Traumatic hip dislocations can have devastating complications such as osteoarthritis or osteonecrosis. The aim of this study was to identify the variables and prognostic factors associated with clinical and radiological outcome after a traumatic hip dislocation at long-term follow-up.
Material and methodsA review was performed of all dislocations and fracture-dislocations of the hip from January 1999 to December 2012. A computed tomography scan was performed after reduction in all cases. The Harris Hip Score and modified Merle-d’Aubigné–Postel method were used for clinical evaluation and radiological assessment was performed according to the Thompson and Epstein classification.
ResultsThere were 30 cases in 29 patients with a mean follow-up of 11 years (range, 4–17). The great majority were simple dislocations (21; 70%) vs. complex dislocations (9; 30%). Closed reduction was performed in less than 6h in all except one case (29; 96.7%). All of the patients with simple dislocations had an excellent outcome without radiological signs of osteoarthritis at the end of the follow-up (p<0.01). Overall, arthritic signs had developed in 4 patients (13.3%) and avascular necrosis was noted in 3 patients (10%). Five patients with intraarticular fragments were treated non-operatively, and 3 of them developed arthritic changes (p<0.05).
ConclusionOur study suggests that complex dislocations are associated with poorer functional and radiological outcomes than simple dislocations. We also found a strong association between intraarticular fragments and osteoarthritis, so surgical fragment removal could be considered in these cases.
Las luxaciones o fracturas-luxaciones de la cadera pueden suponer severas complicaciones como la artrosis o la necrosis. El objetivo de este estudio fue identificar las variables y los factores pronósticos asociados con resultados clínicos y radiológicos a largo plazo tras una luxación traumática de cadera.
Material y métodosSe realizó un estudio retrospectivo de todas las luxaciones y fracturas-luxaciones tratadas desde enero de 1999 a diciembre de 2012. Una tomografía axial computerizada fue realizada tras la reducción en todos los casos. Para la evaluación de los resultados clínicos se utilizó el Harris Hip Score y la escala Merlé-d’Aubigné–Postel, mientras que los resultados radiológicos se evaluaron con la clasificación de Thompson–Epstein.
ResultadosSe identificaron 30 casos en 29 pacientes, con un seguimiento medio de 11 años (rango 4–17). Existió una mayor frecuencia de luxaciones simples (21; 70%) respecto a luxaciones complejas (9; 30%). Se realizó una reducción cerrada en menos de 6h en todos los casos excepto en uno (29; 96,7%). Todos los pacientes con luxaciones simples tuvieron excelente resultado sin signos radiológicos de artrosis al final del seguimiento (p<0,01). Del total de la muestra, 4 pacientes desarrollaron signos artrósicos (13,3%) y 3 pacientes presentaron necrosis avascular (10%). Cinco pacientes con fragmentos intraarticulares fueron tratados de forma conservadora, y 3 de ellos desarrollaron artrosis (p<0,05).
ConclusiónNuestro estudio muestra que las luxaciones complejas tienen peores resultados funcionales y radiológicos que las luxaciones simples. Hemos encontrado una fuerte asociación entre cuerpos libres intraarticulares y artrosis, por lo que la extracción de esos fragmentos podría ser considerada.
The hip joint is highly intrinsically stable due to the bone anatomy and soft tissues that form it, therefore, it requires high-energy trauma to dislocate. For this reason, patients with this sort of injury must be thoroughly assessed to identify associated craniofacial, chest, abdomen, spine and lower limb problems. Traumatic dislocation of the hip can have severe complications that include osteonecrosis, post-traumatic arthrosis, heterotopic ossifications, sciatic nerve injuries and other musculoskeletal injuries. This lesion is an orthopaedic emergency, and must be promptly diagnosed and reduced.
Various prognostic factors have been described, including the time interval between the injury and reduction, joint congruence, the type of dislocation, stability after reduction and associated injuries.1–3 Although timely reduction is considered one of the most important factors, there is no consensus as to the time interval that might result in complications. Some authors have demonstrated fewer complications after emergency reduction (under 24h),1–4 while others papers have not demonstrated time to have an effect.5,6
The objective of this study was to identify the variables and prognostic factors associated with long-term clinical and radiological outcomes after traumatic dislocation of the hip.
Material and methodsA retrospective study was undertaken of all the hip dislocations and hip fracture-dislocations treated in our centre from January 1999 to December 2012. The inclusion criteria were a complete clinical and radiological history, patients with skeletal maturity and a minimum follow-up of 4 years. Patients with intellectual disabilities and therefore unable to answer the functional questionnaires were excluded, as were pathological fractures. Written informed consent was obtained in all cases. The patients’ demographic data, mechanism of injury, type of dislocation and time of reduction and associated injuries and comorbidity were recorded. The Injury Severity Score (ISS) was used to assess the severity of multiple injuries,7 since polytraumatised patients have a poorer associated prognosis.4,5 Our radiological protocol included an anteroposterior radiography of the pelvis and oblique Judet views (alar and obturator) if an acetabular fracture was suspected. Computerised axial tomography (CAT) was performed in all cases. The hip dislocations were classified as simple (pure dislocation with no associated fracture) and complex (associated with acetabular or head of femur fracture). They were divided into anterior or posterior dislocations, depending on the anatomical position of the femoral head. The posterior dislocations were categorised using Thompson–Epstein's8 classification and the anterior dislocations with Epstein's classification.9 Both classifications were described specifically to define the dislocation according to its posterior or anterior direction. Pipkin's10 classification was used to assess femoral head fractures and the system proposed by Stewart and Milford was used to describe stability after reduction.11
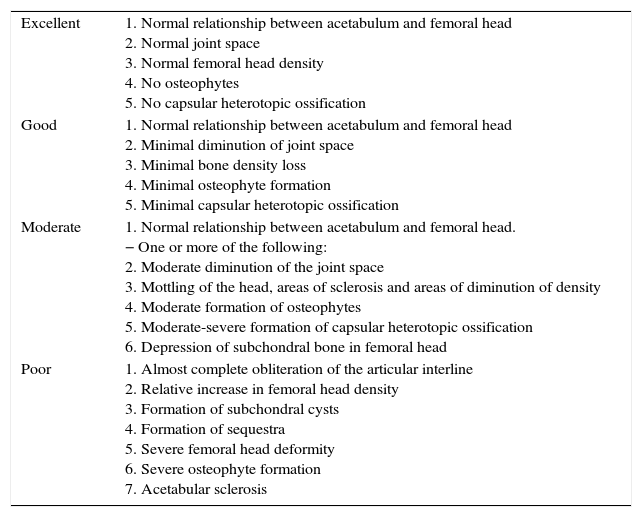
A clinical assessment was undertaken at the last follow-up session consisting of a physical examination and anterior–posterior and axial hip X-rays, which were analysed by two of the authors (X.F. and A.S.). The clinical outcomes were assessed using the Harris Hip Score (HHS)12 and Merlé-d’Aubigné–Postel's modified method.13 The radiological outcomes were analysed using Thompson–Epstein's5 classification (Appendix 1), Tönnis’ classification to assess the grade of arthrosis14 and Brooker's classification for the periarticular heterotopic ossifications.15 Steinberg's classification was used to quantify the degree of avascular necrosis of the femoral head.16 We tried to identify other complications, such as instability or recurrent dislocation, infection, haematoma, neurovascular lesions, deep vein thrombosis and mortality.
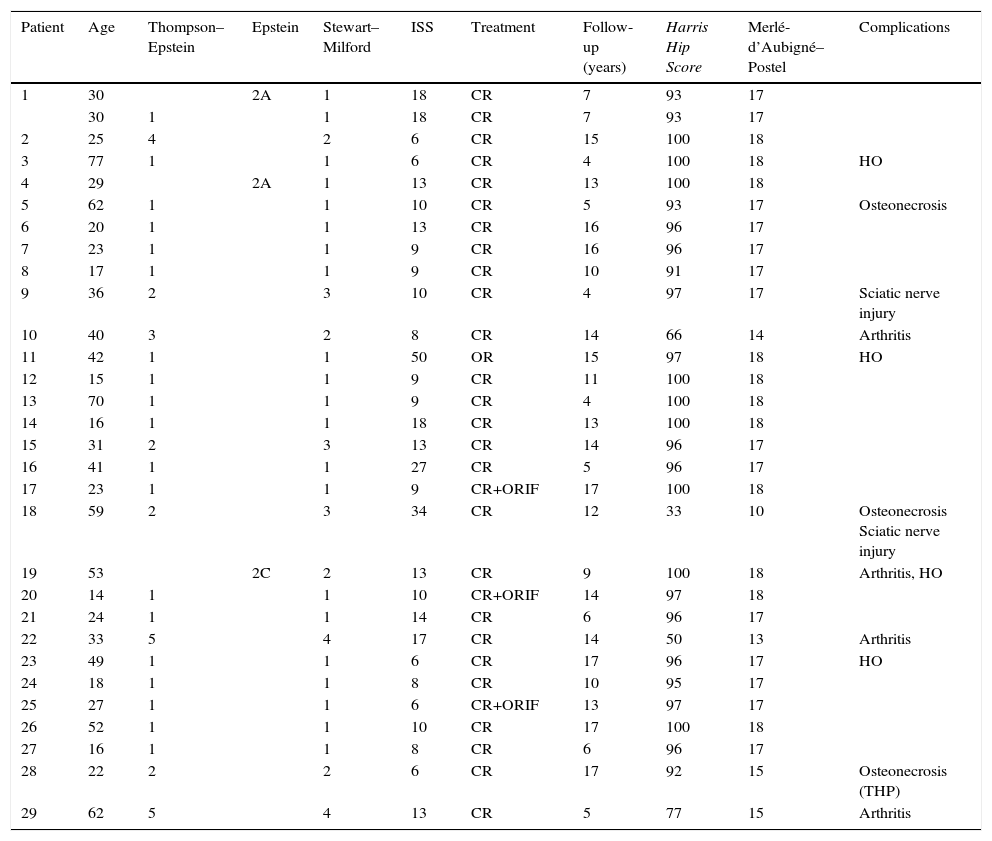
A total of 39 patients with 40 traumatic hip dislocations were identified. Six patients were excluded due to an incomplete clinical history or insufficient follow-up. Two patients died from unrelated diseases and one patient with a hip fracture-dislocation associated with a pathological injury, therefore a final analysis was made of 30 dislocations in 29 patients (Appendix 2).
A statistical analysis was performed of the sample, calculating frequencies and percentages of the categorical variables and the mean and standard deviation (or median and interquartile ranges) for the continuous variables. The Chi-squared test (or Fisher's exact test) was used to evaluate the relationship between possible associated factors and the clinical and radiological results. The non-parametric Wilcoxon and Kruskal–Wallis tests were also used. All these statistical analyses were undertaken using SAS 9.4 and a p value <0.05 was considered statistically significant.
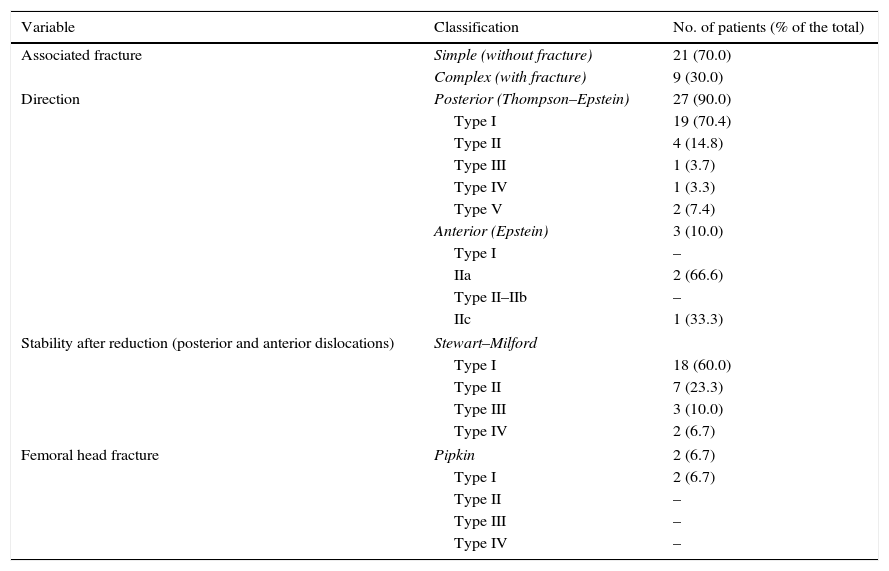
ResultsOf the 29 patients, there were 20 males and 9 females and the mean age at the time of the injury was 35 years (range, 14–77 years). The mean follow-up was 11 years (range, 4–17 years). The most common mechanism of injury was a traffic accident (20; 66.7%), followed by sports accidents (4; 13.3%), falls from a height (3; 10%) and low-energy trauma (3; 10%). Excluding the patients with low-energy trauma, the mean ISS was 13.5 points (range, 6–50 points). The majority of the dislocations were posterior (27; 90%) and only 3 were anterior (10%). In terms of associated fractures, 21 cases (70%) were simple dislocations and 9 (30%) complex dislocations, i.e., with associated fractures of the acetabulum or femoral head. The most common type of fracture was of the posterior wall (5 cases), followed by femoral head fractures (2 cases), one transverse fracture of the acetabular roof and one fracture of the anterior wall. The distribution of the sample according to the various classification systems used is shown in Table 1. In all of the patients, except one, it was possible to perform a prompt closed reduction in under 6h (29; 96.7%). The exception was a patient who required open reduction due to an irreducible dislocation, the CT scan revealed several acetabular fragments and interposition of soft tissue. This patient was treated 16h after the initial trauma using the Kocher–Langenbeck approach, removing the intra-articular fragments.
Classification of hip dislocations and fracture-dislocations.
| Variable | Classification | No. of patients (% of the total) |
|---|---|---|
| Associated fracture | Simple (without fracture) | 21 (70.0) |
| Complex (with fracture) | 9 (30.0) | |
| Direction | Posterior (Thompson–Epstein) | 27 (90.0) |
| Type I | 19 (70.4) | |
| Type II | 4 (14.8) | |
| Type III | 1 (3.7) | |
| Type IV | 1 (3.3) | |
| Type V | 2 (7.4) | |
| Anterior (Epstein) | 3 (10.0) | |
| Type I | – | |
| IIa | 2 (66.6) | |
| Type II–IIb | – | |
| IIc | 1 (33.3) | |
| Stability after reduction (posterior and anterior dislocations) | Stewart–Milford | |
| Type I | 18 (60.0) | |
| Type II | 7 (23.3) | |
| Type III | 3 (10.0) | |
| Type IV | 2 (6.7) | |
| Femoral head fracture | Pipkin | 2 (6.7) |
| Type I | 2 (6.7) | |
| Type II | – | |
| Type III | – | |
| Type IV | – | |
All the patients of this series were treated by traction after the reduction, using soft tissue traction in simple dislocations with a mean of 1.3 weeks (range, 1–3) and skeletal traction in patients with associated fractures over 2.4 weeks (range, 1–6). Surgery was performed after the reduction in 3 patients, 2 due to a fracture of the posterior wall of the acetabulum (Thompson–Epstein type II), and one with a transverse fracture of the acetabulum (Thompson–Epstein type IV). All these cases were operated with osteosynthesis using a reconstruction plate with screws and the Kocher–Langenbeck approach. A post-operative period of offloading was established at between 4 and 12 weeks (mean, 7 weeks).
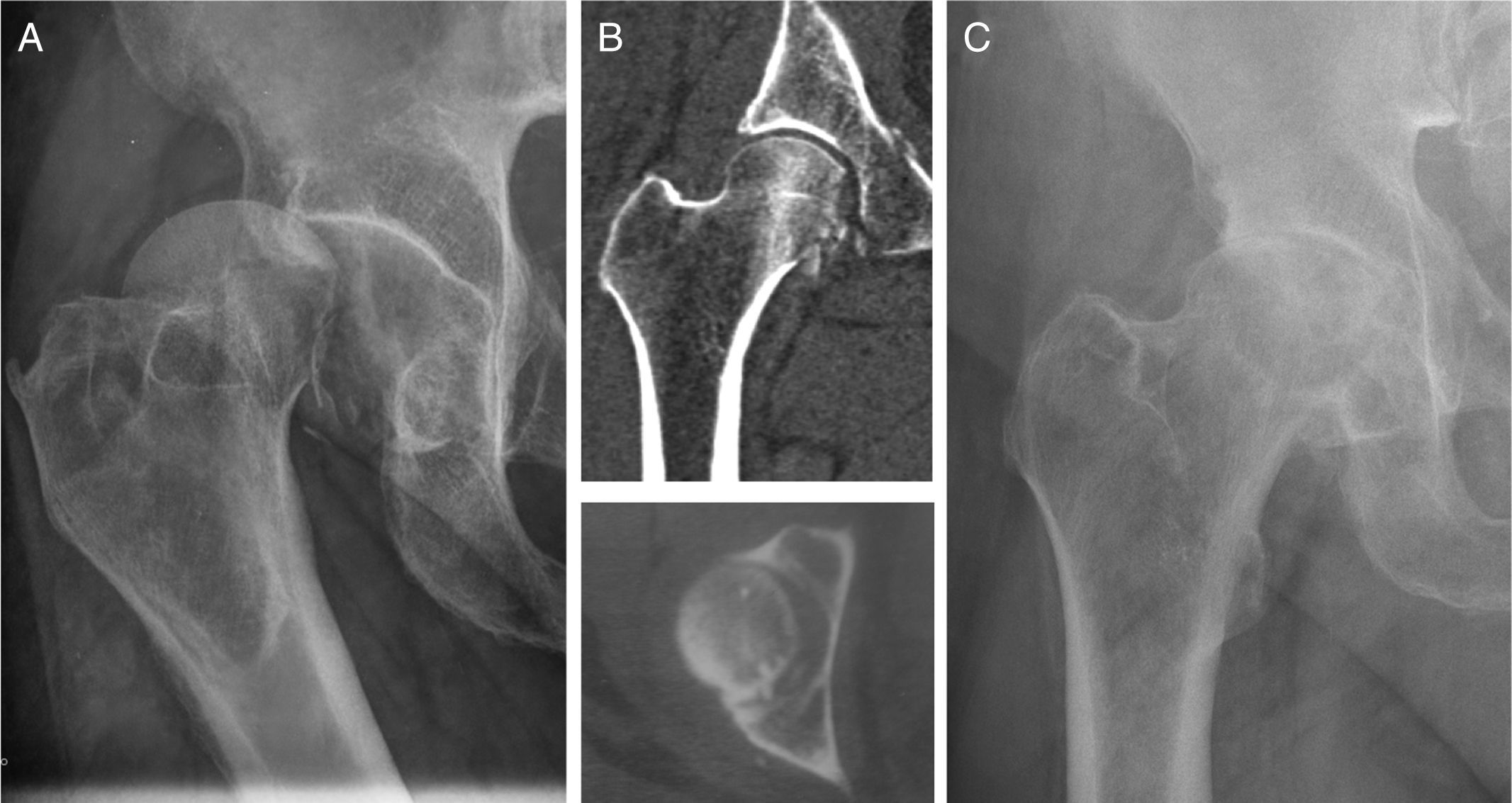
The CT scan after the reduction showed intra-articular fragments in 6 cases (20%). One of these was the patient who required surgery for reduction and resection of the intra-articular fragments, while the other 5 were treated conservatively. It was decided not to operate on 4 patients because the intra-articular fragments were below the fovea, and the other patient was not operated due to associated medical comorbidity (Fig. 1). All these cases had a posterior dislocation (4 cases were initially classified as complex dislocations and 2 as simple dislocations).
(A) Patient No. 22. Posterior fracture-dislocation of right hip associated with femoral head fracture (Thompson–Epstein type V). (B) CAT after closed reduction revealing intra-articular fragments in the posteromedial and lower area of the hip. Most of the fragments were below the fovea. The central fragment was not removed due to the patients’ associated medical comorbidities. (C) Plain X-ray showing arthritic changes in the hip, 12 years after the initial injury.
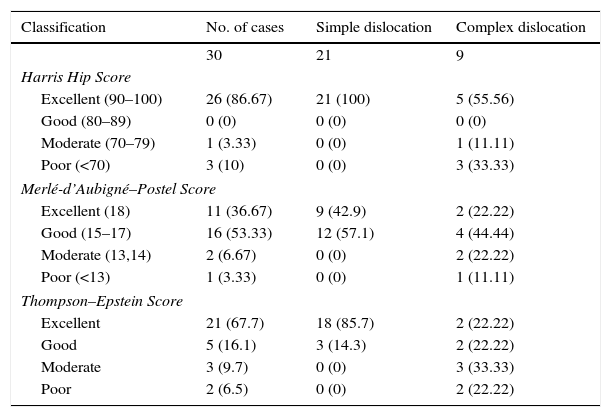
The functional and radiological outcomes were classified with the HHS, Merlé-d’Aubigné–Postel and Thompson–Epstein scales (Table 2). According to the HHS, the results were excellent in 25 cases (83.3%), moderate in one case (3.3%) and poor in 4 (13.3%). All the patients with simple dislocations had an excellent outcome, with a mean of 93.7 (range, 93–100), while those with complex dislocations had a mean HHS score of 79 (range, 33–100). On the Merlé-d’Aubigné–Postel scale, the patients with simple dislocations had a mean score of 17.4 (range, 17–18) and those with complex dislocations a mean of 15.2 (range, 10–18). The radiological analysis with Thompson–Epstein classification showed excellent (18; 85.7%) or good (3; 14.3%) results in the patients with no associated fractures. Furthermore, the results were excellent or good in 4 cases with complex dislocations, moderate in 3 and poor in the remaining 2.
Relationship between functional/radiological outcomes and type of dislocation.
| Classification | No. of cases | Simple dislocation | Complex dislocation |
|---|---|---|---|
| 30 | 21 | 9 | |
| Harris Hip Score | |||
| Excellent (90–100) | 26 (86.67) | 21 (100) | 5 (55.56) |
| Good (80–89) | 0 (0) | 0 (0) | 0 (0) |
| Moderate (70–79) | 1 (3.33) | 0 (0) | 1 (11.11) |
| Poor (<70) | 3 (10) | 0 (0) | 3 (33.33) |
| Merlé-d’Aubigné–Postel Score | |||
| Excellent (18) | 11 (36.67) | 9 (42.9) | 2 (22.22) |
| Good (15–17) | 16 (53.33) | 12 (57.1) | 4 (44.44) |
| Moderate (13,14) | 2 (6.67) | 0 (0) | 2 (22.22) |
| Poor (<13) | 1 (3.33) | 0 (0) | 1 (11.11) |
| Thompson–Epstein Score | |||
| Excellent | 21 (67.7) | 18 (85.7) | 2 (22.22) |
| Good | 5 (16.1) | 3 (14.3) | 2 (22.22) |
| Moderate | 3 (9.7) | 0 (0) | 3 (33.33) |
| Poor | 2 (6.5) | 0 (0) | 2 (22.22) |
Values shown as frequency and percentages in brackets.
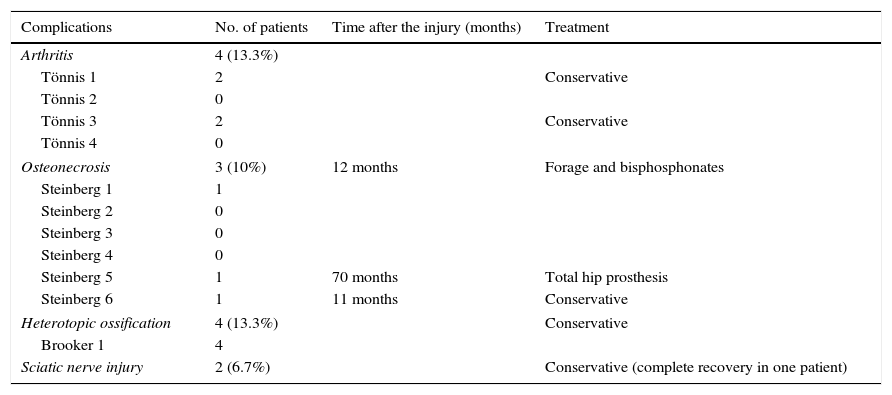
Our study identified various complications (Table 3). At the end of follow-up, arthritic signs were observed in 4 patients (13.3%). They had all suffered complex dislocations (3 posterior and one anterior), and using Tönnis’ classification, 2 were classified as grade 3 and another 2 grade 1. Of the 5 patients with intra-articular fragments who were treated conservatively, 3 developed arthritis (2 Tönnis grade 3 and one grade 1). Avascular necrosis was identified in 3 patients (10%), and a prompt closed reduction was achieved in all cases in under 6h. Of these patients, one was treated satisfactorily by forage of the femoral head, another required a total hip prosthesis and the last was treated conservatively. Two patients had a sciatic nerve injury before the reduction (6.7%), and both had complex dislocations (Thompson–Epstein type II). Only one of these patients managed a full recovery, after the initial injury.
Complications and their treatment.
| Complications | No. of patients | Time after the injury (months) | Treatment |
|---|---|---|---|
| Arthritis | 4 (13.3%) | ||
| Tönnis 1 | 2 | Conservative | |
| Tönnis 2 | 0 | ||
| Tönnis 3 | 2 | Conservative | |
| Tönnis 4 | 0 | ||
| Osteonecrosis | 3 (10%) | 12 months | Forage and bisphosphonates |
| Steinberg 1 | 1 | ||
| Steinberg 2 | 0 | ||
| Steinberg 3 | 0 | ||
| Steinberg 4 | 0 | ||
| Steinberg 5 | 1 | 70 months | Total hip prosthesis |
| Steinberg 6 | 1 | 11 months | Conservative |
| Heterotopic ossification | 4 (13.3%) | Conservative | |
| Brooker 1 | 4 | ||
| Sciatic nerve injury | 2 (6.7%) | Conservative (complete recovery in one patient) | |
The statistical analysis did not find any statistically significant association between poor clinical/radiological results or complications and the ISS scores, mechanism of injury, time of reduction and the patient's age. The presence of intra-articular fragments was significantly associated with the onset of arthritis, since 3 of the 5 patients who were treated conservatively developed degenerative signs (p<0.05). Likewise, a statistical association was found between the presence of associated fractures and arthritis, since this finding was present in 44% (4 out of 9) of the patients with complex dislocations. None of the patients with simple dislocations developed arthritis at the end of follow-up. This pattern was also confirmed with the Thompson–Epstein classification, with good or excellent outcomes in all the simple dislocations (p<0.01). There was a strong correlation between these findings and the clinical outcomes. All the patients with simple dislocations had a good or excellent outcome (HHS>80 or Merlé-d’Aubigné–Postel>14) 44% of the patients with complex dislocations had a moderate or poor outcome.
DiscussionTraumatic hip dislocations are an orthopaedic emergency and diagnosis is relatively simple by physical examination and plain X-ray. However this disorder is frequently associated with polytraumatised patients and in this scenario, early diagnosis and prompt treatment can be complex. Some authors have shown a poorer prognosis in patients with severe associated injuries.1,5 Pape et al. showed a mean ISS score of 31 points (range, 19–66), but even for this type of patient a diligent attitude in short and medium term treatment is recommended.17 These authors only collected long-term data (a mean of 8 years) on 13 patients. Although 10 patients had excellent or good clinical outcomes, 5 showed signs of arthritic change and 7 had necrosis of the femoral head. Compared with this study, our series showed a mean ISS of 13 points (range, 6–50). Our hypothesis is that these lower values might explain our better results, but we were not able to find a significant association between the ISS and the clinical or radiological outcomes.
Various complications have been published after hip dislocation or fracture-dislocation. Necrosis of the femoral head occurs in between 5% and 40% of cases, and it has been suggested that this risk increases in the time between the injury and reduction. Traditionally early reduction is advocated and some authors have confirmed that a delay of more than 6 or 12h is a major prognostic factor.11,18,19 Sahin et al. showed better results in patients whose reduction was achieved in the first 12h after the initial injury compared to cases with a later reduction.2 However, they found no differences with regard to osteonecrosis. Other studies have shown that the time of the reduction is not a significant prognostic factor. Letournel and Judet found no differences in the rate of osteonecrosis in patients whose reduction was performed in the first 6h, from 7 to 24h, or from 2 to 3 days.6 In a more recent study, Bhandari et al. did not find that the time of reduction was associated with poorer functional or radiological outcomes.20 These authors suggest that the mechanism of injury might cause irreversible damage to the vascularisation of the femoral head, even if an early reduction is achieved. In our study, we could not confirm that the time of the reduction was a prognostic factor since all the patients underwent prompt reduction. The patients who developed osteonecrosis of the femoral head (3 cases) were treated with a closed reduction in under 6h.
Post-traumatic arthritis is the most common long-term complication and is associated with acetabular or femoral head fractures.21 In our study, 4 patients (13.3%) developed hip arthritis, and all of them had complex dislocations, while none of the patients with simple dislocations showed arthritic signs at the last follow-up. Another factor to highlight is late reduction, which has been associated with degenerative changes in some studies.2,22 We found a strong correlation between radiological signs and clinical outcomes, since all the patients with simple dislocations had good or excellent outcomes with the HHS and Merlé-d’Aubigné–Postel scales. On the other hand, other authors have found arthritic changes after simple dislocations, ranging from 4.5% and 25%.1,2,5,11 With regard to complex dislocations, a recent study demonstrated that the quality of the reduction of the associated fracture was the most important predictor for the onset of arthritis. This paper concluded that the patients who did not have an anatomical reduction developed arthritis, while this complication was only encountered in 25.5% of those who had an appropriate reduction. Furthermore, this latter group of patients had better hip functionality for more years.20 Various authors have observed the relationship between free fragments and poorer results, indicating that removing these fragments is necessary in some cases.22,23 Foveal or infrafoveal fragments are a controversial issue and it is possible for them not to be removed.24 There is consensus on removing fragments that are trapped between the joint surfaces to minimise chondral damage and the progression of arthritis. In our study, 4 patients with free intra-articular bodies below the fovea were treated conservatively, since these patients had no articular blockage. However, 2 of them (50%) developed arthritis. Removal of these free bodies might have reduced the possibility of subsequent arthritis, but other factors might have been implicated. The other patient with free intra-articular bodies who was not operated, due to medical comorbidities, developed degenerative signs.
Heterotopic ossifications are a relatively common complication after a dislocation and their frequency varies between 7.5% and 64%.17,23 Various risk factors have been associated with this complication, such as associated fractures, severe muscle damage, surgical intervention, high ISS and concomitant cerebral neurological or spinal injury.17,25 We found this complication in 4 patients (12.9%), all of them were Brooker type I, with no functional repercussions. Sciatic nerve injury occurs in 10%–15% of cases.11 The mechanism tends to be compression or stretching of the nerve by posterior dislocation and has been associated with the time of reduction.26 Functional recovery depends on the type of injury, but some authors have published it occurring in 70% of cases.27 In this study, sciatic nerve injury was found in 3 patients (9.6%), all of whom had associated acetabular fractures, and the prognosis was poor, since only one patient made an adequate recovery.
The limitations of this study are the relatively small sample size and the variability of follow-up. However, our outcomes show a strong association between intra-articular fragments and the onset of arthritis, therefore removing these free bodies (by open or arthroscopic surgery) might be considered. Although some authors have considered that small infra-foveal fragments that enable joint congruence might not be removed, our study shows that arthritis developed in 60% of patients with these fragments. We established that complex dislocations have been associated with poorer functional and radiological outcomes and, although the simple dislocations had good outcomes, more long-term studies are required to establish the ultimate prognosis of these patients.
Level of evidenceLevel of evidence iv.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their centre of work regarding the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
| Excellent | 1. Normal relationship between acetabulum and femoral head 2. Normal joint space 3. Normal femoral head density 4. No osteophytes 5. No capsular heterotopic ossification |
| Good | 1. Normal relationship between acetabulum and femoral head 2. Minimal diminution of joint space 3. Minimal bone density loss 4. Minimal osteophyte formation 5. Minimal capsular heterotopic ossification |
| Moderate | 1. Normal relationship between acetabulum and femoral head. − One or more of the following: 2. Moderate diminution of the joint space 3. Mottling of the head, areas of sclerosis and areas of diminution of density 4. Moderate formation of osteophytes 5. Moderate-severe formation of capsular heterotopic ossification 6. Depression of subchondral bone in femoral head |
| Poor | 1. Almost complete obliteration of the articular interline 2. Relative increase in femoral head density 3. Formation of subchondral cysts 4. Formation of sequestra 5. Severe femoral head deformity 6. Severe osteophyte formation 7. Acetabular sclerosis |
| Patient | Age | Thompson–Epstein | Epstein | Stewart–Milford | ISS | Treatment | Follow-up (years) | Harris Hip Score | Merlé-d’Aubigné–Postel | Complications |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 30 | 2A | 1 | 18 | CR | 7 | 93 | 17 | ||
| 30 | 1 | 1 | 18 | CR | 7 | 93 | 17 | |||
| 2 | 25 | 4 | 2 | 6 | CR | 15 | 100 | 18 | ||
| 3 | 77 | 1 | 1 | 6 | CR | 4 | 100 | 18 | HO | |
| 4 | 29 | 2A | 1 | 13 | CR | 13 | 100 | 18 | ||
| 5 | 62 | 1 | 1 | 10 | CR | 5 | 93 | 17 | Osteonecrosis | |
| 6 | 20 | 1 | 1 | 13 | CR | 16 | 96 | 17 | ||
| 7 | 23 | 1 | 1 | 9 | CR | 16 | 96 | 17 | ||
| 8 | 17 | 1 | 1 | 9 | CR | 10 | 91 | 17 | ||
| 9 | 36 | 2 | 3 | 10 | CR | 4 | 97 | 17 | Sciatic nerve injury | |
| 10 | 40 | 3 | 2 | 8 | CR | 14 | 66 | 14 | Arthritis | |
| 11 | 42 | 1 | 1 | 50 | OR | 15 | 97 | 18 | HO | |
| 12 | 15 | 1 | 1 | 9 | CR | 11 | 100 | 18 | ||
| 13 | 70 | 1 | 1 | 9 | CR | 4 | 100 | 18 | ||
| 14 | 16 | 1 | 1 | 18 | CR | 13 | 100 | 18 | ||
| 15 | 31 | 2 | 3 | 13 | CR | 14 | 96 | 17 | ||
| 16 | 41 | 1 | 1 | 27 | CR | 5 | 96 | 17 | ||
| 17 | 23 | 1 | 1 | 9 | CR+ORIF | 17 | 100 | 18 | ||
| 18 | 59 | 2 | 3 | 34 | CR | 12 | 33 | 10 | Osteonecrosis Sciatic nerve injury | |
| 19 | 53 | 2C | 2 | 13 | CR | 9 | 100 | 18 | Arthritis, HO | |
| 20 | 14 | 1 | 1 | 10 | CR+ORIF | 14 | 97 | 18 | ||
| 21 | 24 | 1 | 1 | 14 | CR | 6 | 96 | 17 | ||
| 22 | 33 | 5 | 4 | 17 | CR | 14 | 50 | 13 | Arthritis | |
| 23 | 49 | 1 | 1 | 6 | CR | 17 | 96 | 17 | HO | |
| 24 | 18 | 1 | 1 | 8 | CR | 10 | 95 | 17 | ||
| 25 | 27 | 1 | 1 | 6 | CR+ORIF | 13 | 97 | 17 | ||
| 26 | 52 | 1 | 1 | 10 | CR | 17 | 100 | 18 | ||
| 27 | 16 | 1 | 1 | 8 | CR | 6 | 96 | 17 | ||
| 28 | 22 | 2 | 2 | 6 | CR | 17 | 92 | 15 | Osteonecrosis (THP) | |
| 29 | 62 | 5 | 4 | 13 | CR | 5 | 77 | 15 | Arthritis |
ISS: Injury Severity Score; HO: heterotopic ossification; THP: total hip prosthesis; OR: open reduction; ORIF: open reduction and internal fixation; CR: closed reduction.
Please cite this article as: Moreta J, Foruria X, Sánchez A, Aguirre U. Factores pronósticos tras una luxación traumática de cadera. Estudio retrospectivo a largo plazo. Rev Esp Cir Ortop Traumatol. 2017;61:367–374.