To study young patients after scoliosis surgery in order to determine risk and prevention factors for developing a crankshaft phenomenon (CP).
MethodsRetrospective study of a cohort of 26 patients. Six were excluded due to progression of various conditions. Crankshaft was defined as an increase in the Cobb angle>10°, or the Mehta angle (DAVC)>10°, or any decrease in the apex-rib thoracic distance, or increase in the vertebral apical lumbar translation (TVA). Patients with and without CP development were compared in order to analyse preoperative, surgical and postoperative risk factors, as well as the influence of different surgical techniques.
ResultsThe mean follow-up was 83.9 months. Nine patients (45%) developed the crankshaft phenomenon. Only immaturity parameters were associated with development of CP. No preoperative or postoperative radiographic parameters appeared to influence its development. The amount of correction may be a protective factor (41.4% vs. 61.4%, P=.06). The double approach was able to prevent the development of CP (0%) compared with single posterior instrumentation (44%), P=.02.
DiscussionNone of these preoperative factors seemed to predispose to CP: gender or etiology, T5–T12 kyphosis or apical hypokyphosis, coronal Cobb, vertebral rotation, or DAVC. The residual postoperative Cobb, achieved kyphosis, or wired instrumentation vs. hooks, also seemed to have no influence.
ConclusionIn patients with open triradiate cartilage under 11 years of age, it seems advisable to correct by double approach to avoid the appearance of the crankshaft phenomenon.
Estudiar los pacientes inmaduros con cartílago trirradiado abierto, operados de escoliosis, en busca de factores de riesgo y de prevención para desarrollar un fenómeno de crankshaft (CP).
Material y métodosEstudio retrospectivo de una cohorte de 26 pacientes. Seis se excluyeron por progresión de distinta etiología. Se definió crankshaft como un aumento del Cobb mayor de 10°, o una diferencia del ángulo de Mehta (diferencia ángulo vértebra-costilla, DAVC) mayor de 10°, o cualquier disminución de la distancia ápex-costilla torácica o aumento de la traslación vertebral apical lumbar (AVT, sigla del inglés apical vertebral translation). Se compararon los pacientes con y sin desarrollo de CP para analizar los factores de riesgo preoperatorios, quirúrgicos y postoperatorios. Se estudió la las influencia de distinta técnicas quirúrgicas.
ResultadosEl seguimiento medio fue de 83,9 meses. Nueve pacientes (45%) desarrollaron el CP. Sólo los parámetros de inmadurez ósea se asociaron al desarrollo de CP. Ningún parámetro radiográfico preoperatorio o postoperatorio parece influir en su desarrollo. La cantidad de corrección podría ser un factor de protección (41,4 vs. 61,4%; p = 0,06). El doble abordaje fue capaz de evitar el desarrollo de CP (0%) en comparación con la instrumentación única posterior (44%), p = 0,02.
DiscusiónNo se ha conseguido demostrar que estos factores preoperatorios predispongan a la aparición de crankshaft: sexo o etiología, cifosis T5-T12, hipocifosis apical, Cobb coronal, rotación vertebral o DAVC. Tampoco parecen influir el Cobb postoperatorio residual, la cifosis conseguida, o la instrumentación con alambres frente a ganchos.
ConclusiónEn los pacientes con cartílago trirradiado abierto menores de 11 años parece aconsejable corregir la escoliosis mediante doble abordaje para evitar el fenómeno del cigüeñal o CP, progresión de la deformidad tras una artrodesis posterior por crecimiento anterior vertebral.
Dubousset1 coined the term “crankshaft phenomenon” (CP) to describe scoliosis progression after having achieved solid posterior arthrodesis in immature patients. This phenomenon is produced by the continual anterior vertebral growth in the presence of a posterior fusion posterior that acts as suspenders, forcing the spine into a progressive lordoscoliosis with rotation in the direction of the original deformity.1,2
Various authors have studied the postoperative progression of the fused curves, both in idiopathic2–13 as well as in congenital scoliosis.8,14–16 However, there are only a few studies that have analyzed immature patients with triradiate cartilage (TRC) still open.3,5,6,8,10,11,14 The final study showed rates of CP after instrumented posterior arthrodesis of between 15% and 75%. To prevent the development of this phenomenon, some authors recommend performing an additional anterior apical fusion.2,5–10,13,15,17–19
In spite of what has been published, these studies do not cover a great number of patients; in addition, they are not homogeneous with respect to surgical approach, type of instruments used, definition of progression, state of patient maturity, or curve etiology. For these reasons, there is still strong controversy about the prevalence of CP, the risk factors, and how to prevent it with success during treatment.
The objective of this study was to investigate the risk factors associated with the development of CP in immature patients operated on for scoliosis with open TRC, and assess whether this phenomenon could be prevented using anterior apical fusion.
Materials and methodsWe reviewed the clinical histories of 26 skeletally immature patients, operated on for progressive scoliosis by the same surgeon, in a single hospital center. The work followed the ethical standards established in the Declaration of Helsinki.
The criteria for inclusion were diagnosis of scoliosis, open TRC with Risser 0 at the time of surgery, and a minimum follow-up period of 2 years. We excluded 6 patients due to a progression secondary to non-painful pseudoarthrosis (3), incorrect selection of fusion levels with adding-on phenomenon (2), and disconnection of caudal hook (1). In the end, there were 20 patients included in the study.
The variables studied were sex, chronological age at the time of surgery, Risser sign, location of the curve, curve etiology, surgical approach, type of instrumentation, and use of sublaminar wires.
Patient X-rays were reviewed preoperatively, a year after the operation, and at the end of follow-up. The parameters reviewed in the frontal X-ray included the Risser sign; Cobb angle; apical vertebral rotation (AVR) using the Perdriolle method; apical vertebral translation (AVT) measured in the main thoracic or thoracolumbar curves as the distance between the vertebral apex and the thoracic cage on the side of the curve convexity, or in the main lumbar curves as the distance from the apex to the vertical sacral line; rib-vertebra angle difference (RVAD) or Mehta angle; and the deviation of the trunk. In the sagittal plane, we measured T5–T12 thoracic kyphosis and kyphosis at the apex of the deformity.
The parameters measured 1 year from the postoperative period and at the end of follow-up. The postoperative progression of the curve or the crankshaft phenomenon (CP) was defined as an increase of more than 10° in the Cobb angle,2–8,11,14,15 or an increase in RVAD greater than 10°,2,3,5,7,8,10,11,14 or an increase in AVR greater than 10°,5 or a decrease in thoracic AVT or an increase in lumbar AVT.2,8
To calculate the AVT, we found the average of the translations that reflected progression in both thoracic and lumbar curves (absolute value), being reflected as a negative figure in the case of progression. We then compared the crankshaft and no crankshaft groups.
Mean age was 10.3±3.6 years (2–14.9 years), 9 (45%) of the patients being younger than 11. In the surgery, all the patients had Risser 0. The dysplastic curves included 1 patient with Klippel–Trenaunay syndrome, 1 with arthrogryposis, and 1 with Angelman syndrome. One year after surgery, the Risser stages were distributed as follows: in 16 patients, Risser 0; in 2 patients, Risser 1; and in 2 patients, Risser 2. At the end of follow-up, the Risser stages were distributed in the following manner: in 9 patients, Risser 4; and in 11 patients, Risser 5. Average follow-up was 6.9 years (24–240 months). Mean preoperative frontal Cobb angle was 62±17°, and the preoperative T5–T12 angle was 29.9±23°.
We used SPSS® software (version 11.5, SAS Institute Inc., Cary, NC, USA) for the statistical analysis. The distribution of these variables was shown as mean and standard deviation. The comparisons between variables was performed using the Mann–Whitney U, Fisher's exact test, and χ2 statistics, as appropriate, with a level of significance of 95% (P<.05).
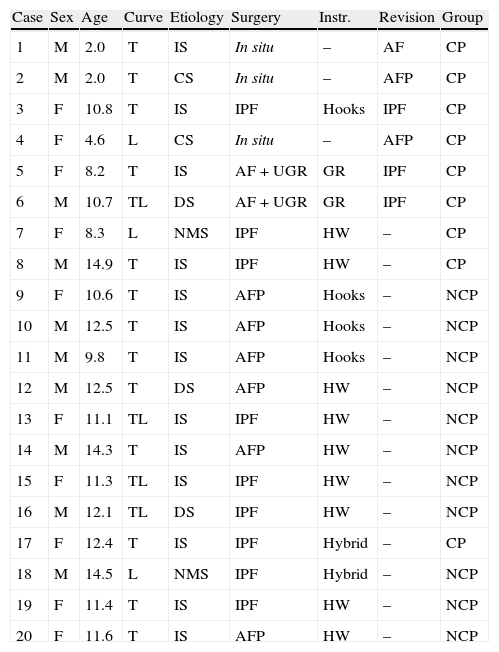
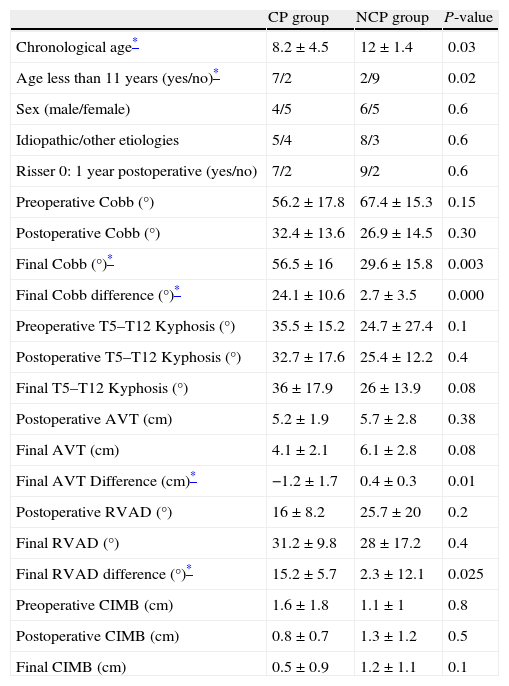
ResultsOf the 20 patients reviewed, 9 (45%) developed crankcase phenomenon and were designated the CP group. There were 11 patients that did not develop the CP; these constituted the no crankcase phenomenon (NCP) group (Table 1). Table 2 presents the main data for the preoperative period, 1 year postoperatively, and at the end of follow-up. The variables of chronological age and age less than 11 years showed significant differences (P=.03 and P=.02) between both groups. Sex and curve etiology did not differ between the groups (P>.05) (Table 3).
Demographic data.
| Case | Sex | Age | Curve | Etiology | Surgery | Instr. | Revision | Group |
| 1 | M | 2.0 | T | IS | In situ | – | AF | CP |
| 2 | M | 2.0 | T | CS | In situ | – | AFP | CP |
| 3 | F | 10.8 | T | IS | IPF | Hooks | IPF | CP |
| 4 | F | 4.6 | L | CS | In situ | – | AFP | CP |
| 5 | F | 8.2 | T | IS | AF+UGR | GR | IPF | CP |
| 6 | M | 10.7 | TL | DS | AF+UGR | GR | IPF | CP |
| 7 | F | 8.3 | L | NMS | IPF | HW | – | CP |
| 8 | M | 14.9 | T | IS | IPF | HW | – | CP |
| 9 | F | 10.6 | T | IS | AFP | Hooks | – | NCP |
| 10 | M | 12.5 | T | IS | AFP | Hooks | – | NCP |
| 11 | M | 9.8 | T | IS | AFP | Hooks | – | NCP |
| 12 | M | 12.5 | T | DS | AFP | HW | – | NCP |
| 13 | F | 11.1 | TL | IS | IPF | HW | – | NCP |
| 14 | M | 14.3 | T | IS | AFP | HW | – | NCP |
| 15 | F | 11.3 | TL | IS | IPF | HW | – | NCP |
| 16 | M | 12.1 | TL | DS | IPF | HW | – | NCP |
| 17 | F | 12.4 | T | IS | IPF | Hybrid | – | CP |
| 18 | M | 14.5 | L | NMS | IPF | Hybrid | – | NCP |
| 19 | F | 11.4 | T | IS | IPF | HW | – | NCP |
| 20 | F | 11.6 | T | IS | AFP | HW | – | NCP |
AF: anterior fusion; AFP: anterior fusion and posterior instrumentación; AF+UGR: anterior fusion and unilateral posterior growing rods; CP: crankshaft phenomenon; CS: congenital scoliosis; DS: dysplastic scoliosis; F: female; GR: growing rods; HW: hybrid with wires; Instr.: instrumentation; IPF: instrumented posterior fusion; IS: idiopathic scoliosis; L: main lumbar curve; M: male; NCP: no crankshaft phenomenon; NMS: neuromuscular scoliosis; T: main thoracic curve; TL: main thoracolumbar curve.
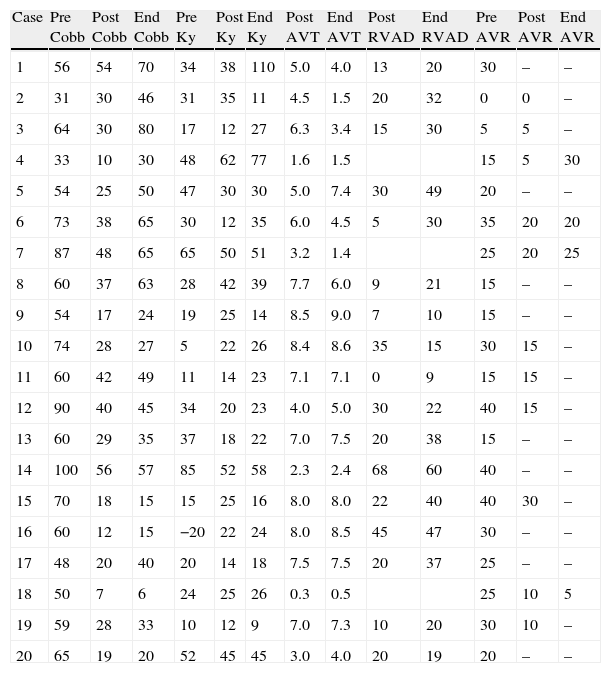
Sample data.
| Case | Pre Cobb | Post Cobb | End Cobb | Pre Ky | Post Ky | End Ky | Post AVT | End AVT | Post RVAD | End RVAD | Pre AVR | Post AVR | End AVR |
| 1 | 56 | 54 | 70 | 34 | 38 | 110 | 5.0 | 4.0 | 13 | 20 | 30 | – | – |
| 2 | 31 | 30 | 46 | 31 | 35 | 11 | 4.5 | 1.5 | 20 | 32 | 0 | 0 | – |
| 3 | 64 | 30 | 80 | 17 | 12 | 27 | 6.3 | 3.4 | 15 | 30 | 5 | 5 | – |
| 4 | 33 | 10 | 30 | 48 | 62 | 77 | 1.6 | 1.5 | 15 | 5 | 30 | ||
| 5 | 54 | 25 | 50 | 47 | 30 | 30 | 5.0 | 7.4 | 30 | 49 | 20 | – | – |
| 6 | 73 | 38 | 65 | 30 | 12 | 35 | 6.0 | 4.5 | 5 | 30 | 35 | 20 | 20 |
| 7 | 87 | 48 | 65 | 65 | 50 | 51 | 3.2 | 1.4 | 25 | 20 | 25 | ||
| 8 | 60 | 37 | 63 | 28 | 42 | 39 | 7.7 | 6.0 | 9 | 21 | 15 | – | – |
| 9 | 54 | 17 | 24 | 19 | 25 | 14 | 8.5 | 9.0 | 7 | 10 | 15 | – | – |
| 10 | 74 | 28 | 27 | 5 | 22 | 26 | 8.4 | 8.6 | 35 | 15 | 30 | 15 | – |
| 11 | 60 | 42 | 49 | 11 | 14 | 23 | 7.1 | 7.1 | 0 | 9 | 15 | 15 | – |
| 12 | 90 | 40 | 45 | 34 | 20 | 23 | 4.0 | 5.0 | 30 | 22 | 40 | 15 | – |
| 13 | 60 | 29 | 35 | 37 | 18 | 22 | 7.0 | 7.5 | 20 | 38 | 15 | – | – |
| 14 | 100 | 56 | 57 | 85 | 52 | 58 | 2.3 | 2.4 | 68 | 60 | 40 | – | – |
| 15 | 70 | 18 | 15 | 15 | 25 | 16 | 8.0 | 8.0 | 22 | 40 | 40 | 30 | – |
| 16 | 60 | 12 | 15 | −20 | 22 | 24 | 8.0 | 8.5 | 45 | 47 | 30 | – | – |
| 17 | 48 | 20 | 40 | 20 | 14 | 18 | 7.5 | 7.5 | 20 | 37 | 25 | – | – |
| 18 | 50 | 7 | 6 | 24 | 25 | 26 | 0.3 | 0.5 | 25 | 10 | 5 | ||
| 19 | 59 | 28 | 33 | 10 | 12 | 9 | 7.0 | 7.3 | 10 | 20 | 30 | 10 | – |
| 20 | 65 | 19 | 20 | 52 | 45 | 45 | 3.0 | 4.0 | 20 | 19 | 20 | – | – |
AVR: apical vertebral rotation; AVT: apical vertebral translation; Ky: kyphosis; RVAD: rib-vertebra angle difference; End: end of follow-up; Pre: preoperative; Post: 1 year postoperative.
Results.
| CP group | NCP group | P-value | |
| Chronological age* | 8.2±4.5 | 12±1.4 | 0.03 |
| Age less than 11 years (yes/no)* | 7/2 | 2/9 | 0.02 |
| Sex (male/female) | 4/5 | 6/5 | 0.6 |
| Idiopathic/other etiologies | 5/4 | 8/3 | 0.6 |
| Risser 0: 1 year postoperative (yes/no) | 7/2 | 9/2 | 0.6 |
| Preoperative Cobb (°) | 56.2±17.8 | 67.4±15.3 | 0.15 |
| Postoperative Cobb (°) | 32.4±13.6 | 26.9±14.5 | 0.30 |
| Final Cobb (°)* | 56.5±16 | 29.6±15.8 | 0.003 |
| Final Cobb difference (°)* | 24.1±10.6 | 2.7±3.5 | 0.000 |
| Preoperative T5–T12 Kyphosis (°) | 35.5±15.2 | 24.7±27.4 | 0.1 |
| Postoperative T5–T12 Kyphosis (°) | 32.7±17.6 | 25.4±12.2 | 0.4 |
| Final T5–T12 Kyphosis (°) | 36±17.9 | 26±13.9 | 0.08 |
| Postoperative AVT (cm) | 5.2±1.9 | 5.7±2.8 | 0.38 |
| Final AVT (cm) | 4.1±2.1 | 6.1±2.8 | 0.08 |
| Final AVT Difference (cm)* | −1.2±1.7 | 0.4±0.3 | 0.01 |
| Postoperative RVAD (°) | 16±8.2 | 25.7±20 | 0.2 |
| Final RVAD (°) | 31.2±9.8 | 28±17.2 | 0.4 |
| Final RVAD difference (°)* | 15.2±5.7 | 2.3±12.1 | 0.025 |
| Preoperative CIMB (cm) | 1.6±1.8 | 1.1±1 | 0.8 |
| Postoperative CIMB (cm) | 0.8±0.7 | 1.3±1.2 | 0.5 |
| Final CIMB (cm) | 0.5±0.9 | 1.2±1.1 | 0.1 |
AVT: apical vertebral translation; CIMB: coronal imbalance; CP: crankshaft phenomenon; NCP: no crankshaft phenomenon; RVAD: rib-vertebra angle difference.
All the patients that developed the CP had a final increase in the frontal Cobb angle (difference between 1 year postoperatively and the end of follow-up), with a mean increase of 24±10.6°. This figure showed a statistical difference compared with the NCP group (2.7±3.5°), P=.000 (Table 3). The NCP group obtained an initial postoperative correction of 61%, while that of the CP group was 41.4% (P=.06).
There were no statistically significant differences between the groups (P>.05) (Table 3) in initial thoracic T5–T12 kyphosis (NCP 24.7° vs. CP 35.5°), its correction after surgery (NCP 0.7° vs. CP −2.7°), or loss at the end of follow-up (NCP 0.5° vs. CP 3.8°).
The NCP group presented a difference in mean final absolute AVT of +0.4cm, while the CP group presented a mean difference of −1.2cm (P=.01) (Table 3). Of the 9 patients that developed CP, 8 showed a progression in AVT, with a final average of −1.5cm. None of the patients in the NCP group showed a reduction (progression) of this distance at the end of follow-up (P=.000).
The Mehta angle or RVAD was measured in the 17 patients that presented main thoracic or thoracolumbar curves. This angle increase significantly in the CP group (NCP 2.3° vs. CP 15.2°; P=.02) (Table 3). All the patients that developed CP presented an increase in RVAD greater than 10°, with an average of 16.6±4.9° at the end of follow-up. Even so, 6 patients in the NCP group also showed a rise in the degree of obliquity in the ribs, although it was slight.
No relevant information was obtained from the data on AVR and on the kyphosis of the apical segment. There were no statistically significant differences between the groups in Risser stage or in the change in trunk imbalance (P=.3) (Table 3).
Surgical parametersNone of the 6 patients with anterior apical fusion and posterior solid instrumented arthrodesis developed CP (Table 1). Of the 9 patients on which an instrumented arthrodesis (posterior only) was performed, 4 (44%) developed CP during follow-up. The 3 patients on which we performed a posterior fusion in situ developed CP; likewise, the 2 patients on which we performed an anterior apical fusion accompanied by a posterior unilateral growing rod (without additional lengthening) developed CP (P=.01). These 5 patients were surgically revised, as was 1 patient with a failed posterior instrumented arthrodesis. The growing rods were replaced with bilateral rigid rods; 1 patient with fusion in situ received a posterior instrumented fusion. We rescued the other 3 patients with an anterior fusion, to attempt to halt the increase in the deformity.
Comparing the patients instrumented with sublaminar wires (9) and without wires (8), we found that 77% of those in which wires were used did not develop CP, while 50% of those in which wires were not used developed CP. Sublaminar wires were used for the treatment of larger curves (preoperative Cobb angle of 72°), while hooks were used in curves of lesser magnitude (preoperative Cobb angle of 59°). The correction obtained was very similar (56.8% with wires vs. 57.4% with hooks), but the final postoperative loss was 6° for the group using wires and 16° for the group using hooks. However, none of these figures had statistical support (P>.05).
DiscussionWith this study, we attempted to investigate new data about the prevalencia and the risk factors in the development of CP in patients with scoliosis and skeletal immaturity (open TRC), as well as the treatment to follow to prevent it.
Some authors indicate that a chronological age of less than 11 years,2,4,11,12 a skeletal age of less than 10 years,4,14 or a 0–1 Risser stage2,9 are associated with a greater prevalence of CP. Sanders et al.7 emphasized the importance of TRC and of the speed of the growth peak as fundamental predictors for CP development.5,11,20 Since then, there are only a few studies that have begun to include skeletally immature patients (with open TRC) to study CP, showing rates that range from 15% to 75%.6,8,10,14
In our study, all the patients had open TRC, 0 Risser stage, and were on average younger than 11 years, so they were at high risk of developing CP.2,4,5,8,11,14,15 We found postoperative CP in 45% of the patients. The CP appeared in the most immature patients (with a mean age of 8.2 years). Patients younger than 11 displayed a risk of 78% of developing CP, in contrast with the 18% risk of those older than 11 years. The Risser stage at the time of surgery did not seem to be associated with this phenomenon.
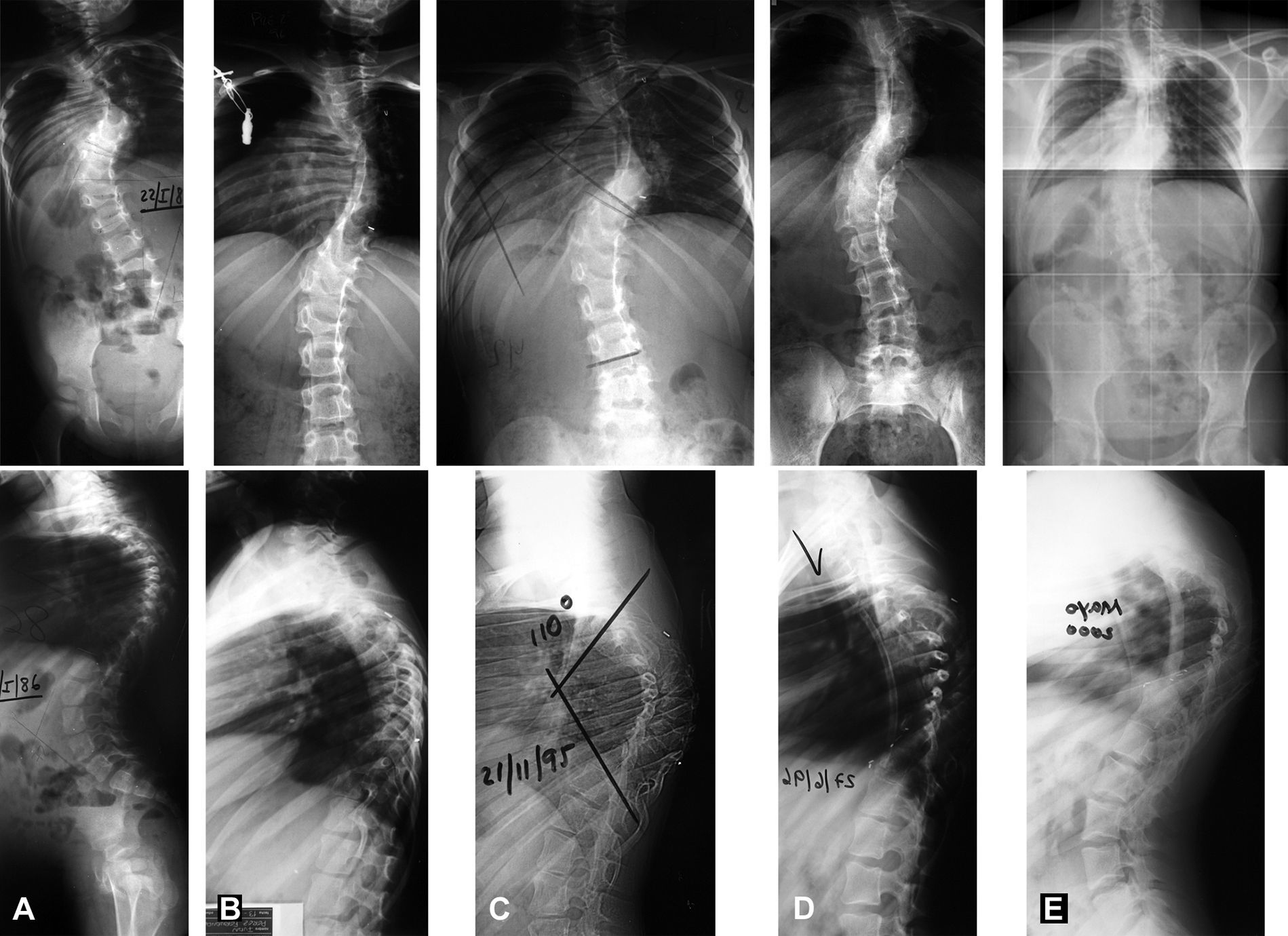
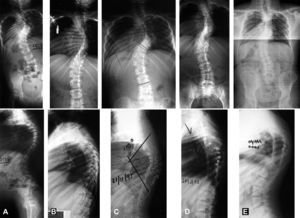
All the patients that developed CP had an increase in the frontal Cobb angle (between the postoperative assessment and the end of follow-up) greater than 10° (established as definition) with a mean increase of 24°. All these patients showed an increase in the Mehta angle (RVAD), with an average of 16°, although some patients without CP also had a slight rise in the rib angle. In addition, all the patients (except for 1) that developed CP had a variation in AVT, with an average progression of 1.5cm, which did not occur in any of the patients without CP. As is shown in this article, CP presents not only as a significant progression in the frontal Cobb angle, but also with other signs of 3-dimensional progression of the deformity, such as narrowing of the hemithorax in the curve convexity, increasing the rib obliquity, or apical rotation kyphosis (Fig. 1).
Case 1. Patient with idiopathic scoliosis. At 2 years of age, posterior fusion was performed in situ (A). The postoperative images show moderate correction (B). At 10 years old, the patient developed a crankshaft phenomenon with an increase in the frontal Cobb angle of 14° and the development of a very marked rotational kyphosis of 110° (C). An anterior approach was performed to halt the sagittal rotation collapse, with discectomy, arthrodesis and pedicle rib graft (D). Thirteen years later, at the age of 25 (E), the patient remains balanced and the graft has provided protection against an increase in the collapse.
In contrast to what has been published,4,9 the preoperative curves of greater magnitude failed to show a greater risk of CP (67° NCP vs. 56° CP) in our study. However, the curves of greater magnitude were treated more aggressively (many of them with double approaches), and as we will see later, the anterior apical fusion in the presence of a solid posterior instrumentation protected our patients from CP. The postoperative Cobb angle (26° NCP vs. 32° CP) did not seem to be associated with progression of the final curve. Nevertheless, better correction in the immediate postoperative period (61% NCP vs. 41% CP) seems to have a tendency toward protection against the development of CP.
It has been suggested that preoperative thoracic hypokyphosis can lead to a greater risk of developing CP,21–24 while a well-molded postoperative kyphosis could protect against it.2,17,23,25 This postoperative kyphosis can be restored better using wires than with any other type of instrumentation,26,27 thus providing protection against CP.3 In our study, the initial kyphosis (24° NCP vs. 35° CP), its surgical correction (25° NCP vs. 32° CP), and the loss at the end of follow-up (0.7° NCP vs. −2.7° CP) failed to show an association with the development of CP. Although only 23% of the patients fused with sublaminar wires developed CP, in comparison with 50% of those in which thoracic hooks were used, we cannot statistically demonstrate the benefits of the wire in preventing progression. Even though references on this subject have begun to appear, there are still no studies that demonstrate that using thoracic screws for correcting these curves yield additional benefits against the development of CP (35% in the series published).28
TreatmentThe CP has been avoided in all our patients in whom we performed from the first an anterior apical fusion with solid instrumented posterior spinal fusion. When only a unilateral posterior growing rod was added after the anterior fusion, the patients had to be rescued in the end because they had developed CP. Some authors have published the fact that anterior apical fusion may contribute to an increase in postoperative kyphosis,25,29 and that it may also interrupt anterior vertebral growth, helping to prevent CP.2,5–10,13,15,17–19,28 However, in our opinion, an additional solid posterior fusion is needed to prevent this phenomenon. The lack of a rigid posterior arthrodesis could be the reason why other authors failed to brake its development in spite of a prior anterior fusion.6,13 Another way in which other authors have approached this situation has been adding anterior instrumentation to the dorsal anterior fusion, in Lenke 1 curve surgery; however, there is still controversy over the protection of this system against the development CP.30
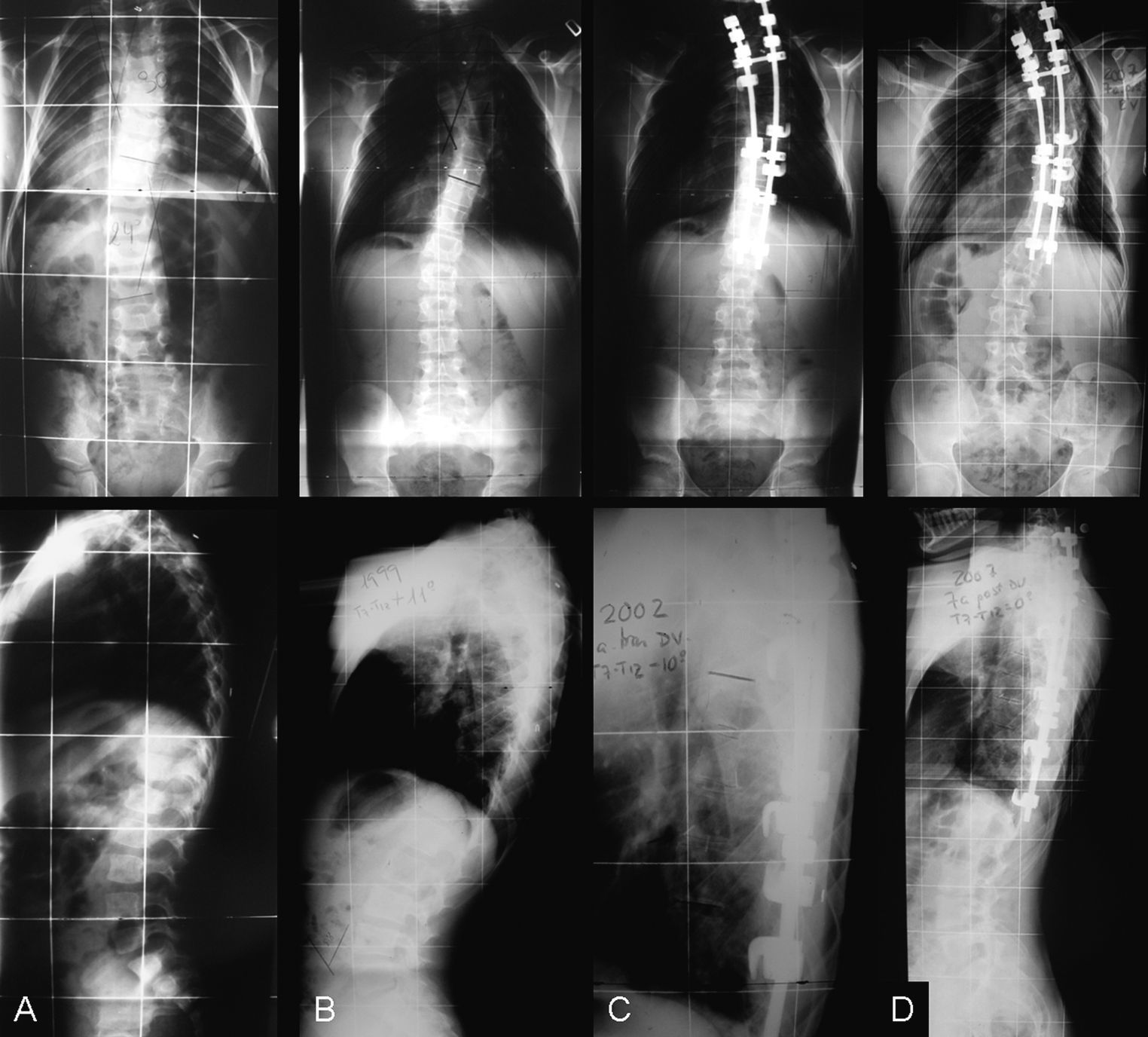
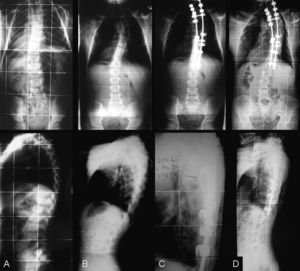
Posterior fusion in situ has shown the highest rates of CP.2 However, it must be remembered that this technique was used in the youngest patients, with great potential of anterior growth. In these patients, even with surgical revision, the progression in the evolution may not be controlled (Fig. 2). The thoracic deformity associated in these patients probably affects the progression of the spinal deformity.
Case 2. Patient with hemivertebra in T6. At 2 years of age, T2–T8 posterior fusion was performed in situ (A). At the age of 14, the thoracic curve had progressed from 30° to 46°, the rib-apex distance had decreased 3cm, and the Mehta angle had risen by 12° (B). As the peak of high speed growth had begun, a double approach was performed, with discectomy and anterior fusion with additional posterior instrumentation (C). Seven years later, the frontal Cobb angle had begun to progress again, the rib-apex distance had decreased, and the obliquity of the Mehta angle had increased (D). The double approach revision failed to halt the progression of the deformity.
The bibliography2–6,8,10,11,28 shows rates between 5% and 97% in the development of CP after instrumented posterior arthrodesis. Our study yielded a rate of 44%, but only 1 patient had to be operated again.
There are some limitations in our study. It was a retrospective study, with heterogeneous etiologies and various surgical methods, with a limited sample size. However, we limited our inclusion criteria very strictly to very immature patients at high risk of developing CP, and the lengthy follow-up (a mean of 7 years) has made it possible to assess the results at a very long term.
In conclusion, neither preoperative and postoperative thoracic kyphosis, nor the magnitude of the rib curve, seem to be associated with the development of CP. The crucial risk factor is skeletal immaturity: the patients younger than 11 years that present open TRC may have a significantly greater risk of developing CP and, if this occurs, they will need surgical revision in the majority of the cases. We are aware of the difficulties involved in an additional anterior approach, and that some authors have questioned its necessity.3,4,8,31 However, our data suggest that these immature patients can benefit from a double approach with anterior apical fusion and concurrent solid instrumented posterior spinal fusion.
Level of evidenceLevel of evidence 4.
Ethical responsibilitiesProtection of personas y animalsThe authors declare that the procedures followed conformed to the ethical standards of the responsible committee of human experimentation and that they were in agreement with the World Medical Association and the Declaration of Helsinki.
Data confidentialityThe authors declare that they followed the protocols of their work centre on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent for participating in this study.
Right to privacy and informed consentThe authors obtained informed consent from the patients and/or subjects included in the article. This document is in the possession of the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please, cite this article as: Pizones J, et al. Factores pronósticos del fenómeno de crankshaft en los pacientes con escoliosis y cartílago trirradiado abierto. ¿Es el doble abordaje la solución? Rev Esp Cir Ortop Traumatol. 2013;57:170–7.