The correction of thoracic and lumbar spine fractures with a short instrumentation using Schanz screws, is an effective method for stabilization and sagittal balance restoration.
Materials and methodsBidirectional observational study, included patients undergoing arthrodesis with Schanz screws to manage thoracic and lumbar fractures, the general characteristics, type, and location of the fracture, besides the gain in height of the vertebral body and segmental angle were analyzed before and after surgery. Clinical and imaging control was performed postoperatively and 1 month after this. p-value<.05 was statistically significant.
ResultsOf 35 patients undergoing arthrodesis, 13 were excluded due to the absence of images and follow-up. There was a higher proportion of men, the main location of the fracture and AO spine classification was in T12 and type A4/B1 respectively, there was no intraoperative complication, no transfusion was required, and a short hospital stay. A mild complication was presented in the follow-up. The average pre and postoperative change was 12 degrees in the Cobb angle and 5.2mm vertebral body height in the fractured vertebra, these changes were statistically significant.
ConclusionThoracolumbar and lumbar spine fracture correction with short segment fixation using Schanz screws, is an effective, safe and fast, showing significantly vertebral height gain and segmental angle correction, as a consequence, a correction of the balance and alignment of the spine.
La corrección de fracturas de columna torácica y lumbar con una instrumentación corta con tornillos Schanz es un método eficaz para la estabilización y la restauración del balance sagital.
Materiales y métodosEstudio observacional bidireccional, incluyeron pacientes sometidos a artrodesis con tornillos Schanz para manejo de fracturas torácicas y lumbares, se analizaron las características generales, tipo y ubicación de la fractura, además de la ganancia en la altura del cuerpo vertebral y ángulo segmentario antes y después de la cirugía. Se realizó control clínico e imagenológico postoperatorio y 1 mes después de esta. El valor p<0,05 fue estadísticamente significativo.
ResultadosDe 35 pacientes sometidos a artrodesis, 13 se excluyeron por ausencia de imágenes y seguimiento. Hubo una mayor proporción de hombres, la principal ubicación de la fractura y clasificación AO spine fue en T12 y tipo A4/B1 respectivamente, no hubo complicación intraoperatoria, no se requirió transfusión y corta estancia hospitalaria. En el seguimiento se presentó una complicación leve. El cambio pre y postquirúrgico fue de 12° en el Angulo Cobb y 5.2mm de altura en la vértebra fracturada, siendo estadísticamente significativos.
ConclusiónLa corrección de la fractura de la columna toracolumbar y lumbar con fijación de segmento corto con tornillos Schanz es efectiva, segura y rápida, y muestra una ganancia significativa de la altura vertebral y la corrección del ángulo segmentario, como consecuencia, una corrección del equilibrio y la alineación de la columna vertebral.
Spinal cord injury (SPI) is an event which leads to changes in sensory function, motor functions, normal autonomy and also may affect the physical, psychological and social wellbeing of the patient.1 Aetiologically, over 90% of SPI cases are caused by traffic accidents, violence, sports or falls and combined with the fact that the lesions of the spinal column often occur at a relatively young age, their socio-economic impact is significant.2
The locations most often affected in spinal cord trauma are: the sub axial cervical spine region (50%), followed by the thoracic region (35%) and the lumbar region (11%). Of these latter two, the thoraco-lumbar junction is affected in 50%–78% of patients who are neurologically intact.2,3 The aim of fracture treatment is mainly to obtain and maintain a stable reduction leading to early mobilization and in the last instance, to a satisfactory attachment and function. A secondary objective is sagittal balance restoration and this has gained force during the last decade.
In neurologically intact patients, the decision to undertake surgery depends on the post-traumatic kyphotic stability and deformity. There are different types of systems for open or percutanous fracture reduction, and also short or long attachments. Among the spine surgeon’s resources is the Schanz screw system which has a long lever arm that can be used to stabilise the spine, correct post-traumatic kyphosis and offer great construction rigidity once in place, with the benefit a short instrumentation has. Due to the above, the aim of this study was to present the experience in dorsal and lumbar fracture correction using a short fixation technique with Shanz pedicle screws.
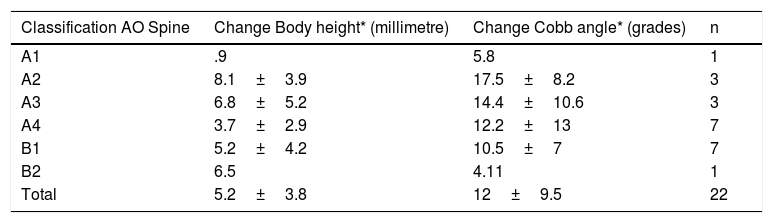
Materials and methodsA bidirectional case series study (retrospective and prospective) was performed, of patients who had undergone surgery for arthrodesis with Schanz screws for the management of traumatic thoracic and lumbar fractures. Patients were excluded from the study if data were lacking from their medical records, or there were no control and/or follow-up postoperative images. Sociodemographic information was collected, together with location and type of fracture in accordance with the AO Spine classification,4 pre and postoperative height of the fracture vertebral body and the Cobb angle (also called segmentary angle), and intra and postoperative complications. Regarding clinical and imaging follow-up, this was performed on the first postoperative day and month (Fig. 1). Routine radiography and computerized axial tomography (CAT) was taken for all patients of the thoracic and lumbar spine at the time of the trauma. Given the availability of hospital resources, magnetic resonance of the thoracic and lumbar sacral spine was made of selected patients who were waiting for this, to determine lesion of the posterior ligament complex.
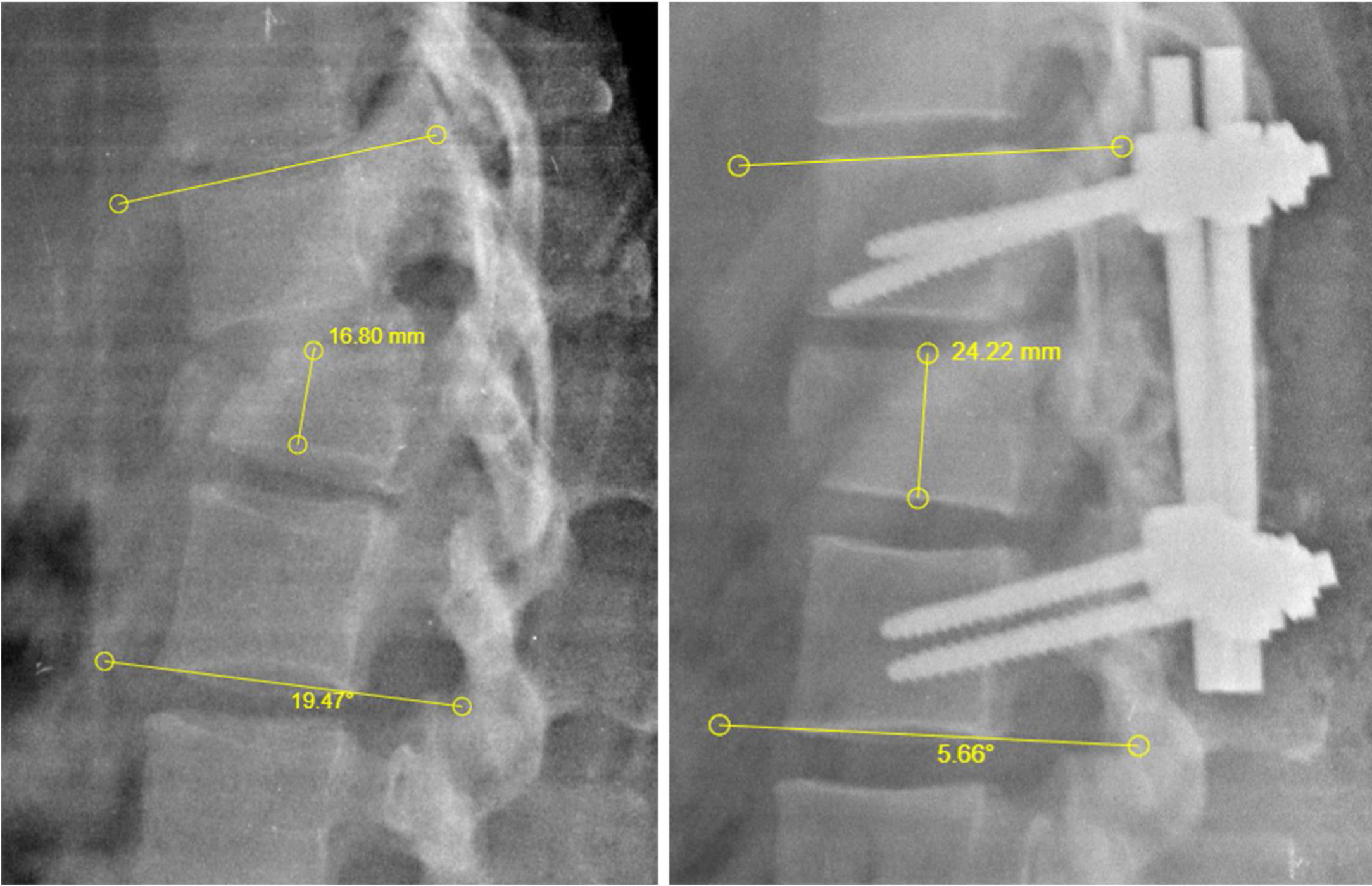
Measurement of the Cobb height and angle. Lumbar radiography in lateral projection pre and post surgery to outline taking of measurements of Cobb height and angle. Height of the vertebral body, measured by taking the distance between the upper and lower disk of the fractured vertebra, expressed in millimetres. Cobb angle: this is the angle resulting from the intersection of the two 90° angles taking as repair the upper disk of the upper vertebra and the lower disk of the lower vertebra compared with the fractured vertebra, expressed in grades.
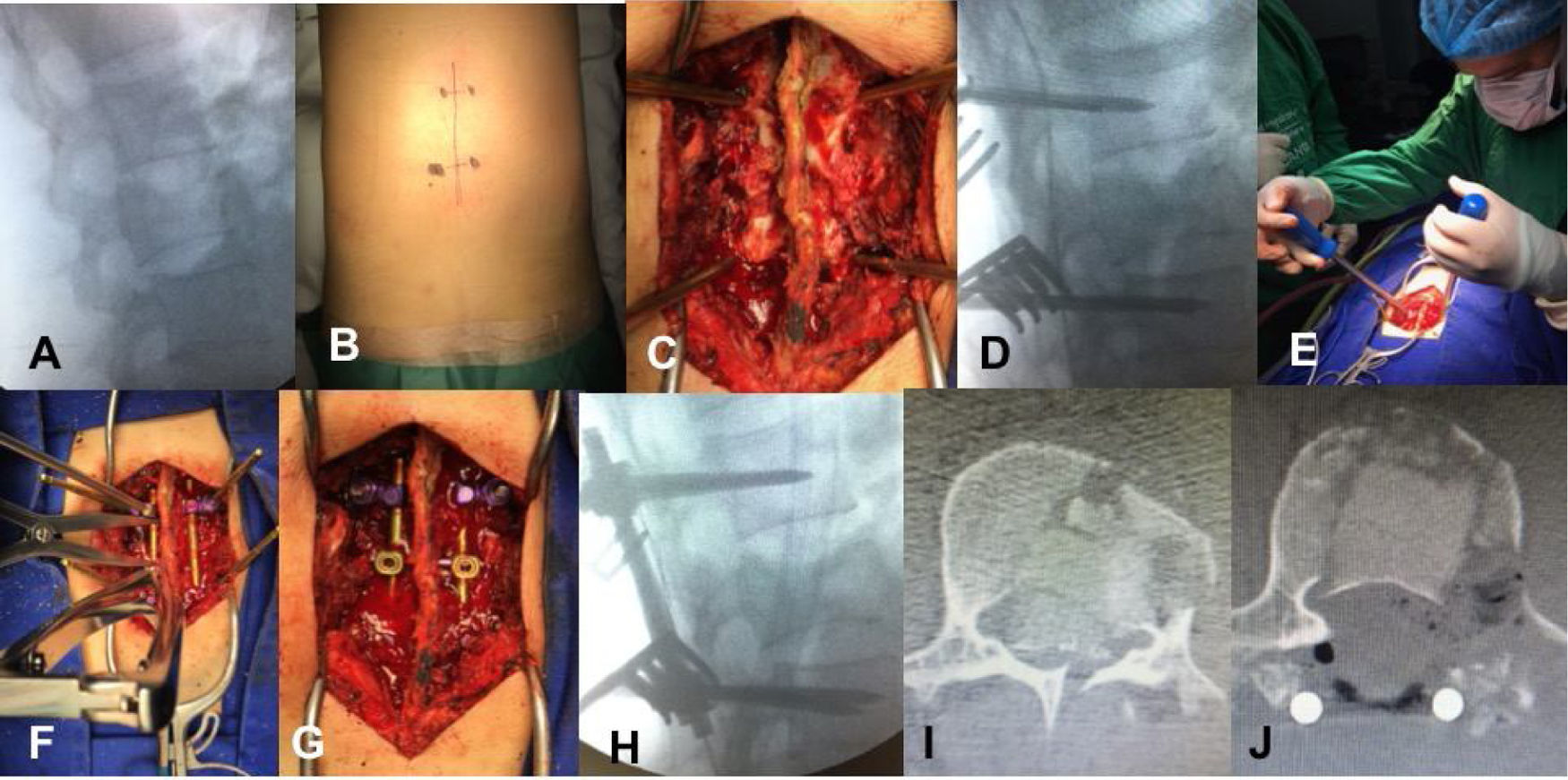
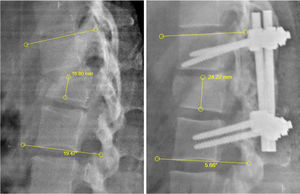
The patient was placed in prone position, with upper members extended, with pressure areas protected by rolls. Fluoroscopy marked the mid line and the pedicles of the vertebrae above and below the surgical fracture line. Subperiosteal dissection followed to expose posterior elements of the spine. Biplane fluoroscopy was used to place the Schanz screws bilaterally. The diameter of the screws had been previously measured in imaging. The screws were always to be placed proximal in bloodflow direction for better leverage. Reduction and ligamentotaxis manoeuvres followed with fixation of patellas and rods. Sharp round bur was used for scarification of bone surface and heterologous bone graft placement. Haemostasis was confirmed, layered closure and 1/8 epifascial hemovac drainage was left as required. In some cases, where bone fragments may be found inside the canal, laminectomy and impaction is performed on them (Fig. 2).
Surgical techniques for placing the Schanz screws. A) Fluoroscopic marking of the fracture, deployed in anteroposterior and lateral projections) Marking of midline surgical wound, pedicles of vertebra above and below fractured vertebra are marked. C) Subperiosteal dissection, passing fluoroscopy-guided Schanz screws. D) Confirmation of appropriate passage of Schanz screws. E) Reduction manoeuvre towards upper vertebra, with same manoeuvre towards lower. F) Distraction and ligamentotaxis. G) After fixation of system, scarification of bone surface performed and bone graft inserted. H) Intraoperative lateral view of arthrodesis and fracture reduction. I) Bone fragments inside the canal. J) Imaging proof of posterior intracanal bone fragments on laminectomy and impaction of them.
The quality of our data was verified with a randomised review of 10% of data. Descriptive statistical analysis was performed for all variables considered in the analysis and for selected subgroups. The Shapiro-Wilk test was used to determine data normality; data with normal distribution were presented as averages and standard deviation and those without a normal distribution were presented as median and interquartile ranges. The Student’s t-test was used to analyse continuous quantitative data from the same group and with normal distribution (change in the Cobb angle and pre and postoperative vertebral body height). The Stata statistical prorgramme version 14.0 was used for analysis, with statistical difference being considered if p≤.05 with 95% CI.
ResultsThird five patients underwent open reduction of vertebral fracture by means of the Schanz screws from January 2016 to March 2020 in the Hospital Santa Clara, Bogotá, Colombia. Thirteen patients were excluded, since there were no postoperative images and outpatient clinical follow-up.
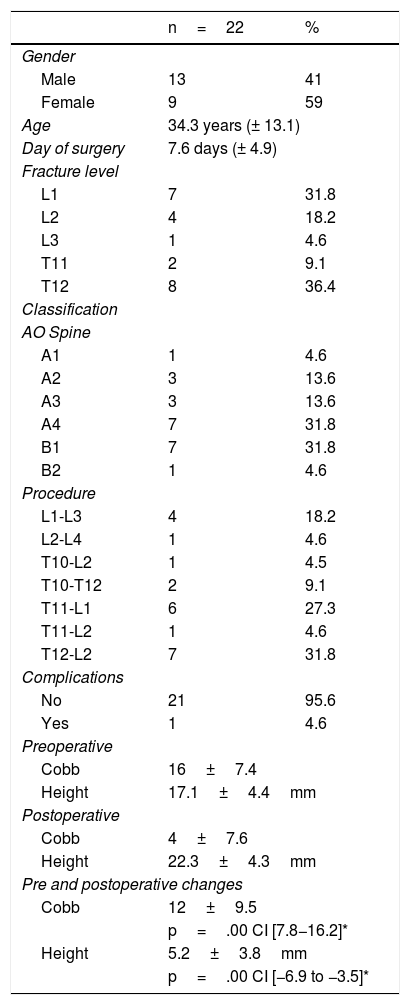
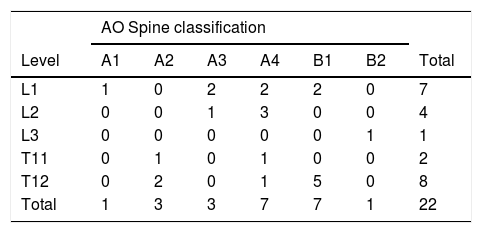
Analysis was performed with a total of 22 patients, where the majority were male, with an average mean age of 34 and time of onset to surgery of eight days. The levels most affected T12 and L1; within these, the most common type of fracture was B1 and A3/A4, respectively. None of the patients presented with intraoperative complications, and only one patient had a minor (seroma) complication, which was spontaneously resolved during follow-up (Tables 1 and 2). Time in surgery was between one hour and 1.5h. No red blood cells or other type of haemoderivatives were required for transfusion either intra or postoperatively and all patients were discharge early whenever possible.
Sociodemographic characteristics.
| n=22 | % | |
|---|---|---|
| Gender | ||
| Male | 13 | 41 |
| Female | 9 | 59 |
| Age | 34.3 years (± 13.1) | |
| Day of surgery | 7.6 days (± 4.9) | |
| Fracture level | ||
| L1 | 7 | 31.8 |
| L2 | 4 | 18.2 |
| L3 | 1 | 4.6 |
| T11 | 2 | 9.1 |
| T12 | 8 | 36.4 |
| Classification | ||
| AO Spine | ||
| A1 | 1 | 4.6 |
| A2 | 3 | 13.6 |
| A3 | 3 | 13.6 |
| A4 | 7 | 31.8 |
| B1 | 7 | 31.8 |
| B2 | 1 | 4.6 |
| Procedure | ||
| L1-L3 | 4 | 18.2 |
| L2-L4 | 1 | 4.6 |
| T10-L2 | 1 | 4.5 |
| T10-T12 | 2 | 9.1 |
| T11-L1 | 6 | 27.3 |
| T11-L2 | 1 | 4.6 |
| T12-L2 | 7 | 31.8 |
| Complications | ||
| No | 21 | 95.6 |
| Yes | 1 | 4.6 |
| Preoperative | ||
| Cobb | 16±7.4 | |
| Height | 17.1±4.4mm | |
| Postoperative | ||
| Cobb | 4±7.6 | |
| Height | 22.3±4.3mm | |
| Pre and postoperative changes | ||
| Cobb | 12±9.5 | |
| p=.00 CI [7.8−16.2]* | ||
| Height | 5.2±3.8mm | |
| p=.00 CI [−6.9 to −3.5]* | ||
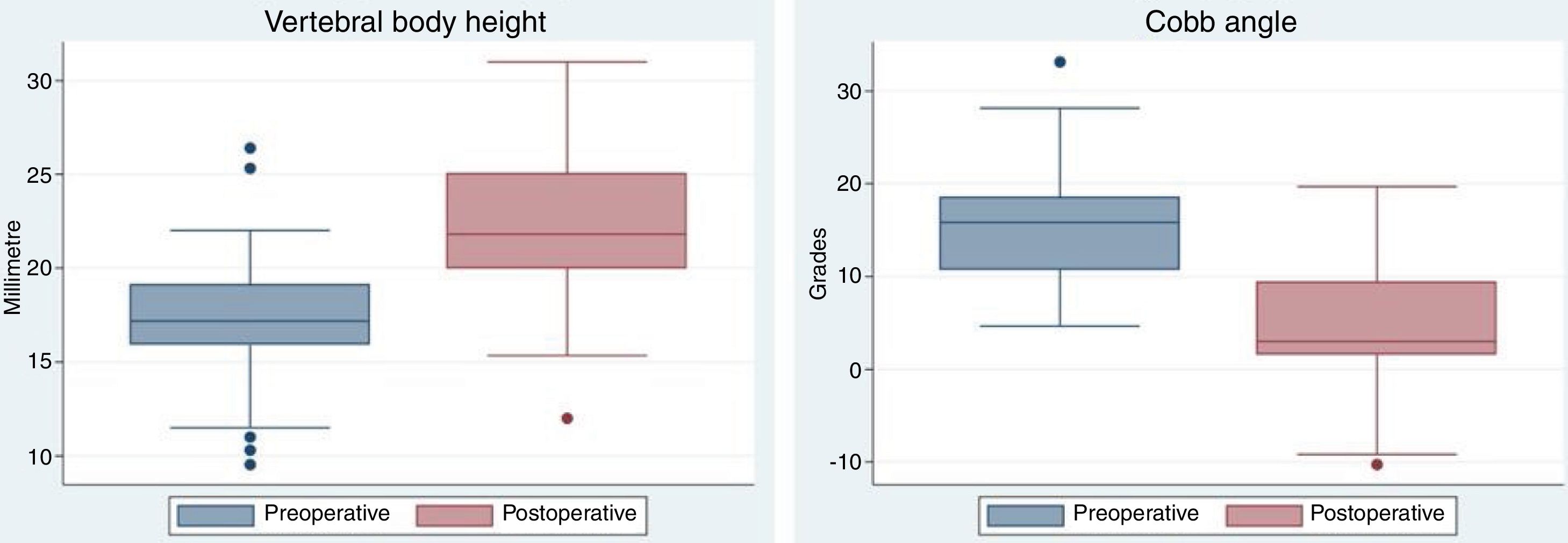
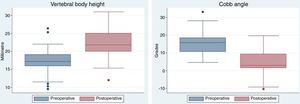
Regarding Cobb height and angle before and after surgery, Fig. 3 contains box plots with a change of 5.2mm being appreciated in the height and reduction of the Cobb angle of 12° in the postoperative period and this was statistically significant (Table 1). We also observed a relationship between the recuperation of the vertebral height and the Cobb angle with the fracture severity; with fracture of minor severity there was usually greater correction of size and Cobb angle reduction, compared with more severe fractures (A4 and B). Despite this, in more severe fractures it is of note that there is an increase in the height of the postoperative vertebral body of between 3.7 and 6.5mm and correction of the Cobb angle of between 4 and 12° (Table 3). Medical and imaging control was performed during the first postoperative month, with no loss of height, deforming in kyphosis or material failure observed.
Relationship between type of fracture and change in body height and Cobb angle after surgery.
Most thoraco-lumbar fractures are stable, with no neurological complications and are generally able to be treated non-surgically with a thoraco-lumbar support corset, leading to early moving around. However, unstable fractures lead to disability, deformity and significant neurological impairment.4,5 At present controversy still exists regarding appropriate imaging studies, indications for surgical treatment, time of surgery, approach and type of surgery, the need for fusion and the role of decompression of the spinal canal.5 Indications for surgery include: progressive neurological impairment; spinal cord compression; rotational instability; progressive symptomatic kyphosis; kyphosis>30°; concomittant lesions which require early immobilization; AO Spine type A4, B and C fractures. Relative indications also exist which include: loss of height>50%; canal compromise >50%; facet fracture and posterior spinal column lesion or posterior ligament complex.4–7 Treatment objectives of thoraco-lumbar fracture is spinal canal decompression and nerve root for neurological recovery; restoration and maintenance of height and vertebral recuperation with sagittal balance; rigid fixation for early moving about and rehabilitation and the prevention of progressive neurological lesions and kyphotic deformity.7 Surgical approach is posterior, anterior or a combination of these. These may be performed with long or short instrumentation, percutaneous or open, with fusion or without it, with canal decompression or without it, depending on the clinical symptoms and imaging results from each patient.
It has been determined that fixation with posterior pedicle screw is simple, widely known, effective, reliable and safe for the reduction and stabilisation of most fractures and continues to be the most widely used technique for fracture instrumentation with a posterior approach. These are superior systems for restoring and maintaining spine alignment, due to the fact they cross the three biomechanical columns of the spine, provide a longer lever arm through which the screw can convey greater corrective forces than those achieved by other fixation systems which only join posterior elements, applying forces, applying multidirectional correction forces and resisting loads on multiple planes.5,8–11 The disadvantages include instrumentation failures; pseudo-osteoarthritis; dural tearing and/or cerebrospinal fluid leak; dissection of extensive tissue sample exposing entry points; prolonged operations with significant blood loss and major risk of infection; neural tissue injury; inappropriate neurological decompression; insufficient correction of kyphosis; the need for delayed extraction of instrumentation and artefacts in posterior diagnostic images after implant. Rigid fixation may accelerate degeneration of the adjacent moving segment.5
In the posterior approach, instrumentation may be made by short fixation (this includes the normal proximal and distal adjacent vertebrae) or long fixation (two level above and below the fracture level). Short instrumentation has been beneficial due to several advantages such as the arthrodesis of fewer moving segments, which reduces time in surgery, lowers preoperative bleeding and prevents the loss of the lumbar lordosis associated with flat back syndrome, correction of the kyphotic deformity and lastly sagittal balance, provides greater initial stability, early painless mobility and indirect decompression of the spinal canal through a combination of postural reduction and distraction through ligamentotaxis.5,12,13 Li et al. concluded in their meta-analysis that radiographic indexes and implant failure were better in the long fixation group than in the short fixation group but the long fixation prolonged the length of the operation and clinical results suggested that there were no differences between the two types of fixation and selection of the appropriate method had to be cautiously made in an individualized manner.12 In contrast to Li, in their meta-analysis Ally et al. suggested that, although there were no differences in the kyphosis between fixation groups of short and long segment in the final follow-up, kyphosis progression occurred in both groups.13 Similar findings were encountered by Pellisé et al., who found no significant changes in the biomechanical properties of cadaveric spines with long or short segment.14 Similarly, Wu et al. demonstrated that there were no differences in range of movement between short and long fixation. They suggested the use of long instrumentation in the case of osteoporosis, probably because it provides greater mechanical rigidity for initial fixation and may reduce the probability of segmentary collapse.15 In the study by Shehaby et al. short fixation provided comparable correction to long segment fixation. They considered that the loss of correction could minimise the appropriate selection of appropriate cases for fixation of short segments, the latter being reserved for mild to moderate degrees of initial kyphosis.16 Different types of disadvantages relating to this short instrumentation were described, with an incidence of 9% to 54% of implant failure, loss of reduction between 50% and 0% (re-kyphosis) in long term follow-up, and 50% of patients with material failure had moderate to severe pain.17,18
There are different transpedicle instrumentation systems. In our experience, we considered that fixation with Schanz screws is superior to instrumentation with pedicle monoaxial screws and/or polyaxial screws, and for this reason in future studies we aim to compare our results with conventional pedicle screw fixation systems. We should note that this has already been studied, with consideration that the Schanz type pedicle screw system is superior due to its structure and the transmission of load of the Schanz threaded bar (similar to conduction in the shape of “] [“) which are more similar to the posterior lumbar spine (butterfly shaped conduction) than the convention pedicle screw (similar to conduction in the “| |”) shape. Also, the type of construction managed by the system, with a cantilever type movement, allows flexion r extension forces to be applied when the implant is inserted, thereby immediately restoring the vertebral body height and sagittal alignment.10,11,19–23 In our study the gain in vertebral body height of the fracture and the reduction of postoperative Cobb angle, which affects improvement of the sagittal alignment of the vertical columnar, maintained this reduction during the follow-up period. Similar events were found in recent publications, using short segment fixation for thoraco-lumbar and lumbar fractures, reporting that this technique leads to a satisfactory reduction and maintenance of the reduction in fractured vertebra.20–22 This, combined with the before-mentioned, makes it a safe procedure with minimal complications. We reported just one minor complication in the study, a subcutaneous seroma which was resolved with conservative treatment.
In this study we compared patients with screws in the proximal and distal vertebra to the fractured vertebra. It is not always possible to use a pedicle screw in the fractured vertebra for several reasons, such as intraoperative technical difficulties, percentage of vertebral body collapse, pedicle anatomy and pedicle compromise due to the fracture. However, the literature confirms the benefit of instrumentation in fractured vertebra because this fixation improves anterior and middle spine stability of the injured vertebra, restores vertebral height, aids correction of kyphosis with less loss over time and has a lower rate of implant failure, which leads to a reduction of the risk of back pain.24–26 Disadvantages are the longer time in surgery and intraoperative bleeding.27
Our aim in the future is to compare patients who undergo instrumentation with Schanz screws with and without fixation of the fractured vertebra, and also to compare this pedicle fixation system with other available options (polyaxial screws, uniplanar and/or monoaxial screws). This study will continue with the recruitment and follow-up of patients who have undergone dorsal and lumbar fracture correction aimed at including a larger number of patients and a longer follow-up period. The limitations of this study are that patients were collected retrospectively, and this conditions bias in data collection. The sample size was small and the follow-up time short for material failure and delayed complication observation. The Schanz screw fixation system was not compared to another arthrodesis system and did not resemble the construction size (short vs. long fixation). We aim to make comparisons in future studies.
ConclusionThoraco-lumbar and lumbar spine fracture correction with short segment fixation using the Schanz screw system is an effective, safe and fast method for fracture stabilisation and sagittal alignment correction, with a gain in fracture vertebral body height and reduction in Cobb angle in post-traumatic segmentary kyphosis. It also offers great construction rigidity once in place, with minimum associated morbidity.
Level of evidenceLevel of evidence III.
FinancingThis study did not receive any type of financing.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Gómez Vega JC, Vergara Lago MF. Reducción abierta de fracturas toracolumbares y corrección del balance sagital usando tornillos Schanz. Rev Esp Cir Ortop Traumatol. 2021;65:229–236.