The elderly population candidate for total hip arthroplasty (THA) is increasing exponentially in developed countries, due to the high prevalence of osteoarthritis (OA). The objective is to identify the overall survival in patients over 85 years with primary OA who underwent THA.
Material and MethodsRetrospective observational study in patients over 85 years with primary hip OA performing a THA between 2012 and 2019. Demographic, clinical, comorbidity, complications, functionality and pain variables were collected. A descriptive analysis was performed and survival was estimated with the Kaplan-Meier method and the differences in pain and functionality before and after surgery with the McNemar-Bowker test.
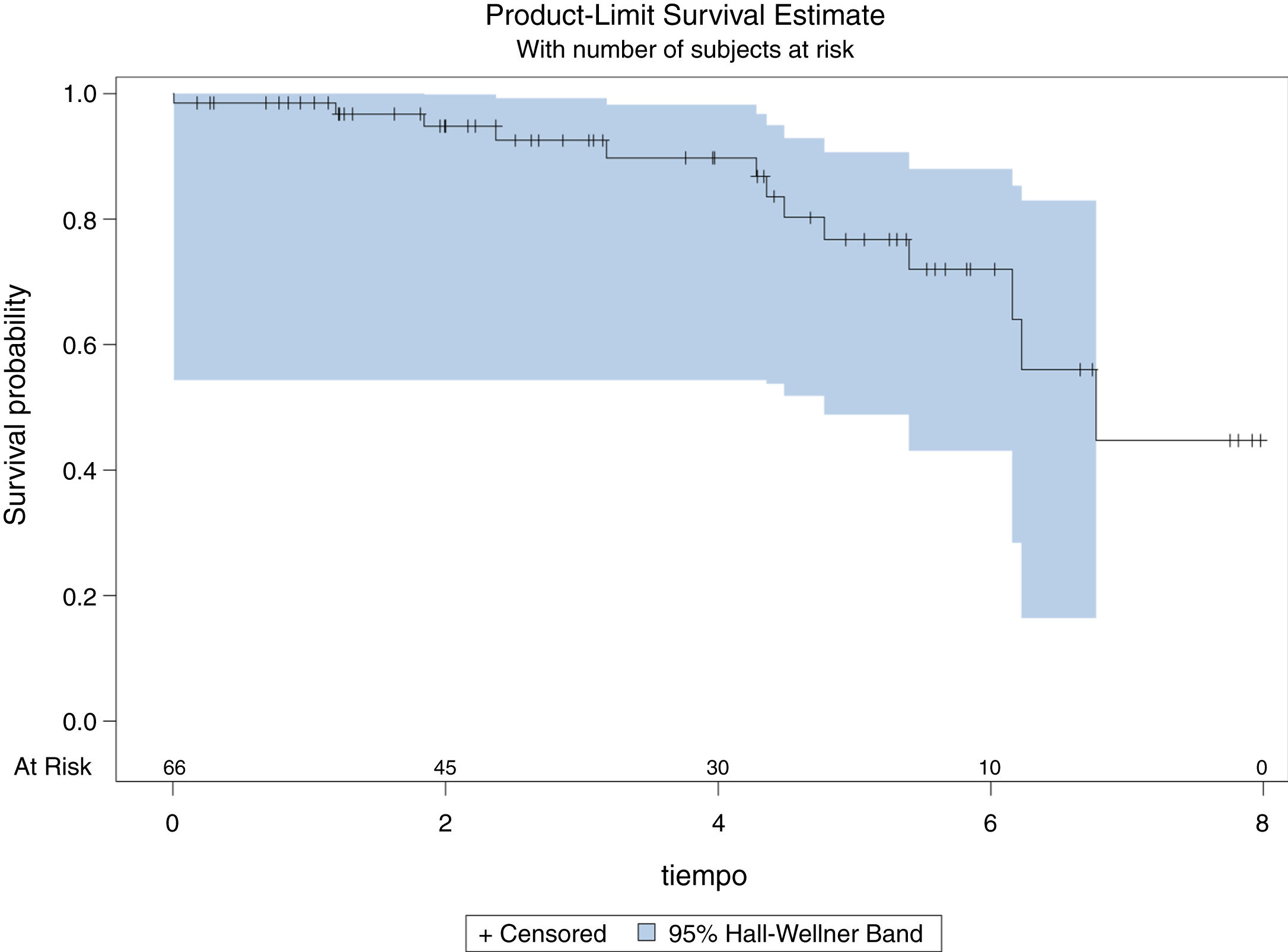
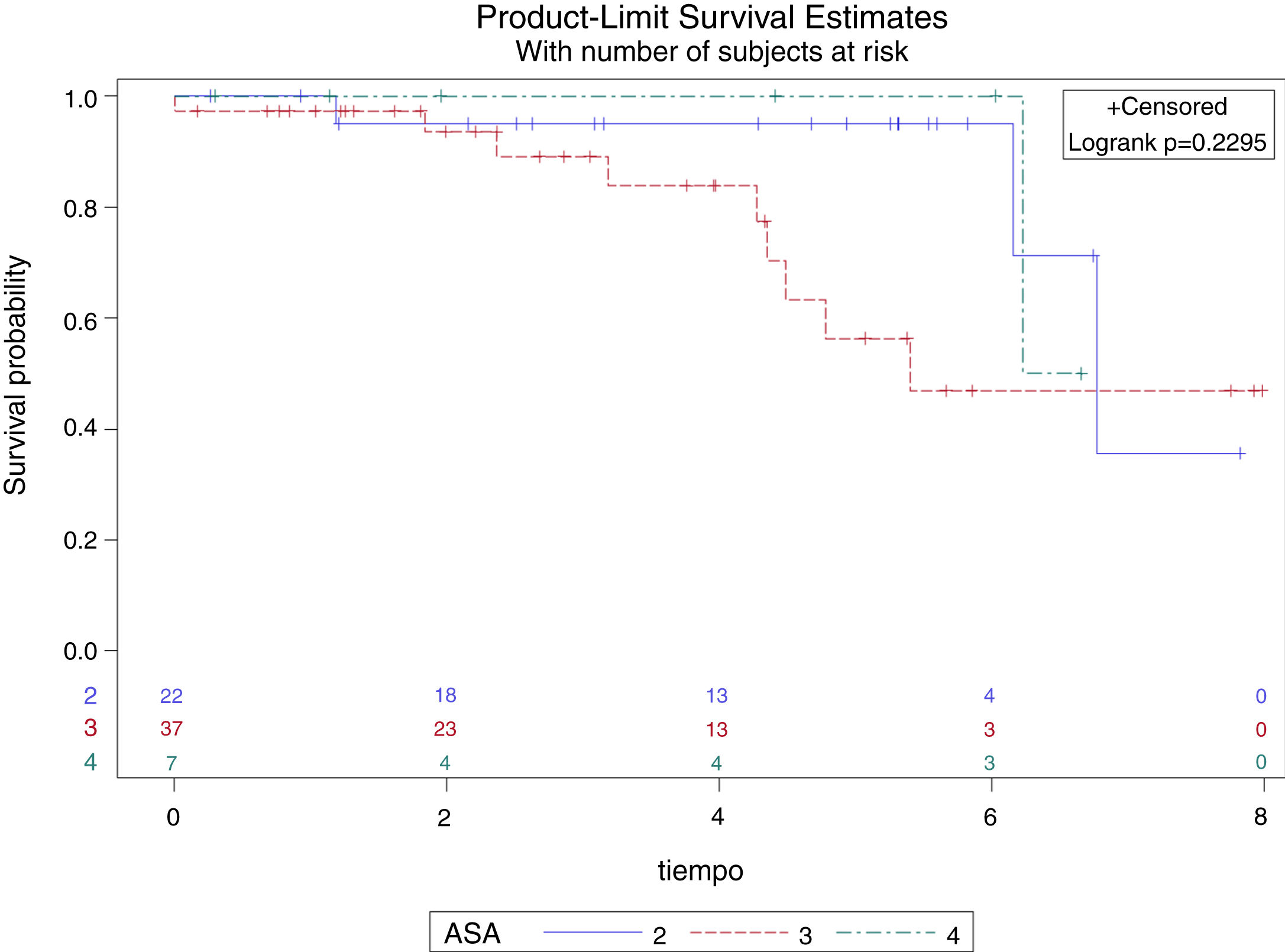
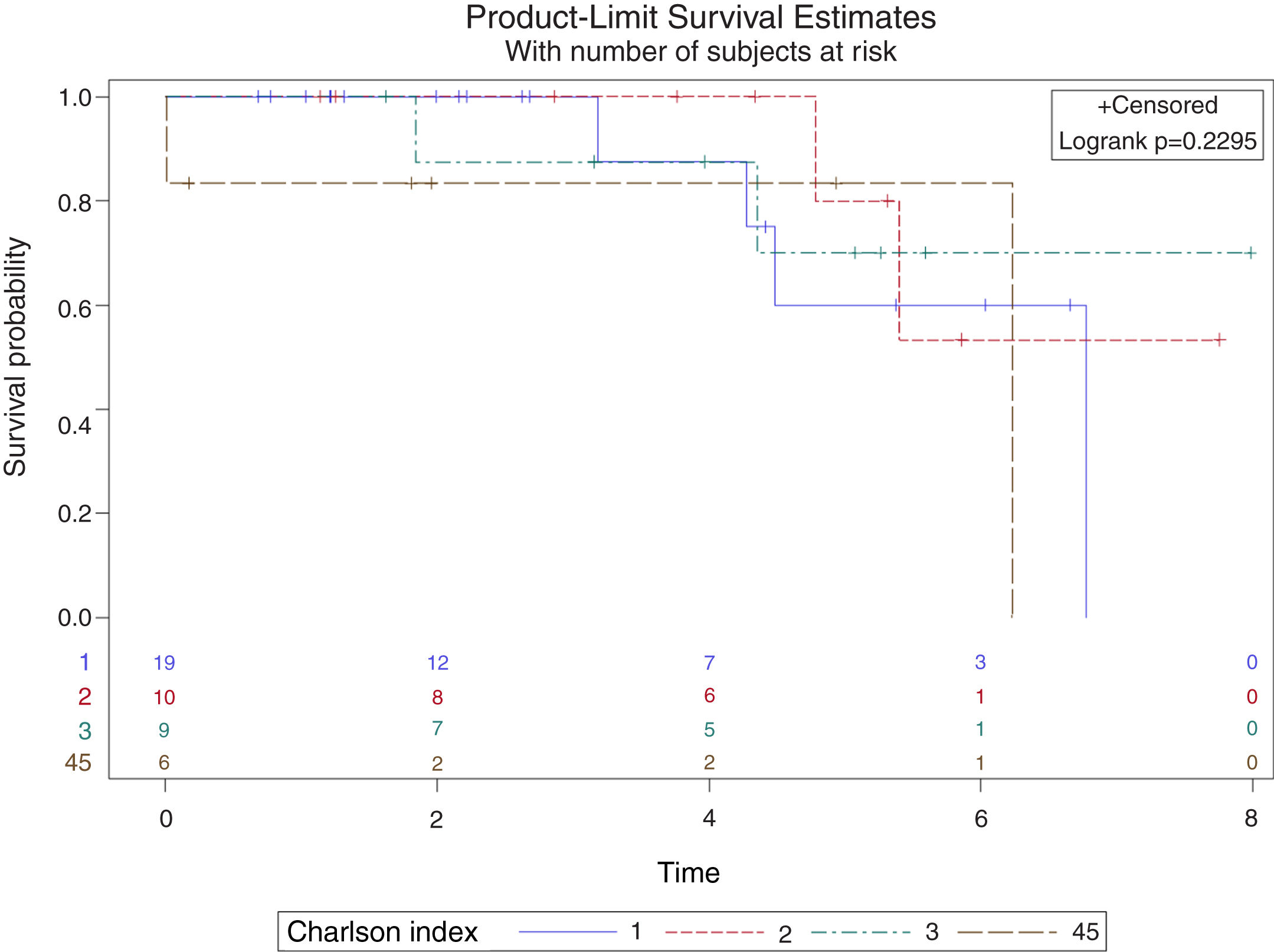
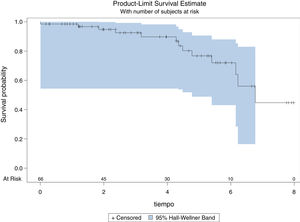
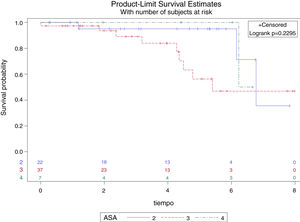
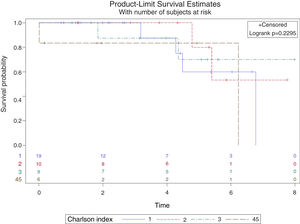
ResultsWe included 66 patients, 40 women and 26 men with a mean age of 87.22 years, of whom 15 had high comorbidity (Charlson> 2). Only 14 patients presented complications in the postoperative period, the most frequent was the confusional syndrome (5); and the most serious one, a death (1), with a median of admission of 8 days. Two cases of dislocation were detected during a mean follow-up of 3.61 years, without requiring revision surgery. Improvement of pain was evident after surgery (p < 0.0001). The median overall survival is 6.77 years, with no difference in survival adjusted by the Charlson index (p = 0.75) or by ASA anesthetic group (p = 0.23).
ConclusionsWith good patient selection, TCA is a good option for those patients over 85 years of age with functional limitations or pain due to OA.
La población anciana candidata a artroplastia total de cadera (ATC) está aumentando exponencialmente en países desarrollados, por la prevalencia de osteoartrosis (OA). El objetivo es identificar la supervivencia global en pacientes de más de 85 años con OA primaria intervenidos de ATC.
Material y MétodosEstudio observacional retrospectivo en pacientes mayores de 85 años con OA primaria de cadera intervenidos entre 2012 y 2019. Se recogieron variables demográficas, clínicas, de comorbilidad, complicaciones, funcionalidad y dolor. Se realizó un análisis descriptivo y se estimó la supervivencia con el método de Kaplan-Meier y las diferencias en el dolor y la funcionalidad pre y postoperatorias con el test de McNemar-Bowker.
ResultadosSe incluyeron 66 pacientes, 40 mujeres y 26 varones con edad media de 87,22 años, de los que 15 presentaron alta comorbilidad (Charlson >2). Solo 14 pacientes presentaron complicaciones en el postoperatorio, siendo la más frecuente, el síndrome confusional (5); y la de mayor gravedad, un éxitus (1), con una mediana de ingreso de 8 días. Se detectaron 2 casos de luxación durante un seguimiento medio de 3,61 años, sin precisar cirugía de revisión. Se evidenció mejoría del dolor tras la cirugía (p < 0,0001). La mediana de supervivencia global es de 6,77 años, sin diferencias en la supervivencia ajustada por Índice de Charlson (p = 0,75) o grupo anestésico ASA (p = 0,23).
ConclusionesCon una buena selección del paciente, la ATC es una buena opción en mayores de 85 años con limitaciones funcionales o dolor por OA.
The elderly population in developed countries has increased over recent decades due to the increase in life expectancy.1 According to the Instituto Nacional de Estadística overall life expectancy in Spain amounts to 83.19 years.2 The group of those aged 85 or more years old, corresponding to more than 1.5 million individuals in spain,3 has increased exponentially, leading to the coining of terms such as the “old-elderly” or the “fourth age”.4 A growing number of patients aged 85 years or older will be candidates for total hip arthroplasty (THA) in the coming years, because of the higher incidence of hip osteoarthrosis (OA) in the elderly.5,6
Although THA has been proven to improve pain, mobility and quality of life in patients with coxarthrosis,5 few studies of elderly groups are available, particularly those over the age of 85 years. They are usually papers with small sample sizes, or ones that do not distinguish between primary hip surgery6 vs. hip revision surgery or hip vs. knee arthroplasty.7 Age was thought to be a relative surgical contraindication for years, due to increased medical comorbidity and the short life expectancy of elderly patients.8 Nevertheless, the latest studies recommend that surgery should not be ruled out solely because of age, as the preoperative conditions of each patient should be evaluated on an individual basis.9 In fact, one study shows that THA in patients above the age of 80 years has more benefits than it does in younger age groups.10
Our chief aim is to identify overall survival and survival adjusted for comorbidity in patients aged 85 years or more, operated for THA due to primary OA. The secondary objective was to evaluate the prevalence of adverse events during hospitalisation, as well as during the out-patient follow-up of patients above the age of 85 years operated for THA.
Material and methodsThis is a retrospective observational study. The inclusion criterion was subjects aged 85 years or more with primary hip OA operated for THA, according to the classification “Total hip replacement”, (9th version of the International Classification of Diseases, CID 9 MC) in the electronic clinical history (ECH) system from 1 January 2012 to 31 December 2019. The year 2012 was chosen as the study start date to facilitate patient data access and gathering, as it was in this year that the ECH system was implemented in our hospital.
The procedures were carried out by 7, experienced orthopaedic surgeons in the hip unit. All of the patients followed the general THA protocol available in our hospital to ensure suitable pre-anaesthetic assessment, multidisciplinary care during hospitalisation, (orthopaedic surgery, rehabilitation and, in this age group, geriatric care) together with appropriate follow-up as, out-patients. Patients with a cause other than primary hip OA were excludedgeriatric care), such as, intracapsular fractures or OA secondary to the sequelae of previously diagnosed diseases (developmental hip dysplasia, Perthes’ disease or avascular necrosis due to the chronic ingestion of glucocorticoids), or those who had been subjected to a second surgical operation or THA revision surgery. Authorisation was requested from the clinical research ethics committee, this was received on February 25, 2020, for this project.
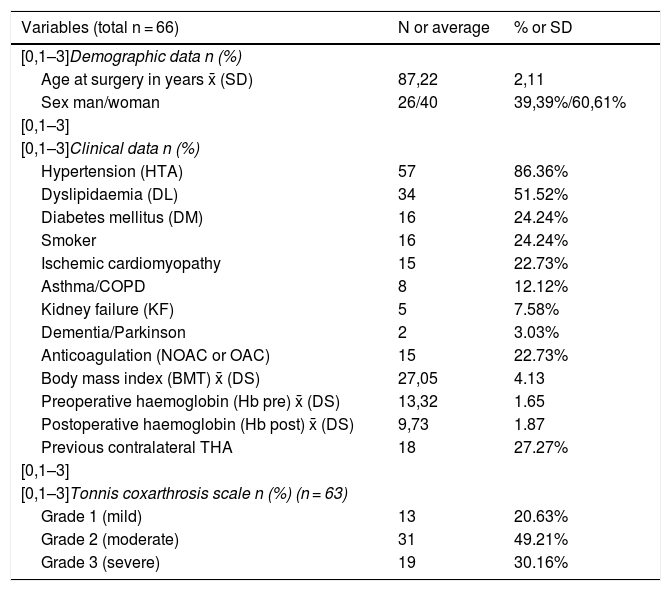
Tables 1–3 show the demographic variables (sex, age at the moment of surgery, current age, life-stage and date of death), clinical data (cardiovascular risk factors, systemic diseases, body mass index, anticoagulation and previous contralateral THA), analytical data (haemoglobin before and after surgery) radiological data (hip arthrosis Tonnis scale11), preoperative comorbidity (the anaesthesia scale of the American Society of Anaesthesiology [ASA] and the abbreviated version of the Charlson index),12 perioperative data (type of anaesthesia, laterality, surgical approach, prosthesis model and cementation) and patient monitoring before and after the operation (the need for transfusion, duration of hospitalisation, destination after discharge, functionality before and after surgery in terms of the possibility of walking, pain before and after surgery standardised on the WHO analgesic scale,13 medical and surgical complications during hospitalisation, and surgical complications during out-patient follow-up).
Description of the demographic, clinical, analytical and radiological data of the patients included in the study.
| Variables (total n = 66) | N or average | % or SD |
|---|---|---|
| [0,1–3]Demographic data n (%) | ||
| Age at surgery in years x̄ (SD) | 87,22 | 2,11 |
| Sex man/woman | 26/40 | 39,39%/60,61% |
| [0,1–3] | ||
| [0,1–3]Clinical data n (%) | ||
| Hypertension (HTA) | 57 | 86.36% |
| Dyslipidaemia (DL) | 34 | 51.52% |
| Diabetes mellitus (DM) | 16 | 24.24% |
| Smoker | 16 | 24.24% |
| Ischemic cardiomyopathy | 15 | 22.73% |
| Asthma/COPD | 8 | 12.12% |
| Kidney failure (KF) | 5 | 7.58% |
| Dementia/Parkinson | 2 | 3.03% |
| Anticoagulation (NOAC or OAC) | 15 | 22.73% |
| Body mass index (BMT) x̄ (DS) | 27,05 | 4.13 |
| Preoperative haemoglobin (Hb pre) x̄ (DS) | 13,32 | 1.65 |
| Postoperative haemoglobin (Hb post) x̄ (DS) | 9,73 | 1.87 |
| Previous contralateral THA | 18 | 27.27% |
| [0,1–3] | ||
| [0,1–3]Tonnis coxarthrosis scale n (%) (n = 63) | ||
| Grade 1 (mild) | 13 | 20.63% |
| Grade 2 (moderate) | 31 | 49.21% |
| Grade 3 (severe) | 19 | 30.16% |
Data expressed as n (%) or average (Standard Deviation [SD]).
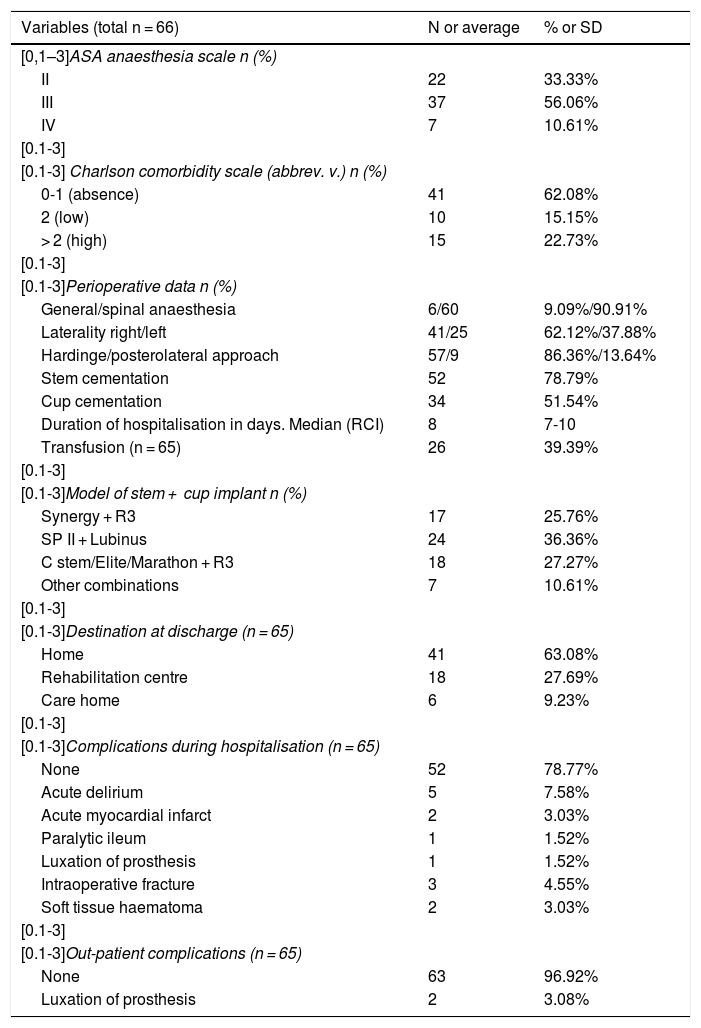
Description of preoperative comorbidity, perioperative and follow-up data of the patients included in the study.
| Variables (total n = 66) | N or average | % or SD |
|---|---|---|
| [0,1–3]ASA anaesthesia scale n (%) | ||
| II | 22 | 33.33% |
| III | 37 | 56.06% |
| IV | 7 | 10.61% |
| [0.1-3] | ||
| [0.1-3] Charlson comorbidity scale (abbrev. v.) n (%) | ||
| 0-1 (absence) | 41 | 62.08% |
| 2 (low) | 10 | 15.15% |
| > 2 (high) | 15 | 22.73% |
| [0.1-3] | ||
| [0.1-3]Perioperative data n (%) | ||
| General/spinal anaesthesia | 6/60 | 9.09%/90.91% |
| Laterality right/left | 41/25 | 62.12%/37.88% |
| Hardinge/posterolateral approach | 57/9 | 86.36%/13.64% |
| Stem cementation | 52 | 78.79% |
| Cup cementation | 34 | 51.54% |
| Duration of hospitalisation in days. Median (RCI) | 8 | 7-10 |
| Transfusion (n = 65) | 26 | 39.39% |
| [0.1-3] | ||
| [0.1-3]Model of stem + cup implant n (%) | ||
| Synergy + R3 | 17 | 25.76% |
| SP II + Lubinus | 24 | 36.36% |
| C stem/Elite/Marathon + R3 | 18 | 27.27% |
| Other combinations | 7 | 10.61% |
| [0.1-3] | ||
| [0.1-3]Destination at discharge (n = 65) | ||
| Home | 41 | 63.08% |
| Rehabilitation centre | 18 | 27.69% |
| Care home | 6 | 9.23% |
| [0.1-3] | ||
| [0.1-3]Complications during hospitalisation (n = 65) | ||
| None | 52 | 78.77% |
| Acute delirium | 5 | 7.58% |
| Acute myocardial infarct | 2 | 3.03% |
| Paralytic ileum | 1 | 1.52% |
| Luxation of prosthesis | 1 | 1.52% |
| Intraoperative fracture | 3 | 4.55% |
| Soft tissue haematoma | 2 | 3.03% |
| [0.1-3] | ||
| [0.1-3]Out-patient complications (n = 65) | ||
| None | 63 | 96.92% |
| Luxation of prosthesis | 2 | 3.08% |
Data are expressed as n (%), average (standard deviation) or median (Interquartile range).
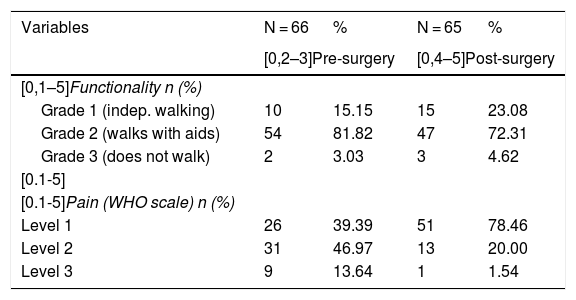
Description of functionality and pain data before and after surgery of the patients included in the study.
| Variables | N = 66 | % | N = 65 | % |
|---|---|---|---|---|
| [0,2–3]Pre-surgery | [0,4–5]Post-surgery | |||
| [0,1–5]Functionality n (%) | ||||
| Grade 1 (indep. walking) | 10 | 15.15 | 15 | 23.08 |
| Grade 2 (walks with aids) | 54 | 81.82 | 47 | 72.31 |
| Grade 3 (does not walk) | 2 | 3.03 | 3 | 4.62 |
| [0.1-5] | ||||
| [0.1-5]Pain (WHO scale) n (%) | ||||
| Level 1 | 26 | 39.39 | 51 | 78.46 |
| Level 2 | 31 | 46.97 | 13 | 20.00 |
| Level 3 | 9 | 13.64 | 1 | 1.54 |
Data are expressed as n (%).
All of the above-mentioned variables were obtained from the different sources of information available in the ECH, including the pre-anaesthesia report, the hospital admission report. The surgical protocol and implementation sheet, the intraoperative anaesthesia protocol and the remarks on evolution in out-patient visits. The patients were followed up, with check-ups scheduled for the 1st, 3rd, 6th and 12th months, as well as annual check-ups after the second year. All of the patients were examined (n = 66) in March 2020, with a minimum follow-up time of 6 months. In the case of those patients for whom no recent information was available about their health or potential postoperative complications due to the loss of out-patient monitoring (n = 12), a search for information was undertaken in the HORUS data platform of Madrid Health Service.
All of the patients were given the antibiotic prophylaxis stipulated by the infection commission protocol: 2 g IV cefazolin in the operating theatre (30 min beforehand), repeating 3 more doses of 1 g IV cefazolin every 8 h after the first dose, except in cases of allergy to betalactamic drugs, administering 1 g IV vancomycin in the ward (1 h beforehand), repeating 2 doses more of 1 g IV vancomycin every 12 h after the first dose. Blood transfusion criteria were set at a range below 8–8.5 Hb. If the patient had no cardiac pathology 2 erythrocyte concentrates were administered, accompanied by ½ an ampule of 40 mg furosemide when the figure was below 8–8.5 Hb, although the threshold may be higher if there are symptoms (dizziness, palpitations…) or haemodynamic repercussions (hypotension, tachycardia…). To prevent the risk of transfusion in elective surgery Hb was optimised prior to surgery and before admission, if the anaesthetist considered this advisable.
The study variables were subjected to a descriptive analysis. Continuous quantitative variables are expressed as an average with standard deviation (SD) or as a median and interquartile range, depending on whether or not normal distribution could be assumed. The Kolmogorov-Smirnov normalcy test was used to evaluate the said assumption. Categorical variables are expressed as absolute frequencies (n) and relative frequencies (%). Respecting the sample size, the incidence of subjects who fulfilled the inclusion criteria was estimated to stand at 8–9 patients/year, so that recruitment of 64–72 subjects during the study duration (8 years) was foreseen.
The Kaplan-Meier method was used to estimate overall survival as well as survival according to ASA group and the Charlson index. The median and CI values were obtained by bootstrap analysis. The survival probability distributions of the different ASA and Charlson index groups were compared using the log-rank test. Differences in pain and functionality before and after surgery were tested using the McNemar-Bowker test. Changes in haemoglobin between the moments before and after surgery were studied using the Student t-test for associated samples. Changes in haemoglobin throughout the follow-up comparing the group of subjects who received a transfusion and the group who did not were studied using an ANOVA of repeated measurements with an intersubject factor. The relationship between categorical anticoagulation variables before surgery and the need or not for transfusion was analysed using the chi-squared test. P values < .05 were considered to be statistically significant for all of the analyses.
ResultsSixty-six patients with an average age at the moment of surgery of 87.22 (SD: 2.11) years were included, of which 26 (39.39%) were men and y 40 (60.61%) were women. Their clinical, analytical and radiological data are shown in Table 1. The most common cardiovascular risk factors and the most prevalent diseases were hypertension (83.36%), dyslipidaemia (51.52%), diabetes mellitus (24.24%), smoking (24.24%) and ischemic cardiomyopathy (22.73%). Their average body mass index was 27.05 kg/m2 (SD: 4.13) and average preoperative haemoglobin was 13.32 g/dl (SD: 1.65). A total of 15 (22.73%) patients were taking acenocumarol or new oral anticoagulants, 18 (27.27%) had a contralateral THA and 50 (79.37%) had moderate (type 2) or severe (type 3) degrees of coxarthrosis on the Tonnis scale. In 3 patients it was not possible to access preoperative X-ray images to evaluate their degree of arthrosis.
The most relevant preoperative, perioperative and follow-up comorbidity data are shown in Table 2. According to the ASA anaesthesia scale, 22 (33.33%) patients were classified as ASA II, 37 (56.06%) as ASA III and 7 (10.61%) as ASA IV. 62.12% (41 subjects) had low level comorbidity (score 0 o 1), while 15 (22.73%) had high level comorbidity (score 3 or higher), according to the abbreviated Charlson index. Spinal anaesthesia was the most widely used form of anaesthesia, in up to 60 (90.91%) of patients, and Hardinge’s approach was used in 57 (83.36%) of patients. 41 (62.12%) right hips and 25 (37.88%) left hips were operated. 52 stems were cemented (78.79%) as were 34 (51.54%) cups which, when combined, give 34 (51.51%) completely cemented prostheses and 18 (27.27%) hybrid prostheses. Respecting the model of prosthesis, 17 (25.76%) were Synergy stems with a R3 (S&N) cup, 24 (36.36%) were cemented Lubinus cups with a cemented SP II stem (Waldemar Link) and 18 (27.27%) consisted of a cemented C-stem (J&J), Élite (J&J) o Marathon (S&N) with an uncemented R3.
78.79% of patients had no complications during hospitalisation. However, 8 (12.13%) had a medical complication: 5 acute delirium, 2 acute myocardial infarcts and one paralytic ileum. One death was recorded on the 3rd day after the operation, in the context of a patient with acute hypoactive delirium. None suffered a urine or lower respiratory infection, pulmonary embolism or deep vein thrombosis during hospitalisation. The other 6 (9.1%) had a complication associated with the surgical intervention, including one prosthetic luxation that was treated with closed reduction and conservative management with abduction orthosis, 2 soft tissue haematomas that did not require drainage and 3 intraoperative fractures (2 fractures of the greater trochanter during insertion of the cemented stem, which were resolved using cerclages in the same surgical operation, and one fracture of the anterior acetabulum rim during implantation of the uncemented cup, which required no additional treatment). No patient had an infection of the surgical wound.
Hospitalisation in a ward lasted for a median time of 8 (RCI 7−10) days, and 41 (63.08%) of the patients returned home after discharge. The postoperative average haemoglobin was 9.73 g/dl (SD: 1.87), and in 26 (39.39%) patients it was necessary to transfuse one or two erythrocyte concentrates, with levels in this subgroup below 8.7 Hb in all cases. Hb preoperative optimisation with iron was only recorded in 3 patients (4.54%). Changes in haemoglobin from the moment before surgery to the moment afterwards were –3.59 g/dl (SD: 2.02), which was statistically significant (P < .0001). Study of the changes in Hb during the follow-up period (before and after surgery) which compared the group of subjects who received a transfusion (–5.057 Hb) and the groups of subjects who received no transfusion (–2.637 Hb), showed differences between both groups (P < .0001). However, no association was found between anticoagulation and the need for transfusion, as 23.08% of the patients who required transfusion were anticoagulated. This figure is very similar (22.50%) in the case of the patients who did not need a transfusion (P = .9564).
Two THA luxations that had been implanted using a posterolateral approach stand out as complications during the postoperative out-patient follow-up. One case was treated by closed reduction and abduction orthosis, while closed reduction was not used in the other because of the poor general condition of the patient, so it remained as a deep-rooted prosthetic luxation that was clinically well-tolerated. Thus 96.92% of cases had no surgery-associated complications during the follow-up time. There were no cases of septic or aseptic prosthesis loosening.
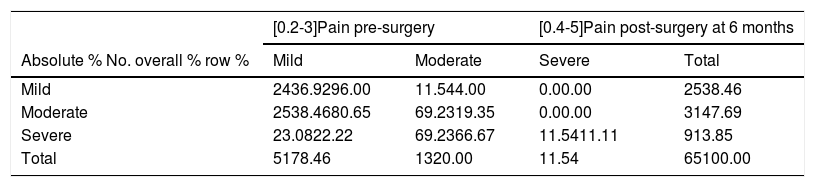
Patient distribution according to degree of pain on the WHO analgesic scale (Table 3) prior to surgery is 39.39% with mild pain, 46.97% with moderate pain and 13.64% with intense pain. After the operation 51 patients (78.46%) had adequate pain control without the need for opiates (level 1), while only one (1.54%) required stronger opiates (level 3). Statistically significant differences according to the McNemar-Broker test were found in the distribution of pain before and after surgery, at 6 months. 25 subjects (80.65%) with moderate pain discontinued the use of weak opiates, passing to the first analgesic level or mild pain (P < .0001). Likewise, 8 patients with intense pain discontinued the use of stronger opiates (third level), as 2 of them passed to the first level (22.22%) and the other 6 (66.67%) passed to the second level, with a statistical significance of P = .047 (Table 4).
Analysis of differences in pain before and after surgery, using the McNemar-Bowker test.
| [0.2-3]Pain pre-surgery | [0.4-5]Pain post-surgery at 6 months | |||
|---|---|---|---|---|
| Absolute % No. overall % row % | Mild | Moderate | Severe | Total |
| Mild | 2436.9296.00 | 11.544.00 | 0.00.00 | 2538.46 |
| Moderate | 2538.4680.65 | 69.2319.35 | 0.00.00 | 3147.69 |
| Severe | 23.0822.22 | 69.2366.67 | 11.5411.11 | 913.85 |
| Total | 5178.46 | 1320.00 | 11.54 | 65100.00 |
| Losses = 1 | |
|---|---|
| Adjusted P value | |
| Mild pre/mild post: severe pre/severe post | .5 |
| Mild pre/mild post: mod. pre/mod. post | < .0001 |
| Severe pre/severe post: mod. pre/mod. post | .047 |
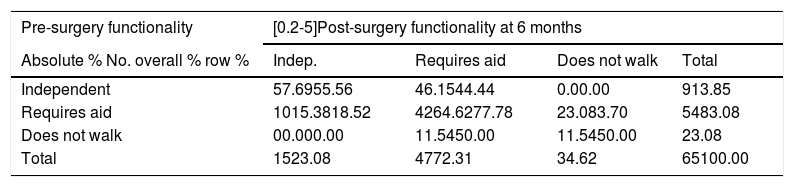
Pre-and post-surgery functionality was analysed based on the possibility of walking. 54 patients (81.82%) walked with aids (sticks, a frame or the support of a person) before surgery. At 6 months after the surgical operation only 47 (72.31%) patients walked with aids, and 15 (23.08%) walked unaided. Nevertheless, no statistically significant differences were found according to the McNemar-Broker test (Tables 3 and 5).
Analysis of differences in functionality according to ability to walk before and after surgery using the McNemar-Bowker test.
| Pre-surgery functionality | [0.2-5]Post-surgery functionality at 6 months | |||
|---|---|---|---|---|
| Absolute % No. overall % row % | Indep. | Requires aid | Does not walk | Total |
| Independent | 57.6955.56 | 46.1544.44 | 0.00.00 | 913.85 |
| Requires aid | 1015.3818.52 | 4264.6277.78 | 23.083.70 | 5483.08 |
| Does not walk | 00.000.00 | 11.5450.00 | 11.5450.00 | 23.08 |
| Total | 1523.08 | 4772.31 | 34.62 | 65100.00 |
| Losses = 1 | |
|---|---|
| Adjusted P value | |
| Independent pre/independent post: does not walk pre/does not walk post | 1.00 |
| Independent pre/independent post: requires aid pre/requires aid post | .36 |
| Does not walk pre/does not walk post: requires aid pre/requires aid post | 1.00 |
A total of 53 (80.3%) patients were alive in March 2020, when the study data were reviewed. The median overall survival (p50) is 6.77 years (CI 95%: 6.15752- unknown), and it is not possible to calculate the upper margin due to the lack of events (deaths) during follow-up (Fig. 1). The mortality rate during the first year was 3.03% (2 patients) and the average follow-up duration of the patients is 3.61 years (SD: 2.21). During the follow-up 3 patients with ASA II (13.64%) died, as did 9 patients with ASA (24.32%) and one with ASA IV (14.29%). No statistically significant differences were found in survival according to ASA groups (log rank P = .229), as may be seen in Fig. 2. No statistically significant differences were found in the probability of survival in the groups with different Charlson index scores (log rank P = .749), i.e., greater comorbidity is not associated with a lower rate of patient survival, according to our results (Fig. 3).
As is the case in our study, the majority of published works reflect a higher percentage of women (range 60.29-74.40%)4,5,9 and right hips, such as in the Finnish registry by Ogino et al. (57.6%).1 Hypertension stands out as the most prevalent disease (83.36%), with a range from 45.15 to 76.7% in the other publications.4,6,9 The body mass index was mildly higher (27.05 kg/m2) than a Canadian study of 49 THA in nonagenarians (24.3 kg/m2). In this same study preoperative haemoglobin was 13 g/dl, a figure very similar to ours (13.32 g/dl).5 No relevant papers were found in the bibliographical search which describe the percentage of patients with anticoagulation or their standardised degree of coxarthrosis.
The most numerous ASA classification group of patients corresponded to ASA III (56.06%), which is similar to the finding by Petruccelli et al. (71.8%)5 or Jauregui et al. (64%).14 66.1% of the patients of Miric et al. were classified as ASA III or higher (66.67% in our study), which as is logical, means there was a higher percentage than in groups of younger patients with less comorbidity.6 Spinal anaesthesia was the form used the most often, at 90.91%, and this figure varies widely in the bibliography depending on anaesthetic preferences (from 8.62%7 to 46.46%14).
78.78% of the prostheses had a cemented component. The majority of them use a combination of cemented components, amounting to 51.51% in our study. Ogino et al. showed that based on Finnish arthroplasty registry data that the survival of implants in this age group is shorter for uncemented prostheses, underlining the importance of cementing the femoral component. It has been proven that a higher number complications occur with uncemented implants in elderly patients.1 As a general rule, in our case Dorr A and B type femurs wee operated with a cemented or uncemented implant based on the decision of the surgeon, although type C Dorr were always cemented to achieve optimum fixing of the implant and prevent potential complications (loosening or fracture…).
Nevertheless, geographical differences in the use of models or cementing preferences in Northern vs Southern Europe have to be taken into account.
In the same Finnish registry the model that was used the most often (50.1% vs 36.36% in our study) is the cemented Lubinus cup with an SP II stem (Waldemr Link).1 As can be seen in Table 2, different models of commercially available prosthesis were implanted (more than 15 combinations), which means we have to partially group the table of results to show them in a more summarised form. This high level of variability may be explained by the preferences of the surgeon and, most especially, the lack of hospital competitive bidding in the first years of the study (2012–2015). These hospital awards have led to increased uniformity in implant use, so that now the majority of stems implanted are by Synergy with R3 cups, or SP II stems with Lubinus cups in almost all of the patients (n = 18/19) during the last two years (2018 and 2019).
Our figure of 21.21% of patients with complications during admission is similar to the 25.6% of perioperative complications cited by Petrucelli et al.,5 or the 26% mentioned by Karuppiah et al.7 Other older studies mention a range from 23.8%-46.8% of perioperative medical complications.15,16 Our lower rate of complications, which is similar to those obtained in more recent studies, may be due to the gradual introduction of improvements in the care of these patients by multidisciplinary teams such as ours (orthopaedic surgeons, geriatricians, rehabilitators and social workers …). We believe that such teams are fundamental in preventing and treating potential medical complications during hospitalisation, together with the early rehabilitation of walking in these elderly patients. In any case, the data vary depending on the complications which are included, and in fact some studies differentiate between minor and major complications,14 or between surgical and medical ones,17 so that this hinders the comparison of results.
As was pointed out above, 12.13% of our patients had a medical complication. Wurtz et al. reported 27.5% of medical complications in a group of 46 octogenarians operated for THA,18 and Skinner et al. reported 13.2% in a group of nonagenarians with an average age of 92.18 years.17 Our perioperative mortality rate was 1.52%, which is mildly below the range from 2.1%-6.4% reported in the most recent bibliography.5,9,15 On the other hand, studies over the last two decades have shown a surgical complications rate of from 7% to 10.5%,15,17 which is very similar to the 9.1% of our patients who had surgical complications during hospitalisation.
The median duration of hospitalisation time in a ward was 8 days, which is in the lower margin of the range (7.6–13 days) described in the current literature.4,5,9,17 The most frequent destination at discharge was the patient’s usual home (63.08%), which is similar to the 52% published by Gregory et al.,9 or the 59% published by Berend et al.,16 although this figure varies widely in the literature depending on whether or not there are rehabilitation support centres. We believe that all of these positive figures for the average duration of hospitalisation or intrahospital complications ae due to the good working of the rehabilitation department, and most especially to the geriatric unit which treats patients over the age of 85 years, as this is a differentiating aspect of the general THA protocol in our hospital. Several studies have shown that integrating geriatrics in hospital care reduces the medical complications and duration of admission of elderly patients operated for hip fracture.19,20
96.92% of the patients had no surgery-related complications during out-patient follow-up. No case of periprosthetic fracture, infection of the prosthesis or aseptic loosening was recorded after out-patient follow-up, in spite of the fact that the latter is the most frequent cause of prosthesis revision in elderly patients.1 We believe that this low figure of complications may be explained by the small size of the sample, the shorter life expectancy of the patients which restricts the duration of follow-up, and their reduced functional demand in comparison with younger age groups. Nevertheless, we consider aspects such as antibiotic prophylaxis to be very important to prevent infection of the prosthesis, as well as health education, which offers the patients specific recommendations regarding the safe range of movement of the joint and the prevention of falls, to reduce the risk of luxation or periprosthetic fracture, respectively.
39.39% of the patients received a blood transfusion after surgery, which is below the range of from 55.3%-68% shown in the literature.15,17 In spite of this positive datum, we believe it is important to continue improving hospital protocols which have the aim of reducing postoperative transfusion rates, such as the preoperative optimisation of haemoglobin levels in elderly patients. Jans et al. show an association between preoperative anaemia in elderly patients and the probability of transfusion during their hospitalisation.21 Although our study only found that 3 patients were given iron prior to surgery, other patients may also have received iron in the context of primary care.
There was a –3.59 g/dl difference between haemoglobin levels before and after surgery. Skinner et al. found a difference of–4.01 g/dl Hb respecting the preoperative level in patients above the age of 90 years operated for THA.17 No statistically significant association was found between anticoagulation and the need for transfusion. This is doubtless due to strict compliance with pre-anaesthesia recommendations for the time needed to reverse the effect of oral anticoagulants, and coagulation was tested on the same day as the operation.
Patients were found to reduce their use of analgesics after the intervention, especially major and minor opiates, to go down to a lower level of analgesia, while even if they remained at the same level they reduced their use of analgesic medication such as NSAIDs. This is highly important in the elderly, as OA is a chronic disease that requires indefinite analgesic regimes which have not been studied in clinical trials as they exclude this age group. There are also additional risks for the elderly due to polymedication or kidney failure, so that they sometimes have suboptimum analgesic treatment, with poor pain control.22–24 Dimitriou et al. recently showed that THA in appropriately selected elderly patients improved pain, functionality and quality of life, with low rates of mortality.25
No statistically significant differences were found regarding walking before and after the operation. The 3 established values for this variable involve an excessive simplification of a variable as complex as the functionality of walking. We believe that a larger sample size would have shown the statistical significance of this functional improvement, which was observed clinically in many patients. In fact, 10 patients of the 54 who required help for walking were able to walk independently without the need for sticks. We believe that more patients did not abandon the use of walking sticks for two reasons: the feeling of security they give while walking outside the home, together with other orthopaedic problems such as gonarthrosis or contralateral coxarthrosis.
The median overall survival stands at 6.77 years, which is significantly high for the average of this group of elderly patients (87.22 years), which surpasses the average life expectancy (83.19 years) at birth in Spain.2 This may be explained because these “super-selected” patients with functional limitation and pain due to coxarthrosis are included in the waiting list for surgery because they are generally in good general health and with a lower level of comorbidity than could be expected at their age.6 Karuppiah et al. show that these selected patients have a far longer life expectancy (96.1 years)than the general population in their age group.7
The overall survival rate (82%) is higher than those obtained in the majority of available studies, such as a recent one with a survival rate of 41% 4 years after the operation, with an average age of 91.3 years at the moment of surgery.5 Some older studies from the 1990s show survival rates in patients over the age of 89 years of 70% at 3 years26 or 50% at 5 years.27 The average duration of follow-up time is 3.61 years, one of the longest. Pagnano et al. performed a 3.2 year follow-up15 while Petruccelli et al. did so for 3.8 years5 in nonagenarian patients. The rate of mortality in the first year is 3.03%, which is within the range published for similar studies (1.5%-7.7%).4–7
Respecting the limitations of this study, it is retrospective and has the limitations intrinsic to this type of design. Gathering data on variables by consulting ECH implies that some of them were not properly recorded or had been recorded incompletely or more subjectively, without being able to use standardised scales such as the Harris Hip Score. It was not possible to compare the results for pain or functionality before and after surgery in our sample with those of patients in other others7,16 that used scales (the Harris Hip Score) and which doubled their score at 6 months after THA, showing improved results.
However, the study sample contains enough patients to carry out the corresponding statistical analysis with valid results that are statistically significant in some cases. The distortion in selection of the patients based on comorbidities may be mentioned, as this may mean the sample does not reflect the general characteristics of patients in their age group. That is, it is possible that the sample is not representative. Nevertheless, it does allow us to analyse the parameters of this selected group that are associated with a good postoperative prognosis. Due to all of these considerations we believe that it is important to operate these selected elderly patients with pain and restricted mobility, in the light of the good results and those of other similar studies. Our results, which could be representative at a national level, agree with those published in other hospitals around the world, as we have tried to show.
With respect to the strengths of this study, the long follow-up of the patients may be underlined, with an average of 3.61 years (3 months to 8 years) in a specialised high volume hospital. The maximum time range for patient inclusion is 8 years, which makes it possible to have a homogeneous and updated sample, contrasting with periods of inclusion lasting for 15 or 20 years in some series. The longer this period is, the more patients it is possible to recruit. However, improvements in medicine, anaesthesia and surgical techniques which were introduced during the time during which patients can be included increases the heterogeneity of the sample, and may even lead to changes in the recruitment protocol or the loss of information during data gathering.
ConclusionsTo conclude, in our study we demonstrated that THA must be considered in elderly patients over the age of 85 years as a solution to reduce their pain and achieve a higher quality of life, with greater independence and functionality. Age should not be an exclusion criterion or an absolute contradiction, but rather each patient should be evaluated individually to see whether the benefit of the intervention counterbalances its risks. Further prospective studies with large sample sizes are required to determine the risk factors and clinical profile with greater exactitude, to establish a specific protocol for this group of patients.
Level of evidenceLevel of evidence iii.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank Carmen Romero Ferreiro of the Unidad de Investigación y Soporte Científico del Instituto de investigación –imas12– CIBERESP.
Please cite this article as: Gómez Alcaraz J, Pardo García JM, Sevilla Fernández J, Delgado Díaz E, Moreno Beamud JA. Artroplastia total primaria de cadera en pacientes mayores de 85 años: riesgos, complicaciones y resultados a medio-largo plazo. Rev Esp Cir Ortop Traumatol. 2021;65:13–23.