The aim of this study was to report the short-term results and complications of partial humeral head resurfacing (HemiCup®) in patients treated by avascular necrosis.
Material and methodsBetween 2010 and 2014, 9 patients who underwent partial resurfacing of humeral head were evaluated. All the patients were treated by avascular necrosis. The mean follow-up was 44 months (minimum 24 months). The average age was 47 years (range 32–57 years). The patients were evaluated clinically and radiologically. Complications were reported.
ResultsThe patients had a significant improvement in functional scores and mobility between the pre-operative and last follow-up control. The Constant score improved from 35 to 79 points (p<.001), ASES score improved from 31 to 76 points (p<.001), forward flexion and external rotation improved from 101° to 150° (p<.001), and from 24° to 45° (p<.001), respectively. One patient presented symptomatic glenoid wear during follow-up, requiring revision surgery.
ConclusionIn our patients treated by avascular necrosis, the partial resurfacing of humeral head (HemiCup®) demonstrated a significant improvement in functional scores and mobility with an average follow-up of 44 months.
El objetivo de este trabajo es reportar los resultados a corto plazo y las complicaciones de la artroplastia de superficie del húmero proximal (HemiCup®) en pacientes tratados por necrosis ósea avascular.
Material y métodosEntre 2010 y 2014 fueron evaluados 9 pacientes a los que se les realizó una artroplastia de superficie del húmero proximal. Todos los pacientes fueron tratados por necrosis ósea avascular. El seguimiento promedio fue de 44 meses (mínimo 24 meses). La edad promedio fue de 47 años (rango 32-57 años). Los pacientes fueron evaluados cínica y radiológicamente. Se reportaron las complicaciones.
ResultadosLos pacientes presentaron una mejoría significativa en los scores funcionales y la movilidad entre el preoperatorio y el último control en el seguimiento. El score de Constant mejoró de 35 a 79 puntos (p<0,001), el score de ASES mejoró de 31 a 76 puntos (p<0,001), la flexión anterior y la rotación externa mejoraron de 101 a 150° (p<0,001) y de 24 a 45° (p<0,001), respectivamente. Un paciente presentó desgaste sintomático en la glena durante el seguimiento, requiriendo una cirugía de revisión.
ConclusiónEn nuestra serie, la artroplastia parcial de superficie del húmero proximal (HemiCup®) demostró una mejoría significativa en los scores funcionales y la movilidad en pacientes tratados por necrosis ósea avascular, con un seguimiento promedio de 44 meses.
Avascular bone necrosis (ABN) of the humeral head is a rare condition. It can develop spontaneously, with no apparent aetiology (primary) or, in most cases, in association with a specific condition or risk factor (secondary), the most common being corticosteroid use and post-traumatic necrosis.1–4
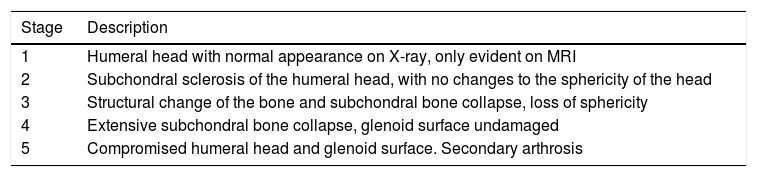
The classic symptoms include pain, stiffness, loss of mobility and reduced function. The different stages of ABN of the humeral head are classified by Cruess2 (Table 1) through a modification of Ficat's classification for ABN of the proximal femur.5
Cruess stages. Avascular bone necrosis of the humeral head.
| Stage | Description |
|---|---|
| 1 | Humeral head with normal appearance on X-ray, only evident on MRI |
| 2 | Subchondral sclerosis of the humeral head, with no changes to the sphericity of the head |
| 3 | Structural change of the bone and subchondral bone collapse, loss of sphericity |
| 4 | Extensive subchondral bone collapse, glenoid surface undamaged |
| 5 | Compromised humeral head and glenoid surface. Secondary arthrosis |
MRI: magnetic resonance imaging.
Treatment for ABN of the humeral head varies according to the development stage of the disease. Patients in the initial stages, where there is no subchondral collapse (Cruess 1 and 2), are candidates for both non-surgical treatment and core decompression surgery of the necrosis by drilling, depending on its clinical progression.6,7
In advanced stages (Cruess 3–5), a prosthetic replacement of some type is required. Patients with advanced humeral compromise, with no glenoid compromise (Cruess 3–4), are candidates for a hemiarthroplasty. When there is glenoid surface involvement (Cruess 5), a total shoulder arthroplasty is indicated.
The traditional prosthetic models, with intramedullary stem, have been widely used for this group of patients with good results.8–10 Although they currently enable more versatility in coupling between the humeral head and the stem, a theoretical limitation with these types of implants is their limited capacity to precisely reproduce the anatomy of the humeral head,11,12 considering that this is an anatomical site with great variability of inclination, retroversion and centre of rotation, not only between different patients but also between the shoulders of the same patient.13
The use of surface replacements, total or partial, has gained in popularity since they enable bone capital to be saved, with the advantage of adequately restoring the normal anatomy of the humeral head.4,14–17
The aim of this paper is to report the functional results and complications of a series of patients treated for ABN by partial resurfacing of the humeral head using the HemiCup® system, with a minimum follow-up of 2 years.
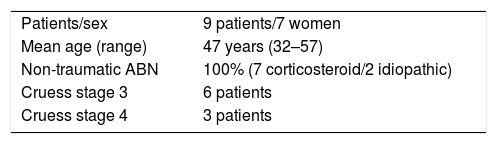
Materials and methodsBetween June 2010 and June 2014, 10 patients were treated for ABN of the humeral head by partial humeral head resurfacing using the HemiCup® surface, Arthrosurface®. Two patients had bilateral compromise, although at the time of study they had only undergone treatment to one shoulder. One patient was lost to follow-up, and 9 patients were included in the series (9 prostheses). The average age was 47 (range 32–57). Five procedures were performed on 5 women and 4 men. Seven prostheses were placed in the right shoulder, and 2 in the left. The dominant limb was involved in 7 cases. The minimum follow-up was 24 months. The patients were classified by conventional radiography and magnetic resonance using the Cruess classification for ABN of the humeral head.2 Seven patients were classified as Cruess grade 3, and 2 as Cruess grade 4. All the patients had less than 40% loss of bone capital of the humeral head measured by MRI.18 The ABN aetiology was secondary to corticosteroids in 7 cases and idiopathic in 2 patients (Table 2).
The indication for surgery in all cases was pain and functional limitation of the affected shoulder, which had failed to respond to non-surgical treatment (physiotherapy, medication, modification of activity) and was negatively affecting the patients’ activities of daily living.
All the procedures were performed under combined anaesthesia (interscalene block and general anaesthesia) by the same experienced surgeon (MR).
Surgical techniqueThe deckchair position was use in all cases. Using a deltopectoral approach, the rotator interval was identified, approaching the joint by disinsertion of the subscapularis tendon. Before capsulotomy, controlled dislocation of the humeral head was performed. Once the injury had been identified, it was measured on the antero-posterior and lateral plane, as well as in depth, using specific guidelines. The central screw was placed according to the surgical technique. Once the size of the implant had been established, the humeral head was reamed. Finally, the definitive component was placed impacting it to the central screw using a Morse cone system.
The subscapsularis was anatomically reinserted using transbone stitches. All the patients underwent tenodesis of the long portion of the biceps. One patient underwent simultaneous repair of the supraspinatus.
A 40mm prosthesis was used in all cases.
The patients were immobilised using a sling for 4 weeks, allowing flexo-extension movements of the elbow and wrist, limiting forward flexion and abduction of the shoulder. After the first month all the patients started a rehabilitation regimen that lasted 6–8 weeks. They gradually resumed their activities as tolerated.
All the patients were assessed pre- and postoperatively by an examiner who was not the treating surgeon. Functional scores (Constant and ASES),19,20 the visual analogue pain scale and mobility between the preoperative situation and the final follow-up session were analysed. X-rays were taken on the antero-posterior plane, scapular Y and axillary views. Signs of glenoid loosening or erosion were evaluated, using the criteria described by Rispoli et al.21: absent (no signs of glenoid wear), mild (partial or total piercing of the subchondral plate), moderate (wear approaching the lateral coracoid process), severe (medial wear to the lateral coracoid process).
The Constant, ASES and mobility score variables (measured in grades) were considered continuous and are presented with measures of central tendency and dispersion. The variables of our sample adjusted to a normal distribution, therefore, the results are described as means and standard deviation.
The Student's t-test was used for comparison between the pre and post-operative results, with a level of significance set as p<.05. STATA software version 13.0 was used for the statistical analysis.
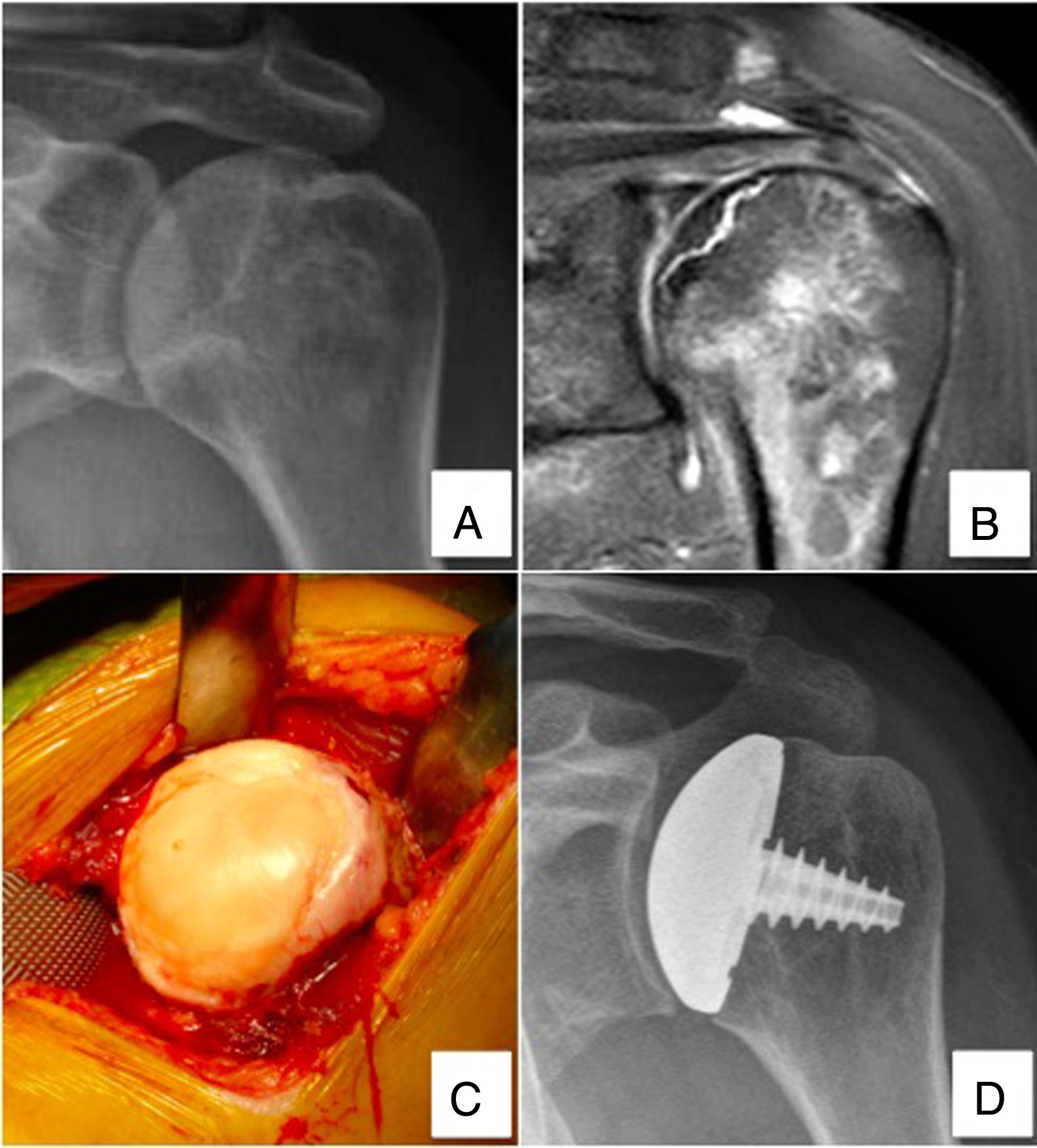
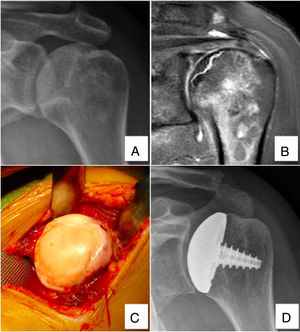
ResultsNine humeral head resurfacing prostheses were analysed in patients treated for ABN (Fig. 1).
51-Year-old patient diagnosed with humeral head ABN treated with partial resurfacing arthroplasty (HemiCup®). (A and B) Radiography and magnetic resonance imaging of the left shoulder showing signs of subchondral collapse, and integrity of the glenoid surface (Cruess 3). (C) Intraoperative image showing loss of humeral head sphericity. (D) Control radiography at 52 months postoperatively, showing good outcome.
The mean follow-up was 44 months (range 24–62 months).
According to the classification of Rispoli et al.,21 none of the patients had signs of glenoid wear at time of surgery.
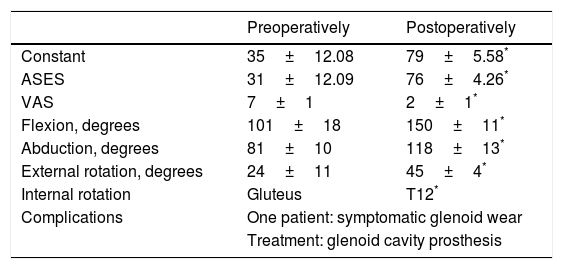
The patients showed significant improvement in their functional scores between the preoperative situation and the final follow-up (Table 3). The Constant score improved from 35±12.08 preoperatively to 79±5.58 (range 70–88) postoperatively (p<.001). The ASES score improved from 31±12.09 (range 16–43) preoperatively to 76±4.26 (range 70–100) postoperatively (p<.001). The values on the visual analogue pain scale improved from 7.3±.8 (range 6–9) preoperatively to 2.2±1 (range 0–3) postoperatively (p<.001).
Functional results and complications.
| Preoperatively | Postoperatively | |
|---|---|---|
| Constant | 35±12.08 | 79±5.58* |
| ASES | 31±12.09 | 76±4.26* |
| VAS | 7±1 | 2±1* |
| Flexion, degrees | 101±18 | 150±11* |
| Abduction, degrees | 81±10 | 118±13* |
| External rotation, degrees | 24±11 | 45±4* |
| Internal rotation | Gluteus | T12* |
| Complications | One patient: symptomatic glenoid wear | |
| Treatment: glenoid cavity prosthesis | ||
VAS: visual analogue pain scale.
Mean follow-up of 44 months (range 24–62).
Mobility had improved significantly on the physical examination. Forward flexion increased from an average of 101±18° to 150±11°. Abduction increased from an average of 81±10° to 118±13°. External rotation improved from an average of 24±11° to 45±4°. Internal rotation improved from a preoperative average “gluteal” level mobility to a postoperative average “T12” level (p<.001).
On the radiological assessment, one patient presented mild signs of glenoid wear,21 associated with return of pain and functional limitation at 38 months after the resurfacing arthroplasty, having made more than 2 years of good progress in terms of pain and function. The reappearance of these symptoms was interpreted as secondary to the glenoid wear and revision surgery was performed, with placement of the glenoid prosthetic component. The patient made good progress after the second procedure.
DiscussionThe results of the short-term follow-up of this series of patients in advanced stages of ABN (Cruess 3 and 4), with no glenoid compromise, treated with partial humeral head resurfacing using the HemiCup® system, show a significant improvement in functional scores and mobility with a mean follow-up of 44 months.
Although ABN of the humeral head is a rare disorder, it is associated with pain, stiffness, loss of mobility, and reduced function of the affected shoulder.
In the initial stages (Cruess 1 and 2), the literature states that these patients are candidates for non-surgical treatment (observation, anti-inflammatories, kinesiology, injections) or for a decompressive procedure with drilling, depending on clinical progression.6,7
As subchondral bone collapse and joint compromise develop, prosthetic replacement becomes the appropriate treatment option.
Most of the papers published in the literature on the surgical treatment of ABN of the humeral head22 agree in that the patients they include are in the fifth decade of life, and preservation of bone capital, wear of the glenoid joint surface and the likelihood of revision surgery in the future are essential aspects to consider when choosing the implant.
Conventional intramedullary prostheses have been used traditionally with good results for patients with advanced stages of ABN of the humeral head.8,10
Although these series show significant improvements in functional scores and mobility, there are considerable associated complications, in some cases up to 30%,8 which include rotator cuff injuries, instability, glenoid wear in hemiarthroplasties, and loosening of the glenoid component in total prostheses.
On analysing the results of hemiarthroplasty using a stemmed prosthesis for ABN, Smith et al. reported a series of 32 patients with an average follow-up of 12 years, all treated for corticosteroid-related ABN of the humeral head. The authors describe that although this procedure is associated with significantly improved functional scores and mobility, 42% of the patients stated that they were not satisfied, 38% with moderate to severe pain, due to symptomatic glenoid wear.3
This limitation associated with symptomatic glenoid wear has been described by other authors when analysing the results of hemiarthroplasty using a stemmed prosthesis for ABN of the humeral head.9,23
Surface arthroplasties have gained in popularity as an alternative for preserving bone capital, achieving results that are similar to those of models with cemented intramedullary stems.24,25
Levy et al.,26 in a series of 49 patients treated with surface arthroplasties with a minimum follow-up of 10 years, described an 82% satisfaction rate among their patients, 19 of these prostheses being indicated due to ABN, and this group achieved the best functional results.
Partial resurfacing of the humeral head is another prosthetic alternative for this group of patients. It is designed to treat focal injuries of the humeral head, partially resurfacing the joint surface.
Biomechanical studies describe how partial resurfacing restores the centre of rotation of the humeral head more precisely compared to hemiarthroplasty, with less eccentric overload on the glenoid, reducing wear to it.14
Partial resurfacing removes the restriction caused by static coupling between the prosthetic humeral head and the intramedullary stem, and in turn allows positioning and measurement of the prosthetic component taking the remaining articular cartilage as the benchmark.
There are few published reports on the results of this type of prosthetic model in ABN of the humeral head.
Franceschi et al.22 recently performed a systematic literature review on patients with ABN of the humeral head, treated surgically. They included twelve papers in their analysis, 3 of which studied patients treated with decompression surgery, 8 examined the results of patients treated with hemiarthroplasty or total shoulder prosthesis, and only one4 examined patients treated with surface prostheses. The authors conclude that the follow-up in the available papers is scanty, and they highlight this as a significant limitation.
In 2009, Uribe and Botto-van Bemden4 reported the results of 11 patients diagnosed with ABN of the humeral head treated with partial resurfacing (HemiCup®). With a mean follow-up of 30 months, the patients achieved good and excellent results in their functional scores, with 142° of forward flexion and 46° of external rotation, similar results to those of our series. Unlike our study, their patients had no complications.
Sweet et al.27 studied 19 patients treated with the HemiCup® system (4 for ABN and 15 for primary arthrosis), and concluded that partial arthroplasty of the humeral head is an effective procedure for treating pain and function, with a high rate of patient satisfaction, reporting 15% of complications in the 32 months of mean follow-up, all of which occurred in patients treated for primary arthrosis.
Mansat et al.,28 in a clinical and radiological analysis of 61 patients treated with surface prostheses for different diagnoses, with a mean follow-up of 36 months, concluded that although this type of prosthesis reproduces the normal anatomy of the humeral head, their patients had a tendency to glenoid wear, with recurrence of pain in 17% of the cases, and 8% requiring revision surgery to a total shoulder prosthesis. We should stress that this tendency to glenoid wear was probably due to the indication for surgery, since all the patients with complications were operated for primary arthrosis, associated with a tendency to valgus placement of the humeral prosthetic component demonstrated by the authors. None of the patients operated due to ABN presented with complications.
Although an essential point for study would be to compare the stemmed prosthetic models and the resurfacing models in terms of glenoid wear, currently there is insufficient evidence in the literature on series that analyse the results in patients treated for ABN using the current stemmed prosthetic models, which enable greater versatility in placing the head component, and moreover, the series that analyse surface prostheses are limited in terms of follow-up and number of patients. Another essential point on considering the high percentage of complications published in the series of Smith et al.,3 in relation to glenoid wear, is that this paper reports the long-term results of hemiarthroplasty for ABN (12 years on average). Because there is little evidence on the long-term results of other prosthetic models, it is too early to reach conclusions on this point.
A limitation of our study is that it analyses a small number of patients, with a follow-up period limited to the present. However, as ABN is a rare disorder, this series summarises the few similar reports previously published in the literature, and therefore we believe that it contributes towards interpreting the results of this type of prosthesis in this group of patients. Although there is the need in theory to undertake prospective and randomised studies, there are few because of the rareness of this condition and their methodological difficulties.
In our series, partial resurfacing of the humeral head (HemiCup®) showed a significant improvement in the functional scores and mobility of patients treated for ABN, with a mean follow-up of 44 months.
Level of evidenceLevel of evidence iv.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Ranalletta M, Bertona A, Tanoira I, Rossi LA, Bongiovanni S, Maignón GD. Resultados de la artroplastia parcial de superficie para el tratamiento de pacientes con necrosis ósea avascular del húmero proximal. Rev Esp Cir Ortop Traumatol. 2019;63:29–34.