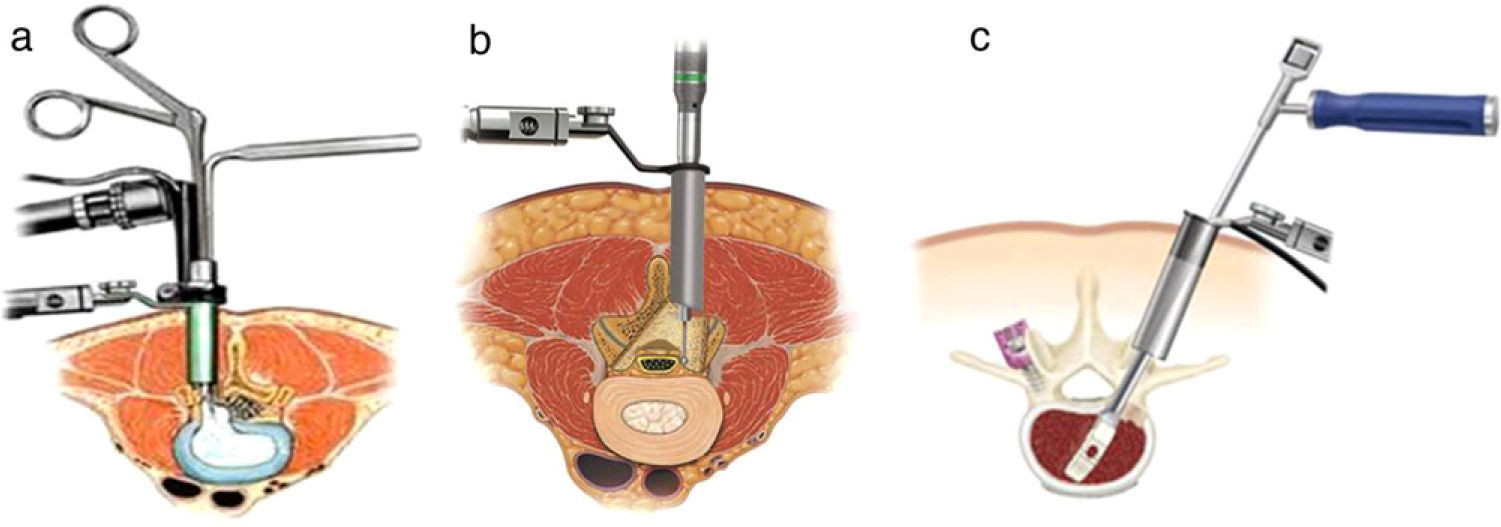
Despite the enthusiasm observed in the literature regarding the application of minimally invasive spine surgery (Fig. 5), we must highlight the scarcity of comparative studies in this field. A recent literature review49 found only 9 studies related to these techniques. We could not find any benefit in minimally invasive surgery referred to lumbar disc herniations, transforaminal lumbar interbody fusions (TLIF) or posterior lumbar interbody fusions (PLIF). Instead, there was a trend towards greater safety of open approaches in these procedures, mainly when using implants. Regarding lumbar disc herniations, reducing fascial incisions from 7 to 3cm did not shorten hospital stay or reduce the morbidity of the procedure in a study with level II SE.50 Similarly, another study with level I SE which compared traditional discectomy and microdiscectomy with the Caspar technique found significant differences (albeit so moderate that they may not have clinical significance) in operative time, bleeding, hospital stay and postoperative lumbalgia.51 The technique of transmuscular tubular discectomy through 18–22mm diameter tubes was introduced in order to favour and accelerate recovery, but has not shown significant advantages over conventional microdiscectomy.52 The same applied when discectomy was performed through an 11.5mm trocar.53 The absence of differences between both techniques may be due to the fact that both can be considered as minimally invasive.54 In fact, at 1 year there are no differences in multifidus atrophy verified by MRI with either technique.55 However, this procedure can be performed by an even more reduced route. Transforaminal disc surgery can be done through a skin incision of 6mm. Nevertheless, a level I study which compared endoscopic transforaminal discectomy with conventional microdiscectomy found similar sciatica relief and functional results, but greater lumbar pain during follow-up.56 Microendoscopic discectomy required more operative time but resulted in shorter hospital stay, with similar clinical and neurological final outcomes (level II SE).57
Regarding the treatment of lumbar canal stenosis, canal release with less aggression for the structures that form it has also been attempted. Unilateral or bilateral laminotomy is one of the limited procedures proposed to decrease the risk of instability after classic laminectomy. The results after unilateral laminotomy were equivalent to those obtained with laminectomy, whilst bilateral laminotomies provided a significant improvement in terms of reduction of symptoms and degree of dysfunction (level I SE).58 Another method to treat stenosis in a minimally invasive manner is through central microendoscopic decompression via a modified unilateral approach. Although this method requires more operative time and its clinical outcomes are similar to those of classic decompression by laminectomy, muscle trauma and risk of residual instability are minimal, enabling early mobilisation and decreasing hospital stay and postoperative pain, with satisfactory neurological and functional results. The level of muscle-type CPK isoenzyme is less than after classic laminectomy (level II SE).59 A comparison between the conventional microsurgical technique and endoscopic canal release did not show significant differences between them (level I SE).60
Posterior interbody arthrodesis by a transforaminal route is another alternative that has been used for a less aggressive intervertebral fusion, with less separation of the neural elements than by bilateral posterior interbody arthrodesis. This procedure can be carried out through an open or a minimally invasive approach. The MRI detects significant multifidus oedema when performing a conventional open TLIF, whereas if the procedure is performed using a minimally invasive technique, the muscle appears almost normal.61 Minimally invasive TLIF has similar long-term results and fusion index as open TLIF, but with the added benefits of less postoperative pain, earlier start of rehabilitation, shorter hospital stay and less complications (level II SE).62 In studies with 2 years of follow-up, this entailed a lower cost of minimally invasive TLIF versus open TLIF, showing an equivalent improvement in QALY.63
Regarding the PLIF procedure, the degree of multifidus atrophy was also much lower with a minimally invasive technique compared to a conventional open technique.64 Clinical results were significantly better, hospital stay was shorter and complications were less with a reduced PLIF approach (level II SE).65
Anterior lumbar interbody fusion (ALIF) has also been attempted with minimally invasive techniques, through a 5cm skin incision or by a transperitoneal or retroperitoneal route using a laparoscope, but no significant differences were observed (level II SE).66
Posterior instrumentation screwed to pedicles can be performed through a percutaneous route, resulting in only 3% of the screws in an “unacceptable” position.67 This caused less disruption to the paravertebral musculature than the open technique68 and provided a 50% improvement in trunk extension.
In summary, we must emphasise the scarcity of quality literature capable of supporting the use of any of the methods mentioned with sufficient SE recommendations. The clinical results and fusion rates achieved with minimally invasive procedures were similar to those achieved with traditional open techniques. So far, there is little evidence to justify minimally invasive anterior approaches, given the substantial rate of complications, longer operative time and the need for a long and expensive learning curve. The data for posterior minimally invasive approaches appear more promising, without the disadvantages of anterior approaches.69,70
OsteosynthesisDespite being an evolving and developing field, there are no quality publications which establish the advantages or disadvantages of minimally invasive versus conventional open techniques for the same fixation system. There is 1 work with level II SE which compared the use of osteosynthesis through minimally invasive plates and conventional open reduction and fixation of distal tibial fractures. This work found no significant differences between the 2 techniques.71
Evidently, intramedullary nails involve less invasion of soft tissues than osteosynthesis with plates, but the 2 procedures in this work could not be compared since they involved different philosophies and concepts, and bone aggression was also different. For obvious reasons, there are no high-quality, comparative works in this sense. We can only mention some, with level I or II SE, which found no significant differences between either method in the treatment of diaphyseal humeral fractures72 or distal diaphyseal tibial fractures.73
HipMinimally invasive approaches for hip replacement surgeryIn recent years, especially in the early 2000s, there has been a trend towards reducing approaches in hip prosthesis implantations. Smaller routes, about 8–10cm in size, have been proposed, with the same objectives as all minimally invasive surgeries, that is, less soft tissue damage, less blood loss, less postoperative pain, shorter hospital stay, faster rehabilitation and improved patient satisfaction, largely following the basic premises of classic approaches (Fig. 6). All are based on classic approaches with different variations74 and all make use of the concept of “moving window”, that is, the ability to see and reach the required field by moving the point of view to the desired location through the use of separators. In fact, in this technique there are more “shifters” than separators, which also avoid excessive tension on the edges and ends of the incision.
As the results vary considerably depending on the specific features of each route, we will highlight their characteristics. There is a minimally invasive variation of the Moore posterolateral pathway.75 It offers an excellent view of the acetabulum and femoral stem, is technically simple and does not require specialised instrumentation. It has been widely used and has extensive bibliographic support. Berger76 proposed an anterolateral route which required disinsertion of the anterior third of the gluteus medius, offering a good access to the acetabulum but a poor one to the femur. Special separators were recommended for this technique. Leaving these difficulties aside, the same author described a route with a double incision to access the acetabulum and femur separately, obtaining a poor view of the acetabulum and even poorer view of the femur. It required an image intensifier and special instruments to implant the stem, with the risk of causing femorocutaneous nerve injury and periprosthetic femoral fracture.77 The enthusiasm aroused in the beginning waned over time, and at present the technique has been practically abandoned. A minimally invasive anterior route has also been proposed,78 shortening the classical Smith-Petersen route, but it requires a special surgical table and instrumentation.
The “mini” posterior approach for total hip arthroplasties (THA) is the one with most available studies and with some quality SE.79 One study with level II SE80 compared the classic posterior approach of 23±2.1cm with a “mini” approach of 8.8±1.5cm. It showed that blood loss, length of stay, position of the components and complications were similar in both, but operative time was significantly less and the Harris scale score was better with the “mini” technique. Another study with level II SE81 compared a posterior approach of 15cm in length with another of 8cm, and found the same results, except that bleeding and persistence of postoperative claudication were less with the “mini” incision. A third study with level II SE compared a standard posterior route with a mean length of 20.2cm (range: 14.8–26cm), with a “mini” technique of 11.7cm (range: 7.3–13cm) and found a faster improvement in function with the “mini” alternative, although the results in terms of pain, function and range of motion showed no differences at 1 year from the intervention.82
One study with level I SE found no differences when using a posterior approach of less than 10cm or a standard approach, 16cm in length.83 Another study with level I SE reported that the posterior hip approach through a route 10±2cm in length enabled better control of postoperative pain, a shorter hospital stay and less use of walking aids. At 6 weeks and 3 months of the intervention, there were no differences between both groups.84
As for the double route, cadaver studies have shown that it is not possible to perform a THA by minimally invasive surgery (MIS) with double incision without causing substantial damage to the external rotators, abductor muscles or both. The lesion was significantly greater than with a posterior MIS.85 Another study with level I SE showed that the double route was a more complex procedure, with a mean operative time 20min longer than the posterior “mini” route and a slower recovery.86 The results at 2 months and at 1 year were the same and the complication rates were similar.86,87
A systematic review of the medical literature did not provide convincing evidence of any significant advantage of a small incision compared to a standard one when performing THA, except for a shorter scar, which is not synonymous with being better.88 Furthermore, 1 study with level II SE reviewed scars resulting from THA by MIS or conventional approaches and showed that plastic surgeon observers graded 30% of the “mini” scars as low quality, compared to only 7% of the conventional scars. Up to 20% of the “mini” scars were considered good, compared to 50% of the conventional. Regarding scarring problems, these appeared in 10% of the “mini” scars while there were none with the conventional approach. In total, 97% of patients considered as higher priorities the relief of pain and the duration of the arthroplasty procedure than the size of the resulting scar.89
One study with level II SE90 showed that the rehabilitation protocol, aggressive or conventional, had more influence on the result than the route employed to perform THA implantation. A systematic review of the clinical effectiveness and cost-effectiveness of MIS in hip arthroplasties for osteoarthritis, compared with a standard technique, found that the MIS had some small perioperative advantages, such as less blood loss and operative time, shorter hospital stay and faster recovery. It seemed to have a similar cost per procedure to the standard option, but the evidence regarding long-term results was too limited to ensure an advantage.91 Our view is that there is still a lack of long-term results and high-quality studies.92
Finally, an important question arises that we bring to the attention of the readers: is the MIS route to place a THA really MIS? A comparative study observed the alteration of biological parameters in “minimally invasive” approaches versus conventional total hip arthroplasties and found no evidence that a difference of 5cm in the skin incision influenced soft tissue lesion secondary to implantation.93 The observed increase during the postoperative period of IL-6 levels was unrelated to the size of the incision.81 Neither were there significant differences found in the mean level of postoperative C-reactive protein (CRP) when comparing both techniques.83 Analysing these studies, we can conclude that soft tissue alterations are more related to the surgical procedure itself than to the size of the route employed.
Hip arthroscopyOne review of the medical literature analysed the existing SE for hip arthroscopy.94 It found sufficient SE (grade B recommendation) to support this technique in the treatment of femoroacetabular impingement. The existing evidence to support a recommendation for use of hip arthroscopy in the treatment of labral lesions, extra-articular injuries, septic arthritis and articular free bodies was poor (grade C recommendation, in favour). There was conflicting, poor-quality evidence (grade C) against the use of hip arthroscopy for the treatment of intermediate or moderate coxarthrosis. Moreover, at this point we must apply the considerations mentioned previously for elbow arthroscopy.
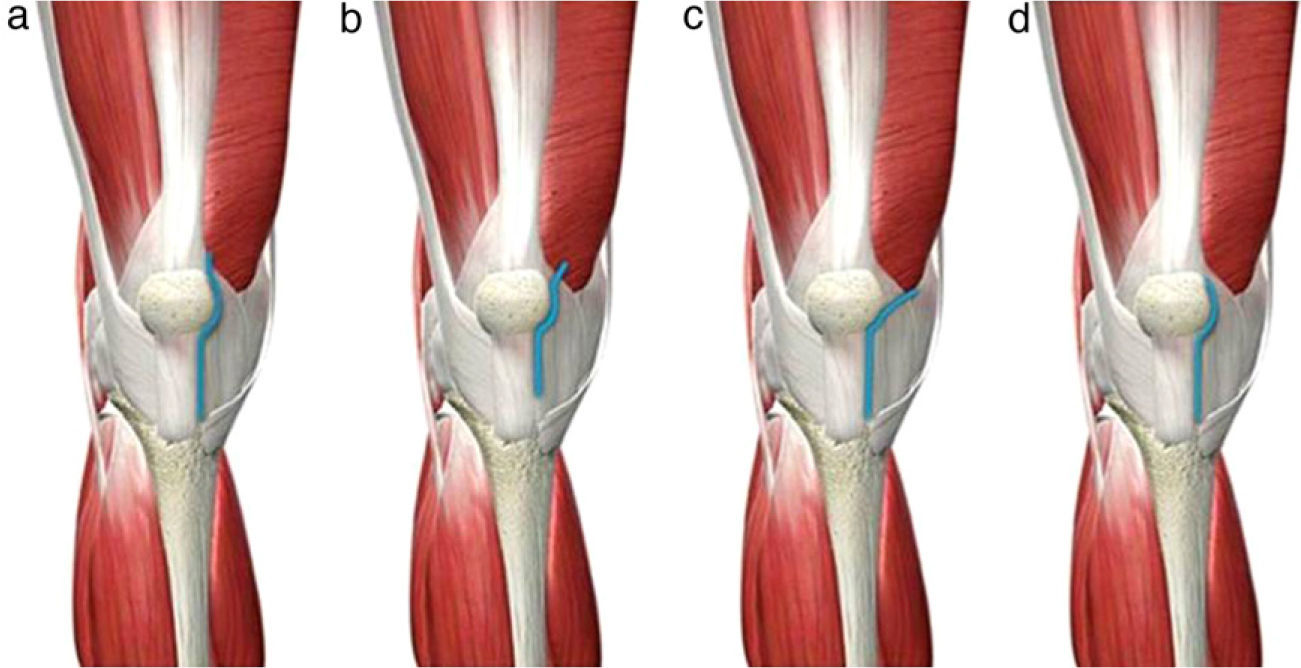
KneeMinimally invasive approaches for knee arthroplastiesMinimally invasive approaches to the knee reduce the incision length to about 7–10cm, and attempt to minimise manipulation and injury to periarticular soft tissues (mainly muscles and tendons, avoiding incisions through them), as well as everting the patella (Fig. 7).95 Both specific instrumentation and modular implants are desirable in order to perform these minimally invasive techniques without problems.96,97
Minimally invasive knee approaches. (a) Medial parapatellar, reducing the length of the classical route and with minimal incision of the quadriceps tendon in the tendon insertion of the vastus medialis. (b) Midvastus, penetrating about 2cm through the vastus medialis muscle body. (c) Subvastus, raising the vastus medialis. (d) Quad-sparing, without altering the tendinous structures of the quadriceps.
Given the characteristics of unicompartmental arthroplasties in terms of limited exposure field and small implant size, it seems logical to start with this procedure. There is 1 work with level II SE, referring to unicompartmental tibiofemoral arthroplasties, which showed a shorter duration of the intervention by using a “mini” incision, as well as less blood loss, shorter time to independent ambulation, less time to reach 90° flexion, shorter hospital stay and a higher degree of flexion at 6 months after surgery, with significant differences compared to conventional incision.98
No significant differences were detected in any of the parameters evaluated by 1 study with level II SE when comparing total knee arthroplasties (TKA) performed through a midvastus incision with those by a conventional route.99 The score on the Knee Society scale was better for the midvastus route at 6 weeks after surgery, but this became level with the conventional technique at 12 weeks. These same results were found by 1 work with level I SE published recently by Spanish authors,100 where the benefit provided by minimally invasive techniques disappeared at 6 months after surgery. The radiological position of the components was similar with both routes (level II SE).101 In a different work, knee mobility, function and scores on the Oxford and Knee Society scales were better for the MIS during the first 9 months, but equal thereafter (level II SE).102 A prospective, randomised, double-blind, controlled trial compared quadriceps strength at 3 weeks after surgery, as measured by the isometric and isokinetic extension torque, following bilateral TKA by a midvastus route or a parapatellar route, and the findings were favourable to the former technique. There were no differences regarding step length during ambulation, support time, pain or range of movement.103
One work with level I SE showed significant differences in favour of a subvastus incision versus the conventional technique regarding Knee Society scale score and range of motion, without any increase in the risk of component malposition, operative time or complication rate at 3 years of the intervention.104 A reduced blood loss, lower consumption of analgesics due to less pain and greater knee flexion in the first week had already been reported by a previous study with level II SE.105 In another study with level II SE,106 the subvastus technique without patellar eversion also showed less bleeding, better scores on the Oxford and Knee Society scales and improved mobility, ability to walk and to climb stairs at 6 months from the intervention, compared with the conventional technique everting the patella. However, these differences were not significant at 2 years; only an increased ability to kneel remained significant in the group operated by MIS. The short-term benefits of the subvastus route should outweigh the longer operative time and greater technical requirements of a more demanding technique with reduced visibility and access, needing a mean 15min more of ischemia and presenting a higher rate of complications, according to 1 study with level II SE.107
So as to document whether the subvastus approach was superior to the midvastus procedure in that the former fully preserved the extensor mechanism by not incising the quadriceps, both routes were compared in a randomised controlled trial with level I SE conducted on a group of patients operated with bilateral TKA.108 No significant differences were observed in any of the parameters analysed, including clinical results, muscle strength and mobility, blood loss, operative time and patient preference.
One systematic literature review compared the effectiveness of a conventional parapatellar approach with that of “mini”, midvastus or subvastus approaches. It found that hospital stay was similar between the conventional approach group and that undergoing a midvastus approach. However, there was a significant difference in favour of a subvastus approach, and also in terms of blood loss. Muscular strength recovery was faster with minimally invasive techniques than with conventional ones.109
One study with level II SE110 analysed the differences between the quad-sparing route, the conventional parapatellar approach and the “mini” midvastus approach. It found a significant difference in operative time, which was longer for the quad-sparing route (81±18.7min) compared to the standard route (67±8.1min) and the “mini” midvastus option (65±6.4min). There were no significant differences regarding blood loss, hospital stay or alignment and position of the prosthetic components. The functional outcome of the quad-sparing group was better in the short term, but subsequently became equal to that of the other 2 pathways analysed.
Paradoxically, in contrast to the above results, 1 systematic literature review, albeit with some methodological problems, found that TKA by a conventional approach had a positive effect on postoperative pain and function in relation to MIS techniques.111 One meta-analysis of randomised studies with level I or II SE concluded that, apart from a greater range of flexion in favour of MIS techniques, there were no other significant clinical or radiological differences between TKA performed by a conventional or a minimally invasive route.112 After analysing 4 studies with level I SE, 1 of them showed better results for the MIS compared with a traditional technique until the ninth month of follow-up, while the other 3 did not find any differences as early as 3 months after the intervention.113
In order to study whether minimally invasive knee techniques were truly minimally aggressive on soft tissue, serum levels of creatine phosphokinase (CPK), myoglobin, aldolase, lactate dehydrogenase, glutamic oxaloacetic transaminase and creatinine were compared on days 0, 1, 2, 4, 7 and 14 of the postoperative period between procedures conducted by conventional parapatellar medial, reduced midvastus, subvastus and quad-sparing routes. No differences were observed in any enzyme level. The highest elevation, although not significant, was observed in the midvastus route.114 A recent meta-analysis115 studied the short-term evolution of the conventional parapatellar and midvastus routes. After reviewing 18 works with sufficient SE, which included over 1000 patients, the authors concluded that the midvastus route offered a superior range of motion, less pain, less need for patellar release and fewer complications than the conventional route. The authors also acknowledged that the medium- and long-term results could be modified, as has also been reported by other works discussed.
As for the cost-effectiveness of minimally invasive techniques, it is accepted that inpatient costs are lower than those associated with conventional techniques. However, this difference is not significant and there is no reduction in direct hospital costs. More complete studies are required in order to determine whether any benefits can be observed after discharge.116
As noted in this article, there is abundant literature comparing the access routes for TKA. We may conclude that, at present, there is a difference in favour of MIS techniques during hospital stay regarding a reduced use of analgesics and improved welfare, and even in the first months after implantation. However, the situation becomes level with conventional routes at 6 months from the intervention. The greatest contribution of these techniques for surgeons is the possibility of performing TKA with a smaller incision and causing less soft tissue damage. Moreover, the use of the term “minimally invasive surgery” to describe a procedure which, while decreasing the skin incision, still involves patellofemoral dislocation, femoral, tibial and patellar osteotomies, resection of osteophytes, intramedullary invasion, etc., and seems unreasonable. From the results available, it is irrational to defend MIS routes in TKA stubbornly, at the expense of losing view, damaging skin coverage by excessive separator traction, malpositioning implants and increasing surgical time. Whenever patients undergo TKA, they do not usually require a smaller skin incision for aesthetic reasons, but rather seek assurances of being freed from pain and obtaining good function for as long as possible.
Repair of anterior cruciate ligament lesionsAlready in 1995, 1 work with level II SE117 compared knees which had undergone anterior cruciate ligament (ACL) repair by open surgery or by arthroscopy. It concluded that there were only 3 parameters with significant differences in favour of the arthroscopic technique: mobility of the knee at 1 month of the intervention, muscle atrophy and extension torque at 6 months. It is important to note that ACL repair provides identical results in terms of stability, mobility and muscle strength, regardless of the route employed, as long as the operation is followed by an aggressive functional recovery protocol (level II SE).118 Thus, it seems that the recovery program is more important than the route through which the surgical procedure is performed. The generalisation of arthroscopic repair in this ligament has settled the issue and it is no longer discussed. However, as observed in the 2 works cited, both of significant quality, a reflection on this issue would still be relevant.
Conclusions- 1.
The best access route is that which the surgeon is familiar with, regardless of the size of the scar.
- 2.
A correct view of anatomical structures is essential for orthopaedic surgery. If the surgeon cannot identify references and spaces exactly, the result of the procedure will not be excellent.
- 3.
It makes no sense to “suffer” in the operating room due to not being able to access a location successfully because of the size of the incision.
- 4.
Even if an intervention is planned through a minimal route, the possibility of changing the access by increasing the incision should always be available. A good surgeon must be realistic and avoid delays in surgical time just in order to create small incisions.
- 5.
The advantages of minimally invasive techniques are unquestionable in some specific procedures, but there are still doubts about whether their generalisation is advantageous. There are too few works of high quality and/or SE to demonstrate a superiority of minimally invasive techniques in terms of efficacy and safety compared to conventional techniques.
- 6.
The medical literature generally accepts a greater complexity, need for sophisticated and expensive tools and for a longer learning curve in minimally invasive procedures.
- 7.
Surgeons should attempt to perform the least invasive surgery possible, but also as invasive as required.
Level of evidence III.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Hernández-Vaquero D, et al. Cirugía de mínima invasión frente a cirugía convencional. Una aproximación desde la evidencia científica. Rev Esp Cir Ortop Traumatol. 2012;56:444–58.