The COVID pandemic has made telematic consultations a basic tool in daily practice.
AimsThe main objective of the study is to assess the results of the application of telematic consultations to limit the mobility of patients.
The operational objectives are; to propose a consultation plan, to know how attendance limits consultations and to define which pathologies benefit the most from this plan.
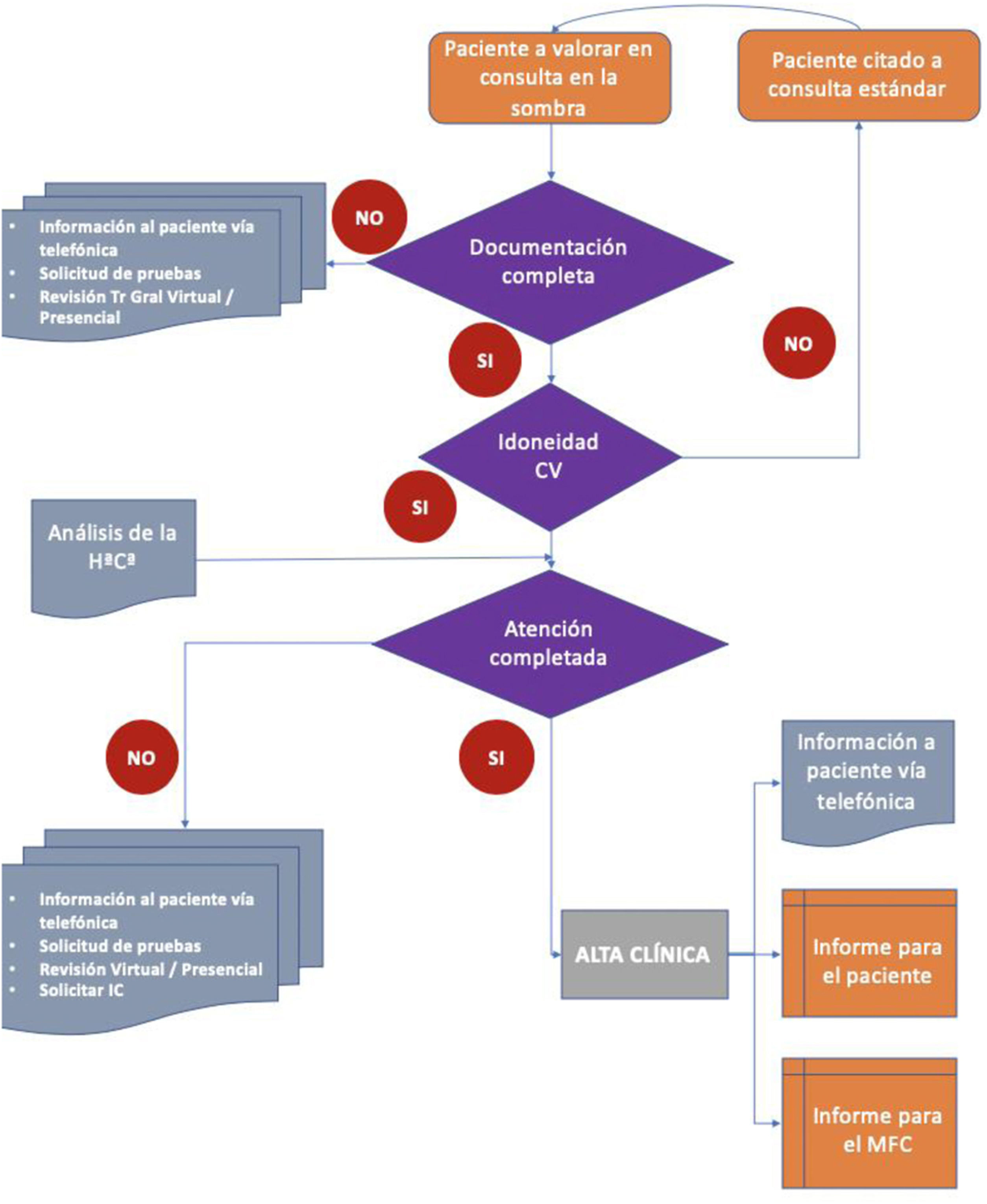
MethodsA scheme is proposed with the creation of pre-scheduled clinic to assess suitability and the possibility of carrying them out in a single non face-to-face act.
ResultsPhone call to 5619 patients were made with a lack of response of 19%
The cases of 74% of the patients that answered were resolved virtually. There is a difference between units, obtaining a higher answering rate from patients appointed to specific clinic units, OR = 0.60, or to general trauma ones, OR = 0.67. The lowest answering rate was obtained from those derived from the emergency department.
Twenty per cent of the consultations were not accompanied by complementary tests that would have favored the resolution in a single act. The general trauma consultations, OR = 0.34, postoperative control, OR = 0.49, and specific unit ones, OR = 0.40, were the ones that better met this requirement.
Out of the remaining patients, the general trauma consultations, OR = 0.50, and those referred to units, OR = 0.54, were the ones that had a higher resolution rate without in- person consultation.
ConclusionsThe cases of 74% of the patients who answered the phone call were resolved virtually.
Cases of 20% of the patients cannot be solved in a single act because they are derived without complementary tests.
Osteosynthesis and postoperative arthroscopic follow-up consultations are the ones that need to be carried out in person the most.
La pandemia COVID ha hecho de las consultas telemáticas una herramienta básica en la práctica diaria.
El objetivo principal del estudio es valorar los resultados de la aplicación de consultas telemáticas para limitar la movilidad de los pacientes.
Son objetivos operativos; proponer un plan de consultas, conocer como limita la asistencia a las consultas, definir qué patologías se benefician mas con este plan.
Material y MétodosSe propone un esquema con la creación de consultas previas a las agendadas para valorar idoneidad y posibilidad de realizarla en acto único no presencial.
ResultadosSe han realizado 5619 consultas con una falta de respuesta telefónica del 19%.
El 74% de los pacientes fueron resueltos de forma virtual. Existe diferencia entre unidades, siendo mas probable la respuesta telefónica para las consulta de unidad, OR = 0.60 o de traumatología general, OR = 0.67 y menos para los derivados desde urgencias.
El 20% de las consultas no se acompañaban de pruebas complementarias. Las consultas de traumatología general, OR = 0.34, control postoperatorio, OR = 0.49, y unidades, OR = 0.40, cumplieron mejor este requisito.
De los pacientes restantes, las consultas de traumatología general, OR = 0.50, y las derivadas a unidades, OR = 0.54, fueron las que se mas se resolvieron sin acudir presencialmente.
ConclusionesSe han resuelto de forma no presencial el 74% de los pacientes que atendieron a la llamada telefónica. El 20% de los pacientes acuden a la visita sin pruebas complementarias. Las consultas de seguimiento de osteosíntesis y postoperatorio de cirugía artroscópica son las que mas precisan de ser realizadas de forma presencial.
Telemedicine is a consolidated tool within trauma and orthopaedic patient care options due to its clinical and economic advantages.1 Due to this, certain conditions have to be fulfilled if it is to be implemented, and these affect the type of pathology in question and patient referral conditions.2
Telemedicine has mainly been used in cases of traumatic injury for those involving what are known as fractures with less variability, without metacarpal displacement and with no risk of displacement of the distal extremity of the radius and the head of the radius. Although the result of these virtual consultations has recognised clinical value, as well as in terms of patient accessibility and economic advantages, it is not always accepted to the same degree. It is better accepted by patients with professional responsibilities, while for students or individuals with certain limitations on their independence it leads to an increased need for check-ups.3
In the same way, use of this technique has consolidated in the follow-up of patients who have been operated using arthroplasty techniques and who are familiarised with filling out functional questionnaires. For these patients, together with the availability of the necessary radiological studies, it is able to replace traditional consultation without the need for travel, although under specific conditions that affect the indications for follow-up as well as patient profile.4,5
This form of medical care was found to play a positive role when it was used in emergency situations, such as those caused by the SARS-CoV-1, Zika and Ebola viruses.6,7 Although it is not the solution in all scenarios, it is an excellent patient care tool when both patient and staff have to restrict their exposure. The chief limitation in the use of telemedicine is the availability of personnel, as well as the need for a communication system that brings together suitable conditions for sufficient intereaction.8
The implementation of virtual consultations involves design work with the involvement of all of the staff levels who are to take part. Complementary studies are also required, together with patients who are able to understand a new paradigm. However, in exceptional circumstances it is possible to adapt the model in a way that offers additional advantages. The current COVID-19 pandemic and state of alarm declared in Spain on 14 March 2020 gave rise to a series of recommendations that demand we adapt our everyday activities, although we often have not had enough time to promote the resulting changes. The condition that was imposed consisted of the need for individuals, patients, family members and professionals to keep their distance from each other, to prevent the possibility of transmission in a situation with the additional uncertainty of the unknown pattern and evolution of the aetiology. The result has supported this capacity for adaptation.9
The first indication from a medical viewpoint is intuitively that the situation has to be brought under better control by suspending all visits that are neither urgent or affect oncological processes. Although many visits in our speciality may be delayed, postponing others may cause irreparable harm to the life or functioning of the patients. Other patients can also be seen in our surgeries, when they have non-urgent pathologies and have sometimes had to endure a long waiting list before being seen. In these cases, the suspension of visits would damage their health, as well as negative economic and professional effects in the case of processes that could restrict their professional development. Although suspending visits by these patients may not cause functional harm, it would reduce their quality of life and professional progress, and we are obliged to limit this as much as possible.
The main aim of this work is to evaluate the results obtained by applying a consultation plan that permits patient care under circumstances I which freedom of movement is restricted, reducing contact and adding to the safety of patients, family members and professionals during the “state of alarm” declared due to the COVID-19 pandemic.
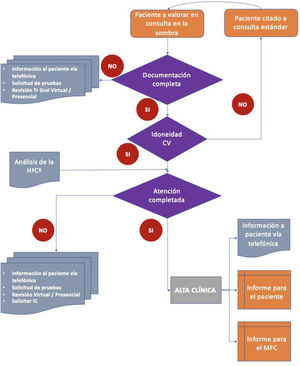
The operational objectives are to propose a parallel plan for consultations that makes it possible to do the following before a face-to-face visit: to analyse patient histories and their degree of adhesion, to discover how far the proposed scheme would reduce patient attendance at consultations, to define which pathologies in our speciality are the most suitable for this treatment plan, and finally to analyse points in our clinical practice which should be improved to maximise remote patient care (Fig. 1).
Material and methodsThe Orthopaedic and Trauma Department (OTD) of hospital XXXX has a catchment area containing a population of 474,000 inhabitants, which varies due to the high proportion of people who take vacations there. The Department offers a total of 2442 consultations per year to see 74,000 patients. These patients can be divided into those who have been referred for evaluation by other specialised hospital care units, as well as those referred by other secondary health centres. The final group is composed of those patients who have been treated in the Emergency Department and those who have received surgery.
Consultations are classified as follows:
- •
Plaster surgery. This includes patients who require monitoring of their trauma pathology after surgery or conservative treatment in the Emergency Department. They are given appointments to monitor setting or the evolution of wounds and the state of soft tissues.
- •
Postoperative surgery. This sees patients who have been operated in planned surgery, with the aim of monitoring the evolution of the wound as well as the achievement of the aim of surgery.
- •
General Traumatology. This surgery evaluates patients who have been referred by their family and community doctor (FCD) due to musculoskeletal symptoms, after the FCD has exhausted the diagnostic and therapeutic options. These consultations are structural, and circumstantially involve other new visits to resolve the demands which arise in time. They consist of accessibility consultations.
- •
Consultations within the unit. In these patients referred by other units in the OTD Department are given appointments after being referred by general traumatology or other hospital departments. After being classified the intervention of a specific unit is requested once diagnostic or therapeutic possibilities have been exhausted. These surgeries are divided so that each treats a single pathology, of the hip, knee, spinal column, foot, tumours, arthroscopy, osteosynthesis, chondral pathology and the upper limbs.
These patients are usually asked to attend the surgery with complementary test results that have been requested by the doctor who asked for the check-up.
It is proposed that a parallel visit be created that would take place the day before the face-to-face visit. It would analyse which medical unit should see the patient, and whether it would be appropriate to request complementary tests, so that only a single visit would be needed. For those patients who could be attended in a single virtual clinical visit, the second step would consist of completing the medical function by completing the protocol of information, recommendation and the issue of reports.
These consultations were designed according to Gnl Tr.: general traumatology. VC: virtual consultation. HªCª: clinical history. IC: interconsultation. FCM: family and community medicine.
Concept 1, including the following characteristics:
- 1
The face-to-face consultation is maintained.
- 2
Creation of a parallel consultation 24−48 hours before the planned date for the face-to-face consultation, with the same agenda as the one the face-to-face consultation will have.
- 3
Analysis of the available documentation, evaluating its exhaustiveness, clinical data, examination and complementary tests. The result may be that the history is considered:
- •
Incomplete. In this case the lacking elements are added and a new appointment is made. The patient is informed that the appointment has been suspended until all of the complementary tests that are required are available.
- •
Complete. These cases are considered suitable to attention in a virtual consultation.
- 4
Evaluate the suitability of being seen in a virtual consultation:
- •
Not suitable. In spite of the availability of all of the elements required for attending to the patient, a face-to-face consultation is considered necessary to complete the process. This may arise due to a particularly sensitive diagnosis, or because a surgical act is to be proposed that requires detailed explanation, or obtaining documents that are certified by the patient.
- •
Suitable: The clinical history is included in the virtual consultation.
- 5
The virtual consultation takes place telephonically to complete the clinical information and circumstances which aid diagnosis. The medical visit involves complying with all administrative work, together with requesting new complementary tests in those cases where this is considered necessary, and the issue of a new check-up appointment when this is indicated.
- 6
For those patients for whom a face-to-face visit is considered to be necessary, it will be maintained.
- 7
The pre-arranged face-to-face visit will be maintained for those patients who require evaluation in person, or those who have to fill out documentation. Nor will the appointment be modified for those patients who wish to be seen in a face-to-face visit, as well as those who did not answer the telephone call.
The OTD Department of hospital XXXXXXXXXXXX has played a full role in the consultations and data gathering. Its representatives then attended the consultations, to conclude the medical visit of those patients who had not finalised the medical function remotely.
The preparation of this work routine as well as the request for access to the identification of patient locations were approved by the hospital management.
Statistical analysisThe following variables were analysed: response to the telephone call, the supply of complementary tests and whether the consultation could take place remotely or whether a face-to-face visit were necessary.
Descriptive statistics were prepared, showing absolute values and percentages according to categories. The complete results are shown in tables.
Contingency tables with contrast were used to compare variables, by means of the χ2 test with Fisher’s correction in the case of values below five. Contrast was analysed for n-1 degrees of freedom, expressing the statistical value and significance of P.
The odds ratio (OR) was used to measure relationships, together with the confidence interval.
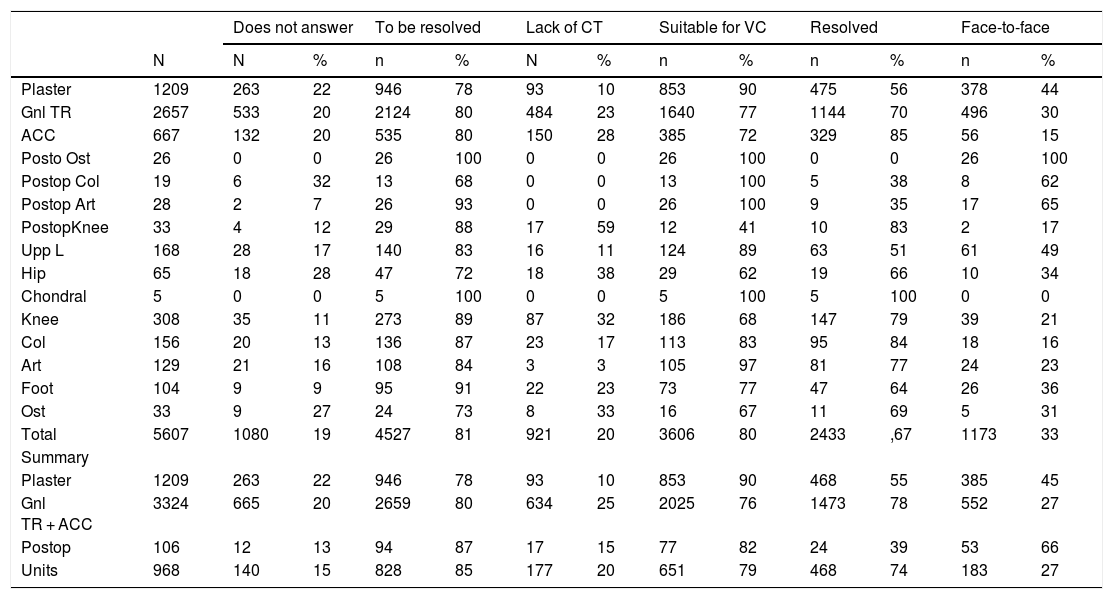
ResultsThe results obtained during the first four weeks of the implementation of remote consultation in the OTD Department of the XXXXXX from 16 March to 13 April 2020 were analysed. A total of 284 consultations took place during this period, 71 per week (Table 1).
Result of the implementation by stages and units.
| Does not answer | To be resolved | Lack of CT | Suitable for VC | Resolved | Face-to-face | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | N | % | n | % | N | % | n | % | n | % | n | % | |
| Plaster | 1209 | 263 | 22 | 946 | 78 | 93 | 10 | 853 | 90 | 475 | 56 | 378 | 44 |
| Gnl TR | 2657 | 533 | 20 | 2124 | 80 | 484 | 23 | 1640 | 77 | 1144 | 70 | 496 | 30 |
| ACC | 667 | 132 | 20 | 535 | 80 | 150 | 28 | 385 | 72 | 329 | 85 | 56 | 15 |
| Posto Ost | 26 | 0 | 0 | 26 | 100 | 0 | 0 | 26 | 100 | 0 | 0 | 26 | 100 |
| Postop Col | 19 | 6 | 32 | 13 | 68 | 0 | 0 | 13 | 100 | 5 | 38 | 8 | 62 |
| Postop Art | 28 | 2 | 7 | 26 | 93 | 0 | 0 | 26 | 100 | 9 | 35 | 17 | 65 |
| PostopKnee | 33 | 4 | 12 | 29 | 88 | 17 | 59 | 12 | 41 | 10 | 83 | 2 | 17 |
| Upp L | 168 | 28 | 17 | 140 | 83 | 16 | 11 | 124 | 89 | 63 | 51 | 61 | 49 |
| Hip | 65 | 18 | 28 | 47 | 72 | 18 | 38 | 29 | 62 | 19 | 66 | 10 | 34 |
| Chondral | 5 | 0 | 0 | 5 | 100 | 0 | 0 | 5 | 100 | 5 | 100 | 0 | 0 |
| Knee | 308 | 35 | 11 | 273 | 89 | 87 | 32 | 186 | 68 | 147 | 79 | 39 | 21 |
| Col | 156 | 20 | 13 | 136 | 87 | 23 | 17 | 113 | 83 | 95 | 84 | 18 | 16 |
| Art | 129 | 21 | 16 | 108 | 84 | 3 | 3 | 105 | 97 | 81 | 77 | 24 | 23 |
| Foot | 104 | 9 | 9 | 95 | 91 | 22 | 23 | 73 | 77 | 47 | 64 | 26 | 36 |
| Ost | 33 | 9 | 27 | 24 | 73 | 8 | 33 | 16 | 67 | 11 | 69 | 5 | 31 |
| Total | 5607 | 1080 | 19 | 4527 | 81 | 921 | 20 | 3606 | 80 | 2433 | ,67 | 1173 | 33 |
| Summary | |||||||||||||
| Plaster | 1209 | 263 | 22 | 946 | 78 | 93 | 10 | 853 | 90 | 468 | 55 | 385 | 45 |
| Gnl TR + ACC | 3324 | 665 | 20 | 2659 | 80 | 634 | 25 | 2025 | 76 | 1473 | 78 | 552 | 27 |
| Postop | 106 | 12 | 13 | 94 | 87 | 17 | 15 | 77 | 82 | 24 | 39 | 53 | 66 |
| Units | 968 | 140 | 15 | 828 | 85 | 177 | 20 | 651 | 79 | 468 | 74 | 183 | 27 |
Gnl TR. = General Traumatology; ACC = Accessibility; Postop = Postoperative; Col = Column; Ost = Osteosynthesis; Upp L = Upper limb; Art = Arthroscopy.
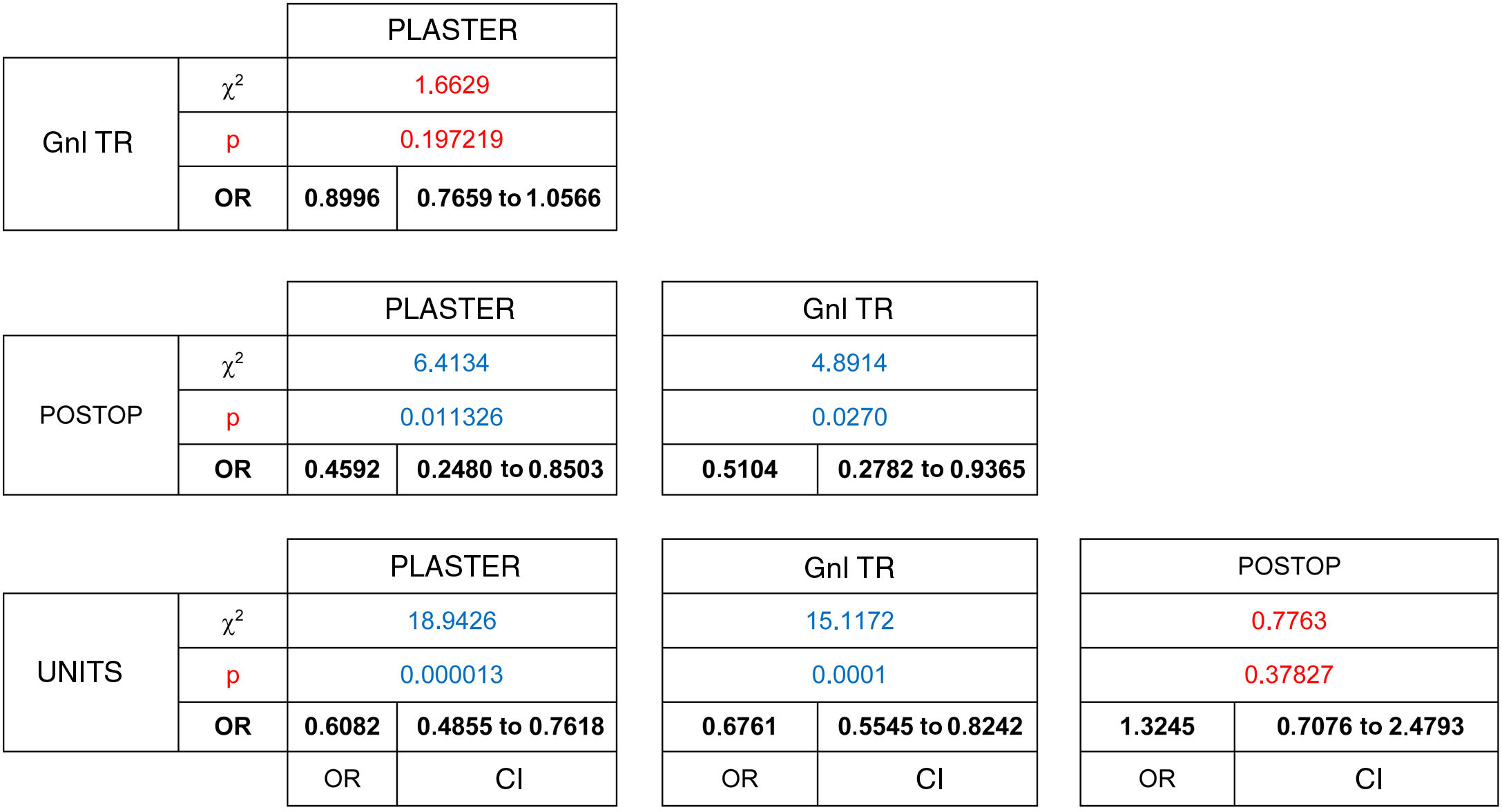
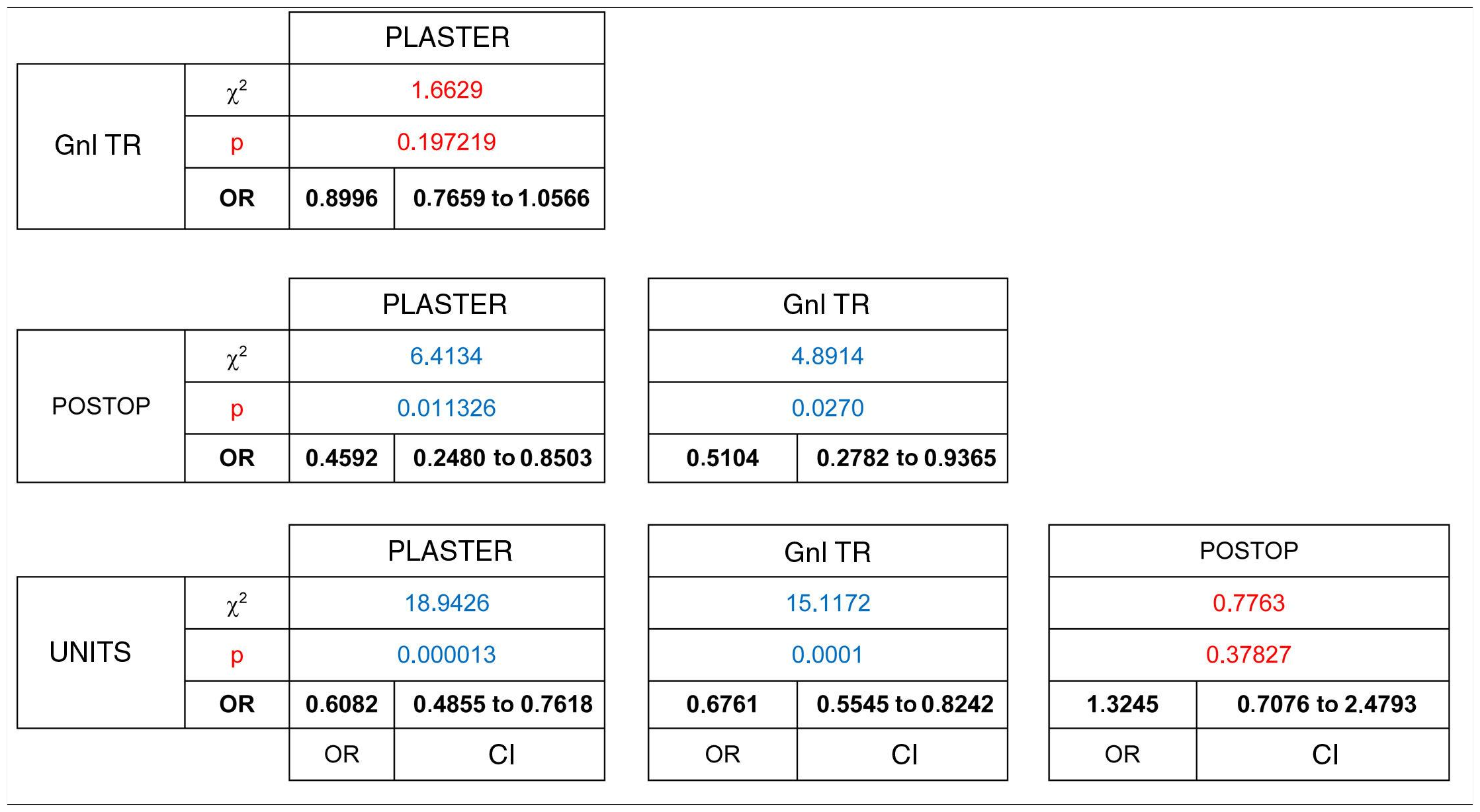
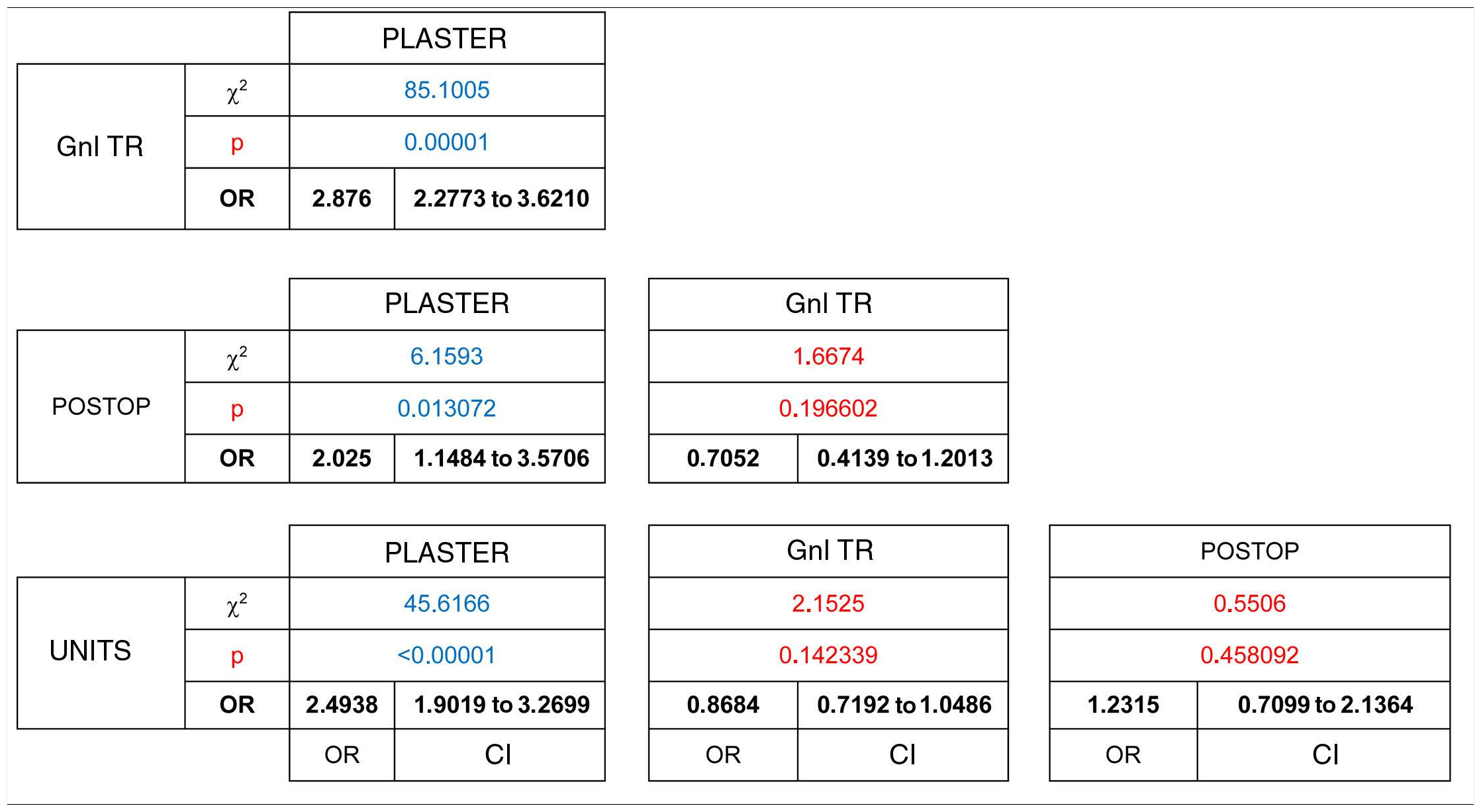
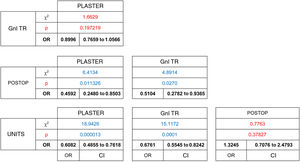
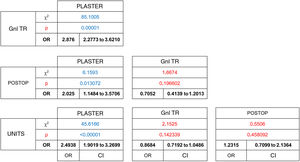
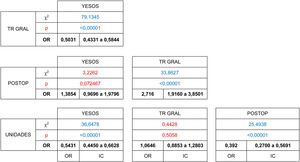
Telephonic contact was attempted in a total of 5619 patients, of whom 81% responded. Statistically significant differences were found in this response rate (χ2 [gl = 3, n = 5619) = 24.6439, P = .000018). Of these, a higher percentage of responses were obtained in those patients who received post-operative examinations (87%) and those who had a planned appointment with the different units (85%). The highest percentage of non-responders corresponded to follow-up consultations for emergency trauma pathology when after initial treatment patients had been referred for follow-up from the hospital emergency department (22%). Significant differences have been shown to exist in terms of the stronger association between unit consultations and not responding to the telephone call, when these are compared with the plaster unit consultations (OR = 0.60 [CI: 0.48 to 0.76]) and those with general traumatology (OR = 0.67 [CI 0.55 to 0.82]).(Table 2)
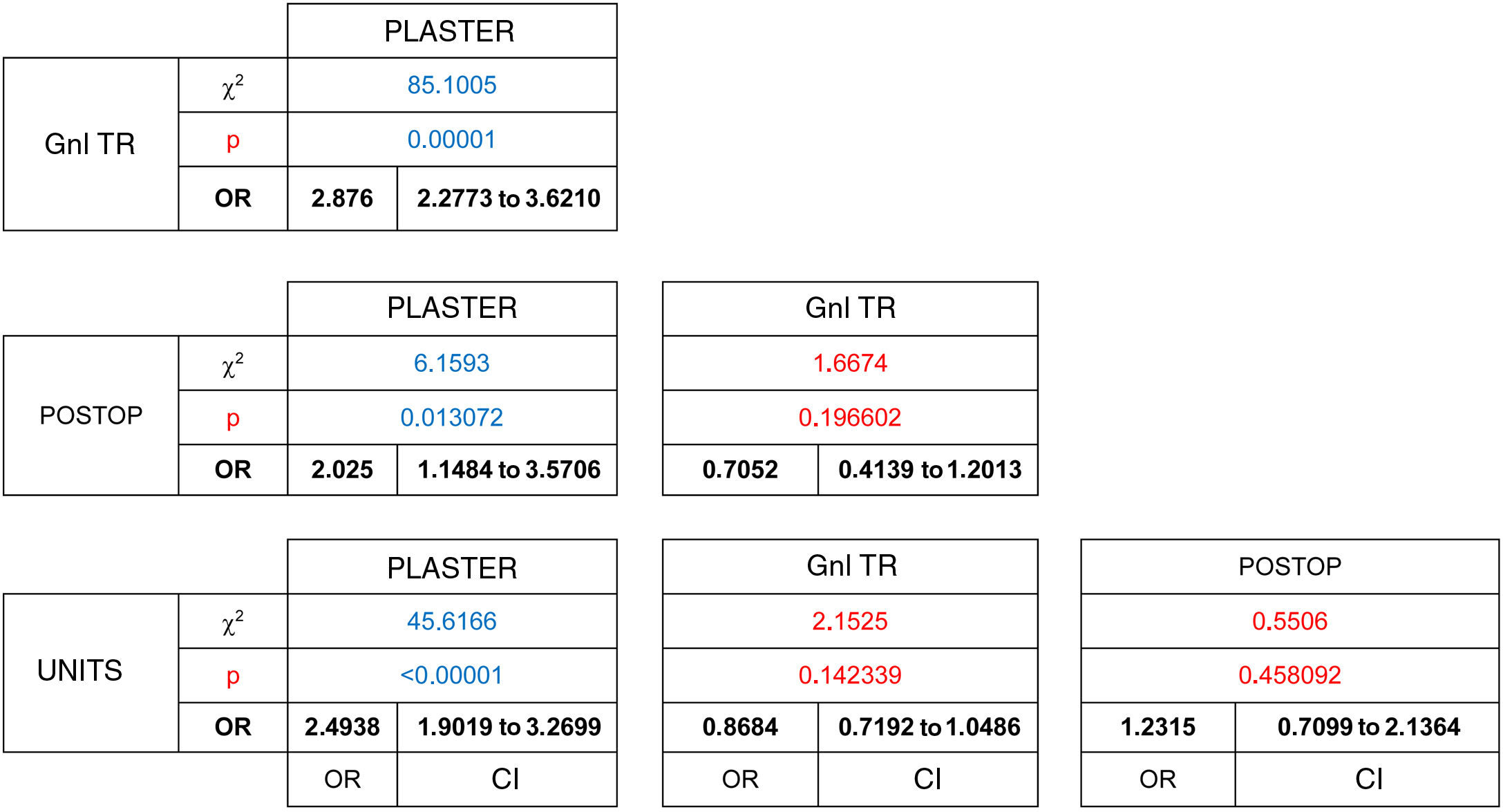
The degree to which complementary tests were appropriate for the visit was analysed for the patients who answered the telephone call. This analysis included the type of study, its quality and the satisfaction with the anatomical segments analysed, according to department protocols. Of these 4527 patients, only 80% had an up-to-date imaging test result at the time of consulting. Thus 20% went to an appointment that they could not finish regarding a diagnosis and proposed treatment, with a statistically significant difference between groups (χ2 (gl = 3, n = 4527) = 98.0395, P = .00001). The consultations by patients to check on recent trauma, plaster consultations, with 10%, and those immediately after operations (15%), were the ones with the highest proportion of patients who planned to visit with imaging test results, in comparison with those who attended a general traumatology consultation (OR = 0.34 [CI 0.27 to 0.43]), a postoperative check-up (OR = 0.49 [CI 0.28 to 0.87]) or a unit consultation (OR = 0.40 [CI 0.30 to 0.52]). On the contrary, as 75% of the patients who planned to visit general traumatology were going to do so without complementary test results, they were the least likely to supply such results at the moment of consultation. (Table 3)
Finally, 3606 patients were found to be suitable for assessment in virtual consultation. These were cases which had recently received surgical treatment; those who had been treated by the Emergency Department (90%) and those who had been operated for non-traumatic pathology (82%) were the ones who fulfilled the requisites for this form of resolution.
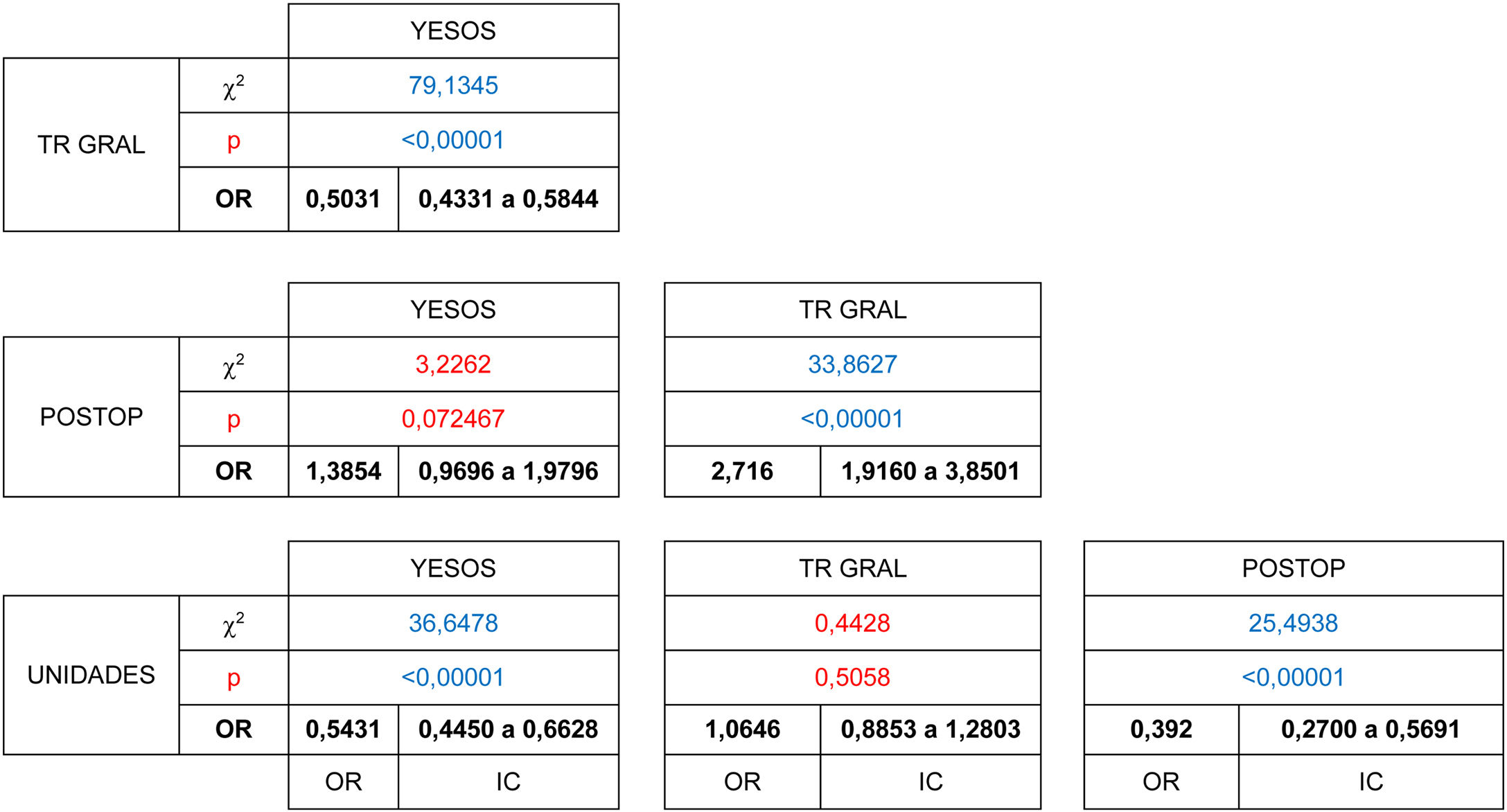
67% of the patients who were candidates to terminate care in consultations, were able to complete the virtual consultation. The difference between groups was shown to be statistically significant (χ2 [gl = 3, n = 2433] = 104.6246, P < .00001). The patients who had received treatment the most recently, patients who had been seen in the Emergency Department (55%) and those in immediate postoperative check-ups (39%) were the ones whose cases were the least suitable for virtual resolution. The patients with general trauma pathology (78%) were more likely to be suitable for virtual resolution than were those referred from the Emergency Department (OR = 0.50 [CI 0.43 to 0.58]) or who had visited to be seen in the units (74%), (OR = 0.54 [CI 0.44 to 0.66]) and could be resolved in this way without requiring a face-to-face visit. (Table 4)
The number of patients who did not need to visit the surgery, either because they were attended virtually (2433), or because the lack of complementary tests which hindered the medical action that was detected was resolved without the need for them to visit the surgery (921), amounted to 74% of the patients who had been called and responded to the telephone call (4527).
DiscussionAlthough remote consultations are a reality in our speciality that have been proven to be useful and economically effective, in our circle there is still resistance against a change of model that involves no direct contact with the patient.10
The current situation in which distancing is imposed between patients, family members and doctors has accelerated. It suddenly became necessary to adapt habitual medical practice to a new form that lacked the requisite structural changes11 and elements to aid communication. Nevertheless, given the doubt about whether it would be possible to properly carry out medical actions, there was still the possibility of face-to-face visits to ensure patient safety.
The exceptional circumstance of this pandemic has led us to use a form of care that we had reserved for repeat prescriptions that did not need medical reassessment. These were restricted to prescribing ortho-prosthetic materials that had to be renewed in the case of chronic pathologies, foot deformities and walking alterations with a neurological cause, where complications and ulcers could be managed by FCM.
We present the results of modelling for the implementation of a dynamic check-up consultation review, evaluating the suitability of offering non-face-to-face attention, for patients who had appointments with different types of surgery in our hospital.
It was not possible to include a control for epidemiological variables such as age, sex or educational level, as it was not possible to offer patients the possibility of selected one type of medical visit or the other.3 Previous publications have shown the differences in the degree to which different demographical sectors of the population accept medical interviews of this type.12 Our group includes patients from rural environments as well as from cities, with different levels of education, and these demographic variables have not been included in the analysis of their responses.
We encountered a barrier that affected the form of communication, as 19% of patients did not answer the telephone call. When the patients who answered the telephone call were analysed, those who were awaiting a check-up after surgery were found to be the most likely to answer. They varied from 100% of those who were waiting to go for a check-up after setting a fracture, to only 68% of the patients who had been operated for a spinal column pathology. It should be pointed out that these were patients who had been operated before the declaration of the state of alarm, although it was in force when they were due to their check-up. This meant that they were expecting to make a visit in the near future. Belonging to this group led to a statistically significant difference vs those patients who were expecting treatment for a general pathology or those who had been seen in the hospital Emergency Department. However, this difference was not significant respecting those patients who were awaiting evaluation in one of the specialised surgeries.
85% of the patients who were awaiting evaluation in a specialised unit answered the call, and those with foot or ankle pathology were the most likely to do so, at 91%. Only 81% of the patients who visited to evaluate hip and pelvis pathology answered the call.
The high number of patients who did not answer the telephone call may be understood to be based on the fact that they had not been informed previously that they may be called, thereby reducing their intentions of answering. This percentage may also be due to the fact that calls were made from terminals that did not identify themselves, so that answering was limited by the fact that other economic activities such as sales departments use this system, too.
The patients who were awaiting evaluation for a general pathology in standard consultations as well as in those created specifically to favour accessibility were the least likely to answer, with 20% of non-responders. The use of telemedicine in attending to patients referred from primary care has been shown to be effective in 69.6% of cases. A face-to-face visit is only necessary for a small number of patients, facilitating specialist care while saving time and impact on patients’ professional activities.13
Ninety percent of the patients who had been seen recently and those with recent trauma had sufficient complementary test results to be seen, as did 85% of those who had received surgery, so they were more likely to be attended in a single act. 74% of the patients referred by primary care and 80% of those referred by units showed the lowest rate of complementary tests completion. This may be because recent consultations are more likely to have the correct complementary tests, while this may not be so for those referred from other care units due to delayed appointments or unit check-ups as they require specific studies, complementary tests are updated less or they fall beyond the scope of possible FCM consultations. These referrals may sometimes arise precisely because of the limitation on requesting specific tests from facilities outside hospitals.14
The patients who require postoperative monitoring or a specific final examination, as well as care in the units, are the ones who are eventually seen the most often in face-to-face consultations. The implementation of remote medicine in the postoperative monitoring of patients has been found by systematic reviews to be effective, with a low rate of complications.15
Finally, only 33% of the patients who answered the remote consultation call required a face-to-face visit. This meant that social distancing was achieved in one of every three patients, and as could be expected, the patients whose surgical wounds were being monitored or who were awaiting the result of X-ray imaging of a setting bone were the ones who most required a visit of this type.
Limitations and strengths of this studyWithin the limitations of this study, it may be considered to have been undertaken by preparing a protocol to remedy the configuration of everyday clinical care. Nevertheless, given the urgent need for this, without the option of previous validation, this means the results have the value of a preliminary study that can be used to introduce corrections in habitual medical practice.
The technological barrier is a variable that should be taken into account. Nevertheless, the study was performed by means of telephone calls, a means of communication that is widely used in society.
Although patients expressed their satisfaction with the possibility of being attended without having to travel, the level of their satisfaction was not quantified by means of a validated questionnaire.
Due to the immediacy with which these consultations were implemented, it was not possible to analyse the degree to which the patients were suitable for consultations of this type or the option of referring them to face-to-face visits. On the contrary, instead of this, the indication for them to be seen in one type of visit or another was based on the clinical doubt as to their capacity to complete the medical act using the available means.
The inclusion of all the steps normally included in a medical visit is understood to be a strong point.
Another strong point of this study is understood to consist of the number of patients included for the extraction of data, although differences were not analysed depending on epidemiological variables such as age, sex or educational level.
ConclusionsIt can be concluded from this analysis that, even without having implemented measures to adapt to virtual-type consultations, patient evaluation and care using this type may attain a high percentage of satisfaction, while the aim of distancing was achieved in 74% of the patients with appointments.
The patients who require X-ray imaging tests or who are being monitored immediately after surgery are the ones who require observation and who attend check-ups. Monitoring fractures treated by osteosynthesis, postoperative arthroscopic surgery and observing soft tissues all require face-to-face attendance to a greater extent.
There is a need to review patient referral protocols for complementary tests, as due to lack of a prescription or suitability, 20% of them would have required a repeat visit for imaging tests that would enable consultation in a single act.
Level of evidenceLevel of evidence IV
FinancingThis work received no financing whatsoever.
Conflict of interestsThe authors have no conflict of interests to declare.
Montañez Heredia E, Nieto Orellana J, Gónzalez García C, Cano Obando L, Cárdenas Rebollo L, Abderrachid Al Chaid Y, Saadouli Arco M, Rodríguez Delourme I, Díez Izquierdo M, Prado Martín de Lucía LF, Durán Garrido J, Fernández Hijano M, Víquez da Silva R, Olofsson Suárez-Bárcena C, Jiménez Garrido C, García Vera JJ, Pérez Cardeña J, Irízar Jiménez S, Esteban del Castillo JL, García Píriz M, Gómez Palomo JM, F, Fernández Martín JA, Huertas Segador P, Santos de la Fuente J, Serrano Fernández J, Estades Rubio F, Fernández de Rota A, García Herrera JM, Leiva Gea A, Lombardo Torre M, Mariscal Lara J, Martín Castilla B, Urbano Labajos V, Sánchez García A, Quirante Sánchez V, Cañada Oya S, Rodríguez Jiménez M, Delgado Rufino B, Queipo de Llano Temboury A, Barón Romero M, López Hermoso MD, Benavente Casajús M, Loring Caffarena T, Chaparro Villar MA, De la Torre Solís, F.
Please cite this article as: Zamora Navas P. Resultado de la implantación de consultas telemáticas en cirugía ortopédica y traumatología durante la pandemia COVID-19. Rev Esp Cir Ortop Traumatol. 2021;65:54–62.