Dual modularity stems seek to more precisely restore anatomy by allowing intraoperative adjustments thanks to modular necks. Our aim is to compare the radiographic length correction with the H MAX-M® Stem versus its monoblock counterpart H MAX-S®.
Material and methodsA prospective cohort study was carried out through consecutive sampling on patients who underwent primary total hip arthroplasty with coxarthrosis diagnosis between 2011 and 2015. One arm of the cohort included patients who were operated with a modular stem and the other with a monobloc stem. Length was measured on the anteroposterior pelvic-bearing radiograph at 6 months. The mean of the measurements obtained for each arm of the cohort were compared with each other.
ResultsNo statistically significant differences were observed in the correction of asymmetry between both groups, determined as the difference in length between the operated hip and the contralateral hip (p=.106). Nor were differences observed in postoperative length values (p=.053). It should be noted that for both the modular stem and the monobloc stem, the majority group is the one with restored length (84.1% and 80.4%, respectively; p=.001).
ConclusionDespite the theoretical advantage of modularity and that having interchangeable parts could be of great interest, in our study, we have not been able to demonstrate a superiority of modular designs compared to monoblock for control of postoperative leg length discrepancy.
Los vástagos con doble modularidad buscan restaurar de forma más precisa la anatomía al permitir ajustes intraoperatorios gracias a los cuellos modulares. Nuestro objetivo es comparar la corrección radiográfica de la longitud con el vástago H MAX-M® frente a su homólogo monobloque H MAX-S®.
Material y métodosSe realizó un estudio de cohortes prospectivo mediante muestreo consecutivo sobre pacientes intervenidos de artroplastia total de cadera primaria con el diagnóstico de coxartrosis entre el año 2011 y 2015. Un brazo de la cohorte incluyó a los pacientes intervenidos con vástago modular y el otro con vástago monobloque. Se midió la longitud en la radiografía anteroposterior de pelvis en carga a los 6 meses. Las medias de las mediciones obtenidas para cada brazo de la cohorte se compararon entre sí.
ResultadosNo se han observado diferencias estadísticamente significativas en la corrección de la disimetría entre ambos grupos determinada como la diferencia de longitud entre la cadera operada y la cadera contralateral (p=0,106). Tampoco se observaron diferencias en los valores postoperatorios de longitud (p=0,053). Cabe decir que tanto para el vástago modular como para el vástago monobloque el grupo mayoritario es aquel con longitud restaurada (84,1 y 80,4%, respectivamente; p=0,001).
ConclusiónA pesar de la ventaja teórica de la modularidad y de disponer de piezas intercambiables podría ser de gran interés, en nuestro estudio no hemos podido demostrar que exista una superioridad de los diseños modulares frente al monoblock para control de la disimetría postoperatoria.
Total hip arthroplasty (THA) is one of the most successful surgical procedures in orthopaedic surgery. Orthopaedics has followed a path based on continuous modifications and improvements in design and materials that seek to improve clinical-functional outcomes and achieve maximum implant longevity by replicating the native anatomy and biomechanics of the hip.
Achieving symmetric limb length after THA remains a surgical challenge in orthopaedics today. Postoperative dissymmetry has an incidence ranging from 1% to 27% after THA.1 In fact, dissymmetry is a severe complication, as differences greater than 10mm induce functional disturbances secondary to low back pain,2 neurological sequelae,3 gait disturbances,4 decreased range of motion and implant instability.5 Intraoperatively, this is a parameter that is difficult to determine.
In 1985, Cremascoli designed the first stem with double socket, head-neck and neck-stem, thus introducing the concept of bimodularity. Double modularity has the theoretical advantage of allowing intraoperative changes of angulation, anteversion and neck length6 with the intention of achieving the most faithful possible reproduction of the native anatomy. This system is based on the idea of providing surgeons with a more versatile system6 that allows them to reproduce the original hip parameters in order to ultimately achieve the greatest longevity of the implant. However, more recent publications have implicated modular interfaces in the release of metal ions with potentially deleterious systemic effects on patient health.7–9
Even so, in any analysis we must bear in mind that not all designs and materials are the same,10 so the results are not generalisable, and a clear distinction must be made between them.
Our hospital has extensive experience in the use of modular prostheses, implanting the first modular prosthesis in the 1990s. In 2008, the model was changed to a double radius socket which, according to in vitro studies, allowed greater control of corrosive phenomena.11 The prosthetic model analysed in this study has been implemented as standard practice in our department up to the date of completion of this study, and we therefore set out to assess the benefits associated with its use. We set out to compare postoperative radiographic correction of limb length with the use of the modular H MAX-M® stem (Limacorporate, San Daniele, Italy) versus its monoblock counterpart H MAX-S® (Limacorporate, San Daniele, Italy).
Material and methodsThis is a prospective cohort study involving patients undergoing surgery with a particular stem model available in modular and monoblock design. Patients were followed for 5years; the study started in 2011 and ended in 2020.
The sample size calculation was performed with GANMO software version 7.12. This was based on preliminary results from 2010 which showed how the length difference between the two hips varied with mean 2.70 and a common standard deviation of 5.8mm. Assuming this standard deviation and accepting an alpha risk of .05 and a beta risk of .20, the minimum sample size required would be 89 patients in the modular group (observation group) and 44 in the monoblock group (reference or stable group). The minimum difference to be detected was 3mm, with differences of more than 10mm12 being considered clinically relevant.
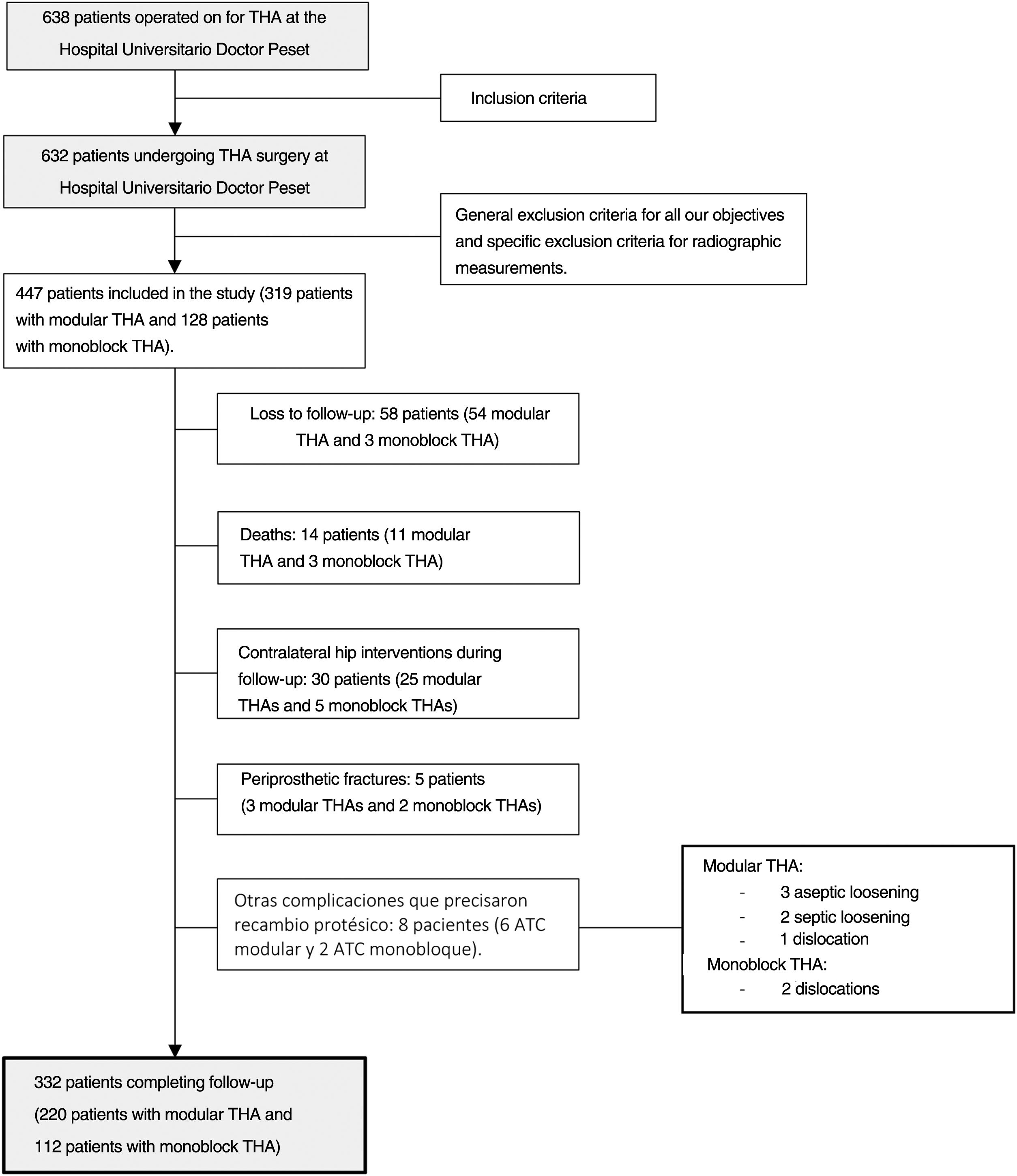
We conducted a consecutive sampling of adult THA patients with a diagnosis of coxarthrosis (primary or secondary to avascular necrosis, Perthes disease, hip dysplasia and epiphysiolysis) performed at our centre from January 2011 to December 2015. This cohort had two groups; one included patient who underwent cementless stem replacement with modular collar and the other included patients who underwent cementless stem replacement with monoblock. The exclusion criteria were any other diagnosis of coxofemoral pathology, carriers of arthroplasty in the contralateral hip prior to inclusion in the study and impossibility of performing anteroposterior pelvis radiography under load. Fig. 1 shows the flow chart of the patient section for the study. A total of 332 patients (220 patients with modular THA and 112 patients with monoblock THA) completed the study. Our centre has a long history in the use of modular primary stems. Both the modular stem and the homologous monoblock stem are available simultaneously. It should be noted that the inclusion of patients in each group of the cohort depended on preoperative planning, intraoperative manoeuvres to check implant stability, soft tissue tension and limb length, as well as surgeon preference.
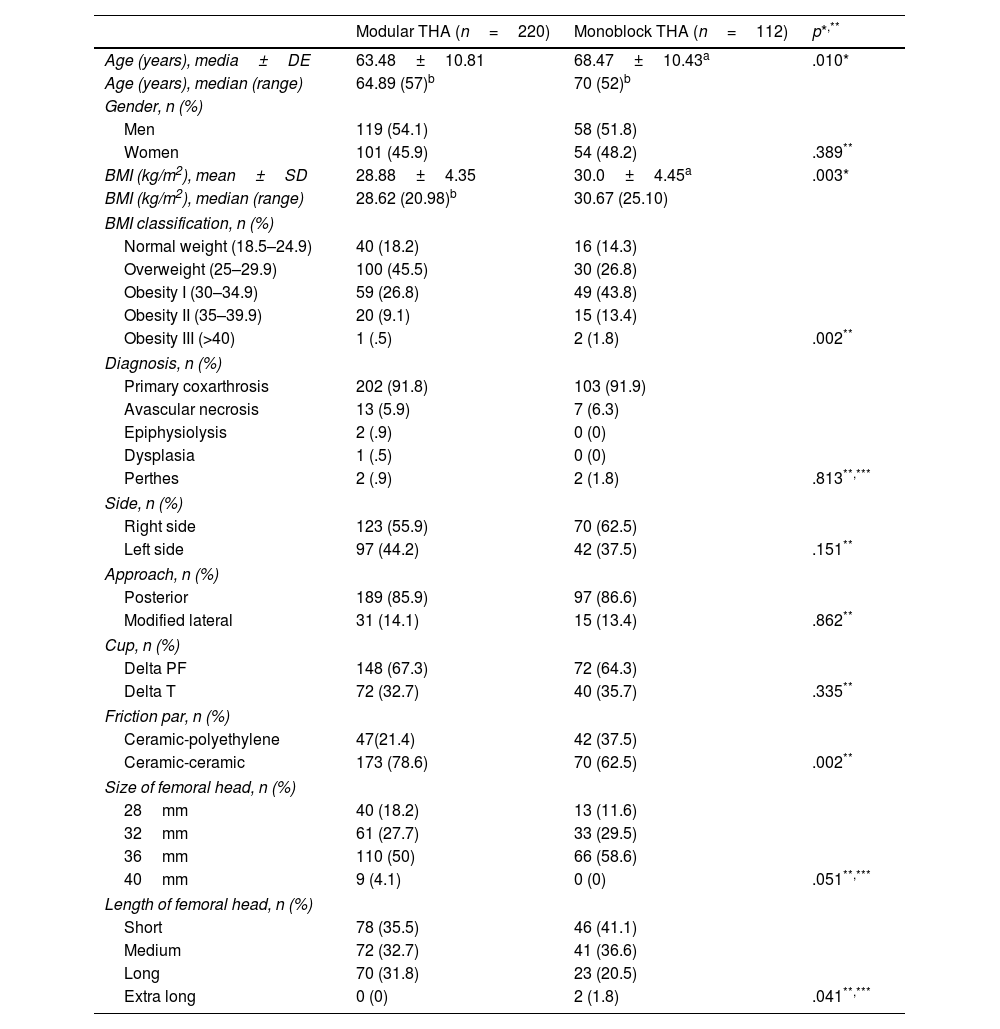
The baseline characteristics of the patients in both cohort groups arms are shown in Table 1, with the population treated with modular stem being younger (p=.010) and with lower body mass index (BMI) (p=.003).
Baseline characteristics of patients who finish follow-up.
| Modular THA (n=220) | Monoblock THA (n=112) | p*,** | |
|---|---|---|---|
| Age (years), media±DE | 63.48±10.81 | 68.47±10.43a | .010* |
| Age (years), median (range) | 64.89 (57)b | 70 (52)b | |
| Gender, n (%) | |||
| Men | 119 (54.1) | 58 (51.8) | |
| Women | 101 (45.9) | 54 (48.2) | .389** |
| BMI (kg/m2), mean±SD | 28.88±4.35 | 30.0±4.45a | .003* |
| BMI (kg/m2), median (range) | 28.62 (20.98)b | 30.67 (25.10) | |
| BMI classification, n (%) | |||
| Normal weight (18.5–24.9) | 40 (18.2) | 16 (14.3) | |
| Overweight (25–29.9) | 100 (45.5) | 30 (26.8) | |
| Obesity I (30–34.9) | 59 (26.8) | 49 (43.8) | |
| Obesity II (35–39.9) | 20 (9.1) | 15 (13.4) | |
| Obesity III (>40) | 1 (.5) | 2 (1.8) | .002** |
| Diagnosis, n (%) | |||
| Primary coxarthrosis | 202 (91.8) | 103 (91.9) | |
| Avascular necrosis | 13 (5.9) | 7 (6.3) | |
| Epiphysiolysis | 2 (.9) | 0 (0) | |
| Dysplasia | 1 (.5) | 0 (0) | |
| Perthes | 2 (.9) | 2 (1.8) | .813**,*** |
| Side, n (%) | |||
| Right side | 123 (55.9) | 70 (62.5) | |
| Left side | 97 (44.2) | 42 (37.5) | .151** |
| Approach, n (%) | |||
| Posterior | 189 (85.9) | 97 (86.6) | |
| Modified lateral | 31 (14.1) | 15 (13.4) | .862** |
| Cup, n (%) | |||
| Delta PF | 148 (67.3) | 72 (64.3) | |
| Delta T | 72 (32.7) | 40 (35.7) | .335** |
| Friction par, n (%) | |||
| Ceramic-polyethylene | 47(21.4) | 42 (37.5) | |
| Ceramic-ceramic | 173 (78.6) | 70 (62.5) | .002** |
| Size of femoral head, n (%) | |||
| 28mm | 40 (18.2) | 13 (11.6) | |
| 32mm | 61 (27.7) | 33 (29.5) | |
| 36mm | 110 (50) | 66 (58.6) | |
| 40mm | 9 (4.1) | 0 (0) | .051**,*** |
| Length of femoral head, n (%) | |||
| Short | 78 (35.5) | 46 (41.1) | |
| Medium | 72 (32.7) | 41 (36.6) | |
| Long | 70 (31.8) | 23 (20.5) | |
| Extra long | 0 (0) | 2 (1.8) | .041**,*** |
BMI: body mass index; SD: standard deviation; THA: total hip arthroplasty.
The investigators adhere to the Oviedo and Helsinki declarations on biomedical research. The ethics committee of our institution gave its approval for the conduct of this study (CEIC code 110/17). The patients included in the study gave their written consent for participation in the study and for the surgical intervention provided by the Spanish Society of Orthopaedic Surgery and Traumatology.
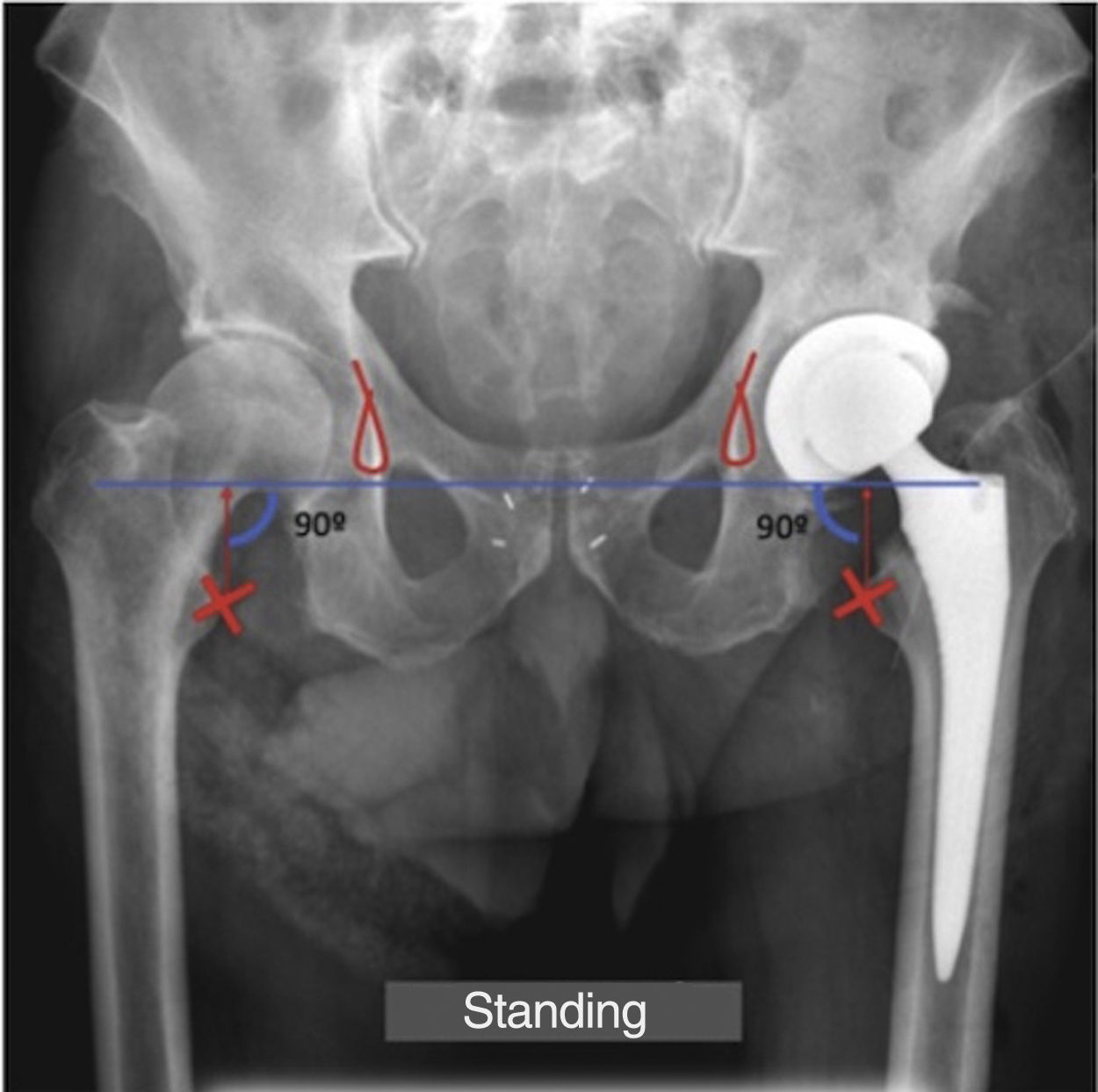
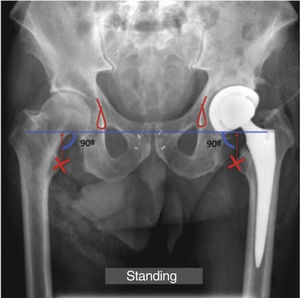
Measurement techniqueAll radiographs were taken on the DR400 system (AGFA HealthCare). Limb length and dissymmetry were assessed radiographically from the anteroposterior radiograph of the pelvis in standing position with knees and feet pointing forward at 6months. We followed the trochanteric method which defines dissymmetry as the difference in the distance between a femoral reference point (the most medial point of the lesser trochanter) and a pelvic reference point (the line joining both radiographic tears or U of the pelvis) on both sides (Fig. 2). The radiographs have been calibrated based on the previously known measurement of the implanted stem.
Surgical techniqueThe surgery was performed by the same four-member surgical team. All surgeries were performed under spinal anaesthesia. The posterior or anterolateral approach was used. Antibiotic prophylaxis consisted of 2g intravenous cefazolin and 240mg gentamicin before anaesthetic induction, followed by post-surgical treatment with 1g intravenous cefazolin every 8h for the first 24h. In case of beta-lactam allergy, cefazolin was replaced by clindamycin 600mg, maintaining the same regimen. Patients received prophylactic treatment for thromboembolic events with low-molecular-weight bemiparin at a prophylactic dose 6h after surgery, which was maintained for 30days.
ImplantsTwo acetabular component designs made of titanium alloy (Ti6A14V) but with different coatings were used, one of porous titanium coated with hydroxyapatite (Delta PF) and the other of trabecular titanium (Delta TT). The femoral head was ceramic in all cases and the insert used was either ceramic or polyethylene. The H-MAX M modular stem and the H-MAX S monoblock stem (Limacorporate, San Daniele, Italy), made of a highly corrosion-resistant titanium alloy (Ti6A14V) with a 55m hydroxyapatite coating, were used as the femoral component. Descriptive data on the implants used are given in Table 1. The interchangeable collars used in the modular implants are made of a cobalt-chromium-molybdenum alloy and have a 12/14 taper with a double radius cross-section and two lateral grooves or channels. They are available in two lengths: short or long. In addition, they have two options of neck-diaphysis angulation, either standard (134) or lateralised (131). These two angulations are available in three different versions: anteverted (+10), neutral (0) or retroverted (10). The appropriate neck was selected based on preoperative planning, intraoperative stability, banded part tension and leg length.
Statistical analysisA descriptive analysis of the length values of the operated hip, the healthy hip and the difference between the two values was performed. Radiographic corrections of dissymmetry at six months were compared in patients with modular stem and monoblock stem. The test applied depended on the normality of the distribution. That is, if the distribution was normal, a Student's t-test was applied and if the distribution was non-normal, the Mann–Whitney U-test was used. We then classified these corrections into three groups by creating a categorical variable based on the magnitude of the limb length difference. We established a group with a value less than a hypocorrection of 10mm (decreased length), another group that is 10mm lower or higher than the contralateral value (restored length) and a third group with a value greater than a hypercorrection of 10mm (increased length). This limit was established following the recommendations found in the literature published up to the present time1. Homogeneity comparisons were performed using the chi-square test at 95% confidence or Fisher's exact test, as appropriate.
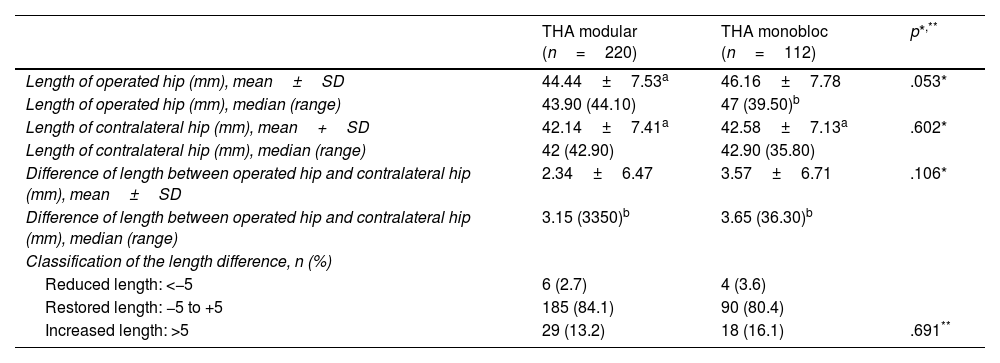
ResultsTable 2 shows the values for the length of the operated limb, the contralateral length and the difference in length between the two limbs. No statistically significant differences were found in any of the three parameters (p=.053, p=.602 and p=.106, respectively) between the two groups. The difference in length in the modular group was 2.34±6.47 and in the monoblock group, 3.57±6.71. The frequency in the distribution of patients according to limb length adjustment (undercorrected, restored or hypercorrected length) is also presented, and no statistically significant differences were found between the modular group and the monoblock group (p=.691). It should be said that for both the modular and monoblock stems, the majority group is the one with the restored length, this result being statistically significant (84.1% and 80.4%, respectively, p=.001, for both groups). On the other hand, in the modular and monoblock groups, we can observe that the length has increased more frequently than decreased, this being statistically significant (p=.005 and p=.001, respectively, for the modular and monoblock groups).
Limb length in patients undergoing modular and monobloc stem surgery at the end of follow-up.
| THA modular (n=220) | THA monobloc (n=112) | p*,** | |
|---|---|---|---|
| Length of operated hip (mm), mean±SD | 44.44±7.53a | 46.16±7.78 | .053* |
| Length of operated hip (mm), median (range) | 43.90 (44.10) | 47 (39.50)b | |
| Length of contralateral hip (mm), mean+SD | 42.14±7.41a | 42.58±7.13a | .602* |
| Length of contralateral hip (mm), median (range) | 42 (42.90) | 42.90 (35.80) | |
| Difference of length between operated hip and contralateral hip (mm), mean±SD | 2.34±6.47 | 3.57±6.71 | .106* |
| Difference of length between operated hip and contralateral hip (mm), median (range) | 3.15 (3350)b | 3.65 (36.30)b | |
| Classification of the length difference, n (%) | |||
| Reduced length: <−5 | 6 (2.7) | 4 (3.6) | |
| Restored length: −5 to +5 | 185 (84.1) | 90 (80.4) | |
| Increased length: >5 | 29 (13.2) | 18 (16.1) | .691** |
THA: total hip arthroplasty; SD: standard deviation.
p represents the comparison between modular and monoblock groups.
Engineers and surgeons have joined forces to solve one of the great challenges of orthopaedics: restoring the biomechanics and anatomy of the native hip. Modularity seeks to faithfully reproduce these parameters. The rationale for using modularity in younger people is based on the importance of improving the longevity of the prosthesis through a more accurate fit of the anatomy in a population that is increasingly demanding joint replacement surgery at a younger age, as mentioned by Berstock et al.13 In addition, the lower BMI in the modular group is based on published biomechanical studies, where a higher body weight means a higher moment of force on the hip and therefore a greater amount of micromotion at the socket. These micromotions result in increased corrosion.8
Radiographic assessment of dissymmetry requires a method that is readily available, accurate and affordable, minimises radiation and has low magnification error. The medical literature has traditionally recommended the teleorthroentgenogram as a method that meets the above-mentioned characteristics, and it has therefore been considered the gold standard.12 However, in clinical practice, certain landmarks on the anteroposterior pelvis radiograph have been used to adequately assess limb dissymmetry,14 instead of using images of the entire lower limbs. According to authors such as Reina-Bueno et al.,15 loading pelvis radiography provides similar data to limb radiography with a positive correlation of their measurements and with less radiation, although they are aware that the teleorthroentgenogram is the only validated method. Meermans et al.16 also state that the loaded anteroposterior pelvis radiograph is as reliable and reproducible as the teleorthroentgenogram. Even so, surgeons must bear in mind that this method does not take into account dyssymmetries due to distal alterations to the hip. In our case, we have used the digital anteroposterior X-ray of the pelvis in standing position, as it meets the minimum requirements previously mentioned, and at the same time allows us to evaluate whether the implanted orthopaedic material is the cause of the alteration in the length of the limb.
Regarding the measurement method used, some authors use the ischial tuberosities as the pelvic reference and the centre of the head as the femoral reference. Meermans et al.16 state that the pelvic tear is better than the line passing through the ischial tuberosities, as it is a more consistent mark and less influenced by the position of the pelvis, while the centre of the femoral head is a more reliable reference point than the lesser trochanter, as the latter is sometimes not well defined and is therefore associated with greater intra-observer variability. Even so, to facilitate measurement and avoid possible bias, we have used the lesser trochanter as the femoral reference point, since it is a greater distance from the tear than the distance between the tear and the centre of rotation of the femoral head. This has allowed us to increase the reliability of our results. In addition, all measurements were performed by the same surgeon, eliminating interobserver variability and minimising estimation bias.
There is no consensus in the literature on the limit value used to consider length restoration.12 However, numerous publications establish a range between 10mm below or above the native length to avoid altering postoperative functional parameters.14,16,17
According to the medical literature, dissymmetry has been published with a mean ranging from 3 to 17mm.17–22 It is noteworthy that the different studies speak of their overall data after implantation of a total hip prosthesis, without specifying the design or including different monoblock models. In our study, as previously mentioned, we relied on a single prosthetic model implanted by a single surgical team, which is one of the strengths of our analysis.
In the analysis of the results obtained in our study with distinction of the prosthetic model used, no statistically significant differences were found in the postoperative dissymmetry or length difference (p=.106) between the group with modular THA and monoblock THA. In reviewing the medical literature, there are few articles comparing length restoration achieved with a double socket stem model versus a monoblock stem. Consistent with our results, Carothers et al.23 report that the TaperKinectiv M/L modular implant (Zimmer, Warsaw, IN, USA) restores the centre of rotation of the head with the same frequency as monoblock implants, and in the analysis of Gerhardt et al.,24 after using the Profemur Z stem (Wright Medical Technology, Arlington, Tennessee, USA), they observed no statistically significant difference in length restoration (less than 5mm difference from the native value). In contrast, Duwelius et al.25 achieve a higher proportion of patients with restored limb length (less than 5mm difference from the native value) in the modular group with TaperKinectiv M/L stem (Zimmer, Warsaw, IN, USA). The same is observed in the study by Archibeck et al.26 using the M/L TaperKinectiv stem (Zimmer, Warsaw, IN, USA), where limb length (difference of less than 1mm from the native value) is restored more frequently in the modular group. We have not found any published article analysing the implant used in our service.
Looking further into our results, we observed that of the 332 patients who completed the follow-up, a dissymmetry between 10mm and 10mm was obtained in 84.1% of the patients in the modular group and in 80.4% of the patients in the monoblock group. This distribution does not show statistically significant differences. In both cases, the predominant group was the one with a restored length, so that, overall, we can say that the objective of restoring biomechanics was achieved in the majority of patients. Lecoanet et al.1 achieved length restoration in 78.6% of patients, while Unnanuntana et al.22 achieved length restoration in 93% of cases. However, we did not always achieve complete length restoration: in patients in whom the operated leg was lengthened, this was 13.2% in the modular group and 16.1% in the monoblock group. Overall, the length was increased in 14.2% of patients. This could be an attempt by the surgeon to achieve prosthetic stability by increasing soft tissue tension, thereby sacrificing limb length. In the literature, an increase in length has been reported in 16%–32% of patients,18 a figure slightly higher than that obtained in our study. In other words, if postoperative dissymmetry is found, it usually consists of a lengthening of the operated leg.27 According to the study published by Lecoanet et al.,1 an increase in length was observed in 14.2% of patients, the same figure as that obtained in our analysis. The study published by Meermanset al.16 found an increase in length in 17.3%, and the study published by Keršič et al.21 found a slightly lower value than that published, with an increase in length in 10% of patients.
As we have seen, the medical literature shows that achieving equality in limb length can be technically complex and difficult to achieve. Moreover, it is a non-modifiable complication in the immediate postoperative period. However, given the potential complications described by the scientific community and the potential source of patient dissatisfaction in the presence of dissymmetry, there is a broad consensus in the orthopaedic community that supports the importance of restoring the length of the operated limb as closely as possible. Although we believe that the availability of interchangeable parts could be of great interest intraoperatively, especially in those cases in which stability is not achieved by other means,28 the scientific evidence obtained in this study in relation to dissymmetry does not allow us to determine the superiority of one design over another. Furthermore, no worse results have been observed for monoblock stems, a logical fact given that they have been a successful design to date in primary hip surgery.24
It is essential to stress the vital importance of careful surgical planning combined with a thorough explanation of the process to the patient in order to create realistic expectations about the outcome that can be achieved after THA. We must also inform patients that there is sometimes a perceived functional discrepancy secondary to post-surgical pelvic obliquity that improves within three to six months.29
Regarding study limitations, we can mention the fact that we have used the anteroposterior pelvis X-ray in standing position, while the gold standard is the teleorthorentogram, which includes the entire lower limbs, taking into consideration other points of possible dissymmetry, such as the femoral diaphysis, the knee, the tibia or the ankle. However, the teleorthorhoentgenogram does not allow us to assess dissymmetry that depends exclusively on the hip implant. In addition, the position of the patient at the time of the X-ray is a parameter that depends on the radiology technician. Finally, we have used the pelvic tear and the lesser trochanter as bony reference points. However, the position of the lesser trochanter may vary depending on the rotation of the leg, so some authors recommend taking the centre of the femoral head as a reference point. Furthermore, we should be aware of the possibility of selection bias as there is, on the one hand, the possibility of changing stem design intraoperatively and, on the other hand, leg length may have been controlled by head length rather than stem design.
ConclusionsModularity aims to avoid any lack of precision thanks to its interchangeable parts, allowing intraoperative adjustment of anatomical parameters. This versatility could be of great interest and help to the surgeon. In our study, for radiographic purposes, we have observed no differences in limb length restoration between modular stems and monoblock stems, through limb length adjustment. Our work does not show a superiority of one design over the other in this aspect. In fact, monoblock stems, with their stem size options, have proven to be a successful design to date. Therefore, the information provided in this paper raises the need for further analysis of the theoretical advantages of using modularity in primary hip surgery, as well as the possible risks involved.
Level of evidenceLevel of evidence II.
Conflict of interestsThe authors have no conflict of interests to declare.
FundingThe authors declare that they have received no funding for the conduct of the present research, the preparation of the article, or its publication.