To describe the characteristics of patients diagnosed with ‘catastrophic hand’ by the plastic surgery department in a tertiary hospital in the period between 2000–2015, analyse the evolution of the use of the term ‘catastrophic hand’ and conduct a review of the literature with a view to proposing the optimal definition for said expression.
Material and methodWe conducted a descriptive and retrospective study of patients diagnosed with ‘catastrophic hand’ who required hospital care by the plastic surgery department of a tertiary hospital in the period between 2000–2015. We conducted a literature review on the use of the term ‘catastrophic hand’ and we applied the classifications proposed in the publications consulted to our results.
ResultsThe number of ‘catastrophic hand’ diagnoses was 133. We observed a downward trend in the use of the term over the years. Applying classifications based on the impossibility of recovery of an acceptable hand (presence of three long fingers and thumb) by reconstructive procedures, only 9 out of 133 patients could be considered to have ‘catastrophic hands’, constituting 6.7% of the total cases.
DiscussionThe term ‘catastrophic hand’ has different meanings, and this generates ambiguity. The use of a classification based on the possibility of obtaining an acceptable hand diminishes its use and improves the approach for such injuries.
ConclusionWe advocate limiting the use of ‘catastrophic hand’ to cases that meet criteria of ‘mutilated hand’ and ‘metacarpal hand’ to avoid indiscriminate use of the term and optimise therapeutic management.
Describir las características de los pacientes diagnosticados de «mano catastrófica» por el Servicio de Cirugía Plástica en un hospital de tercer nivel en el periodo comprendido entre 2000 y 2015; analizar la evolución del uso del término «mano catastrófica», y realizar una revisión bibliográfica con el objetivo de proponer la definición más óptima de dicha expresión.
Material y métodoRealizamos un estudio descriptivo y retrospectivo de los pacientes diagnosticados de «mano catastrófica» que requirieron atención hospitalaria por el Servicio de Cirugía Plástica de un hospital terciario en el periodo comprendido entre 2000 y 2015. Efectuamos una revisión bibliográfica acerca del uso del término «mano catastrófica» y aplicamos a nuestros resultados las clasificaciones propuestas en las publicaciones consultadas.
ResultadosEl número de diagnósticos de «mano catastrófica» fue de 133. Objetivamos una tendencia descendente en el empleo del mencionado término con el transcurso de los años. Aplicando clasificaciones basadas en la imposibilidad de recuperación de una mano aceptable (presencia de 3 dedos largos y pulgar) mediante procedimientos reconstructivos, tan solo 9 de 133 pacientes podían ser considerados «manos catastróficas», constituyendo un 6,7% del total de casos.
DiscusiónEl término «mano catastrófica» posee diferentes acepciones, generando ambigüedad. El uso de una clasificación basada en la posibilidad de obtener una mano aceptable disminuye su utilización y mejora el abordaje de dichas lesiones.
ConclusiónAbogamos por limitar el uso de «mano catastrófica» a los casos que cumplan criterios de «mano mutilada» y «mano metacarpiana» para evitar su uso indiscriminado y optimizar su manejo terapéutico.
Gripping is the basic function of the hand, i.e., the ability to make use of the thumb in opposition to the other long fingers.
Injuries to the hand are frequent, with an incidence of 15 per 1,000 individuals per year. They occur in one third of industrial accidents,1 in one in 5 traffic accidents, and they are the cause of one in every 3 cases of disability. Mutilations are a challenge for hand surgeons, whose aim will be re-implantation or the recovery of function so that the patient is able to recommence their work and/or everyday activities.
The term “catastrophic hand” has traditionally been used to define lesions that affect all or almost all of the tissues and functional systems of the hand (the skin, bones and joints, the arteries and veins, sensory and motor nerves and the muscles and ligaments) usually accompanied by the amputation of fingers. Nevertheless, we have no widely accepted definition or universal criteria for diagnosis.
In 2007 Scheker and Ahmed2 proposed a model that takes five structures into consideration: (1) skin coverage; (2) the vascular system (arteries and veins); (3) the sensory and motor nerve system; (4) the system of muscles and tendons, and (5) the system of joints and bones. They defined a catastrophic injury as one in which damage occurred to at least three of these structures, on condition that one of them is the skin coverage or system of bones and joints.
However, the first requisite for the correct treatment of the lesion is a classification system that makes it possible to set reconstruction objectives. According to Del Piñal3 the criteria for an “acceptable hand” in aesthetic and functional terms are the presence of 3 fingers and the thumb. The minimum finger length is at the level of the middle phalange, which means that the proximal interphalangeal joint (PIJ) must be preserved. The minimum length of the thumb is at the level of the distal phalange, preserving the interphalangeal joint (IJ). The presence of 2 fingers (keeping the integrity of the PIJ) and the thumb constitutes what is known as the “tripod pincer”, which is considered to be the minimum requirement for satisfactory functioning. The presence of one finger (with a complete PIJ) and thumb constitutes the “basic hand”, which makes a very weak pincer motion possible with a mechanism that offers minimum grip. We consider any form of finger amputation that fails to meet the criteria for an “acceptable hand” to be a “disabled hand”. Two different injuries must be differentiated within the latter category, both of which are grouped under the term “severe hand injuries” as it is impossible to achieve an “acceptable hand” by means of reconstructive procedures. These two injuries are the “mutilated hand” and the “metacarpal hand”. We consider a “mutilated hand” to have 2 or 1 fingers. The most widely accepted definition of a “metacarpal hand” is the one described by Wei et al.4 in 1997, which distinguishes between 2 subgroups: “type I metacarpal hand”, which corresponds to the amputation of all of the fingers proximal to the proximal phalange, with a normal thumb or one amputated distal to the IJ, and “type II metacarpal hand”, which corresponds to the amputation of all the fingers proximal to the proximal phalange, with a thumb that is amputated proximal to the IJ. This classification shows how functionally important the thumb is, given that its amputation is equivalent to a 40% loss of hand function and a 25% loss of the function of the whole locomotor apparatus.5
The aims of our study are to describe the clinical and epidemiological characteristics of the patients diagnosed “catastrophic hand” by the Plastic and Cosmetic Surgery Department of the Hospital Universitario Central de Asturias (HUCA) from 2000 to 2015, to analyse how the use of the said term by medical professionals has evolved and to undertake a review of the bibliography to propose a better definition of the term, according to scientific publications.
Material and methodsWe performed an observational and descriptive study of the patients diagnosed “catastrophic hand” who were admitted to the Plastic Surgery Department or who were treated in the Emergency Department of the HUCA in the period from 2000 to 2015. This hospital is the reference centre of the Principality of Asturias. We obtained the approval of the Research Ethics Committee of the Principality of Asturias.
We carried out a search in Pubmed using the following MeSH (Medical Subject Headings) terms: injuries, hand; hand injury; injury, hand; mutilated, hand.
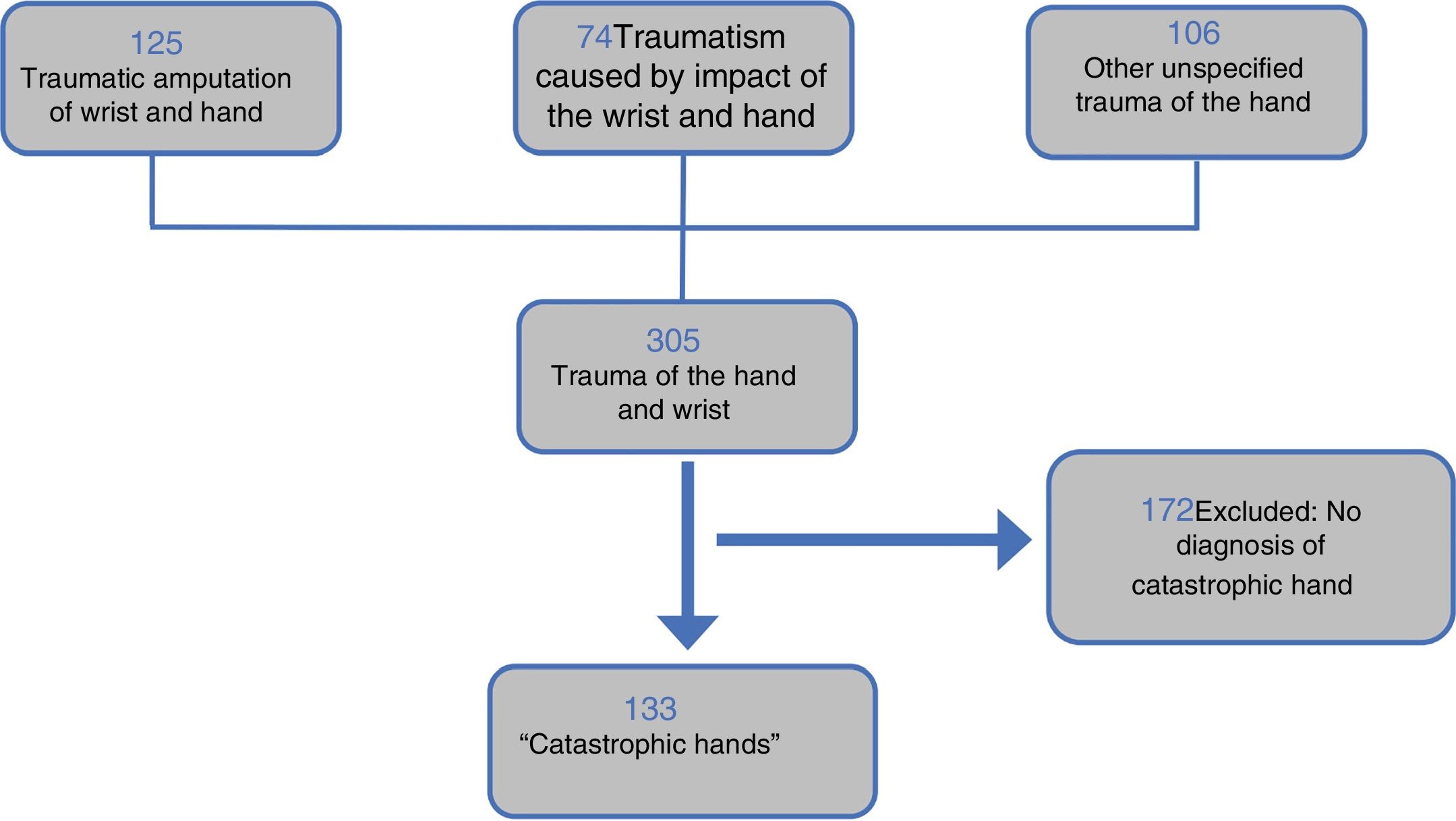
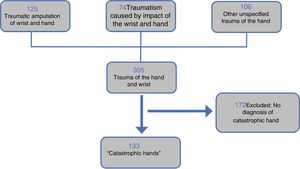
Together with the Clinical Documentation Service we undertook sampling of clinical history numbers, following ICD-10 search criteria: main diagnosis S68 (traumatic amputation of the wrist and hand), with the secondary diagnoses of S67 (traumatism due to impact of the wrist and hand) and S69 (other traumatisms and unspecified ones of the wrist and hand).
The inclusion criteria were patients diagnosed “catastrophic hand” who were admitted to the Plastic Surgery Department of the HUCA or who were treated in the Emergency Department by members of the Plastic Surgery Department (Fig. 1). The period of time studied was from 1 January 2000 to 31 December 2015.
The exclusion criteria were patients who, having been selected by the ICD-10 search criteria, were not diagnosed “catastrophic hand”.
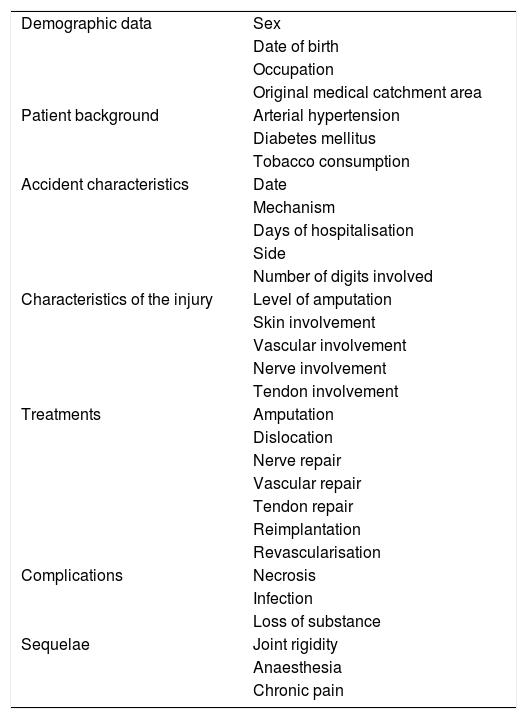
The variables described are shown in Table 1.
Variables included in the study.
| Demographic data | Sex |
| Date of birth | |
| Occupation | |
| Original medical catchment area | |
| Patient background | Arterial hypertension |
| Diabetes mellitus | |
| Tobacco consumption | |
| Accident characteristics | Date |
| Mechanism | |
| Days of hospitalisation | |
| Side | |
| Number of digits involved | |
| Characteristics of the injury | Level of amputation |
| Skin involvement | |
| Vascular involvement | |
| Nerve involvement | |
| Tendon involvement | |
| Treatments | Amputation |
| Dislocation | |
| Nerve repair | |
| Vascular repair | |
| Tendon repair | |
| Reimplantation | |
| Revascularisation | |
| Complications | Necrosis |
| Infection | |
| Loss of substance | |
| Sequelae | Joint rigidity |
| Anaesthesia | |
| Chronic pain |
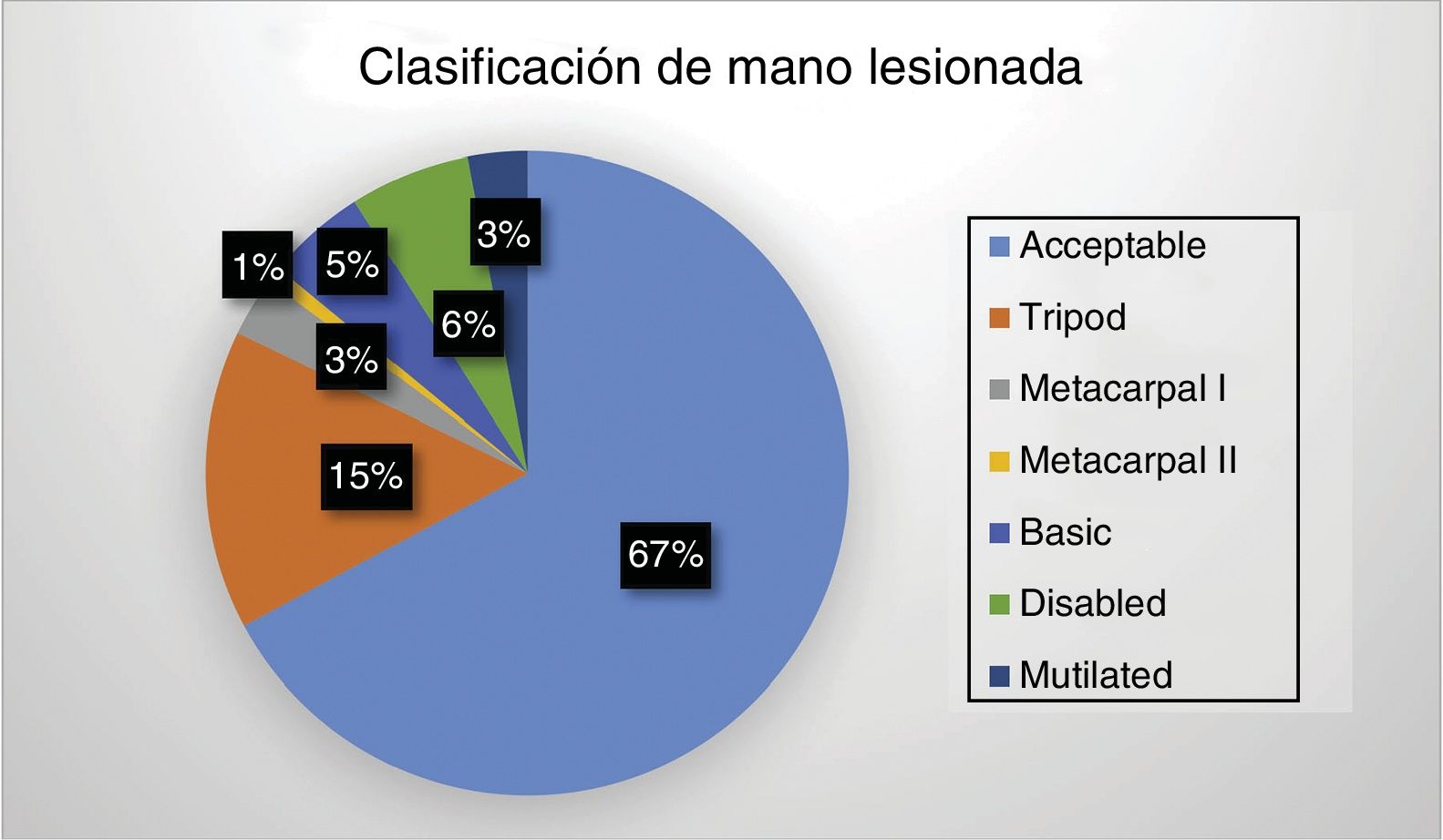
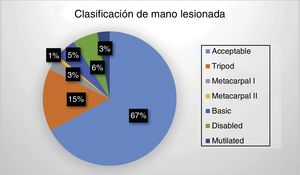
We used the classifications proposed by Del Piñal3 and Wei et al.4 to our results, thereby defining them as hands that were “acceptable”, “mutilated”, “metacarpal i”, “metacarpal ii”, “disabled”, “tripod” and “basic”.
Statistical analysisCategorical and discrete quantitative variables are expressed numerically and as percentages. Quantitative variables are expressed as an average ± standard deviation, or as a mean ± the interquartile range.
Discrete variables were compared using the χ2 test, and quantitative variables were compared using the Student t-test and the ANOVA test, using Bonferroni's test to correct the level of significance.
Descriptive and comparative analysis was carried out using the Stata 13 statistics program (version 13.0, StataCorp.; College Station, Texas, USA).
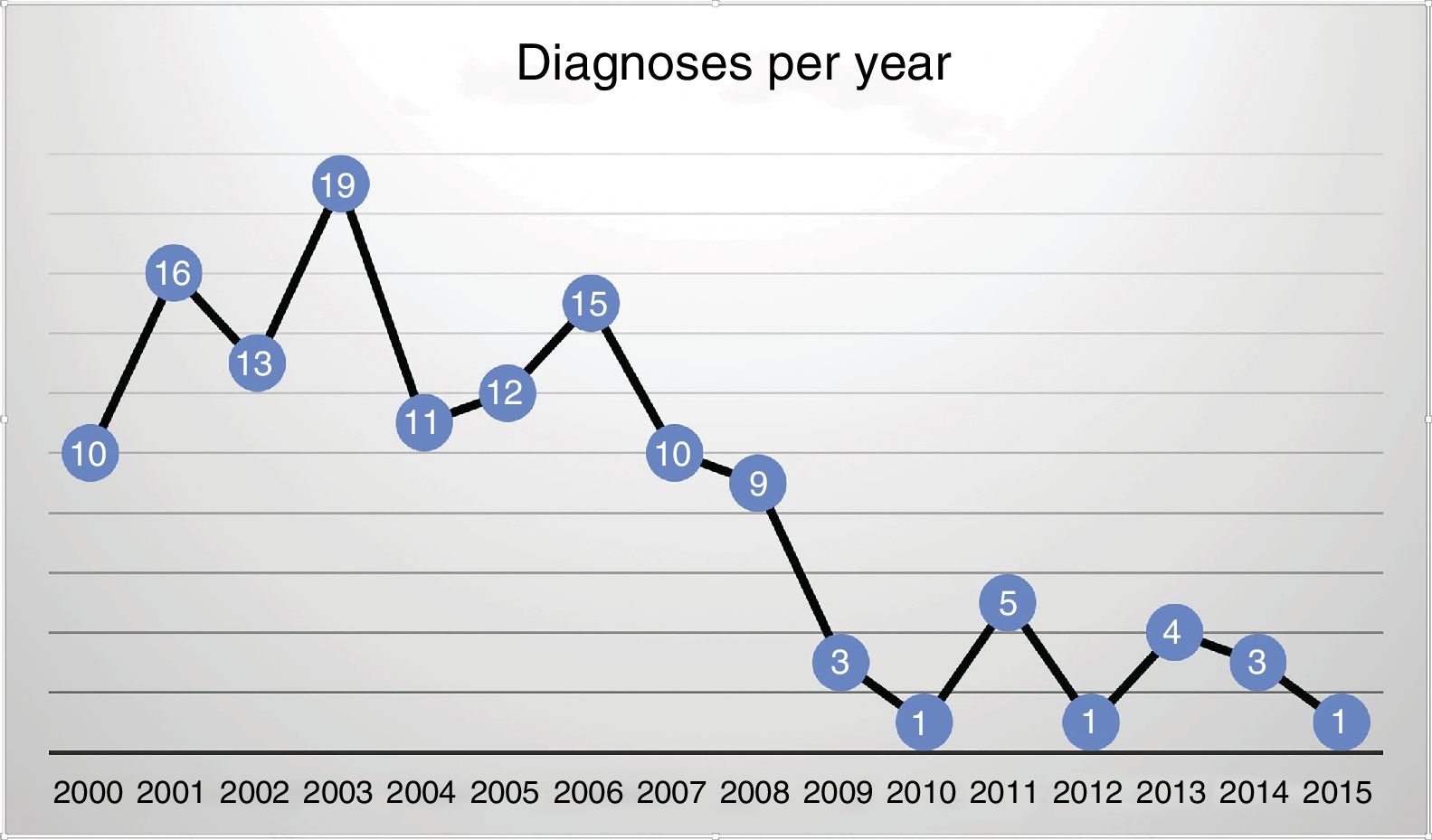
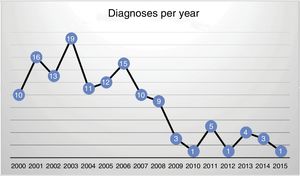
ResultsThere were 133 diagnoses of “catastrophic hand” in the Plastic Surgery Department of the HUCA in the period from 2000 to 2015. Of these cases, 124 (93.2%) were men vs. 9 (6.7%) in women. The patients were aged from 17 to 86 years old (with an average age of 46.6 years old). The highest number of diagnoses were recorded in 2003, with 19 cases (14%), followed by 2001 with 16 cases (12%) and 2006 with 15 patients (11%). On the contrary, from 2009 to 2015 a reduction in the number of cases was detected, at from 1 to 5 cases per year (Fig. 2). The month with the highest incidence of cases was April, with 17 cases (12.8%); and the day of the week with the most cases was Monday, with 29 cases (21.8%).
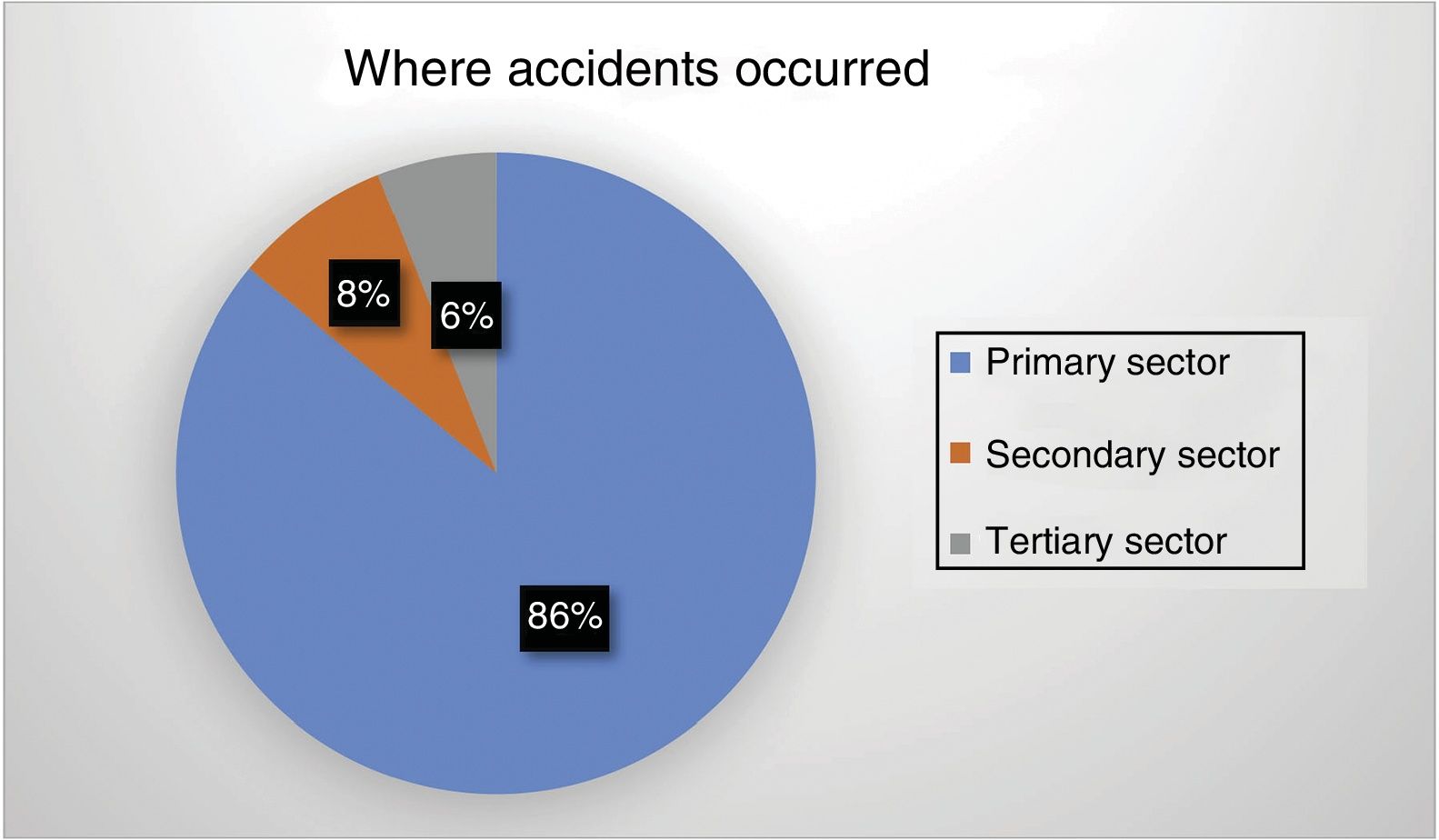
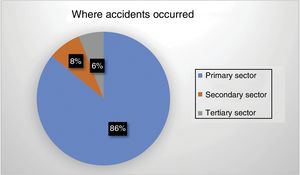
The average duration of hospitalisation was 6 days, with an interquartile range (p25–p75) of 3–9 days. There were 87 patient transfers (65.4%) from other healthcare areas to the HUCA. There were 72 industrial accidents (54.2%), of which 63 (87.5%) were in the secondary sector, 6 (8.3%) were in the primary sector and 4 (5.5%) were in the tertiary sector (Fig. 3). 58 patients (43.61%) were not injured at work. Of these, 15 (25.86%) were retired. No data on this question were found in the clinical histories of the other patients.
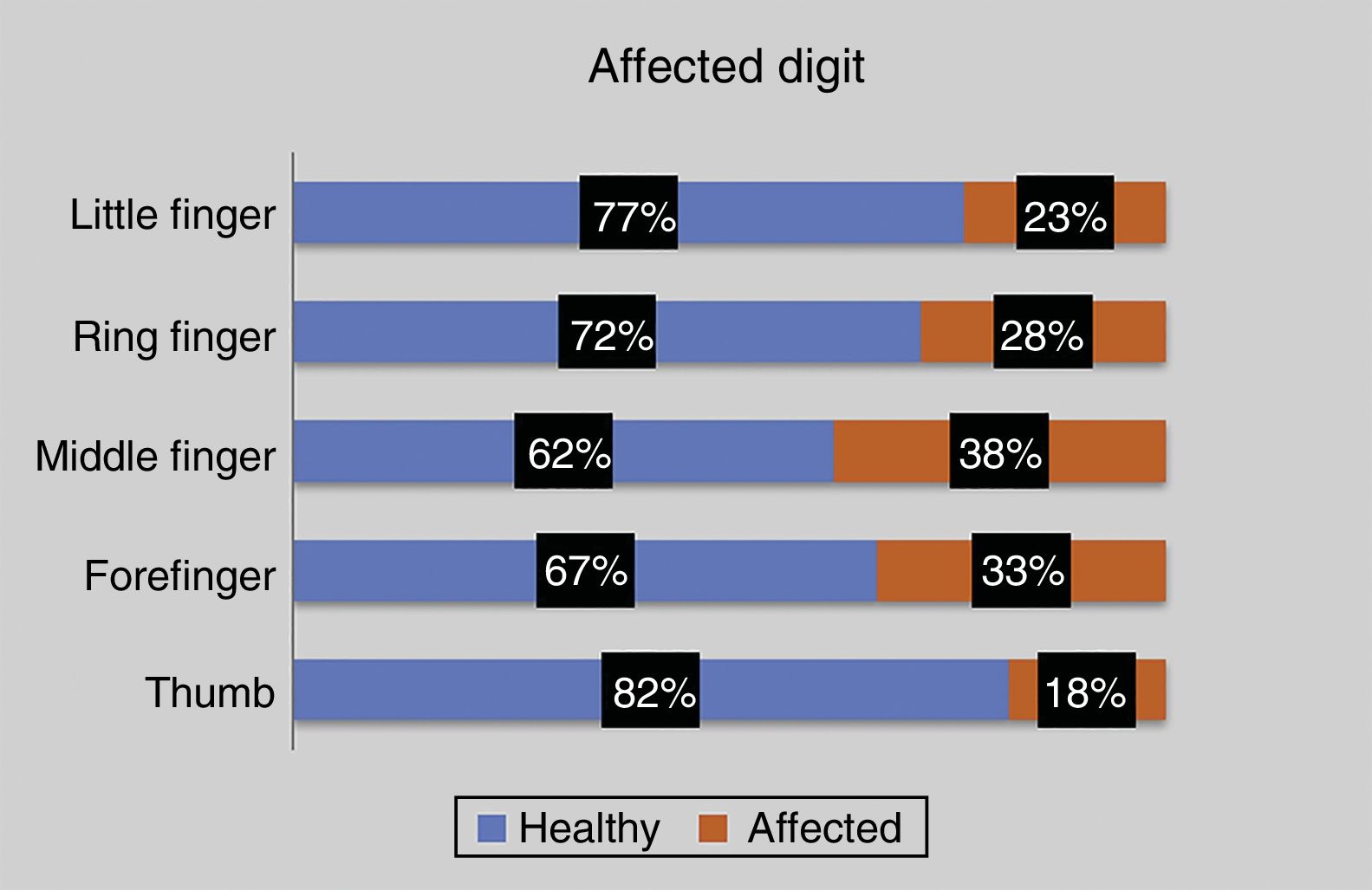
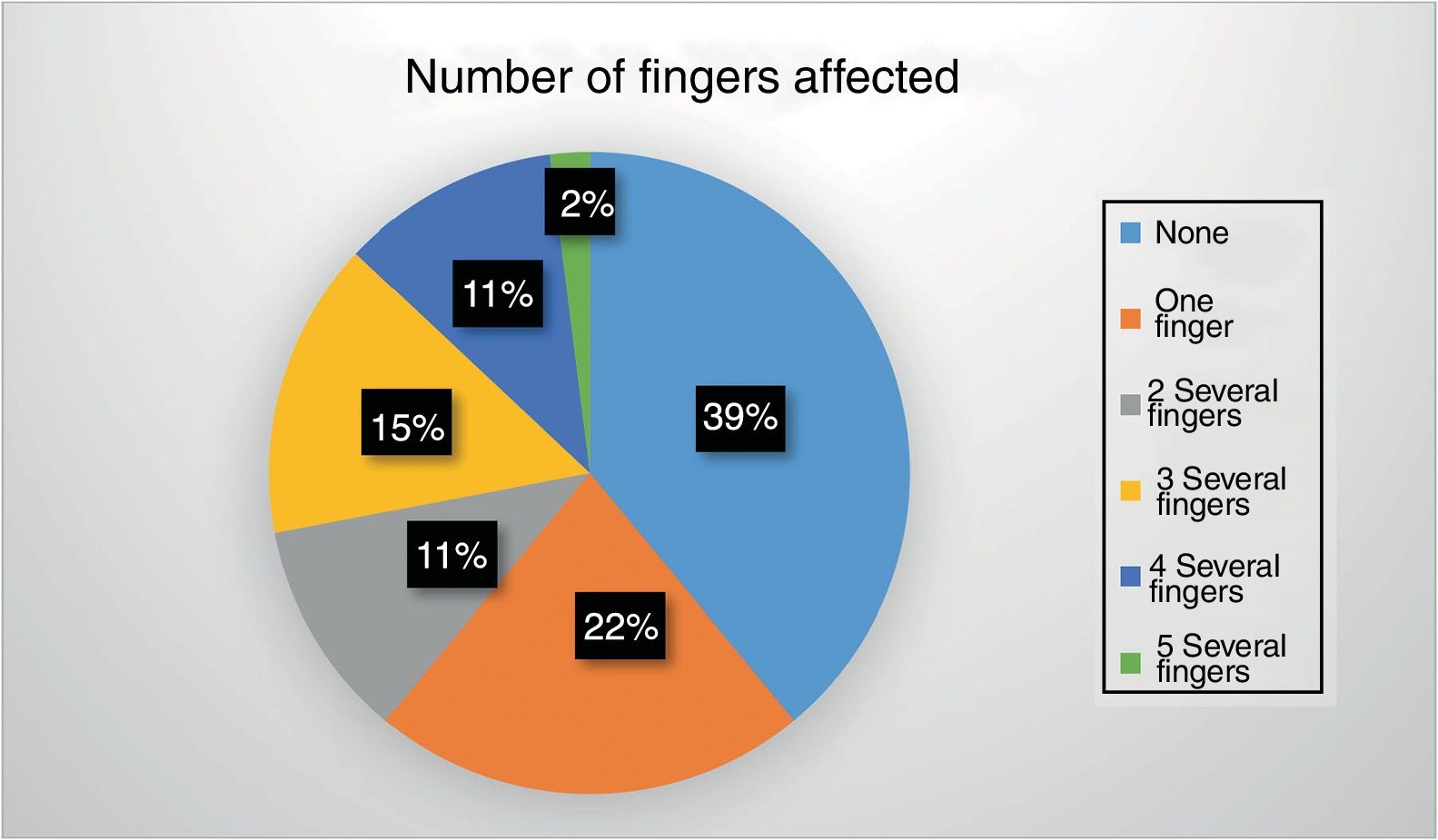
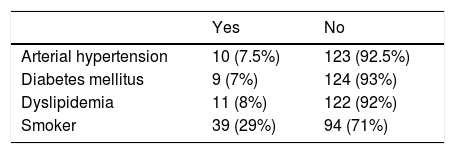
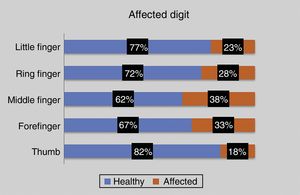
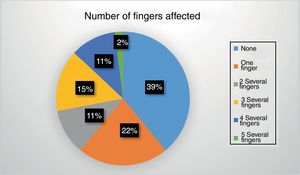
Table 2 shows the medical comorbidities of the patients together with whether or not they smoked. Regarding the causal mechanism, there were 80 cases of incision-impact (60.1%). The left hand was the most frequently involved, with 79 cases (59.4%), as opposed to 54 right hands (40.6%). The average number of injured fingers is 3.7, and the third or middle finger is affected the most often, while the thumb is affected the least often (Fig. 4). Fifty two patients (39.1%) had no amputated fingers, while 29 (21.8%) had one finger amputated and only 3 patients (2.3%) had all five fingers amputated (Fig. 5).
Combined treatment was applied the most frequently in all of the fingers, including osteosynthesis, vascular, nerve, tendon and skin suture.
Forty-six of the 133 patients (34.6%) had some type of complication. Necrosis was the most common complication, with the following results for each finger: 7 thumbs (38.9%); 13 forefingers (50%); 11 middle fingers (37.9%); 11 ring fingers (45.8%) and 5 little fingers (29.4%). This shows that the percentage of complications caused by necrosis is higher than those of all the other causes.
Thirty-six patients (27.1%) required surgery for the treatment of sequelae.
No statistically significant differences were found between the number of fingers that were injured and the duration of hospitalisation. Nor was any association found between the causal mechanism and the number of fingers that were injured.
According to the classifications proposed by Del Piñal3 and Wei et al.,4 we had 89 “acceptable hands” (67%), 20 “tripod hands” (15%), 7 “basic hands” (5.3%), 4 “mutilated hands” (3%), 4 “type I metacarpal hands” (3%), one “type II metacarpal hand” (0.8%) and 8 “disabled hands” (6%) (Fig. 6).
Distribution of injured hand involvement according to the classification subgroups of Del Piñal3 (%).
Complex mutilating hand injuries are a challenge for surgeons. Loss of the ability to grip gives rise to a severe functional limitation that has to be overcome by applying reconstructive objectives.
Our study shows that the most frequent patient profile diagnosed “catastrophic hand” in the HUCA corresponds to a man with an average age of 46 years old who had suffered an industrial accident. This also explains why the most frequent causal mechanism of the injury was incision-impact.
The percentage of accidents suffered by retired patients stands out at 26%, and this is probably due to the ageing of the population in Asturias.
On the other hand, we recorded more than 60% of patient transfers from other medical catchment areas in the Principality of Asturias to the HUCA. This is due to the fact that the said hospital is the reference centre for reconstructive surgery.
An article in Spanish that uses the term “mano catastrófica” was published by Herrera-Tenorio and Gómez-Cansino,6 of the Hospital General de Puebla (Mexico). They define catastrophic hand injuries as those which are multistructural and affect the bone tissue, tendons, neurovascular structures and skin to different degrees. They record a total of 25 patients over a 6 year period who were diagnosed “catastrophic hand” and who required reverse flow forearm skin flap grafts. They emphasise skin defects and coverage of the same instead of reconstruction following finger amputations, showing the range over which the term “catastrophic hand” is used. The majority of their patients were men, although they had an average age of 28.2 years old, which is considerably younger than we recorded in the HUCA. Likewise, the main causal mechanism of the injury was impact, followed by firearms, while we only recorded 20% of cases of impact, and in our case the most frequent mechanism was incision-impact, and with no case caused by firearms due to the difference between the rates of criminality in both countries.
In terms of how the patients were treated, the use of combinations of several surgical techniques stands out. These include osteosynthesis, vascular, nerve and tendon suture and skin coverage, all of which we include in the “combined treatment” variable, given that as these are complex lesions, by definition they affect all of the structures in the hand, and we found very few cases in which treatment consisted of a single technique.
The average duration of hospitalisation was relatively short, at less than one week (6 days). This may be due in part to the fact that only 46 of the 133 (34.6%) patients operated had a complication of some type. Necrosis was the most frequent complication, and this was probably due to the causal mechanism of the injury.
Joint rigidity was the most frequent sequela. This was also the case in the work by Herrera-Tenorio and Gómez-Cansino,6 and this was mainly due to the causal mechanism of the lesion (impact or firearm). It should be pointed out that 36 of the 46 patients with sequela required secondary surgery. This was probably because some of them required medical treatment and/or rehabilitation rather than surgery for chronic pain, rigidity or sensory neuropraxia.
We believe that the most appropriate definition of catastrophic hand is the one that refers to the impossibility of achieving an acceptable hand by means of reconstructive procedures, i.e., a “mutilated hand” or a “metacarpal hand”.
When the classifications proposed by Del Piñal3 and Wei et al.4 as described above are applied, only 9 of the 133 patients may be considered to be true cases of “catastrophic hand”, amounting to 6.7% of the total number of cases recorded. On the basis of these data we may conclude, as we suspected at the start of the study, that in the majority of categories (67% “acceptable hands”, 15% “tripods” and 4.5% “basic hand”) the said diagnosis was applied erroneously, given that the vast majority were hands that could be rendered acceptable by means of reconstructive procedure.
In recent years hand surgeons have become aware of the ambiguity that arises through use of the term “catastrophic hand” when defining a complex hand injury. There is now a clear tendency to cease using this term and to replace it with a more specific description of the lesion in question. We were able to detect this downward tendency in our series, as the majority of diagnoses took place from 2000 to 2005, with a notable fall after 2006.
In 2016 the reconstructive surgery team of Chang Gung Memorial Hospital under Dr. Wei7 introduced the new term “metacarpal-like hand”. This refers to the amputation of all of the fingers and the thumb proximal to their functional length, except for 1 or 2 fingers, including the thumb. These lesions may also be classified as “catastrophic” according to the classification proposed by Del Piñal.3 The treatment of choice are transplants of the toes to the hand. The toes make it possible to improve the functioning of the hand proportionally to the existing deficit. They make it possible for us to achieve a simple or tripod pincer movement in metacarpal and mutilated hands, while in less severe cases they make a practically ad integrum anatomical and functional restoration possible.8–10
This study has limitations due to its retrospective nature, most especially a possible distortion of the information during data gathering. On the other hand, although our sample size is not small in comparison with other published series, we believe that a larger number of cases would increase the statistical power of the study.
To summarise, we believe that the term “catastrophic hand” expresses confusion. Although classically it referred to severe hand trauma with major loss of tissue and functionality, we agree that the definition suggested by Dr. Del Piñal3 is the most appropriate, and we support limiting its usage to cases that meet the criteria for a “mutilated” or “metacarpal” hand.
Level of evidenceLevel of evidence III.
Ethical responsibilitiesProtection of people and animalsThe authors declare that for this research no experiments took place in human beings or animals.
Data confidentialityThe authors declare that no patient data appear in this paper.
Right to privacy and informed consentThe authors declare that no patient data appear in this paper.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: García-Martínez I, Fernández-Álvarez U, Fernández-Ardura T, Fernández-García A, de Juan-Marín M, Pérez-Arias A. Revisión del diagnóstico de mano catastrófica a lo largo de 15 años en un hospital terciario: ¿hacemos un uso adecuado del término? Rev Esp Cir Ortop Traumatol. 2019;63:35–40.