The snapping scapula syndrome is a grating sensation located in the scapulothoracic region that appears with movement. This sign is occasionally related to tumours.
ObjectiveTo show the high incidence of this relationship (clinical sign-tumour), and to be aware of it when performing a differential diagnosis.
Materials and methodsRetrospective study of the elastofibromas dorsi (ED) and scapular osteochondromas (SO), which may have presented with the sign under study in our centre over the last 17 years (1993–2009). Thirty-seven ED and 6 SO were identified. The series was divided into group A (ED) and group B (SO). Mean follow-up was 7 years. The cohorts are made up of 23 women and 4 men with a mean age of 57 years (42–78) in group A, and there were 2 women and 4 men with a mean age of 20 years (11–28) in group B. Action was taken to identify the initial medical sign at diagnosis, the treatment carried out, and the outcome.
ResultsAround 21% of these tumours are reported to be associated with physical activity. The initial symptom was a painful mass in 81% of the patients, followed by a scapular snapping or clicking in 30 out of the 43 patients (70%). The treatment of choice was resection in both groups. A noticeable improvement in terms of pain was seen (VAS 7.5 preoperatively, 2.8 postoperatively).
ConclusionThe presence of snapping scapula has a strong relationship to tumours of the scapulothoracic region. Therefore it is important to be aware of this.
El chasquido escapular es un crujido localizado en la región escapulotorácica que aparece con los movimientos. Este signo clínico está relacionado en ocasiones con los tumores escapulares.
ObjetivoMostrar la alta incidencia de esta relación (tumor escapular-chasquido) para recordar la misma al realizar el diagnóstico diferencial.
Material y métodoEstudio retrospectivo de elastofibromas dorsi (ED) y osteocondromas escapulares (OE), que puedan presentar el signo clínico a estudio, en nuestro centro en los últimos 17 años (1993-2009). Se han identificado 37 ED y 6 OE. El tiempo medio de seguimiento ha sido de 7 años. Se ha divido la serie en grupo A (ED) y grupo B (OE). Las cohortes las forman, en el grupo A: 23 mujeres y 4 varones, media de 57 años (42-78), y en el grupo B: 2 mujeres y 4 varones, media de 20 años (11-28). Se ha procedido a identificar el signo clínico inicial al diagnóstico, el tratamiento realizado y la evolución.
ResultadosSe reporta una asociación entre la actividad física y la presencia de estas tumoraciones del 21%. La clínica inicial fue una masa dolorosa en el 81% de los pacientes, y un chasquido escapular en el 70% (30 de 43). El tratamiento de elección fue la exéresis en ambos grupos, obteniendo una notable mejoría en el dolor (VAS: 7,5 preoperatorio; 2,8 postoperatorio).
ConclusiónLa presencia de chasquido escapular tiene una fuerte relación con los tumores de la región escapulotorácica, por lo que debemos conocer esta asociación.
The clinical sign known as “snapping scapula” consists in a crepitus or creaking from the scapulothoracic region during arm movements. It was first described in 1867 by Boinet1 and later stratified according to the intensity of the sound by Mauclaire.2
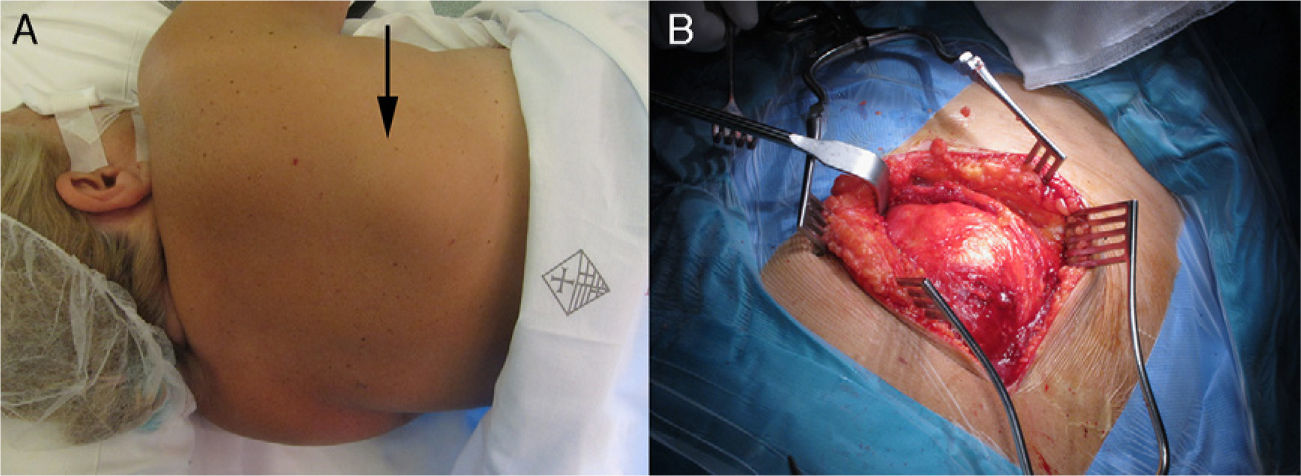
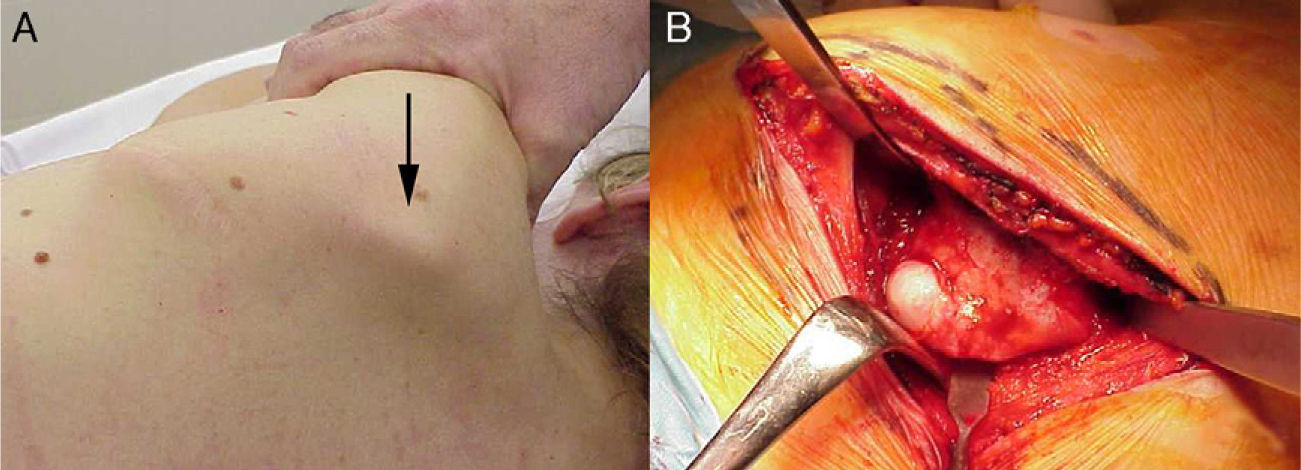
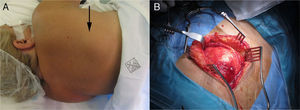
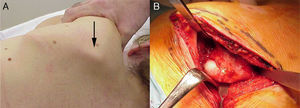
The sound itself is produced by the presence of a soft tissue (Fig. 1) or skeletal (Fig. 2) abnormality between the scapula and the thoracic wall. The effects of this crepitus range from no other symptoms to associated pain of variable intensity.3 It often appears as a diffuse pain of moderate intensity, even going unnoticed and probably underdiagnosed in many cases. It has been demonstrated that the majority of imaging scans provide little information unless there is an associated skeletal injury. Conservative treatment with anti-inflammatory agents and painkillers, along with subsequent physical rehabilitation, normally achieves an improvement of symptoms. Therefore, a clear aetiology of the pain is often not established and this may hide tumoural lesions, such as elastofibroma dorsi (ED) or osteochondroma, the entities studied in this work.
The incidence of scapular tumours such as those studied is around 2%.4,5 As described in classical texts, like that by Dahlin,6 we must bear in mind that there is a wide variety of tumours which can be found in the scapula. Some of these lesions are benign, including chondromas, chondroblastomas, osteoid osteomas, ED or osteochondromas, which we examine in this work. It is also possible to find malignant tumour lesions, such as chondrosarcomas, Ewing sarcomas, osteogenic sarcomas, fibrosarcomas or myelomas among others. Dahlin6 described an incidence of scapular tumours around 0.3% after examining a series of 1853 bone tumours.6 Other authors, such as Ochsner et al.7 reported a scapular location in 19% of thoracic tumours. Dineen and Boltax8 reported 11% of scapular tumours in their series of thoracic wall tumours.
The aim of this work is to present our series of scapular tumours, focusing on scapular osteochondroma (SO) and ED, in order to highlight which of them presented scapular snapping as a relevant clinical sign.
Materials and methodsWe conducted a review of scapular tumours, focusing on ED and SO, at our centre during the last 17 years (1993–2009), examining whether they presented snapping scapula.
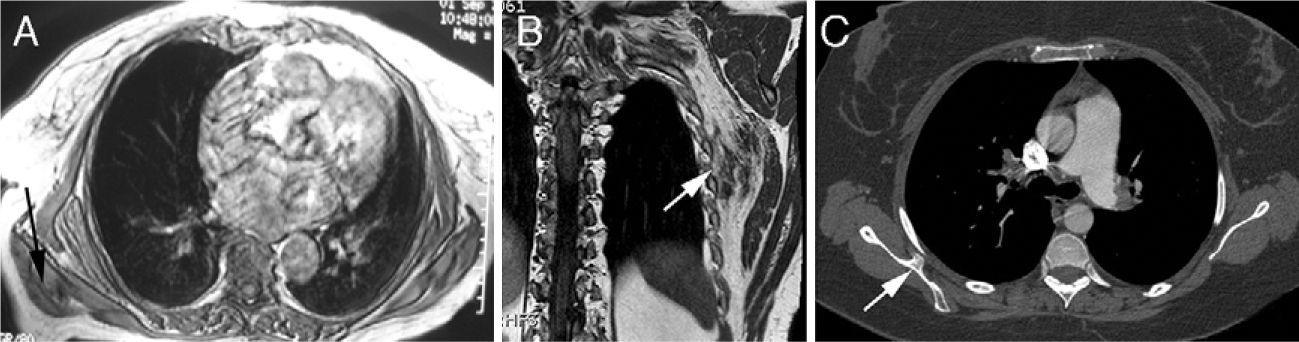
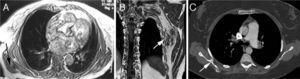
Demographic and clinical data of patients and their evolution were taken from clinical records at our centre. The study focused on these tumours, based on the work by Kuhne et al.9, in which the differential diagnosis of scapular tumours should bear in mind the presence of ED and SO. We formed 2 separate groups: group A included patients who suffered ED (Fig. 3A and B) and group B included those who suffered SO (Fig. 3C).
In group A we found 37 scapular tumours, including 10 bilateral cases, which were confirmed as ED by the anatomopathological study among a cohort consisting of 23 females and 4 males, with a mean age of 57 years (range: 42–78 years). ED was located at the lower edge of the scapula in all cases. In group B, we identified 6 cases of SO among 4 males and 2 females, with a mean age of 20 years (range: 11–28 years).
The mean follow-up period of the cohort was 7 years (range: 2.5–13.4 years). We used a visual analogue scale (VAS) to assess pain, where 0 represented no pain and 10 represented severe pain. The indication for surgery was determined according to the clinical evolution of patients. Conservative treatment was employed with those who had a good evolution of pain, reserving surgery for those cases where pain was severe or persistent (81% of group A and 100% of group B).
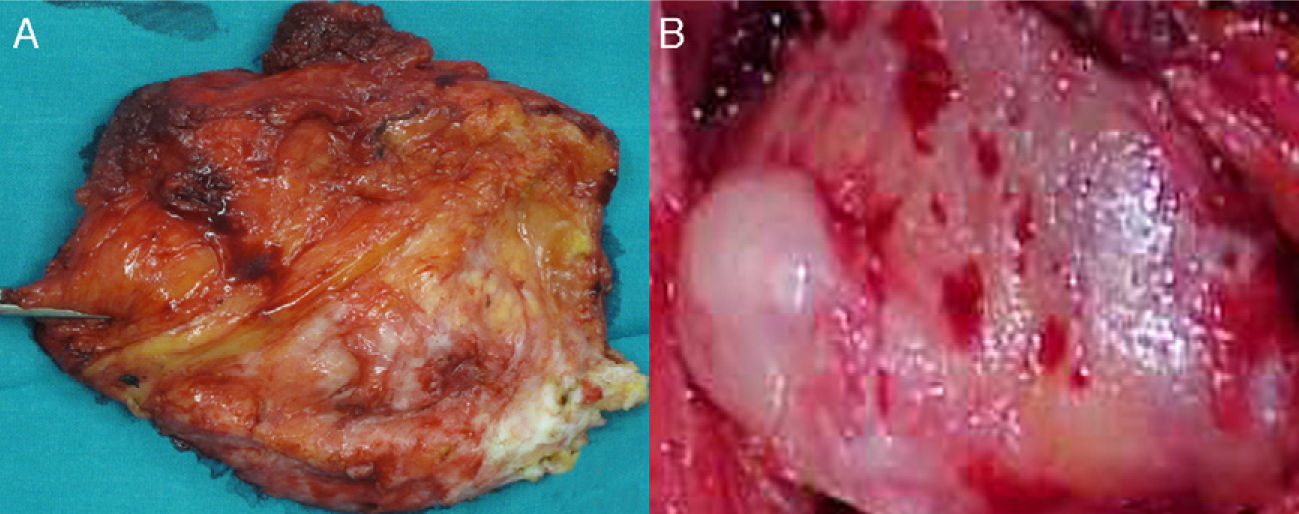
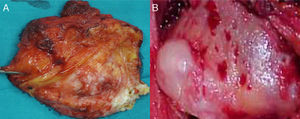
ResultsNo evidence of a family relationship was observed in group A, whilst in group B 1 patient had a family history of multiple exostosing disease. The relationship between the presence of the tumour and snapping scapula when performing physical activities with the upper limb was 21%. The symptom which led to outpatient consultation in most cases (81%) was the presence of a painful mass, followed by scapular snapping (70%; 30 out of 43 patients). The symptoms lasted for a mean period of 14±3.4 months before a diagnosis was obtained, which, in all cases and following the protocol at our centre, was performed through magnetic resonance imaging (MRI). Those cases (4 ED) which presented a more heterogeneous mass whose diagnosis through MRI was inconclusive underwent a Tru-cut® biopsy in order to rule out the possibility of a sarcoma. A total of 7 cases were treated conservatively, with the tumour remaining painless during follow-up. The remaining cases (30) required surgical removal. The anatomopathological examination of the excised specimens showed a firm, non-encapsulated tumour with poorly defined edges (Fig. 4A). Microscopically, the samples presented collagen fibres interspersed with elastic fibres from mature fat cells. In group B, surgical removal of the tumour was performed in all cases, with a period of 16 months (range: 2–36 months) between diagnosis and surgery. The anatomopathological examination of the excised lesion confirmed the diagnosis through the identification of a bone sample covered by histologically normotypical, hyaline cartilage tissue (Fig. 4B).
Operated patients who presented a mean value of 7.5 on the VAS (range: 3–9) obtained improvement to a mean value of 2.8 points (range: 0–7) after treatment (P<.005). Shoulder mobility improved by a mean value of 40±1.2 in posterior flexion (P<.005). The most common complication after surgery was the appearance of subcutaneous haematoma, which was resolved during follow-up. Patients treated conservatively went from a mean VAS score of 5 (range: 2–7) to 2.1 (range: 0–3) at the end of the follow-up period (P<.005). All patients were able to return to their usual level of physical activity prior to the onset of symptoms.
DiscussionThere are various possible causes of snapping scapula, including a single traumatic injury or repetitive motion of the scapulothoracic joint,10,11 anatomical variations of the scapula,12 scapulothoracic bursitis,13 malunion of scapular or costal fractures,14 articular imbalances due to nerve or muscle injury and tumour processes, such as osteochondroma4 or ED.5 In our work we seek to draw attention to the high number of patients who have been treated at our centre for tumours of the shoulder region and whose initial symptom was snapping scapula.
We can find many patients with snapping scapula in the field of sports traumatology, since an increase in its incidence has been reported among patients performing throws, swimming, gymnastics or weightlifting.15 In general, consultation was due to diffuse pain and snapping. It should be noted that those cases in which the cause was a soft tissue injury usually presented milder symptoms than cases where the injury affected the skeleton.13 In turn, imaging tests vary in effectiveness depending on the source of the injury. Plain radiographs are useful in identifying skeletal lesions such as osteochondroma, Luschka's tubercle (a hook-shaped prominence in the superomedial angle of the scapula), costal or scapular abnormalities.12 The efficacy of computed tomography (CT) is a frequent topic of discussion, as several studies have shown its low correlation with the symptoms.16,17 Therefore, this technique is usually reserved for skeletal or cartilaginous lesions identified by radiography. Ultrasonography has not shown a significant diagnostic efficiency. Although it is used to perform image-guided infiltrations,18 its diagnostic use is restricted to isolated cases.19 Lastly, MRI has become the main test to identify potential soft tissue masses, even allowing differentiation between scapulothoracic bursitis and ED.20,21 A Tru-cut® biopsy should be performed to confirm the suspected diagnosis when the MRI does not provide a sufficient level of confidence due to a more heterogeneous tumour. Osteochondromas can often be diagnosed by plain radiography. The problem arises when there is a soft tissue tumour, such as ED, which goes unnoticed unless this option is expressly investigated and MRI is performed.
It is essential to identify the origin of this symptom in order to treat the lesion adequately. Since the literature consists mostly of small series, we present this work which identifies a clear relationship between scapular tumours and snapping scapula. The literature focuses the initial treatment of patients suffering from snapping scapula due to mechanical causes towards conservative therapy, as this option has been shown to obtain improvement in up to 80% of cases.22–24 In turn, some studies have shown scapular snapping in up to 30% of asymptomatic patients.25 Surgical treatment achieves excellent results in cases with bone or soft tissue damage.3,5,14,26
Although the incidence of ED appears to be low (around 2%),5,27 a study on cadavers28 reported changes in the subscapular fascia similar to elastofibroma in 24% of cases aged over 55 years. The treatment of scapular snapping depends on the cause. Thus when the cause is a postural or muscular alteration, winged scapula or scapulothoracic dyskinesias we should select conservative treatment through rehabilitation.29 Other conservative measures may include infiltrations or NSAIDs.
The surgical option is recommended when conservative treatment does not improve symptoms within a period of 6 months.25 The surgical treatment of patients with constant pain in whom the symptoms are due to the presence of an underlying ED or SO tumour has reported good results.5 For those cases where bone incongruence is identified as the cause of symptoms, the literature advocates arthroscopic31 or open surgical resection of the superomedial edge of the scapula.3,30
As seems clear, the literature contains various treatments for snapping scapula, most of them associated with excellent results. This points to the importance of an adequate diagnosis of the cause, as this will condition the treatment to be employed.
The main limitation of this work resides in it being a retrospective and observational study, without a control group. On the other hand, it is based on a significant number of cases compared with the existing literature, as well as a substantial follow-up time.
Considering the data presented in this work, it would appear that we may find cases suffering pain and snapping scapula as a result of an underlying soft tissue tumour relatively frequently in our clinical practice. The optimal treatment for most of these cases will be surgery, with a thorough resection of the tumour.
ConclusionThe presence of snapping scapula appears to be strongly related to tumours in the scapulothoracic region. Therefore, we should be aware of this relationship and bear it in mind in order to provide a correct diagnosis and treatment.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that this work does not reflect any patient data.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Abat F, et al. El chasquido escapular como síntoma de un tumor de la región escapulotorácica. Rev Esp Cir Ortop Traumatol. 2013;57:123-8.