Complex femoral defects with insufficient isthmus (Paprosky III and IV) and Vancouver B3 periprosthetic fractures determines the fixation of the revision stems.
The objective is to evaluate the results of the modular revision stems with diaphyseal anchor and distal block (Revitan Zimmer Biomet GmbH, Winterthur, Switzerland). Our hypothesis is that this procedure offers a stable primary fixation in cases of alteration of the femoral isthmus.
Material and methodsRetrospective cohort study of 38 patients, minimum follow-up of 12 months (12–94) with severe femoral defects treated with Revitan stems distally blocked. An endofemoral or transfemoral approach was used. The subsidence was assessed according to Callahan’s method and bone neoformation according to Nordin. Merle d’Aubigné-Postel was used and complications and reoperations were collected. A statistical analysis was performed with SPSS and a significance level p < 0.05 was considered.
ResultsBetween 2009 and 2017, 147 revisions were carried out with Revitan stem, 38 locked, 23 men and 15 women, with an average age of 74 years and an average follow-up of 64 months. The cause of the review was: 15 septic loosenings, 14 aseptic, two fractures and seven stable fibrous unions. Right fixation was obtained in 27 cases, there were four loosenings, three screw breakages, three infections, one of dislocation and one of femoral nerve injury. The MDP increased significantly from 11.26 to 14.98.
ConclusionsDistally locked conical modular stems are a good alternative in femoral defects with isthmus involvement if proper canal filling and bicortical screw fixation are achieved.
Los defectos femorales complejos con istmo insuficiente (Paprosky III y IV) y fracturas periprotésicas B3 de Vancouver condicionan la fijación de los vástagos de revisión.
El objetivo es evaluar los resultados de los vástagos de revisión modular de anclaje diafisario con bloqueo distal (Sistema Revitan Zimmer Biomet GmbH, Winterthur, Suiza). Nuestra hipótesis es que ofrecen una fijación primaria estable en casos de afectación del istmo femoral.
Material y métodosEstudio de cohortes retrospectivo de 38 pacientes, seguimiento mínimo de 12 meses (12–94) y defectos femorales severos tratados con vástagos Revitan encerrojados. Realizamos una vía endofemoral o una transfemoral. Valoramos el hundimiento según el método de Callahan y la neoformación ósea según Barnett y Nordin. Se utilizó la escala Merle d’Aubigné-Postel y se recogieron las complicaciones y reintervenciones. Se realizó un análisis estadístico con SPSS y un nivel de significación p < 0,05.
ResultadosEntre 2009 y 2017 se realizaron 147 revisiones con vástago Revitan, 38 encerrojados, 23 hombres y 15 mujeres, edad media de 74 años y seguimiento medio de 64 meses. Las causas de revisión fueron: 15 aflojamientos sépticos, 14 asépticos, dos fracturas y siete fijaciones fibrosas estables. Obtuvimos una correcta fijación en 27 casos; hubo cuatro aflojamientos, tres roturas de tornillos, tres infecciones, una luxación y una lesión del nervio femoral. El MDP mejoró de forma significativa de 11,26 a 14,98.
ConclusionesLos vástagos modulares cónicos encerrojados son una buena alternativa en los defectos femorales con afectación ístmica si se consigue un correcto relleno del canal y una fijación bicortical de los tornillos.
The hip revision prostheses indicated in severe femoral defects with insufficient isthmus (Paprosky IIIB and IV)1,2 and in Vancouver B2 and B33 periprosthetic fractures are a major problem for the orthopaedic surgeon due to their technical complexity. At present we have the following surgical alternatives: mega prosthesis with proximal femur, massive proximal allografts, impacted graft technique with long cemented stems and modular diaphyseal anchor stems.4,5 The cases with a deficient isthmus, less than 6 cm and wide channels, more than 18 mm, make the rotational stability of the implants very difficult.6
Sotereanos et al.7 describe satisfactory results with hydroxyapatite-coated titanium prostheses, with distal, custom-made locking screws. Fink et al.6 report good results with the modular curved prosthesis with diaphyseal anchor, Revitan (Zimmer Biomet), with the additional use of distal cross-locking screws in cases of severe isthmic involvement.
The objective of this study was to evaluate the clinical results and complications of femoral defects treated with the Revitan revision stem with diaphyseal anchor and distal locking screws in our department. The hypothesis of our paper is that distal locking with screws provides stable fixation of the implant with a good functional outcome.
Material and methodsRetrospective cohort study of 38 patients with severe femoral defects with a minimum follow-up of 12 months, in which a Revitan modular conical femoral revision stem was implanted with a minimum of two distal locking screws.
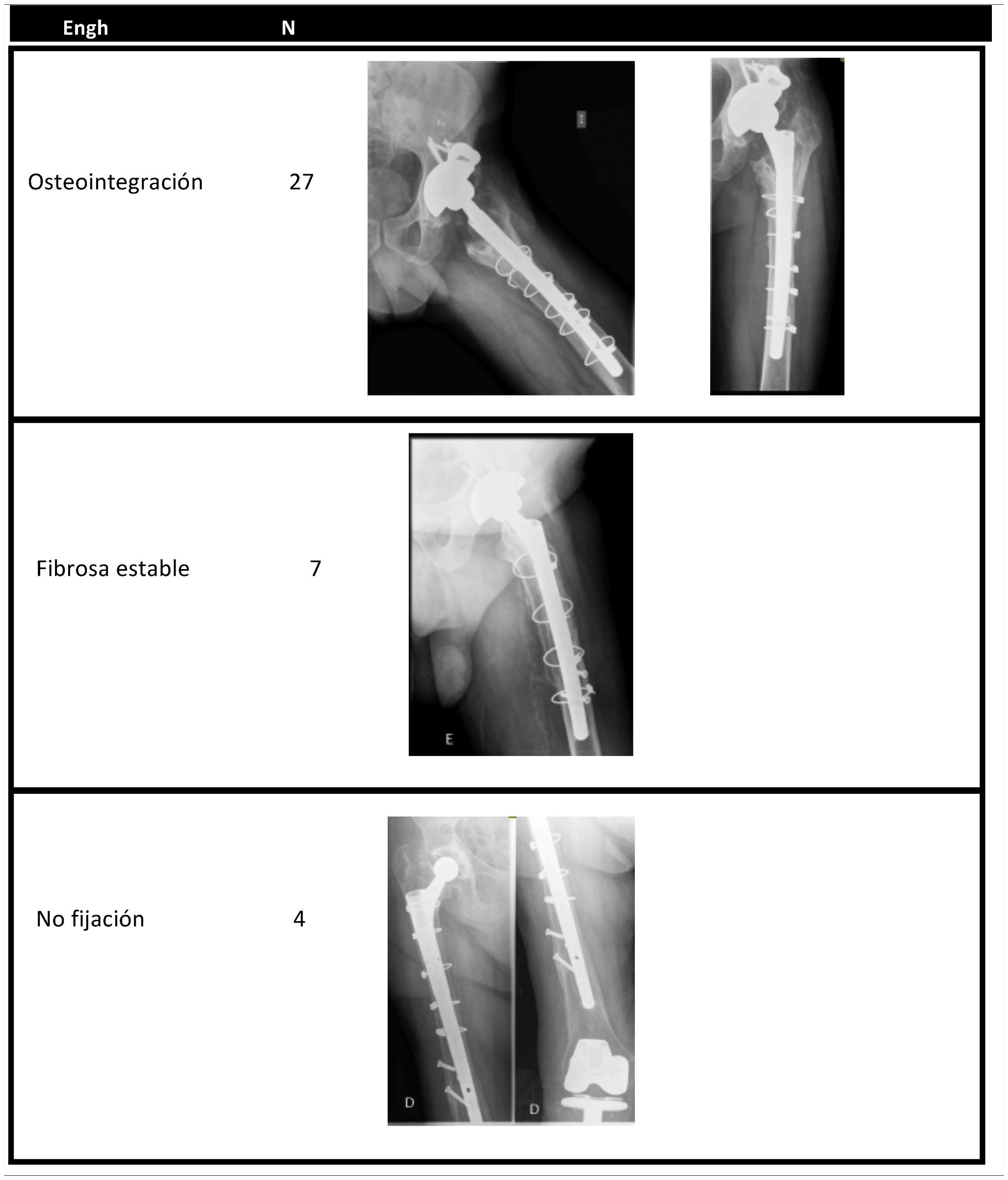
Femoral defects were classified according to the scale by Paprosky et al.1,2 and periprosthetic fractures according to the Vancouver classification.3 The “h” distance (distance from the tip of the trochanter to the most distal point of the osteotomy) was measured in the preoperative planning for extended osteotomy; in cases where the healthy isthmus was less than 4 cm, locking with screws was mandatory. The bone fixation obtained was evaluated according to the classification of Engh et al.8 and the functional result was assessed with the Merle d’Aubigné-Postel (MDP) scale).9 The type and number of medical and mechanical complications were assessed, as well as the number of re-interventions.
The modular curved stem with conical striated distal anchor (Zimmer Biomet), has three titanium femoral anchor components with longitudinal striations of 140, 200 and 260 mm of various gauges, from 16 to 26 mm, combined with different proximal bodies, from 55 to 105 mm, to achieve a correct version and length of the limb. We also have the possibility of placing distal locking screws with gauge of 4.9 mm (three static and dynamic holes), through an automated system with the insertion instruments. The possibility of distal locking is reserved for the use of 200 and 260 mm long rods with a minimum gauge of 18 mm.
The surgeries were performed by three expert hip revision surgeons using two different approaches. The first was the endofemoral approach, after extraction of the prosthetic component. And the second was to perform an extended osteotomy, previously planned, completed at a proximal level following the fracture line in cases of periprosthetic fracture. In all cases, the shortest and thickest possible distal implant was chosen, to limit fixation to a minimum of 4 cm in the femoral isthmus, previously placing a prophylactic cerclage wire to prevent intraoperative fractures. In locked cases the insertion device was used, implanting in all cases two static bicortical locking screws in the lateral-medial plane. Once locked, the appropriate proximal component was chosen for correct reconstruction. The cases which required an extended osteotomy were fixed after reduction of the prosthesis, with two or three cerclage wires. Weight-bearing of 30% body weight was authorised postoperatively, using two crutches, until the sixth postoperative week, limiting flexion of the hip to 70° for the same period.
All the patients were clinically and radiologically examined before surgery and at 3, 6 and 12 months after surgery and every two years thereafter. The radiological tests were evaluated by two different previously trained surgeons, independent of the study. Standard radiographs of the hip in two planes (antero-posterior and lateral femur) were used. The consolidation of the osteotomy or fracture and the correct position of the screws through the two cortices were assessed. Stem failures were assessed using the technique of Callaghan et al.10 Barnett and Nordin thickness11 was calculated immediately postoperatively and one year after the operation, analysing the proximal bone formation according to Böhm and Bischel12,13 and McInnis et al.14 The sum of the thickness of the medial and lateral cortices of the femur at the level of the lesser trochanter was divided by the total diameter of the femur at the same level and its fraction was multiplied by 100.
SPSS for Windows (SPSS Inc., Chicago Ill) was used for the statistical study. The level of statistical significance was established at p < .05.
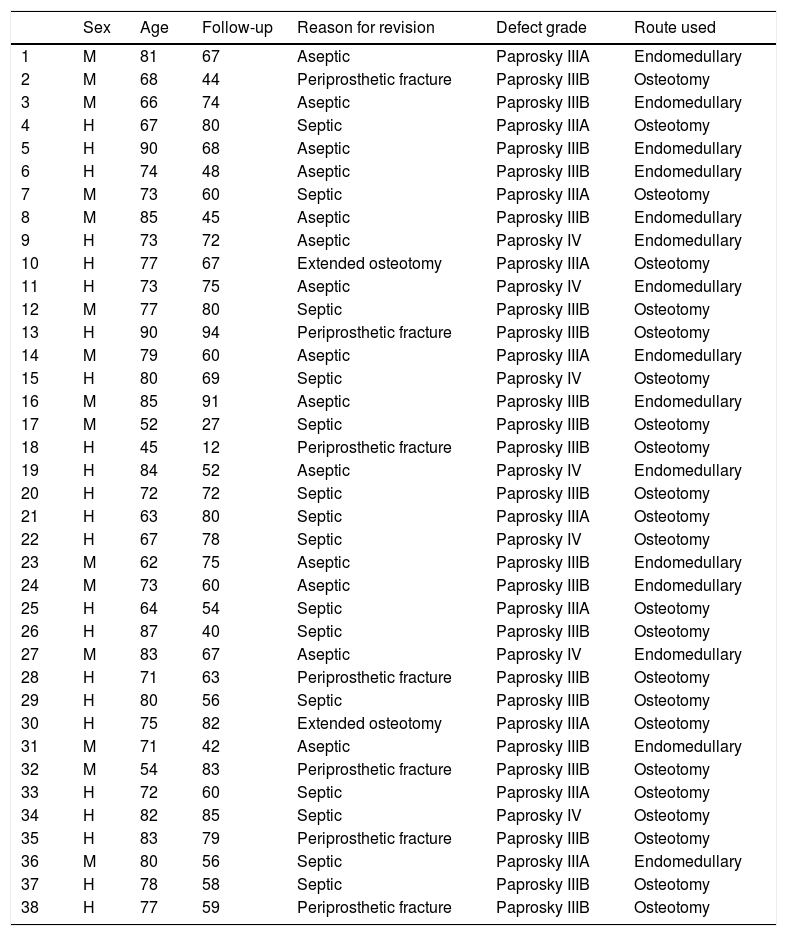
ResultsBetween 2009 and 2017, 147 femoral revisions were performed using the Revitan curved stem in 38 patients (25.85%). The cohort comprised 23 men and 15 women with a mean age of 74 years (45–90 years), with an average follow-up of 64 months (12–94 months). The reasons for revision were 15 cases of septic loosening (39.47%), 14 cases of aseptic loosening (36.8%), seven periprosthetic fractures (18.4%), and two cases of long extended osteotomy (5.2%). The average number of previous prosthetic replacements was 2.7. Regarding the approach used, in 23 cases (60.5%) an extended femoral osteotomy was performed and in 15 cases an endofemoral approach (39.5%). The femoral bone defect according to Paprosky was IIIA in 10 patients (26.3%), IIIB in 21 (55.2%) and IV in seven (18.4%). The seven cases of periprosthetic fractures were Vancouver type B2 (100%) (Table 1). With regard to bone fixation according to Engh et al.,8 osseointegration was obtained in 27 cases (71%), stable fibrous fixation in seven cases (18.4%) and in four cases osseointegration was not achieved (10.5%), and breakage of the distal screws and subsidence of the stem by a mean 15 mm (10–18 mm) (Table 2) was observed. In one of the four cases with screw failure, the screws did not exceed the medial cortex, losing their bicorticality.
Results.
| Sex | Age | Follow-up | Reason for revision | Defect grade | Route used | |
|---|---|---|---|---|---|---|
| 1 | M | 81 | 67 | Aseptic | Paprosky IIIA | Endomedullary |
| 2 | M | 68 | 44 | Periprosthetic fracture | Paprosky IIIB | Osteotomy |
| 3 | M | 66 | 74 | Aseptic | Paprosky IIIB | Endomedullary |
| 4 | H | 67 | 80 | Septic | Paprosky IIIA | Osteotomy |
| 5 | H | 90 | 68 | Aseptic | Paprosky IIIB | Endomedullary |
| 6 | H | 74 | 48 | Aseptic | Paprosky IIIB | Endomedullary |
| 7 | M | 73 | 60 | Septic | Paprosky IIIA | Osteotomy |
| 8 | M | 85 | 45 | Aseptic | Paprosky IIIB | Endomedullary |
| 9 | H | 73 | 72 | Aseptic | Paprosky IV | Endomedullary |
| 10 | H | 77 | 67 | Extended osteotomy | Paprosky IIIA | Osteotomy |
| 11 | H | 73 | 75 | Aseptic | Paprosky IV | Endomedullary |
| 12 | M | 77 | 80 | Septic | Paprosky IIIB | Osteotomy |
| 13 | H | 90 | 94 | Periprosthetic fracture | Paprosky IIIB | Osteotomy |
| 14 | M | 79 | 60 | Aseptic | Paprosky IIIA | Endomedullary |
| 15 | H | 80 | 69 | Septic | Paprosky IV | Osteotomy |
| 16 | M | 85 | 91 | Aseptic | Paprosky IIIB | Endomedullary |
| 17 | M | 52 | 27 | Septic | Paprosky IIIB | Osteotomy |
| 18 | H | 45 | 12 | Periprosthetic fracture | Paprosky IIIB | Osteotomy |
| 19 | H | 84 | 52 | Aseptic | Paprosky IV | Endomedullary |
| 20 | H | 72 | 72 | Septic | Paprosky IIIB | Osteotomy |
| 21 | H | 63 | 80 | Septic | Paprosky IIIA | Osteotomy |
| 22 | H | 67 | 78 | Septic | Paprosky IV | Osteotomy |
| 23 | M | 62 | 75 | Aseptic | Paprosky IIIB | Endomedullary |
| 24 | M | 73 | 60 | Aseptic | Paprosky IIIB | Endomedullary |
| 25 | H | 64 | 54 | Septic | Paprosky IIIA | Osteotomy |
| 26 | H | 87 | 40 | Septic | Paprosky IIIB | Osteotomy |
| 27 | M | 83 | 67 | Aseptic | Paprosky IV | Endomedullary |
| 28 | H | 71 | 63 | Periprosthetic fracture | Paprosky IIIB | Osteotomy |
| 29 | H | 80 | 56 | Septic | Paprosky IIIB | Osteotomy |
| 30 | H | 75 | 82 | Extended osteotomy | Paprosky IIIA | Osteotomy |
| 31 | M | 71 | 42 | Aseptic | Paprosky IIIB | Endomedullary |
| 32 | M | 54 | 83 | Periprosthetic fracture | Paprosky IIIB | Osteotomy |
| 33 | H | 72 | 60 | Septic | Paprosky IIIA | Osteotomy |
| 34 | H | 82 | 85 | Septic | Paprosky IV | Osteotomy |
| 35 | H | 83 | 79 | Periprosthetic fracture | Paprosky IIIB | Osteotomy |
| 36 | M | 80 | 56 | Septic | Paprosky IIIA | Endomedullary |
| 37 | H | 78 | 58 | Septic | Paprosky IIIB | Osteotomy |
| 38 | H | 77 | 59 | Periprosthetic fracture | Paprosky IIIB | Osteotomy |
The MDP thickness increased significantly from 11.26 (SD 3.02) to 14.98 (SD 2.9) with a p < .05.
In all the cases of periprosthetic fractures and extended osteotomies, bone consolidation was obtained.
The Barnett and Nordin11 thickness was very variable, given the heterogeneity of the cases; presenting a reduction of 1.97 8.4 (−17 to 11); and the patients with a Paprosky type IV femoral defect, due to the greater bone defect, presented the greatest reduction, without being statistically significant (p = .16), due to the lower number of cases.
Regarding complications, we observed two cases of acute infection, which required debridement and replacement of mobile parts; one chronic infection, which required suppressive antibiotic treatment; one inveterate hip dislocation; and one crural nerve paralysis, which resolved spontaneously. As intraoperative complications we had three cases of femoral fracture, which required the placement of supplementary cerclage wires. None of the patients were re-operated due to failure of the femoral fixation, since, despite the subsidence and poor functional outcome, the patients refused surgery. All of them are being followed-up clinically and radiographically in our centre.
DiscussionDistal fixation with conical stems has been shown to be useful in femoral revision surgery in patients with large bone defects, since it guarantees good implant stability, promoting new formation of proximal bone.15 The minimum length of the preserved femoral isthmus, established to provide fixation and stability of the implant, has varied according to different authors in recent years. Wagner and Wagner15 described a minimum of 6 cm, while Paprosky and Burnett reduced it to 4 cm in his description of the classification of femoral bone defects.2 The problem lies in type IIIB and IV bone defects and in type B2 and B3 periprosthetic fractures with great involvement of the femoral isthmus, where this stability may be compromised. There are different surgical options for their treatment, such as impacted graft and femoral stem techniques, femoral mega prosthesis, massive allografts, composite prosthesis, long hydroxyapatite coated stems with distal locking screws and curved conical stems with distal locking screws.
Interlocking screws provide increased rotational and axial stability of the femoral component. Mahomed et al.16 report a 320% increase in torsional stability and 230% increase in axial stability with the use of distal locking screws.16 Other biomechanical studies, such as that by Ellenrieder et al.,17 report a high incidence of proximal bone resorption (stress shielding) with supplemental distal locking, and also other authors such as Barnett and Nordin,11 Fink et al.6 and Fraile Suari et al.18 in long distal fixations. Despite this increase in stability, correct filling of the canal with an appropriate intraoperative anchor (press-fit) is mandatory with the cone-on-cone technique, avoiding mechanical failures due to overloading of the screws. Learmonth19 reports screw breakage in five of 22 type B2 periprosthetic fractures, due to the use of undersized rods with little canal filling. However, the presence of residual cement or communication of the fracture and/or osteotomy beyond the necessary 4 cm of healthy isthmus contributes to mechanical failures and subsidence of the femoral stem.18 In our case series, due to the characteristics of the implant used, lengths of the distal component of 200 mm and 260 mm and a minimum gauge of 18 mm could explain the presence of intraoperative fractures and the proximal cortical atrophy (bone resorption) observed. The four cases of fixation failure and non-osseointegration (10.5%) with screw breakage occurred in patients with greater bone defect due to repeated surgeries, greater osteoporosis, history of septic replacement, insufficient canal filling, and short screws that caused subsidence of the stem.
The use of long diaphyseal anchor stems coated with hydroxyapatite has allowed stable fixations, with little proximal bone resorption and few mechanical bolt failures, using smaller gauges (18 mm for locking).19 In their study of 100 cases, Carrera et al.20 observe two stem breaks and one case of screw breakage; the authors report that the additional hydroxyapatite coating would allow rapid osseointegration with less canal filling, thus avoiding intraoperative fractures.
The functional outcomes in our series have shown a significant improvement of MDP thickness, from 11.26 to 14.98, coinciding with other authors who have used the same technique, Fink et al.6 (75 HSS) and Carrera et al.20 (81 HSS), with hydroxyapatite stems and locking bolts.
The limitations of the study are that it is a retrospective study, with a limited number of patients and short-medium term follow-up, although with more cases than other studies referring to the same type of implant. We consider that the collapses and fixation failures occur within the first 12 months, as we have already shown in another publication,18 which is why we established the minimum follow-up at 12 months.
Distal fixation with modular conical stems, supplemented with distal locking screws, offers additional stability in cases with an isthmus of less than 4 cm, following the same philosophy as diaphyseal fixation, with correct canal filling and correct intraoperative anchorage (press-fit) to allow correct osseointegration; the proximal bone loss observed in this type of fixation is a concern.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Marqués López F, Sala Pujals A, Fraile Suari A, Tey Pons M, León García A. Vástagos modulares de anclaje diafisario con tornillos de bloqueo en la revisión de cadera con defectos femorales masivos. Rev Esp Cir Ortop Traumatol. 2020;64:409–414.