The acetabular reconstruction with massive acetabular defects and pelvic discontinuity is a complex surgery with important difficulties for the orthopaedic surgeon. The objective of this study is to show the short and midterm results of the acetabular revision with the Cup-Cage construct in a consecutive series of cases.
Material and methodsRetrospectively we reviewed 22 consecutive patients with massive acetabular defects (8 Paprosky IIIa and 9 IIIB); 5 pelvic discontinuities; 2 pelvic fractures during the implantation of primary arthroplasty, and one pelvic pseudoarthrosis. All were reoperated with a trabecular metal acetabular component and a Cup-Cage. We did clinical and radiological follow-up to detect mechanical failures and loosening of the implant.
ResultsWith a middle follow-up of 45.06 months (12–73 months) we did not see any radiographic failure of the implant (component migration, osteolysis neither rupture of the implant or screws). The complications (13.63%) included one recurrent luxation, one infection and one recurrent subluxation. The Merle d’Aubigné-Postel score improved from 6.91 to 14.36 and the punctuation in the range of motion from 2.91 to 4.36 on average of the values preoperatively and postoperatively respectively and improvement in Harris Hip Score 30 (16–55) to 72 (40–90) in the latest follow up.
ConclusionThe acetabular reconstruction with the Cup-Cage system is a valid alternative for the reconstruction of massive acetabular defects (Paprosky type IIIA and IIIB) and pelvic discontinuities offering good results at short and midterm follow-up.
La reconstrucción acetabular con defectos óseos masivos y discontinuidades pélvicas es un procedimiento quirúrgico complejo que presenta importantes dificultades para el cirujano ortopédico. El objetivo de este estudio es presentar los resultados a corto y medio plazo de la revisión acetabular con el sistema de reconstrucción Cup-Cage en una serie consecutiva de casos.
Material y métodosRetrospectivamente revisamos 22 casos consecutivos de defectos acetabulares masivos (8 Paprosky IIIA y 9 IIIB); 5 discontinuidades pélvicas; 2 fracturas pélvicas durante la implantación de la prótesis primaria, y una seudoartrosis pélvica. Todos fueron revisados con un cotilo de metal trabecular y una caja de reconstrucción tipo Cup-Cage. Se realizó seguimiento clínico y radiográfico de los pacientes para detectar fallos mecánicos o aflojamientos del implante.
ResultadosEn un tiempo de seguimiento medio de 45,06 meses (12-73 meses) no se objetivó ningún fracaso radiográfico del implante (migración del componente, osteólisis ni rotura de tornillos). Las complicaciones (13,63%) incluyeron una luxación recidivante, una infección y una subluxación recidivante; todos precisaron reintervención quirúrgica. El Merle d’Aubigné-Postel mejoró de 6,91 a 14,36 y la puntuación del rango de movilidad, de 2,91 a 4,36 en promedio de los valores preoperatorios y postoperatorios, respectivamente, así como una mejoría del Harris Hip Score de 30 (16-55) a 72 (40-90) en el último control.
ConclusiónLa reconstrucción acetabular con el sistema Cup-Cage es una alternativa válida para la reconstrucción de pérdidas óseas acetabulares masivas (Paprosky tipo IIIA y IIIB) y discontinuidades pélvicas que ofrece buenos resultados a corto y medio plazo.
The reconstruction of acetabular bone loss in revision surgery is a highly complex procedure. In the majority of cases stable attachment is possible with the use of a cementless acetabular component. Trabecular metal tantalum components (Zimmer Biomet), with wedge-shaped boosters and implantor screws, even when in contact with healthy bone below 50%, obtain favourable, promising results due to the improvement of the biomechanical designs of these implants which promote osseointegration. However, any favourable outcome depends on defect extension and location, the quality of the remaining bone and, more important still, the presence of pelvic discontinuity or the size of the defect. Cases of large defects (IIIB) where the lesion affects both acetabular columns and roof with under 50% of patient bone or where there is pelvic discontinuity (this is defined as separation between the distal and proximal parts of the acetabular due to major bone loss or fracture through the acetabular columns)1–3 are technically extremely demanding, since attachment with acetabular tantalum implants alone, even with the use of boosters, is insufficient for the stability of the construct or of the half pelvis in the case of discontinuities. This micro movement would result in loosening and failure of reconstruction.
These situations have usually been treated with the use of reconstruction rings. However, given the impaired stability of these constructs, osseointegration of the implant is impossible and leads to screw breakage and failure of the operation due to implant shifting.
The use of the Cup-Cage has been described as a reliable alternative and a good option for cases with severe defects or pelvic discontinuities. This reconstruction consists in the use of an acetabular component of trabecular tantalum attached with multiple screws and an antiprotrusion ring placed over the cup and anchored to the ischium and upper part of the acetabulum. The ring provides initial stability to the tantalum acetabulum providing osseointegration.
The first midterm studies in reconstruction of severe defects and in pelvic discontinuities are, generally satisfactory.4,5 The aim of this study was to evaluate the clinical outcomes, complications and functional results of the series of acetabular reconstructions with the Cup-Cage construct undertaken in our hospital, for midterm reconstruction of massive acetabular defects and pelvic discontinuities.
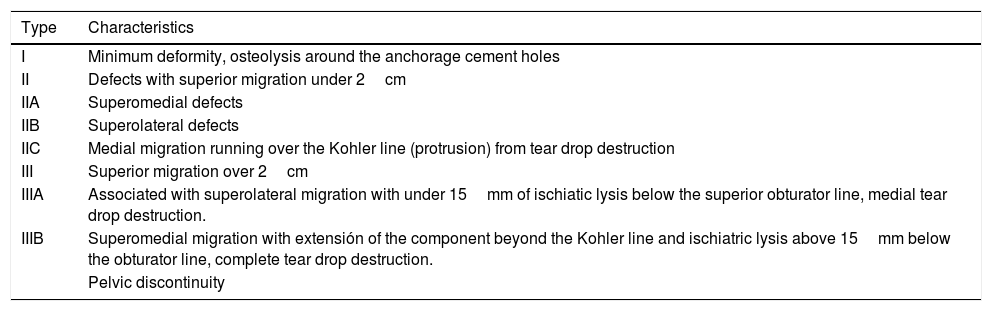
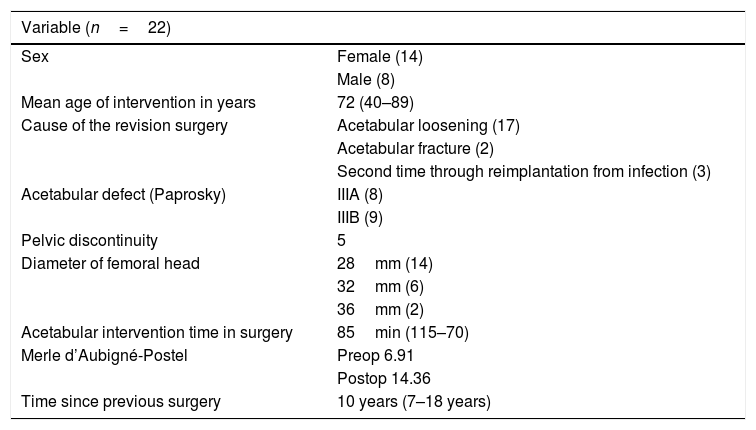
Material and methodsBetween 2009 and 2017, 23 Cup-Cage constructs were implanted for type II-B acetabular defects, in accordance with the Paprosky6 (Table 1) classification and pelvic discontinuities by 3 senior surgeons in the hip unit of our hospital. One patient was excluded because they died 3 months after surgery from medical problems which were unrelated to the revision surgery. As a result 22 patients underwent follow-up. Mean age of patients who underwent surgery was 72 (40–89). There were 14 women and 8 men. Twelve of the patients had undergone prior revision surgery. There were 14 women and 8 men. Twelve patients had presented with previous revision surgeries. The Merle d’Aubigné-Postel functional evaluation scale was used in all patients pre and postoperatively,7 as was the Harris Hip Score scale. Mean follow-up was 45.06 months (12–73 months). Radiographic controls were practised postoperatively with anteroposterior projections of the pelvis and axial projections of the hip which had been operated on after 6 weeks, and after 4, 8 and 12 months, following which follow-up was annual (Table 2), with no follow-up losses to date.
Paprosky classification.
| Type | Characteristics |
|---|---|
| I | Minimum deformity, osteolysis around the anchorage cement holes |
| II | Defects with superior migration under 2cm |
| IIA | Superomedial defects |
| IIB | Superolateral defects |
| IIC | Medial migration running over the Kohler line (protrusion) from tear drop destruction |
| III | Superior migration over 2cm |
| IIIA | Associated with superolateral migration with under 15mm of ischiatic lysis below the superior obturator line, medial tear drop destruction. |
| IIIB | Superomedial migration with extensión of the component beyond the Kohler line and ischiatric lysis above 15mm below the obturator line, complete tear drop destruction. |
| Pelvic discontinuity |
Source: Paprosky et al.6.
.
| Variable (n=22) | |
|---|---|
| Sex | Female (14) |
| Male (8) | |
| Mean age of intervention in years | 72 (40–89) |
| Cause of the revision surgery | Acetabular loosening (17) |
| Acetabular fracture (2) | |
| Second time through reimplantation from infection (3) | |
| Acetabular defect (Paprosky) | IIIA (8) |
| IIIB (9) | |
| Pelvic discontinuity | 5 |
| Diameter of femoral head | 28mm (14) |
| 32mm (6) | |
| 36mm (2) | |
| Acetabular intervention time in surgery | 85min (115–70) |
| Merle d’Aubigné-Postel | Preop 6.91 |
| Postop 14.36 | |
| Time since previous surgery | 10 years (7–18 years) |
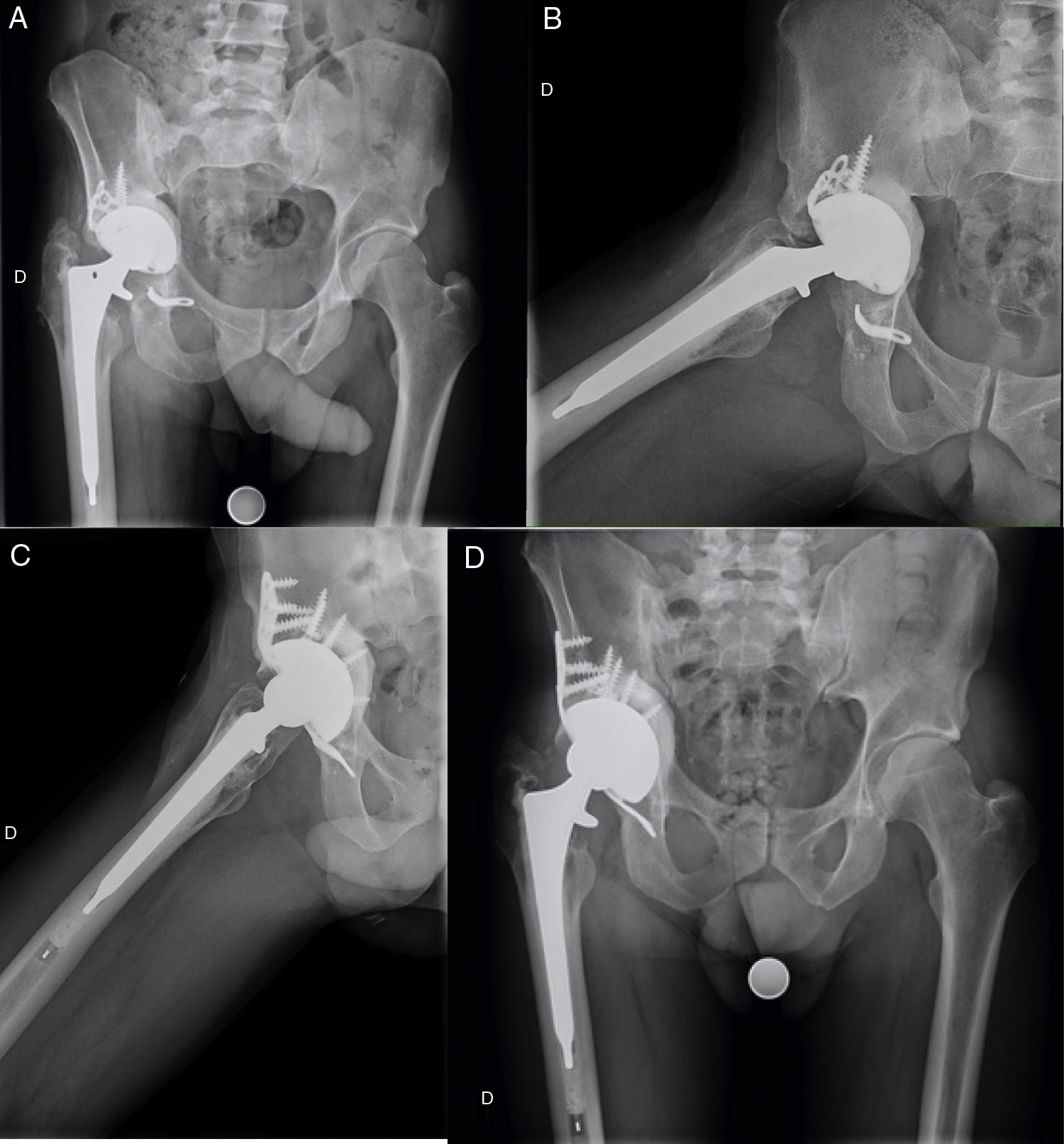
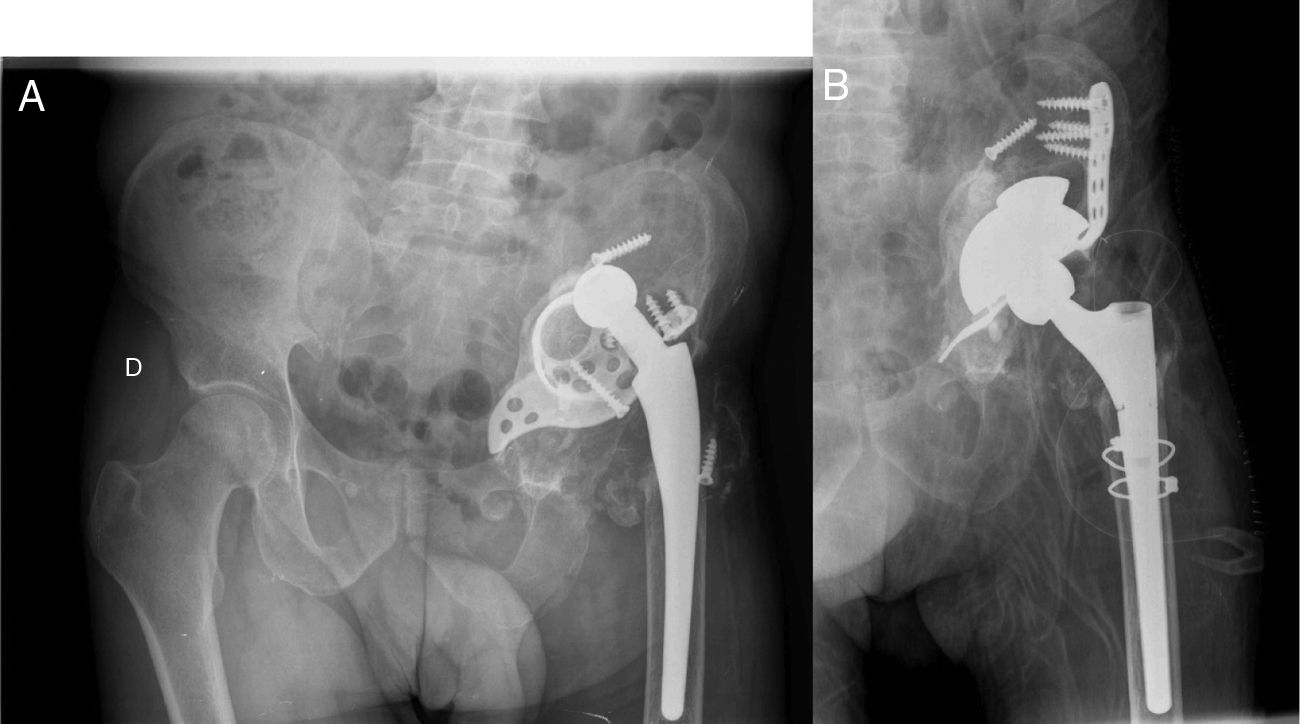
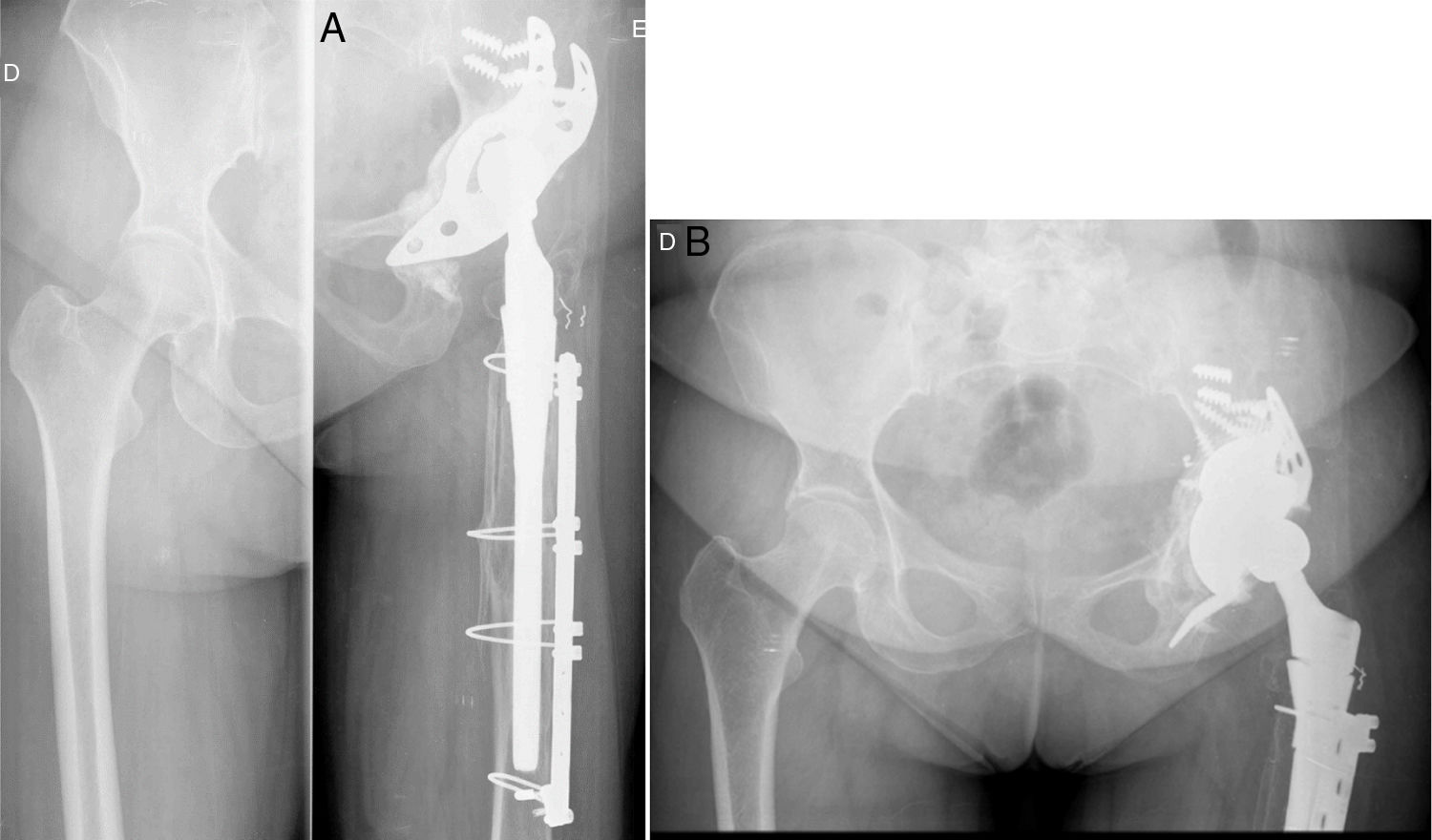
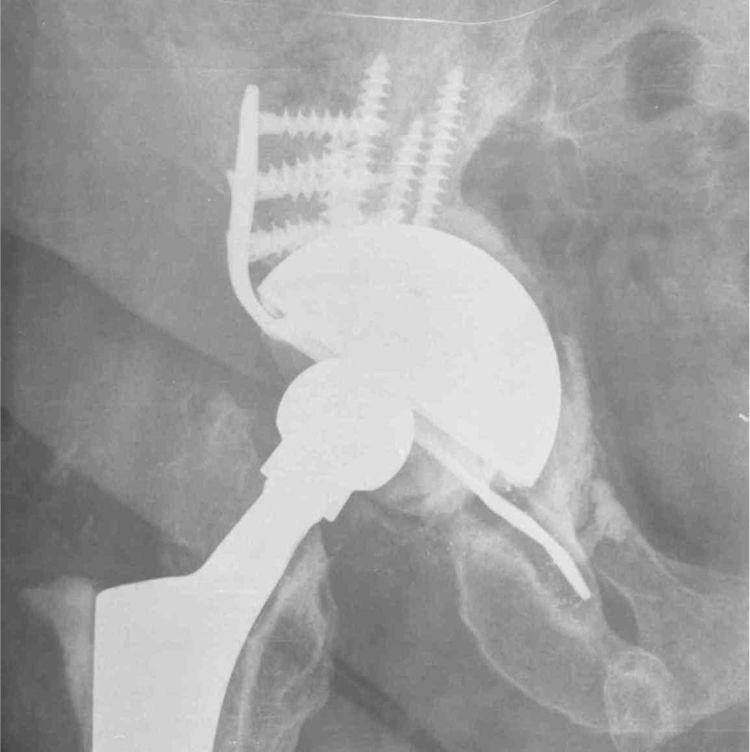
Pelvic discontinuity diagnosis was undertaken by intraoperative events, together with the radiologic study prior to surgery, including computerised tomography in all cases. Following the removal of the old acetabular component, pelvic discontinuity was confirmed when shifting between the proximal and distal section of the acetabulum was proven. In one case, the discontinuity was due to an acetabular fracture when the acetabular component was impacted from a total primary hip replacement in a patient with Paget's disease. In another case this was due to an acetabular pseudo-osteoarthritis after a fracture treated with THR 20 years previously and in a third case pelvic discontinuity was due to fractures of the 2 acetabular columns and fossa 2 weeks after implantation of a primary THR. In the remaining cases the causes of pelvic discontinuity were osteolysis and loosening of the acetabular component (Figs. 1–4).
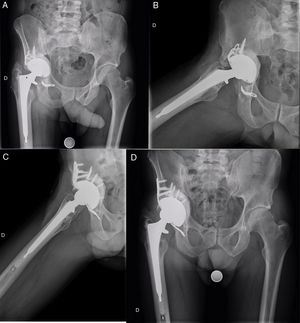
A 40 year-old patient with rheumatoid arthritis in whom total primary hip replacement was implanted in 2003. They later required a cup replacement with a bone graft due to aseptic loosening in 2008. In 2010 they required another cup replacement with bone graft and implantation of a Bat-Cup type reinforcement ring due to aseptic loosening with acetabular protrusion. This also failed in 2012 with implant rupture and aseptic loosening, which was why the Cup-Cage was implanted. Images A and B show the radiographies in anteroposterior and axial projections, respectively, where acetabular loosening with rupture of the ring ischiatic insertion may be observed. Images C and D correspond to radiographic control in the axial and anteroposterior projections 3 and a half years after Cup-Cage implantation, with appropriate integration of the acetabular graft and good implant positioning.
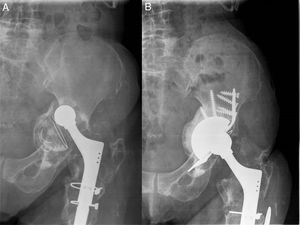
(A) Anteroposterior radiography of a patient who underwent surgery in another centre. Loosening and migration of the acetabular ring is observed. (B) Postoperative radiography after revision with metal trabecular cup with a superior supplement, Cup Cage and bone graft. Correct filling of the acetabular fossa and correct positioning of the implant.
An anterolateral approach was used in all cases. After luxation and posterior exposure of the acetabulum, the component was removed, together with nearby membranes and fibrous tissue. Once the bone tissue was exposed, the size of the bone defect and stability was confirmed to rule out or diagnose a pelvic discontinuity using a trial implant.
After this we inserted a ground allograft to partially fill the defect area, impacted through reverse-mode reaming. We then proceeded to insert, impact and affix the trabecular metal acetabulum. Once in place the Cup-Cage reconstruction construct was implanted inside it, with ischiatic anchorage, with the help of a specific osteotome (under fluoroscopic guidance) and implantor screws in the ilium for good implant stability.
Lastly, the cemented polyethylene insert (Longevity®) was able to correct orientation to obtain good joint stability. In 2 cases the size of the ring allowed for the use of a dual mobility cemented insert (Avantage®, Zimmer Biomet).
Postoperative care consisted of early mobility with the use of 2 sticks for 4 weeks and progressive removal of them for up to 8 weeks. All patients received prophylactic antibiotics with intravenous cefazolin (2g preoperatively and a three-in-one dose of 1g every 8h postoperatively) and anticoagulant therapy at prophylactic doses (40mg enoxaparin) for 4 weeks.
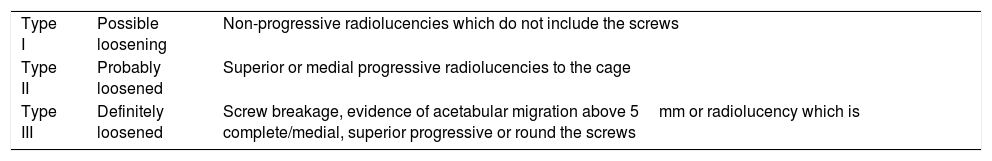
Radiologic evaluation was performed after 6 weeks, and after 4, 8 and 12 months and then at subsequent anual check-ups with anteroposterior and lateral projections of the hip and anteroposterior of the pelvis, with Gill criteria on acetabular loosening as our base8 (Table 3). Particular evaluation was made of the presence of acetabular migrations of over 5mm, the presence of circumpherential radiolucencies, screw lysis and signs of corrosion, together with recovery of the hip rotation centre.
Gill criteria.
| Type I | Possible loosening | Non-progressive radiolucencies which do not include the screws |
| Type II | Probably loosened | Superior or medial progressive radiolucencies to the cage |
| Type III | Definitely loosened | Screw breakage, evidence of acetabular migration above 5mm or radiolucency which is complete/medial, superior progressive or round the screws |
Source: Gill et al.8.
We consider radiologic failure as the observation of Cup-Cage migration by 3mm or more shortly after surgery, with progression of the same for the first 2 years. Massin et al.9 consider that migrations under 3mm are within the margin of error of measurement and radiographic techniques.
Statistical analysisStatistical analysis was performed using the Kaplan–Meier survival curve, with a 95% confidence interval and the Student's t-test for comparison of means.
ResultsDuring surgery it was observed that during implantation of the final trabecular metal cup, the amount of contact it had with the patient's bleeding bone was lower than 50% in all cases. The ground allograft was used in all cases and in 8 of them demineralised marrow bone replacement was added (DBX®, Synthes); a structural graft was not used in any of the cases. The femoral component was also replaced in 18 cases in the same surgical intervention.
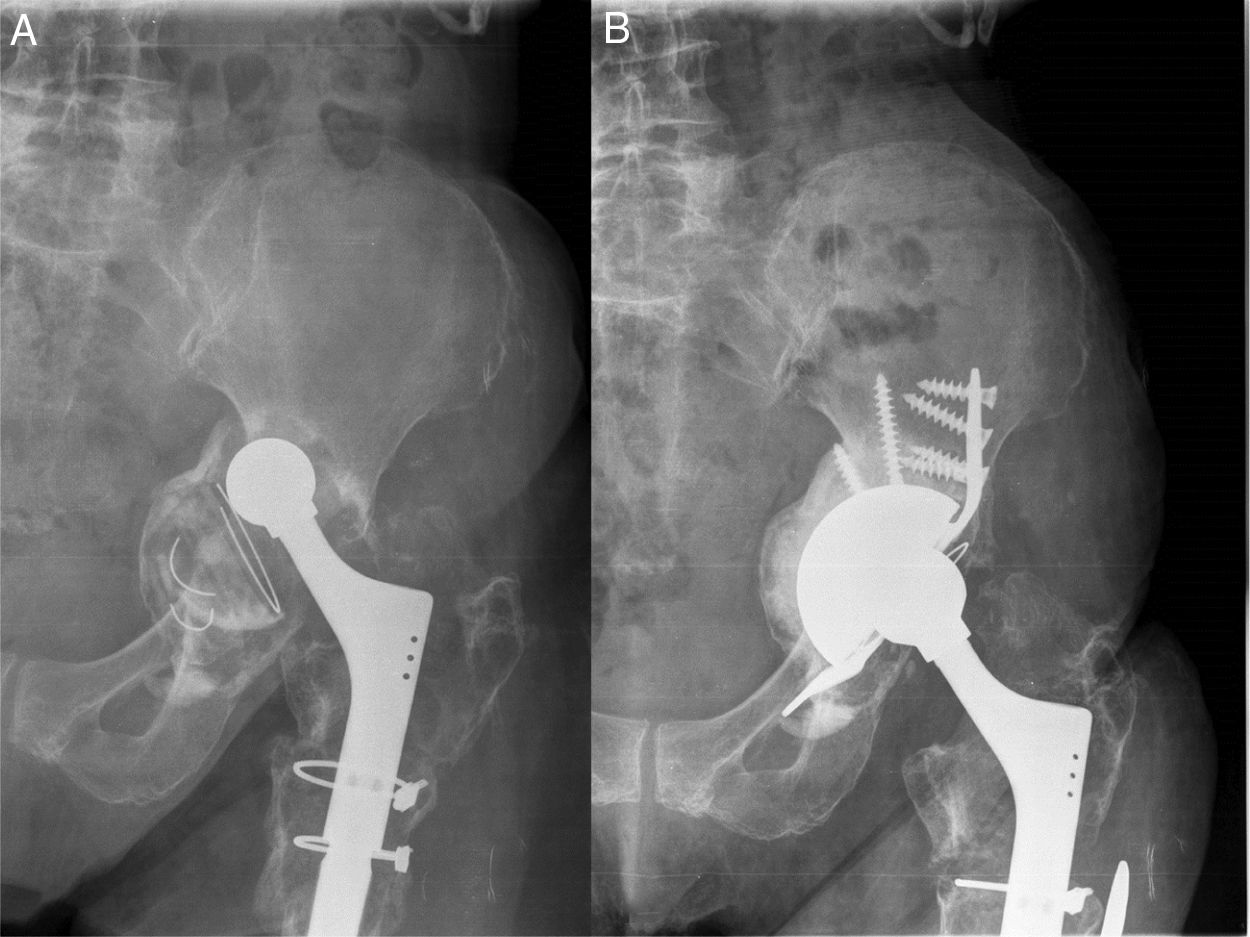
Average follow-up time was 45.06 months (12–73 months), during which no Cup-Cage impairment occurred. At the end of the follow-up there were 3 surgical reinterventions (13.63%): one case of infection where debridement and targeted antibiotic treatment was used; a second case where a recurrent dislocation presented (2 episodes of dislocation) and the patient was reoperated with a replacement of the polyethylene and a larger femoral head; and a third case presented with repeated episodes of subluxation, with no episodes of complete luxation, and this required replacement of the polyethylene and head due to poor range of movement from initial surgery (Fig. 5). Reintervention was not required in any cases for loosening or migration of the Cup-Cage construct.
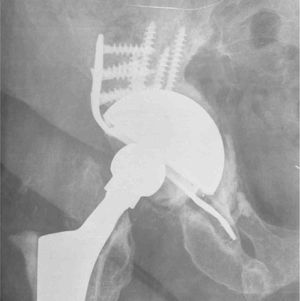
Patient aged 49 years with THR implanted in another hospital 20 years previously, after an accident. (A) Anteroposterior radiograph where shifting of the actabular component is observed, with evidence of pelvic discontinuity due to a pseudo osteoarthritis. (B) Immediate postoperative anteroposterior radiography. (C) Radiographic control after 6 months, with polyethylene decementing. (D) Radiographic control in the immediate postoperative period after the polyethylene replacement.
An improvement was observed in the Merle d’Aubigné-Postel score from 6.91 to 14.36 and in the range of motion score subcategory from 2.91 to 4.36 on average of preoperative and postoperative scales, respectively. The Harris Hip Score significantly improved from a mean of 30 (16–55, SD 10) in the preoperative period to 72 (40–90, SD 15) in the postoperative period, with p=0.001.
Regarding postoperative radiologic control, in no cases was there any movement of over 5mm nor loosening of the Cup-Cage. Recovery of the centre of rotation with a reduction of the vertical distance with the tear drop of 3.5cm at a mean of 1.2cm was obtained. We found one case of local osteolysis around the ischiatric insertion of the Cup-Cage within the context of a prosthetic replacement due to infection, without progression over time and without any medical interpretation. We did not find any cases of screw or implant rupture (Fig. 6).
The survival curves to date are 100%, with no apparent mechanical loosening or deep infection.
DiscussionThe Cup-Cage technique was developed to improve biological attachment of ring reconstructions in major acetabular defects and in pelvic discontinuities. Standard techniques for pelvic discontinuity have not been known to present with very good short and midterm results due to the lack of biological attachment of the implant.10 Villanueva et al.,11 in a review on pelvic discontinuity treatment, concluded that the rate of implant failure was due to biological rather than mechanical factors, and therefore new treatment opportunities should be studied aimed at achieving good osseointegration of the implants. This is improving with the trabecular metal cages. Van Haaren et al.12 studied a series of 71 cases of acertabular replacement with impacted graft combined with a cemented acetabular component. They obtained a survival rate of 72% after 7.2 years of follow-up (1.6–9.7 years); 20 cases required surgical reintervention (70% with type II and IV acetabular defects according to the AAOS classification). They thus concluded that the impacted osseous graft had a high risk of failure and complications, especially in cases of massive acetabular defects and pelvic discontinuities.
The use of ground or structural bone grafts protected by a ring has also had limited results. In a series of 24 type III and IV acetabular defects according to the AAOS classification Buttaro et al.13 opted for acetabular reconstruction using impacted bone graft with a type GAP II reconstruction cage, with a failure rate of 37% (9 cases) after 34 months mean follow-up (24–72 months), 6 of which underwent rescue surgery with a metal trabecular cage.
Goodman et al.14 reported 50% failures in cases of pelvic discontinuity treated with illioischiatic cages. This was a retrospective study of 61 acetabular reconstructions using reconstruction rings, 10 of which presented with pelvic discontinuity. They obtained a satisfactory result in 76% of total cases, but 8 of the 10 pelvic discontinuities presented with some type of complication (3 loosening, 2 of them persistent with the pelvic discontinuity; 2 implant flap fractures and 3 luxation) and only 5 out of the 10 had a satisfactory result after follow-up.
Paprosky et al.15 also reported a 50% failure in a series of 16 pelvic discontinuities treated with different cages, including the Gap II Restoration cage (Osteonics), Reconstruction cage (De Puy), Burch-Schneider (Protek) and Ganz (Protek) ring. Five cases required surgical reintervention (one from infection and 4 from aseptic loosening, 3 of which presented with reconstruction cage fractures) and in 3 cases aseptic loosening was observed which did not require reintervention during the study period (a broken cage was observed in one of them).
Cup-Cage reconstruction technique is promising in the treatment of massive acetabular defects (Paprosky III-B). The porous tantalum cup is unladen and protected by an underlying ring attached to the illium and ischium. Standard rings usually have high failure rates, as previously commented upon, and the theory therefore is that the porous tantalum cup obtains a stable attachment thanks to this protection and this is able to achieve correct osseointegration of the implant. Kosashvili et al.4 obtained favourable results in clinical improvement and quality of life in 88.5% of cases of a series of 26 pelvic discontinuities treated with a trabecular metal shell combined with an allograft and protected by a Cup-Cage. Hipfl et al.5 obtained an 89% survival rate at 5 years in a series of 35 cases of massive acetabular defects and pelvic discontinuities treated by using the Cup-Cage system, without any cases of aseptic loosening replacements.
Since 2003, the majority of pelvic discontinuities have been treated with reconstruction rings, although not all authors use the Cup-Cage. This implant would be indicated in cases where bone stock is not sufficient for obtaining enough initial stability with the use of a trabecular metal cup with or without tantalum boosters.
The Cup-Cage insertion technique has already been previously described by other authors,4,10,16,17 although some use the acetabular distraction technique for chronic pelvic discontinuity treatment, aimed at achieving appropriate initial mechanical stability to allow for bone growth inside, and therefore bypass the discontinuity.
Highly porous tantalum components now manufactured are gaining ground in revision surgery of total hip replacements due to their high capacity in achieving bone growth thanks to their biomechanical properties, including high porosity, high friction coefficient and an elasticity which is similar to the subchondral bone.18–23
Previous studies indicate that bone growth may be achieved through the use of trabecular metal components under unfavourable conditions with limited contact with bleeding bone, which usually accompanies pelvic discontintuities.4,21,23–26
Personalised acetabular components with trabecular metal and 3D manufacture are another option for the treatment of pelvic discontinuities. This is a porous acetabular component designed on a three-dimensional model of the pelvis based on prior computerised tomography of the patient's pelvis. Taunton et al.27 reported 57 pelvic discontinuities treated with this implant; 81% resolved the pelvic discontinuity with stable components after 65 months follow-up. It is notable that there was a 21% postoperative instability, which required surgical reintervention in 10 out of the 12 cases. Other authors also described good short and midterm results with these implants for massive acetabular defects and pelvic discontinuities.28–30 The disadvantages of this method is that considerable time is required to construct the implant (around 4 weeks) and its high cost, and the advantage is that the defect may be reconstructed regardless of its size.
In our series, the Cup-Cage technique provides satisfactory results for the treatment of massive acetabular defects and pelvic discontinuities, with a survival rate of 100% at 45.06 months of midterm follow-up, and without the need for removal of the material in any cases, but with complications arising from the actual revision surgery, such as instability and infection. In a study on biomechanics, Gililland et al.31 showed that the stiffness of attachment obtained in the pelvic discontinuities using the Cup-Cage was similar to the combination of a standard ring associated with a posterior column plaque. The tantalum acetabulum combined with a tantalum ring increased vertical stability through a moderate distraction of the discontinuity,4 and also led to an increase in bone on both surfaces of the discontinuity, bypassing the defect.32 The high percentage of discontinuity recovery was probably explained by the stability of the system once bone growth occurred, which unloads the medial graft during osseointegration.16 In contrast, attachment of standard rings depends on the upper segment screws and ischiatic attachment. This may lead to initially suboptimal stability, with interfragmentary movements of the discontinuity which may lead to reconstruction failure. Recently, Rogers et al.,32 in a series of 62 pelvic discontinuities treated with Cup-Cage or standard rings, obtained a mean follow-up of 35 months and a revision rate of 9.5% versus 29%, respectively.
A notable limitation of our study is that it was retrospective with a short case series, because this technique is only used in a very specific patient profile, in massive acetabular defects and pelvic discontinuities, with the Cup-Cage, in our opinion, being the best therapeutic solution. The versatility of the tantalum boosters has much diminished the need to use this implant due to the large variety of acetabular defect reconstruction options it offers. A further limitation is that follow-up time was not very long, although it was sufficient to provide information on the favourable outcomes obtained in the short and midterm of acetabular reconstruction with massive bone defects and pelvic discontinuities using the Cup-Cage system, because the reconstruction of pelvic stability is the primary objective and is achieved during the first few months. Also, this technique requires a high learning curve, and due to the low number of patients with pelvic discontinuity, it is not advisable that it be undertaken by surgeons who are not experts in prosthetic revision surgery.
ConclusionsAcetabular reconstruction in total hip revision surgery requires correct preoperative and intraoperative classification of the size and location of the bone defects and an evaluation of the presence or non-presence of pelvic discontinuity in order to select the most appropriate implant for reconstruction. Whenever possible the bone defect should be repaired and the centre of hip rotation, and discrepancies in length of lower limbs should be eliminated. For pelvic discontinuities and massive acetabular defects we can say that acetabular reconstruction using a metal trabecular cup combined with Cup-Cage offers good short and midterm results. However this is a complex technique and requires a high learning curve and experience in acetabular revision surgery.
Level of evidenceLevel of evidence IV.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Fraile Suari A, Marqués López F, Cuenca Llavall M, Tey Pons M, León García A. Reconstrucción acetabular con el sistema Cup-Cage para discontinuidades pélvicas y defectos acetabulares masivos. Rev Esp Cir Ortop Traumatol. 2020;64:64–73.