Dual modularity stems were introduced with the theoretical advantage of restoring hip anatomy more precisely through femoral offset and limb length adjustment. Interchangeable necks allow for intraoperative angulation, anteversion and length changes. Our objective is to study whether a better femoral offset correction is achieved with the H MAX-M® prosthesis (Limacorporate, San Daniele, Italy) compared to its monoblock counterpart.
Material and methodsA prospective cohort study was conducted by means of consecutive sampling on adult patients undergoing total hip arthroplasty with the diagnosis of coxarthrosis between January 2011 and December 2015. This cohort has two arms, one arm included patients who underwent modular neck arthroplasty and the other included patients who underwent monoblock total hip arthroplasty. Radiographic offset measurement of the operated hip and the contralateral hip was performed, and the difference between both values was calculated. The mean of the measurements obtained for each arm of the cohort were compared with each other.
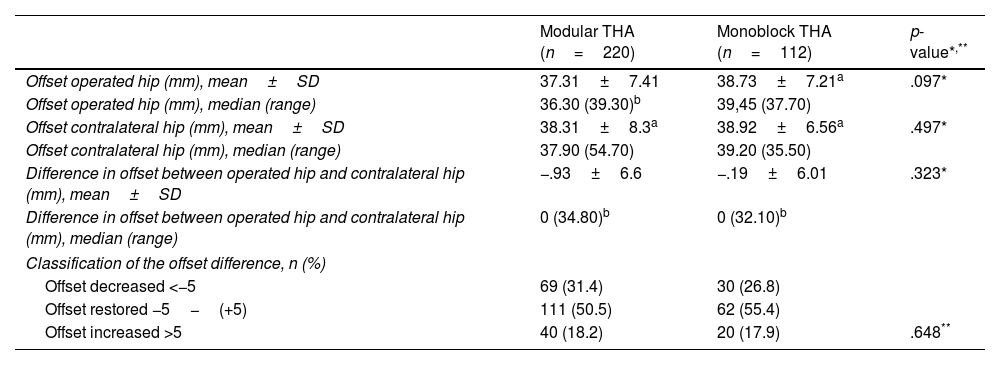
ResultsNo statistically significant differences were observed in the difference in offset between the operated hip and the contralateral hip (p=.323). No statistically significant differences were observed in the correction of the femoral offset, determined as the difference between the operated hip and the contralateral hip (p=.323). Nor were differences observed in the postoperative offset values (p=.097). It should be noted that for both designs, the majority group is the one with restored offset (p=.001).
Los vástagos con doble modularidad fueron introducidos con la ventaja teórica de restaurar de forma más precisa la anatomía de la cadera a través del ajuste del offset femoral y la longitud de los miembros. Los cuellos intercambiables permiten cambios intraoperatorios de angulación, anteversión y longitud. Nuestro objetivo es estudiar si se consigue una mejor corrección del offset femoral con la prótesis H MAX-M® (Limacorporate, San Daniele, Italia) frente a su homólogo monobloque.
Material y métodosSe realizó un estudio de cohortes prospectivo mediante muestreo consecutivo sobre pacientes intervenidos de artroplastia total de cadera con el diagnóstico de coxartrosis desde enero de 2011 hasta diciembre de 2015. Esta cohorte posee 2 brazos: un brazo incluyó a los pacientes intervenidos mediante vástago con cuello modular y el otro a los pacientes intervenidos mediante vástago monobloque. Se realizó la medición radiográfica del offset de la cadera intervenida, la cadera contralateral y se calculó la diferencia entre ambos valores. Las medias de las mediciones obtenidas para cada brazo de la cohorte se compararon entre sí.
ResultadosNo se han observado diferencias estadísticamente significativas en la corrección del offset femoral entre el grupo modular y el monobloque, determinado como la diferencia de offset entre la cadera operada y la cadera contralateral (p=0,323). Tampoco se observaron diferencias en los valores de offset postoperatorio (p=0,097). Cabe decir que tanto para la prótesis modular como para la prótesis monobloque el grupo mayoritario es aquel con offset restaurado (p=0,001).
Total hip arthroplasty is one of the most successful surgical procedures in orthopaedic surgery. Continuous modifications to prosthetic designs and biomaterials over the years have become the primary strategy of surgeons and engineers to improve clinical–functional outcomes by reproducing the native biomechanics of the hip.
Sir J. Charnley was the first to recognise the importance of restoring femoral offset and its impact on abductor moment and soft tissue balancing.1 A decrease in femoral offset medialises the insertion point of the abductor musculature and decreases the abductor lever arm,2 which increases the energy required for normal gait. This situation can lead to Trendelenburg gait and the need for walking aids,3 as well as reduced range of motion1 and increased risk of femoropelvic impingement.3 Decreased abductor moment also increases the resultant force on the hip joint,1 which has been associated with increased polyethylene wear4 and ultimately osteolysis and reduced implant survival.5 In contrast, increased femoral offset increases the abductor lever arm, i.e., stress on the abductor musculature,2 reducing the energy required for normal gait.1 In a clinical context, this situation results in less Trendelenburg gait, less lameness, less fatigue, and less dependence on aids, compared to a decreased offset situation.1 It also improves range of motion free of impingement.3 This increased lever arm minimises the resulting reactive force at the hip joint,1 which means less wear on the surfaces involved in the friction torque.4,6 However, it increases stress in other areas such as the fixation interface7 and the medial cortex, which could trigger early implant failure.8 Therefore, the orthopaedic surgeon should aim for anatomical restoration of the femoral offset to avoid complications from misalignment of the anatomical restoration.
In 1962, Weber developed the first design that included the concept of modularity through a head-neck socket.9 Later, in 1985, Cremascoli designed the first stem with a double socket, head-neck and neck-stem, thus introducing the concept of dual modularity to provide surgeons with a more versatile system.10 Dual modularity has the theoretical advantage of restoring the hip anatomy more accurately through more accurate adjustment of the hip centre of rotation and allowing intraoperative changes in angulation, anteversion, and neck length.10 However, more recent publications have implicated modular interfaces in the release of metal ions with potentially deleterious systemic effects on patient health. Successive series have shown that the addition of trunnions implies increased susceptibility to corrosion due to micromovement at the interfaces.11 However, in any analysis we must bear in mind that not all designs and materials are the same12 and a clear distinction should be made between them.
There are now stems with modular necks on the market that have been used with satisfactory functional results and low complication and revision rates. Our hospital has extensive experience in the use of modular prostheses, implanting the first in the 1990s. The model was changed in 2008, improving the geometry and the design of the metaphyseal anchor. Up to the date that this study was completed, this prosthetic model has been implanted as standard practice in our service, and therefore we considered assessing the benefits associated with its use. Due to the increase in literature references on the risks of using these prosthetic models, our objective was to study whether better anatomical correction of the femoral offset is really achieved with the use of the H MAX-M® prosthesis (Limacorporate, San Daniele, Italy) compared to its monoblock counterpart.
Material and methodsThis is a prospective cohort study involving patients undergoing surgery with a particular stem design. The patients were followed up for a period to check for occurrence of the event of interest, which in this case is impaired offset after surgery in the operated hip. The patients were followed up for 5 years, and the study ended in 2020.
GANMO software version 7.12 was used to calculate the sample size. This was based on preliminary results from 2010 which showed how the femoral offset difference between the two hips varied with a mean of −.72, and a common standard deviation of 6.6mm. Assuming this standard deviation, and accepting an alpha risk of .05 and a beta risk of .20, the minimum required sample size would be 114 patients in the modular group (observation group) and 57 in the monoblock group (reference or stable group). The effect size we aimed to find was differences greater than 5mm.13
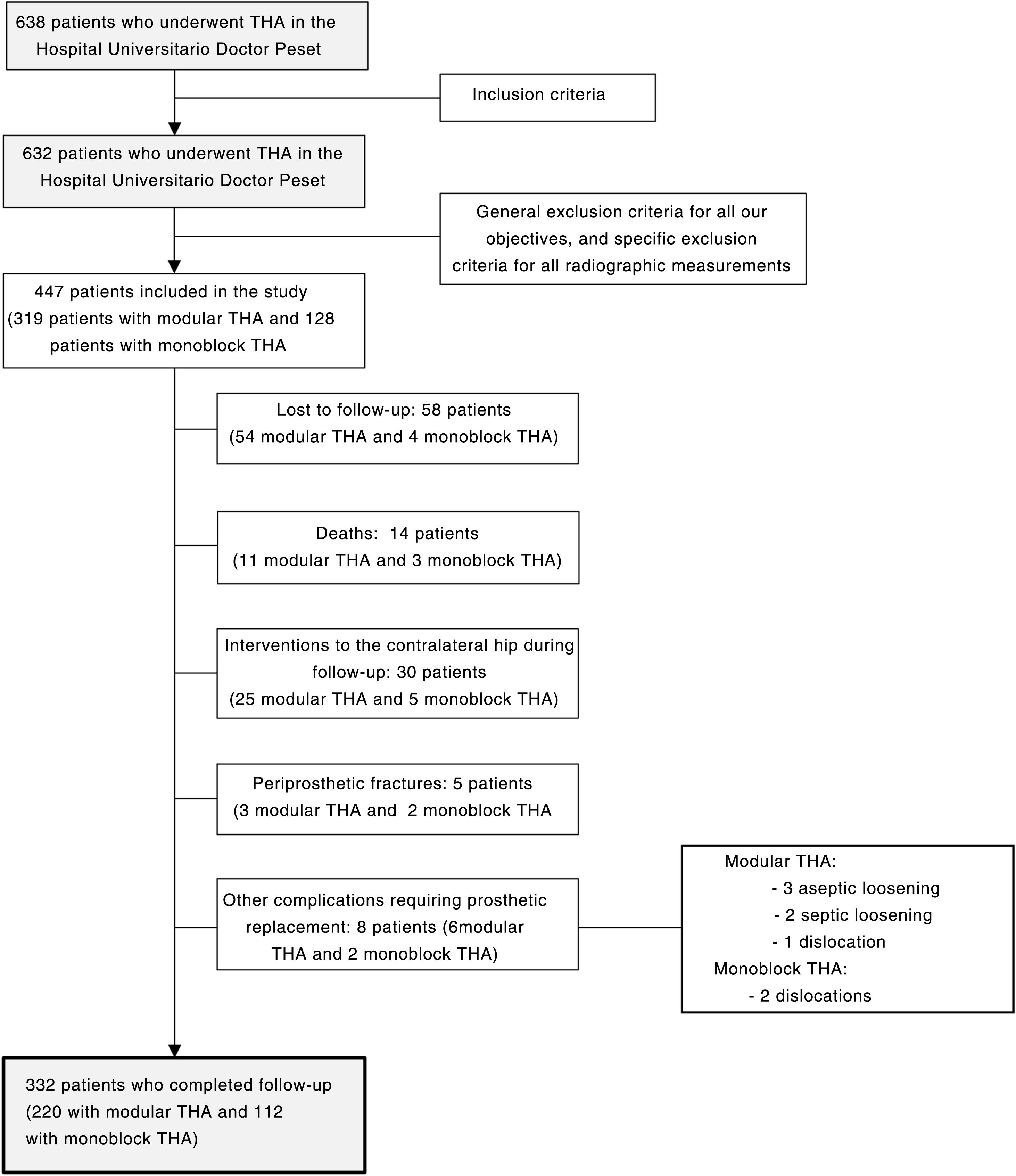
We performed consecutive sampling of adult patients who underwent total hip arthroplasty with a diagnosis of coxarthrosis (primary or secondary to avascular necrosis, Perthes disease, hip dysplasia and epiphysiolysis) conducted in our centre from January 2011 to December 2015. This cohort had 2 arms, one arm included patients operated with cementless stem with modular neck and the other included patients operated with monoblock stem. The exclusion criteria were any other diagnosis of coxofemoral disease, arthroplasty in the contralateral hip prior to inclusion in the study, and advanced coxarthrosis (Tönnis grade III) in the contralateral hip that made it impossible to measure native femoral offset. Fig. 1 shows the flow chart of the patient section for the study. We have a long history of using modular primary stems in our centre, both the modular stem and the homologous monoblock stem. It should be noted that the inclusion of patients in each arm of the cohort depended on preoperative planning, intraoperative measurements, and surgeon preference.
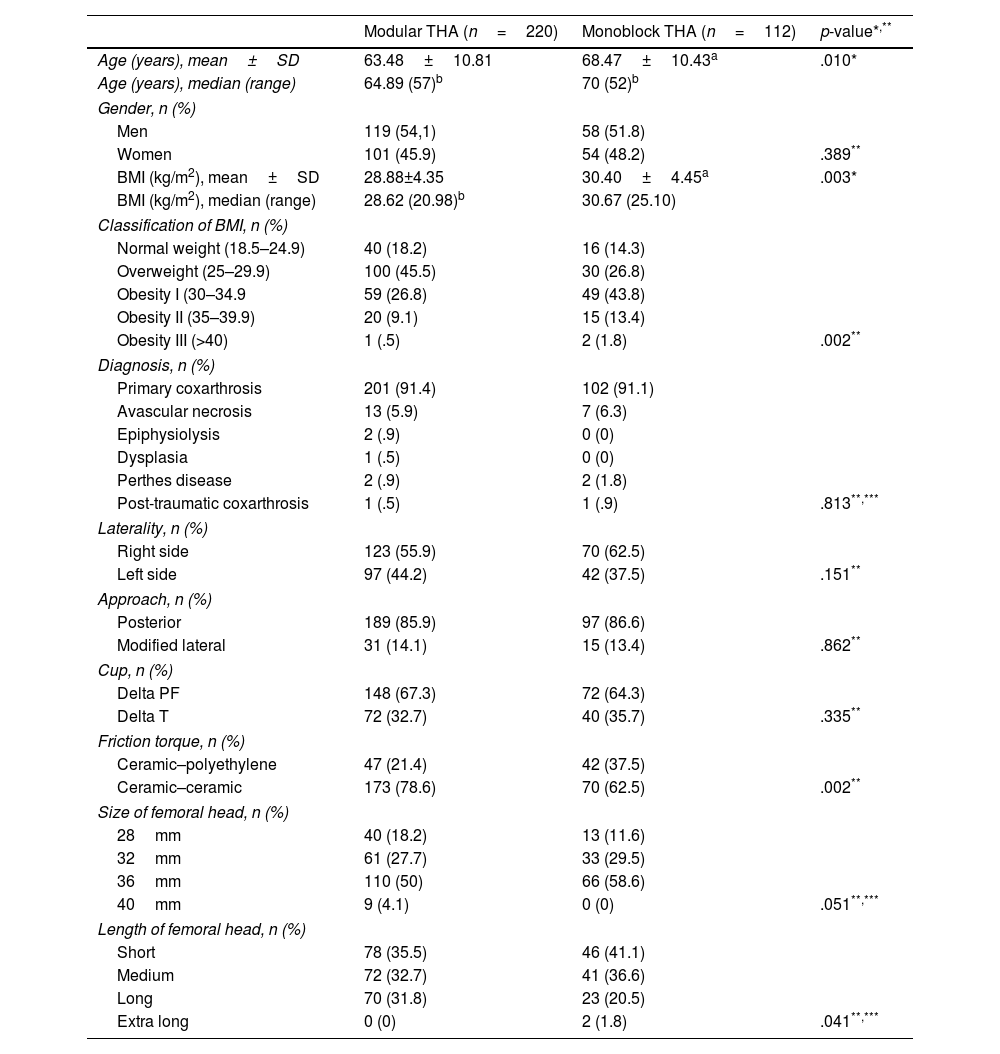
Table 1 shows the baseline characteristics of both arms of the cohort; the population operated with modular stem were younger (p=.010) and had a lower body mass index (p=.003).
Baseline characteristics of the patients who completed follow-up.
| Modular THA (n=220) | Monoblock THA (n=112) | p-value*,** | |
|---|---|---|---|
| Age (years), mean±SD | 63.48±10.81 | 68.47±10.43a | .010* |
| Age (years), median (range) | 64.89 (57)b | 70 (52)b | |
| Gender, n (%) | |||
| Men | 119 (54,1) | 58 (51.8) | |
| Women | 101 (45.9) | 54 (48.2) | .389** |
| BMI (kg/m2), mean±SD | 28.88±4.35 | 30.40±4.45a | .003* |
| BMI (kg/m2), median (range) | 28.62 (20.98)b | 30.67 (25.10) | |
| Classification of BMI, n (%) | |||
| Normal weight (18.5–24.9) | 40 (18.2) | 16 (14.3) | |
| Overweight (25–29.9) | 100 (45.5) | 30 (26.8) | |
| Obesity I (30–34.9 | 59 (26.8) | 49 (43.8) | |
| Obesity II (35–39.9) | 20 (9.1) | 15 (13.4) | |
| Obesity III (>40) | 1 (.5) | 2 (1.8) | .002** |
| Diagnosis, n (%) | |||
| Primary coxarthrosis | 201 (91.4) | 102 (91.1) | |
| Avascular necrosis | 13 (5.9) | 7 (6.3) | |
| Epiphysiolysis | 2 (.9) | 0 (0) | |
| Dysplasia | 1 (.5) | 0 (0) | |
| Perthes disease | 2 (.9) | 2 (1.8) | |
| Post-traumatic coxarthrosis | 1 (.5) | 1 (.9) | .813**,*** |
| Laterality, n (%) | |||
| Right side | 123 (55.9) | 70 (62.5) | |
| Left side | 97 (44.2) | 42 (37.5) | .151** |
| Approach, n (%) | |||
| Posterior | 189 (85.9) | 97 (86.6) | |
| Modified lateral | 31 (14.1) | 15 (13.4) | .862** |
| Cup, n (%) | |||
| Delta PF | 148 (67.3) | 72 (64.3) | |
| Delta T | 72 (32.7) | 40 (35.7) | .335** |
| Friction torque, n (%) | |||
| Ceramic–polyethylene | 47 (21.4) | 42 (37.5) | |
| Ceramic–ceramic | 173 (78.6) | 70 (62.5) | .002** |
| Size of femoral head, n (%) | |||
| 28mm | 40 (18.2) | 13 (11.6) | |
| 32mm | 61 (27.7) | 33 (29.5) | |
| 36mm | 110 (50) | 66 (58.6) | |
| 40mm | 9 (4.1) | 0 (0) | .051**,*** |
| Length of femoral head, n (%) | |||
| Short | 78 (35.5) | 46 (41.1) | |
| Medium | 72 (32.7) | 41 (36.6) | |
| Long | 70 (31.8) | 23 (20.5) | |
| Extra long | 0 (0) | 2 (1.8) | .041**,*** |
BMI: body mass index, SD: standard deviation, THA: total hip arthroplasty.
The investigators adhere to the Oviedo and Helsinki declarations on biomedical research. Our institution's Ethics Committee gave its approval to conduct this study: CEIC code 110/17. The patients included in the study gave their written consent to participate in the study and for the surgical intervention provided by the Spanish Society of Orthopaedic Surgery and Trauma.
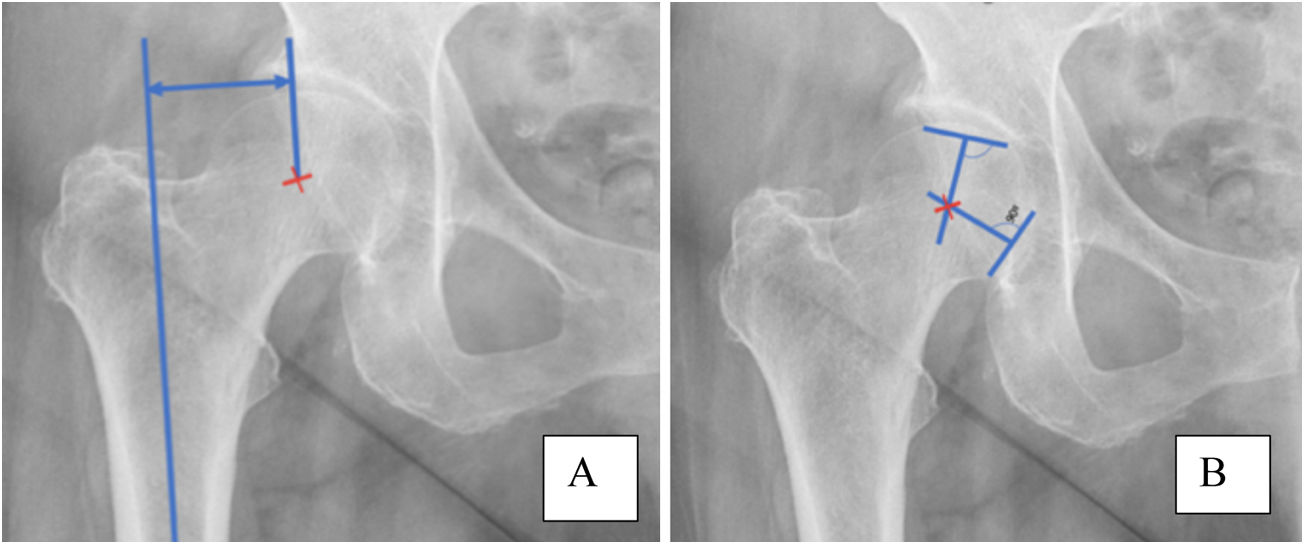
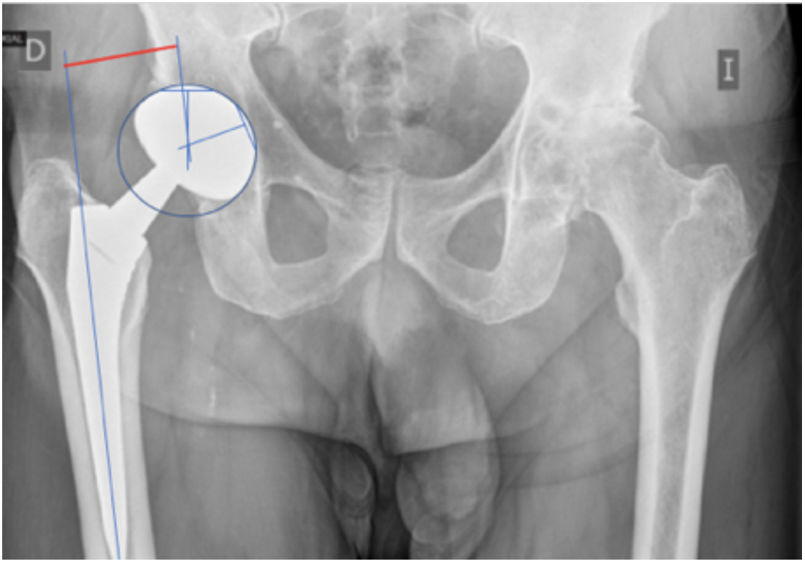
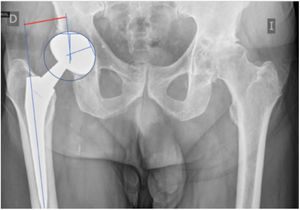
Measurement techniqueAll radiographs were performed on the DR400 system (AGFA HealthCare®). Immediately postoperatively, the femoral offset was measured in both the operated hip and the contralateral hip by an anteroposterior radiograph of the pelvis centred on the pubic symphysis with both legs at 15° of internal rotation held using a foot drop brace with an external wedge. The measurement of femoral offset used was that proposed by Steinberg and Harris and calculated as the perpendicular distance between the centre of the femoral head and the anatomical axis of the femur (Fig. 1).1 When calculating the offset difference between the operated hip and the contralateral hip, a positive value indicates greater length in the operated hip, and a negative value indicates the opposite. Using this parameter, we assess whether the femoral offset is restored when the patient is operated with a certain stem design, as we obtain it by subtracting the postoperative value from the native value. We then analyse whether the figure obtained is within a previously established range.
To determine the centre of the circumference, we draw 2 chords not parallel to each other and which are not diameters of the circumference. From these chords we draw their perpendicular bisectors, which correspond to the straight line perpendicular to the segment drawn through its midpoint. The perpendicular bisector of these 2 chords intersects at the centre of the circumference (Fig. 2). For the operated hip, this measurement was established between the centre of rotation and the longitudinal axis of the stem (Fig. 3).
The surgical procedure was performed by the same team of 4 surgeons. All surgeries were performed under spinal anaesthesia. The posterior or anterolateral approach was used. Antibiotic prophylaxis consisted of 2g intravenous cefazolin and 240mg gentamicin before anaesthetic induction, followed by postoperative treatment with 1g intravenous cefazolin every 8h for the first 24h. In case of beta-lactam allergy, cefazolin was replaced by clindamycin 600mg, maintaining the same regimen. Six hours after the surgery, the patients were given low molecular weight bemiparin at a prophylactic dose for 30 days as prophylactic treatment for thromboembolic events.
ImplantsTwo designs of acetabular component made from titanium alloy (Ti6A14V) were used, but with different coatings, one porous titanium coated with hydroxyapatite (Delta PF) and the other trabecular titanium (Delta TT). The femoral head was ceramic in all cases and the insert used was either ceramic or polyethylene. The H-MAX M® modular stem and the H-MAX S® monoblock stem (Limacorporate, San Daniele, Italy), made of titanium alloy with high corrosion resistance (Ti6A14V) and with a 55μm hydroxyapatite coating, were used as the femoral component. Table 1 gives the descriptive data on the implants used. The interchangeable necks used in the modular implants are made from a cobalt-chromium-molybdenum alloy and have a 12/14 taper, with a double radius cross-section and 2 lateral grooves or channels. They are available in 2 lengths: short or long. They also have 2 options of neck-diaphysis angulation, either standard (134°) or lateralised (131°). These 2 angulations have 3 different versions: anteverted (+10°), neutral (0°), or retroverted (−10°). The appropriate neck was selected based on preoperative planning, intraoperative stability, soft tissue tension, and leg length.
Statistical analysisA descriptive analysis was performed of the femoral offset values in the operated hip and the healthy hip, and the difference between the two values and the immediate postoperative radiographic offset corrections in patients with modular THA and with monoblock THA were compared in the immediate postoperative period. The test used depended on the normality of the distribution, i.e., if the distribution was normal a Student's t-test was used and if the distribution was non-normal the Mann–Whitney U-test. We then classified these corrections into 3 groups by creating a categorical variable based on the magnitude of the femoral offset difference.13 In the case of offset, we established a group with a value less than an undercorrection of 5mm (decreased offset), another group with a value 5mm lower or higher than the contralateral value (restored offset), and a third group with a value greater than a hypercorrection of 5mm (increased offset). This limit was established following the recommendations found in the literature published to date.13 Homogeneity comparisons were performed using the Chi-square test at 95% confidence or Fisher's exact test, as appropriate.
ResultsTable 2 shows the femoral offset data for the operated hip, the contralateral hip, and the offset difference between both hips of the patients who completed follow-up. No statistically significant differences were found in any of the 3 parameters (p=.097, p=.497, and p=.323, respectively) between the two groups. There were also no statistically significant differences in the frequency with which patients were distributed according to femoral offset (undercorrected, restored or overcorrected offset) between the modular and monoblock groups (p=.648). It should be noted that in both stem designs, the restored offset group had the majority (p=.001). On the other hand, in the modular group we can observe how the offset was decreased more frequently than increased (p=.001), while in the monoblock group there is no difference in the frequency with which an increased offset or a decreased offset was achieved (p=.108).
Femoral offset in patients who completed follow-up.
| Modular THA (n=220) | Monoblock THA (n=112) | p-value*,** | |
|---|---|---|---|
| Offset operated hip (mm), mean±SD | 37.31±7.41 | 38.73±7.21a | .097* |
| Offset operated hip (mm), median (range) | 36.30 (39.30)b | 39,45 (37.70) | |
| Offset contralateral hip (mm), mean±SD | 38.31±8.3a | 38.92±6.56a | .497* |
| Offset contralateral hip (mm), median (range) | 37.90 (54.70) | 39.20 (35.50) | |
| Difference in offset between operated hip and contralateral hip (mm), mean±SD | −.93±6.6 | −.19±6.01 | .323* |
| Difference in offset between operated hip and contralateral hip (mm), median (range) | 0 (34.80)b | 0 (32.10)b | |
| Classification of the offset difference, n (%) | |||
| Offset decreased <−5 | 69 (31.4) | 30 (26.8) | |
| Offset restored −5−(+5) | 111 (50.5) | 62 (55.4) | |
| Offset increased >5 | 40 (18.2) | 20 (17.9) | .648** |
SD: standard deviation; THA: total hip arthroplasty.
Restoring hip biomechanics remains a challenge for the orthopaedic surgeon. Modularity seeks an accurate match to the native anatomy of the hip. This versatility of implants may justify the use of modular necks in younger patients. Furthermore, the first generation of interchangeable necks were made of titanium and presented complications due to breakage of the necks secondary to decreased fatigue strength and bending forces.14 They were later replaced by a chromium-cobalt alloy with a lower breakage rate. This resulted in the recommendation to use modularity in patients with low BMI, which would explain the difference found between the two groups in our study.
Sir J. Charnley based his philosophy on the concept of femoral offset.1,2 In routine clinical practice the measurement is made based on routine anteroposterior radiographs of the pelvis which have not been specifically prepared for femoral offset analysis. Knowing that the measurement is influenced by the angle between the neck and the diaphysis, the degrees of hip rotation and the asymmetry with the contralateral side,5,10,15 Pasquier et al.16 claim that these pelvis radiographs are associated with an underestimation of the true amount of femoral offset. In our study, to improve the reproducibility of the measurement and reduce the possibility of error with the anteroposterior pelvis radiograph, we set strict common criteria beforehand for all imaging tests (anteroposterior pelvis radiograph centred on the pubic symphysis with both legs at 15° internal rotation achieved by holding the leg with a foot drop brace with external wedge). We also calibrated these radiographs based on the known implanted stem measurement. This increases the reliability and comparability of the measurements taken. Therefore, the calibrated anteroposterior pelvic radiograph combined with currently available image processing tools is the most used method in routine clinical practice, and its reproducibility, validity, and reliability are well documented.17
In this study we used the femoral offset measurement technique proposed by Steinberg and Harris.1 This is the method most used in the literature, and therefore we were able to compare it with the results published to date. According to Mahmood et al.,18 this technique has good interobserver reliability and intraobserver reproducibility. Authors such as Bonnin et al.19 state that the drawback of this measurement is that it is clearly influenced by femoral rotation, and therefore patient positioning was essential to avoid any measurement error. In the case of the operated hip, this measurement was established between the centre of rotation and the longitudinal axis of the stem. Therefore, we must bear in mind when replacing the joint that the femoral offset is influenced by implant design, head size, neck length, implant size, and stem position within the femoral canal.13,20
Many authors use the contralateral hip in calculating the native offset in preoperative planning, and in the comparative analysis of the postoperative outcome.1,13,21–23 We used this approach in our study because many preoperative radiographs lacked the rigour to measure the same hip preoperatively and compare it with the postoperative measurement; in other words, the preoperative measurement could have introduced a bias, and therefore the comparison was made with the measurement on the contralateral hip. Surgeons should be aware that this could be considered a confounding factor due to the high likelihood of osteoarthritis on the opposite side, and therefore, to minimise this error, we have included only those patients with a contralateral Tönnis grade I or II of osteoarthritis. Furthermore, authors such as Liebs et al.24 state that the femoral offset of both hips is not always the same, with differences of up to 4.6mm having been detected in the literature, therefore using the contralateral hip could constitute an error.
The limit value above which changes in femoral offset produce a negative effect on patient function remains controversial.25 If we review the literature, the range used to consider that femoral offset has been restored is between 5mm lower and 5mm higher than the native value. It has been considered that a femoral offset restoration within this range allows the biomechanical properties of the postoperative hip to be reproduced.1,13,21
As mentioned earlier, in 1985 Cremascoli introduced modular or interchangeable necks with the theoretical advantage of allowing more precise reconstruction of the geometry and providing the surgeon with a more versatile system.10 In our analysis we found no statistically significant difference in the postoperative offset value obtained between the modular and monoblock groups (p=.097). In the modular group the mean offset of the operated hip was 37.31±7.41mm. We found no studies using the implanted prosthetic model in our work. Sakai et al.26 used the ANCA Fit modular system and obtained a postoperative offset of 31.2±5.4mm measured in the Scout CT projection, which is significantly lower than our result (p=.001).
In our study, no statistically significant differences were observed in the offset difference between the operated hip and the contralateral hip between the two groups (p=.323), i.e., no differences were found in restoration of the anatomy when comparing both stem designs. Neither did we find statistically significant differences in the frequency with which offset restoration is achieved between monoblock THAs and THAs with modular neck (p=.648), the majority group being those with restored offset in both models. Along the same lines, if we review the literature, Carothers et al.27 conducted a laboratory study and in 44% of patients they observed no differences in the restoration of the centre of rotation of the head in those operated using the modular M/L Taper Kinectiv stem (Zimmer, Warsaw, IN, United States) compared to the value obtained with its monoblock counterpart, and in those in which a difference was observed, it was between 1 and 2mm. In contrast to our findings, other authors do find statistically significant differences in anatomical restoration. According to Duwelius et al.,28 there is a smaller difference between the operated and native offset in patients operated with modular M/L Taper Kinectiv CTA (Zimmer, Warsaw, IN, USA) compared to monoblock THA. According to Archibeck et al.,29 the use of modular M/L Taper Kinectiv stems (Zimmer, Warsaw, IN, USA) restores the femoral offset more frequently than monoblock stems, although they used a difference of 1mm as the restoration limit, which we could consider unrealistic within the postoperative objectives and, therefore, the difference found may not really be relevant. Gerhardt et al.30 reached the same conclusion after using the Profemur Z stem (Wright Medical Technology, Arlington, Tennessee, United States), and observed greater offset restoration in the modular group compared to the monoblock group (p=.48), the latter showing a higher frequency of increased offset. Even so, the author warns that this is borderline significance, and the sample size should be larger. These 3 authors use anteroposterior pelvis radiography for their analysis.
The results obtained and the long series available have aroused our interest in studying other aspects related to the use of modular stems. One such issue is the dysmetria that may result from adjusting offset and soft tissue tension to achieve prosthetic stability; however, this cohort showed no difference in postoperative dysmetria between the two designs. Therefore, a thorough surgical technique that covers both the resected bone and soft tissue tension was vital to obtain comparable results between the two prosthetic designs. We shall expand upon these data in a subsequent study. Furthermore, these results have laid the groundwork for analysis of the potential risks associated with the use of modularity due to the release of metal debris.
It is important to bear in mind that many of the characteristics of implants are specific to their design; therefore, it is obvious that not all designs and materials are the same, and a clear distinction should be made between them. Even so, although the results should not be extrapolated to all implants, there are no studies that analyse all commercially available implants, and we should always consider the medical literature for ongoing evaluation of our clinical practice.
The limitations of the study are that we based our study on the anteroposterior pelvis X-ray, which is a 2-dimensional image, rather than other more precise techniques such as CT scanning. In addition, positioning the patient during radiography is a parameter that is highly dependent on the radiology technician. Finally, in our study we relied on the measurement of the contralateral hip as a measure of native offset and dysmetria, which could act as a confounding factor.
ConclusionsRadiographically, we observed no differences in our objective of reconstructing the geometry and biomechanics of the hip between modular stems and monoblock stems by adjusting the femoral offset. In our study, neither design is superior to the other in this respect. In fact, monoblock stems, with their choice of cervico-diaphyseal angle and stem size, have proven a successful design thus far. Modularity, on the other hand, aims to avoid any lack of precision thanks to its interchangeable parts, allowing intraoperative adjustment of anatomical parameters. This versatility could be of great interest and help to the surgeon. Therefore, the information provided in this paper flags up the need for more in-depth analysis of the theoretical advantages of using modularity in primary hip surgery, as well as the risks derived from it.
Level of evidenceLevel of evidence II.
FundingThere is no funding source in our research.
Conflict of interestsThe authors have no conflict of interests to declare.