Insertional tendinopathy accounts for 23% of the pathology of the Achilles tendon. Surgery is indicated when conservative treatment of pain and functional limitation fails. Our objective is to analyse the clinical-functional results of surgical treatment with disinsertion, debridement and double row reattachment with high strength suture tape.
Material and methodsWe present 13 patients with insertional Achilles tendinopathy, treated between February 2015 and October 2016. In all of them we performed inverted T-tendon disinsertion, debridement and calcareoplasty followed by double row tendon re-anchorage, without knots, with high resistance suture tape. Functional results were assessed with the AOFAS scale before and after surgery, with an average follow-up of 22 months.
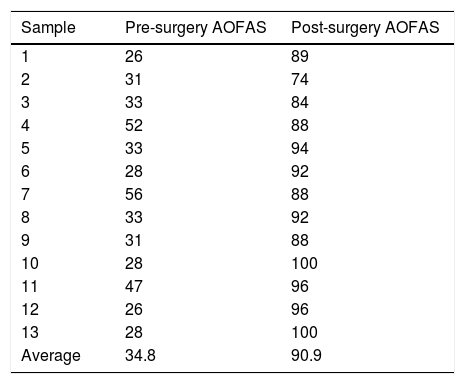
ResultsThe patients, 11 males and 2 females, with an average age of 43 years; presented a preoperative AOFAS score of 34.77±10.1 that reached 90.85±7 points after the operation, with an average increase of 56.08 points (IC95% 48.13–64.02 – p<0.01). The time to return to sports activities was 19 weeks (16–22). There were no complications.
ConclusionThe technique we present reports excellent results as a surgical treatment of insertional Achilles tendinopathy with intralesional calcification; it allows a wide contact surface between bone and tendon and an earlier return to previous sports activity.
La tendinopatía insercional supone el 23% de la patología del tendón de Aquiles. La cirugía está indicada cuando fracasa el tratamiento conservador del dolor y limitación funcional. Nuestro objetivo es analizar los resultados clínico-funcionales del tratamiento quirúrgico con desinserción, desbridamiento y reanclaje en doble hilera con cinta de sutura de alta resistencia.
Material y métodosPresentamos 13 pacientes con tendinopatía insercional de Aquiles, tratados intervenidos entre febrero de 2015 y octubre de 2016. En todos se realizó desinserción del tendón en T invertida, desbridamiento y calcaneoplastia seguido de reanclaje del tendón en doble hilera, sin nudos, con cinta de sutura de alta resistencia. Se valoraron los resultados funcionales con la escala AOFAS antes y después de la cirugía, con un seguimiento medio de 22 meses.
ResultadosLos pacientes, 11 varones y 2 mujeres, con una edad media de 43 años; presentaban una puntuación AOFAS preoperatoria de 34,77±10,1 que alcanzó 90,85±7 puntos tras la intervención, con un incremento medio de 56,08 puntos (IC95% 48,13-64,02 – p<0,01). El tiempo hasta la reincorporación a actividades deportivas fue 19 semanas (16–22). No hubo ninguna complicación.
ConclusiónLa técnica que presentamos reporta unos resultados excelentes como tratamiento quirúrgico de la tendinopatía insercional del Aquiles con calcificación intralesional; permite una amplia superficie de contacto entre hueso y tendón y una reincorporación más precoz a la actividad deportiva previa.
Achilles’ tendon complaints may be classified in 2 major groups, depending on their location: insertional tendinopathy if it affects the enthesis zone, and non-insertional tendinopathy if it is located 2cm proximal to the tuberosity of the calcaneus.1
Insertional tendinopathy or Achilles’ enthesitis represents from 20% to 24% of Achilles’ tendon complaints.2,3 It has multifactorial aetiology and it is associated with intrinsic biomechanical conditions of the foot and ankle as well as with footwear, age, obesity, mechanical overload and impact sports.4,5
It is a chronic process of tendon degeneration associated with the appearance of different degrees of calcification on the enthesis. Clinically it manifests as swelling and pain located on the posterior tuberosity of the calcaneus, together with a functional deficit.2,3 Other complaints affect the enthesis of the tendon and also involve pain in this zone, such as retrocalcaneal bursitis, retrocalcaneal exostosis and Haglund’s deformity, and they may appear in isolation or in association, or with Achilles’ tendon insertional tendinopathy.2
Treatment is initially based on a combination of analgesia, rest and stretching exercises for the Achilles-calcaneal-plantar system, although no therapy has been proven to be effective in the management of this complaint, so that surgical treatment is often used.2,6 Many techniques have been described, and all of them seek to eliminate the degenerate region of the tendon by more or less broad disinsertion for a complete debridement of the inflammatory tissue and calcifications. When necessary resection of the posterior calcaneal bone prominence or calcaneoplasty may be added.2,3,6 Reinsertion of the tendon, with or without elongation, is necessary to obtain good functional results after the intervention.2
The aim of this work is to analyse the clinical-functional results of open transachilles calcaneoplasty technique and double row tendon repair.
Material and methodsPatients over the age of 18 years were included with insertional tendinopathy of the Achilles’ tendon treated surgically with calcaneoplasty technique associated with SpeedBridge® (Arthrex Inc, Naples, FL, U.S.A.).
Diagnosis was clinical and radiological in all cases, with compatible nuclear magnetic resonance imaging: pre-Achilles’ tendon bursitis, insertional tendinopathy with different degrees of tissue degeneration, including partial intratendinous tears and microcacalcifications; no case had a complete tear of the tendon. All of the patients had evolved with persistence of the pain and functional limitation without responding to conservative treatment during at least one year. The patients had no other diseases associated with the foot or ankle. They were all treated surgically from February 2015 to October 2016, with debridement of the pathological tissue and disinsertion and reanchoring of the tendon tissue with two rows of knot-free high strength braided tape using the SpeedBridge® (Arthrex Inc, Naples, FL, U.S.A.) technique. Patients with a follow-up of less than 18 months were excluded. The recorded data included patient age and sex, the foot involved and any complications associated with the intervention during the follow-up period (dehiscence of the surgical wound or superficial/deep infection; tearing of the Achilles’ tendon).
A total of 13 patients were operated following the failure of conservative treatment, with clinical evolution over 35–72 weeks. The clinical/functional results were evaluated using the AOFAS (American Orthopaedic Foot and Ankle Society) scale and the VAS (visual analogue scale) prior to surgery as well as afterwards (at the end of the follow-up period). The duration of rehabilitation treatment was also recorded, together with the time elapsed until the patients resumed their normal sports activities.
Data are expressed as core tendency measurements and they were analysed by the STATA 14/CI (StataCorp) statistical program, using the Wilcoxon test for paired samples. The cut-off point p<.05 was set as the limit of statistical significance.
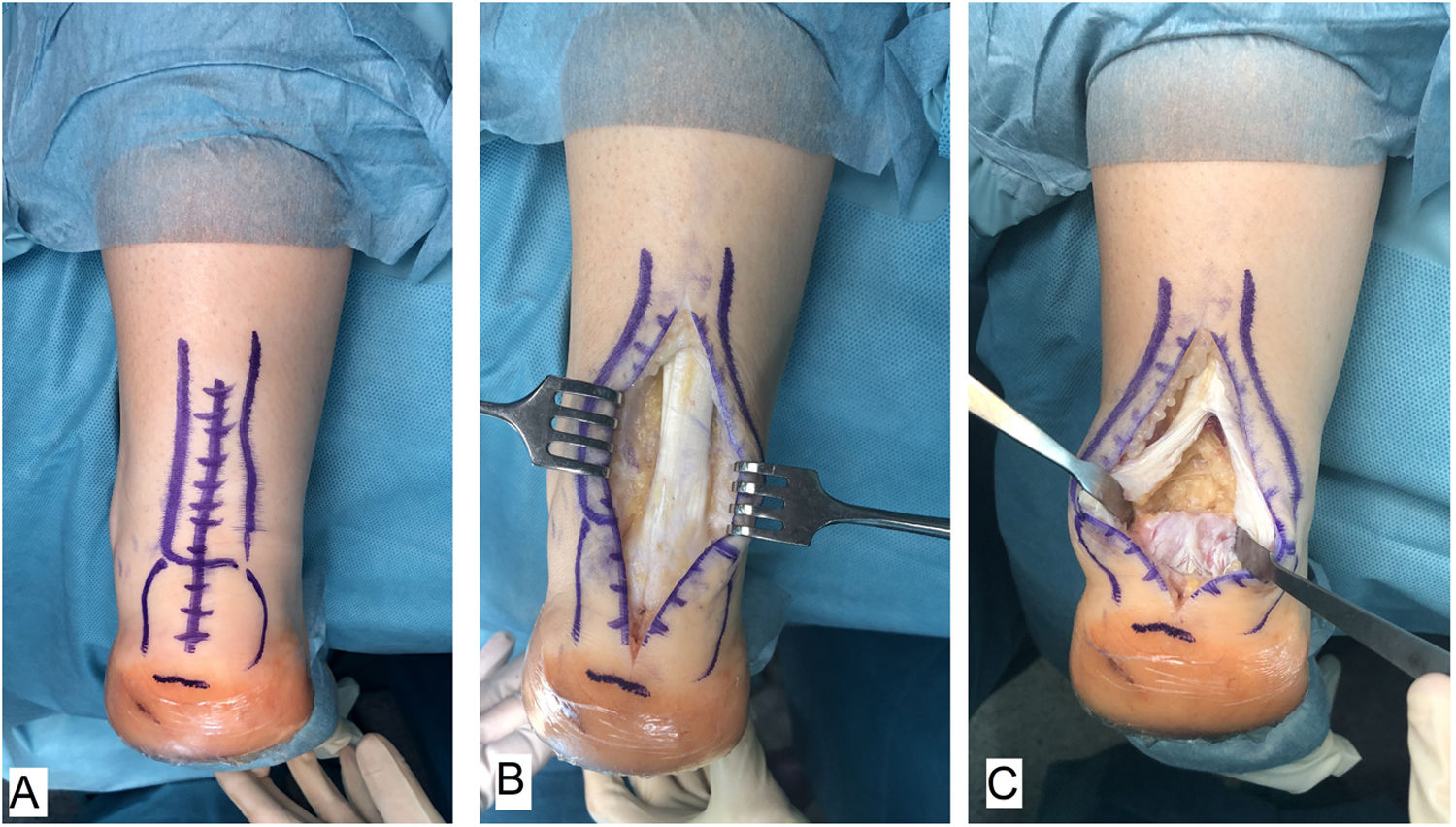
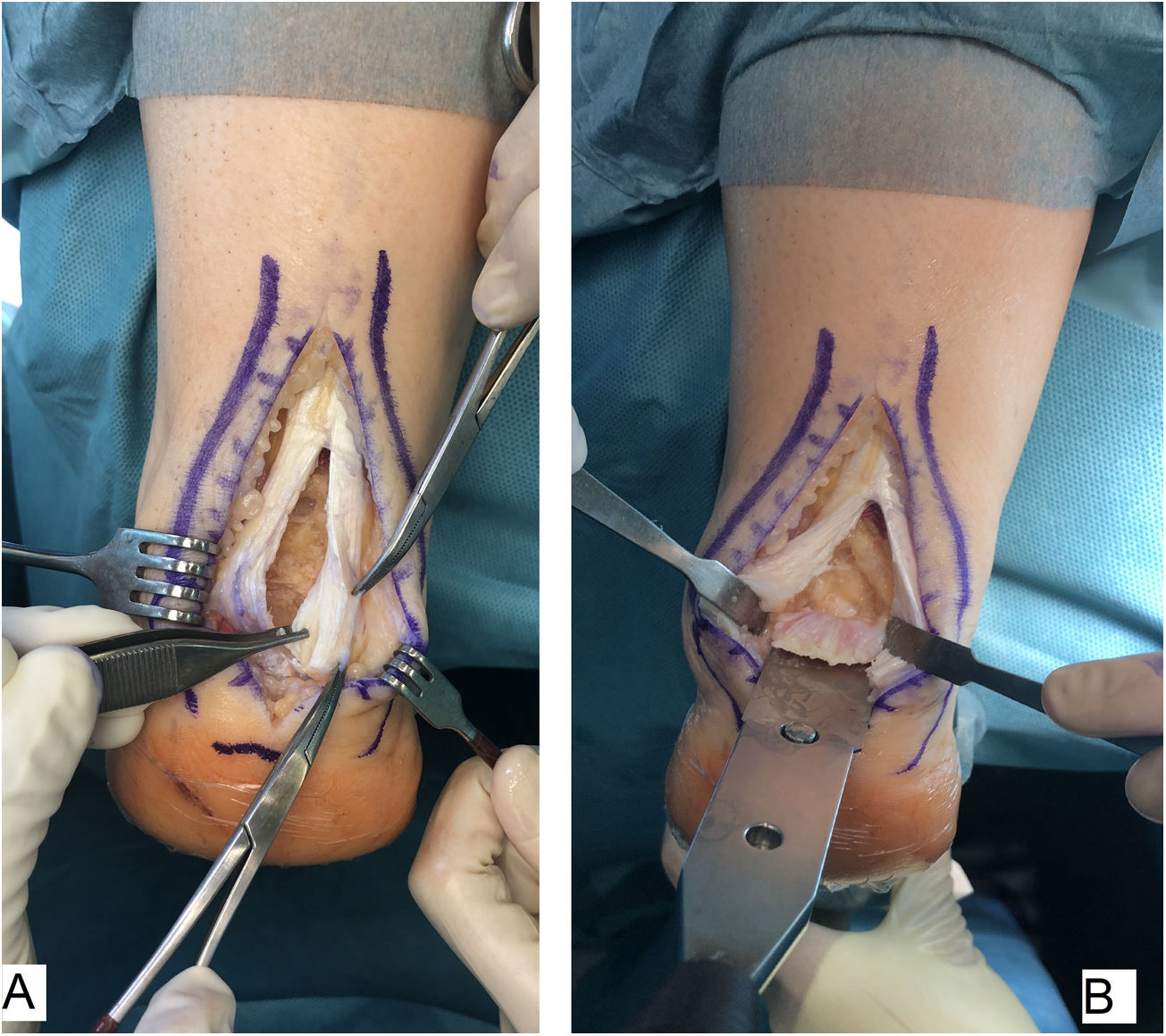
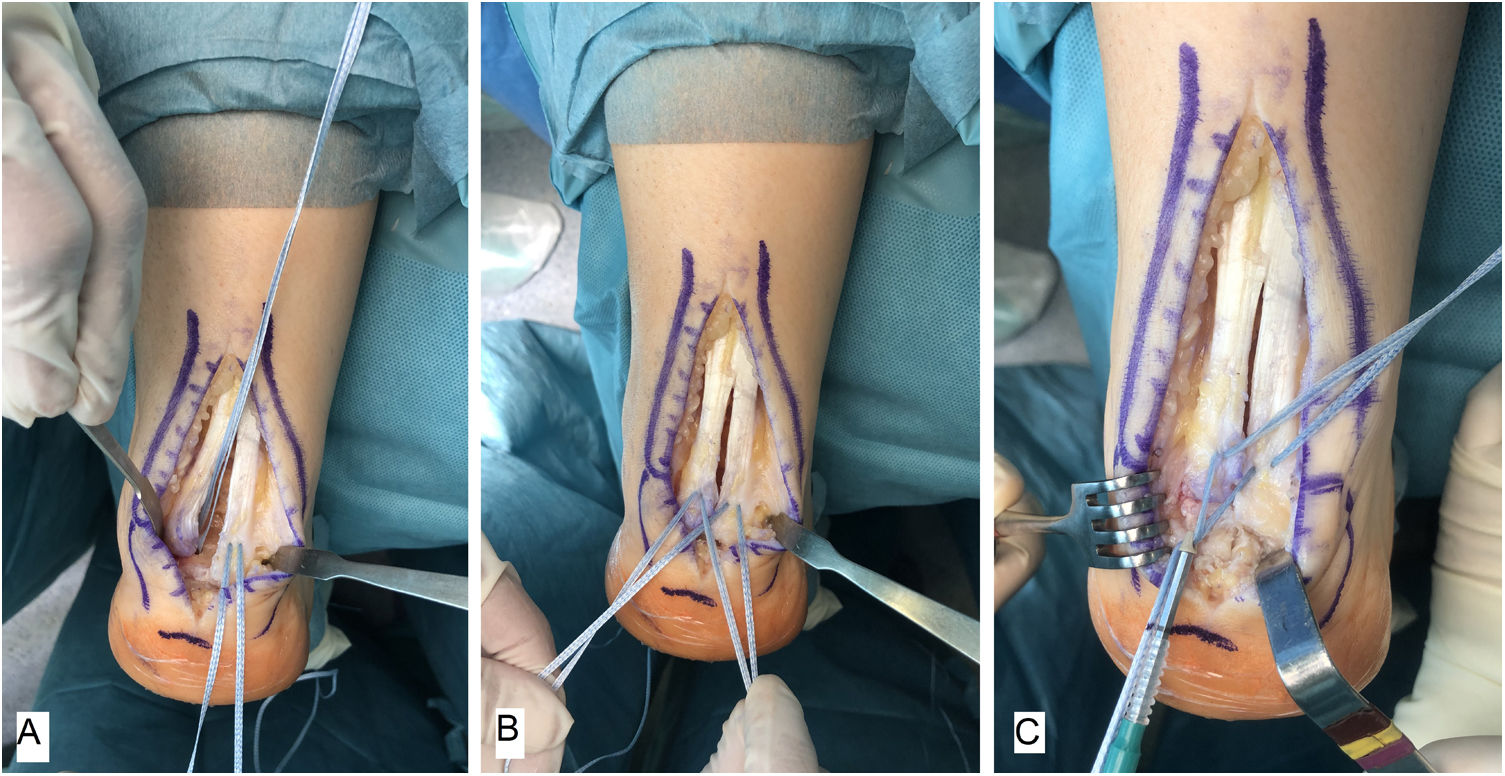
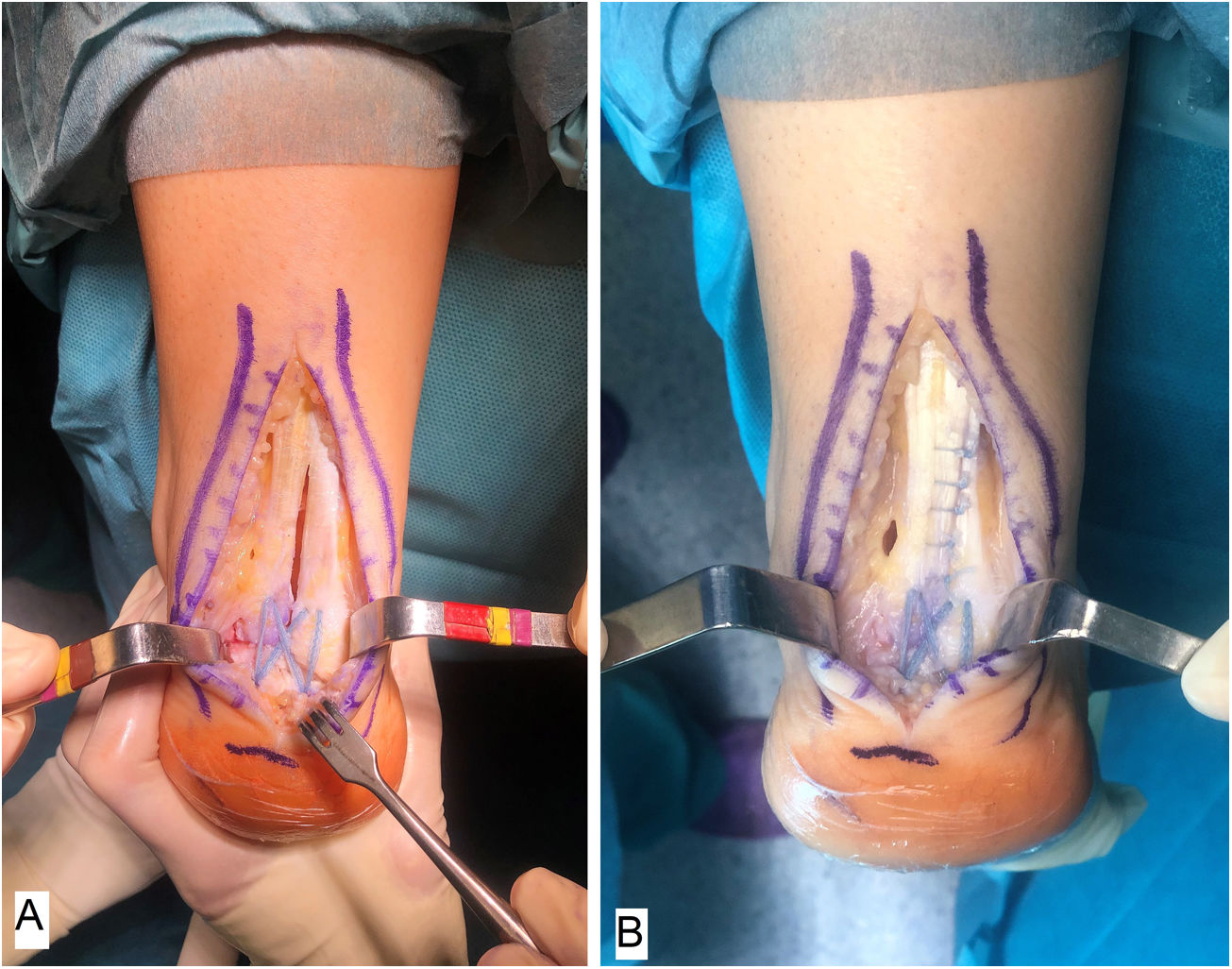
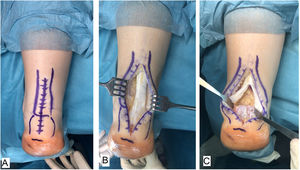
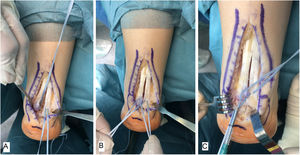
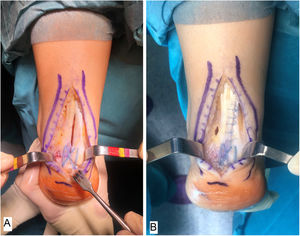
Surgical techniqueAll of the patients were treated by the same surgeon (JVR) using the same surgical procedure. In prone decubitus position with an ischemia sleeve on the thigh and perioperative antibiotic prophylaxis (2g cefazolin, 1g vancomycin in the case of patients allergic to cephalosporin), an incision of approximately 15cm was made along the median line over the Achilles’ tendon, separating both flaps of skin. After identifying the Achilles tendon and its enthesis over the posterior apophysis of the calcaneus, it was partially disinserted in the form of an inverted T, keeping the medial and lateral insertions (Fig. 1). After careful debridement of the degenerate distal portion, including the intratendinous calcifications, exeresis was performed of the posterior exostosis of the calcaneus with an oscillating saw, and the bone surface was prepared for the reinsertion of the tendon (Fig. 2). The tendon was anchored using harpoons and high strength braided tape while maintaining a suitable tension. In our case we use FiberTape® (Arthrex Inc, Naples, FL, U.S.A.) in a crossed double row pattern with no knots, following the SpeedBridge® (Arthrex Inc, Naples, FL U.S.A.) technique (Fig. 3). Lastly, the tendon was repaired using continuous braided 0 bioabsorbable suture, including the parathenon, and the skin was closed using loose vicryl rapide™ bioabsorbable stitches (polyglactin 910) (Fig. 4).
All of the patients were immobilised during 2 weeks with a splint in neutral position; subsequently they were allowed to commence partial assisted loading with crutches and protected by an orthosis (a “Walker” type boot in neutral position). Rehabilitation commenced 4 weeks after surgery, consisting of a combination of electrotherapy and mobility exercises together with gradual discharge muscle strengthening, following the recommendations of the rehabilitation doctor, adapted to the needs of each patient. The orthosis was kept on until 12 weeks of treatment had been completed, after which loading with their usual footwear was permitted, while maintaining rehabilitation therapy for muscle strengthening and proprioception, adapted to the needs of each patient.
ResultsThe study was composed of a total of 13 patients; 11 men and 2 women, with an average age of 43 years (range: 35–55 years). Respecting laterality, 6 patients were operated on their right Achilles’ tendon and 7 were operated on the left side (Table 1). The median duration of follow-up was 22 months (range 18–24 months). Their average on the VAS pain scale was 8.8 in the evaluation prior to surgery and 1.3 points at the end of follow-up. The average score obtained on the AOFAS scale before surgery was 34.8 points, which rose to 90.9 points after surgery (Table 1). There was therefore a statistically significant average increase of 56.1 points (CI 95%, 48.1–64.1; p<.01). None of the patients developed complications during the postoperative follow-up. All of them received complementary rehabilitation therapy guided by the rehabilitation doctor during from 5 to 10 weeks after the removal of the orthosis, and they were able to recommence their leisure time sports activities (paddle tennis, football or basketball) after an average period of 19 weeks (range 16–22 weeks), without any restriction.
DiscussionThe tendon insertion of the Achilles’ tendon over the posterior tuberosity of the calcaneus is a highly specialised fibrocartilage structure, composed of the enthesis itself and the subtendinous bursa.7 Prolonged overloading of the tendon gives rise to the formation of bone spurs due to endochondral ossification and longitudinal intra-substance fissures that are more intense in the tendon-bone load transfer points.7,8 Benjamin et al. conclude that the bone spurs in the enthesis are due to an adaptive process of the tendon, which thereby increases its contact surface with the bone to withstand the mechanical loads it is under.9 These chronic changes are manifested clinically as swelling, pain and functional limitation; diagnosis of insertional tendinopathy is clinical above all, although we may also use complementary imaging techniques such as magnetic resonance imaging which make it possible to differentiate between different degrees of tendon involvement.10
Initial management is conservative in all cases.2,6 it consists of a combination of non-steroid anti-inflammatory analgesics and physical measures such as footwear modification, stretching exercises of the Achilles-calcaneus-plantar system, temporary orthoses and different forms of rehabilitation and physiotherapy treatments. The degree to which these treatments are effective varies widely, depending above all on the severity of the condition and degeneration of the tendon. The results of surgical treatment are better in those patients with intra-substance lesions in magnetic resonance images.10,11 Surgical treatment is indicated when the symptoms persist for more than 3–6 months in spite of conservative treatment.12
Surgical treatment is based on the resection of degenerated tissue, including the bursa and calcifications, with calcaneoplasty of the posterior bone prominence.13 This involves the partial disinsertion of the tendon over the tuberosity of the calcaneus, which may weaken it, with the resulting risk of tearing. Nevertheless, limited debridement may lead to failure of the surgical treatment.14 It has been proven that disinsertion of up to 50% of the tendon surface makes safe early loading possible without complications involving tearing,14 so that broader resections should be accompanied by an incremental technique or tenodesis.13,15,16 Several authors prefer the complete disinsertion of the tendon from the first, as this permits broad resection of the inflamed tendon and better exposure of the bone during the calcaneoplasty, in comparison with disinsertion of less than 50%.15,17 We prefer a central inverted T incision which conserves the medial and lateral insertions, enabling broad debridement of the pathological tissue without the risk of vascular or nerve damage, as this has been proven to give good clinical and functional results over the long-term.18,19
Tendon reinsertion or tenodesis, with or without increment, is associated with good results after surgery.13,15,16 Taking the treatments of the shoulder rotator cuff as the reference, different techniques of reinserting the calcaneal tendon using harpoons have been described, with a single or double row configuration.20–22 In a cadaver-based study Pilson et al. conclude that there is no biomechanical superiority in the double row configuration versus a single row of harpoons.21 On the other hand, Beitzel et al. in another cadaver-based study report a larger contact area that is initially statistically significant, with comparable implant displacement in both groups when it is subjected to repeated loads.23 Nevertheless, the double row configuration has been proven to have a greater bone-tendon contact area for scarring,22–24 which increases the strength of the suture and offers more support for loads that, theoretically, reduces scarring time.22,24 This benefit of the double row has led to widespread use of techniques such as SutureBridge™ (Arthrex Inc, Naples, FL, U.S.A.), an anchorage system that is based on the use of harpoons and high-strength braided suture in a crossed double row configuration which permits safe early loading, above all in young pacientes.25 This technique has been proven to give excellent clinical-functional results over the medium to long term, with a low rate of complications.26,27 Modifications of this technique have been described.28 The modified technique with knots in the proximal suture was found to be biomechanically superior in cadaveric studies that compared both alternatives, as it is stronger in case of repeated loads, and no differences were found in terms of the bone-tendon contact surface or implant failure.29 Alternatives to use of harpoons for tendon reinsertion have been described, with cortical anchorage devices through the bone;30 the corresponding results are comparable to those with the techniques described in cadaveric studies, and they may be of interest above all for osteoporotic bone, as they offer greater load resistance than harpoon anchorages.31
In comparison with the use of high-strength No. 2 conventional suture, several biomechanical studies in animal models have shown that braided tape is superior in tendon repair.32–35 Tape offers better traction resistance and less of a sawing effect on the bone if used through tunnels in the bone32 and less tendon tear when it is subjected to cyclic traction.35 Use of this tape together with harpoons permits a greater maximum load before failure in comparison with conventional suture,33 and it has also been shown to offer a larger contact surface and higher strength than suture made using arthroscopy.34 In spite of the good biomechanical results shown in experimental models, Boyer et al. report a lower rate of tendon tearing after arthroscopic repair of the supraspinatus tendon with braided tape and harpoons in a double row vs repair with conventional suture. However, they did not find that one of these techniques was clinically better than the other over the medium term in a series of 73 patients.36
The SpeedBridge™ technique (Arthrex Inc, Naples, FL, U.S.A.) is a modification of the above-mentioned SutureBridge™ technique, which uses FiberTape® instead of suture thread. There is little in the literature on the use of suture tape in Achilles’ tendon repair,37 although this is the first work to present the results of using suture tape for reinsertion of the tendon in the calcaneus as part of the treatment for Achilles’ tendon insertional tendinopathy. Our work shows good results in terms of improved functional scales as well as the lack of complications, although the latter may be due to the small size of the sample. Skin closure in our hospital uses vicryl rapide™ (Polyglactin 910) absorbable suture that does not require stitches to be removed, minimising wound manipulation. Some similar publications show complications of the soft parts in scars above all.27,38 Rigby et al., in a series of 43 patients treated with high-strength suture in double row configuration, reported 2 cases of wound dehiscence and one deep infection that required FHL transfer in a second stage.27 A similar study with 14 patients reported only one patient with the complication of superficial wound infection.38 Although complications with implants such as tearing or loss of bone anchorage have been reported in cadaver-based studies,23,29 have not been reported in clinical practice.
The chief weakness of this work is the sample size, which impoverishes its statistical significance. On the other hand, the efficacy of the treatment would be shown more strongly by postoperative imaging proof of tendon-bone integration after repair. Fuller studies are therefore required with a higher number of patients, to compare this technique with others that have already been described for the treatment of Achilles’ tendon insertional tendinopathy.
This surgical treatment is easy to reproduce, it had no complications over the short to medium term in our series, and it gives excellent functional results, with a significant improvement in the AOFAS score based on our results.
The larger bone-tendon contact surface achieved by the combination of braided tape and double row construction permitted early load-bearing for the patients, who soon recommenced their previous sports activities without any functional limits.
ConclusionsPartial disinsertion in inverted T of the Achilles’ tendon and repair with two rows is an effective technique for the treatment of insertional tendinopathy. It is easy to reproduce achieves excellent functional results. It also permits easy and safe load-bearing and rapid functional recovery.
Level of evidenceLevel of evidence IV.
FinancingThis study received no specific support from public, private or not-for-profit sector bodies.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Abarquero-Diezhandino A, Vacas-Sánchez E, Hernanz-González Y, Vilá-Rico J. Estudio de los resultados clínico-funcionales de la calcaneoplastia abierta y reparación tendinosa con sistema de cinta y doble hilera en el tratamiento de la tendinopatía insercional del tendón de Aquiles. Rev Esp Cir Ortop Traumatol. 2021;65:47–53.