Ankle fractures represent up to 9% of all fractures, with an increased incidence in the elderly population. Among these fractures, isolated fractures of the lateral malleolus are the most common, representing 65–70% of all cases. The therapeutic decision-making primarily relies on the stability of the ankle ring, considering it stable if affected at one point and unstable if two or more points are affected. Surgical treatment focuses on restoring the length of the fibula, joint reconstruction, stabilising the syndesmosis, and providing a stable fixation. It is crucial to rule out associated injuries that may influence therapeutic management. This article reviews the evaluation and management of lateral malleolus fractures, proposes a decision-making algorithm, and examines several fibular fixation options.
Las fracturas de tobillo representan el 9% de todas las fracturas, con un aumento de incidencia, sobre todo en ancianos. En las fracturas de tobillo, la fractura aislada del maléolo peroneo es la más frecuente, llegando al 65-70% del total. La decisión terapéutica se basa fundamentalmente en la estabilidad del anillo del tobillo, considerándose estable si se afecta en un punto e inestable si son 2 o más. Es crucial descartar lesiones asociadas que puedan influir en la actitud terapéutica. El tratamiento quirúrgico se centra en restablecer la longitud del peroné, la reconstrucción articular, la estabilidad de la sindesmosis y en proporcionar una fijación estable. Este artículo revisa la evaluación y el manejo de la fractura del maléolo peroneo, propone un algoritmo de decisiones y examina diversas opciones de fijación del peroné.
Ankle fractures are very common injuries, lower limb fractures are the most frequent, accounting for 9% of all fractures.1 In recent years, an increase in the incidence of this type of fracture has been observed in all population groups, but especially in the elderly,2 currently the third most common in this group after hip and wrist fracture. Of these fractures, isolated fracture of the peroneal or lateral malleolus is the most frequent, representing 65–70% of all cases.4
The therapeutic decision in ankle fractures is based on stability, the osteoligamentous integrity of the medial column being essential.4,5 The ankle behaves as a ring of bony and ligamentous structures. The stability of this ring will depend on whether it is broken at a single point (stable injury) or whether it is affected at 2 or more points (unstable injury).4,5 In this sense, unimalleolar fractures, which do not present associated injuries, are considered stable and, therefore, in most cases, conservative treatment is recommended, and ambulation with weight bearing is allowed.4,6,7 It is essential in these fibula injuries to rule out key associated injuries, whether in the medial or posterior column or in the syndesmosis, which may influence therapeutic management.4,8–10 On the other hand, bimalleolar and trimalleolar fractures are considered unstable and in general, if patients are ambulant and fit for surgery, they will benefit from surgical treatment.4,6 In the surgical treatment of these unstable injuries, correct reduction (restoring the length of the fibula being a key factor) is essential, as well as providing stable fixation to allow early weightbearing.6 However, in elderly and other fragile patients (diabetic, immunosuppressed, etc.), techniques should be considered to increase stability and/or reduce soft tissue damage.6,11–13
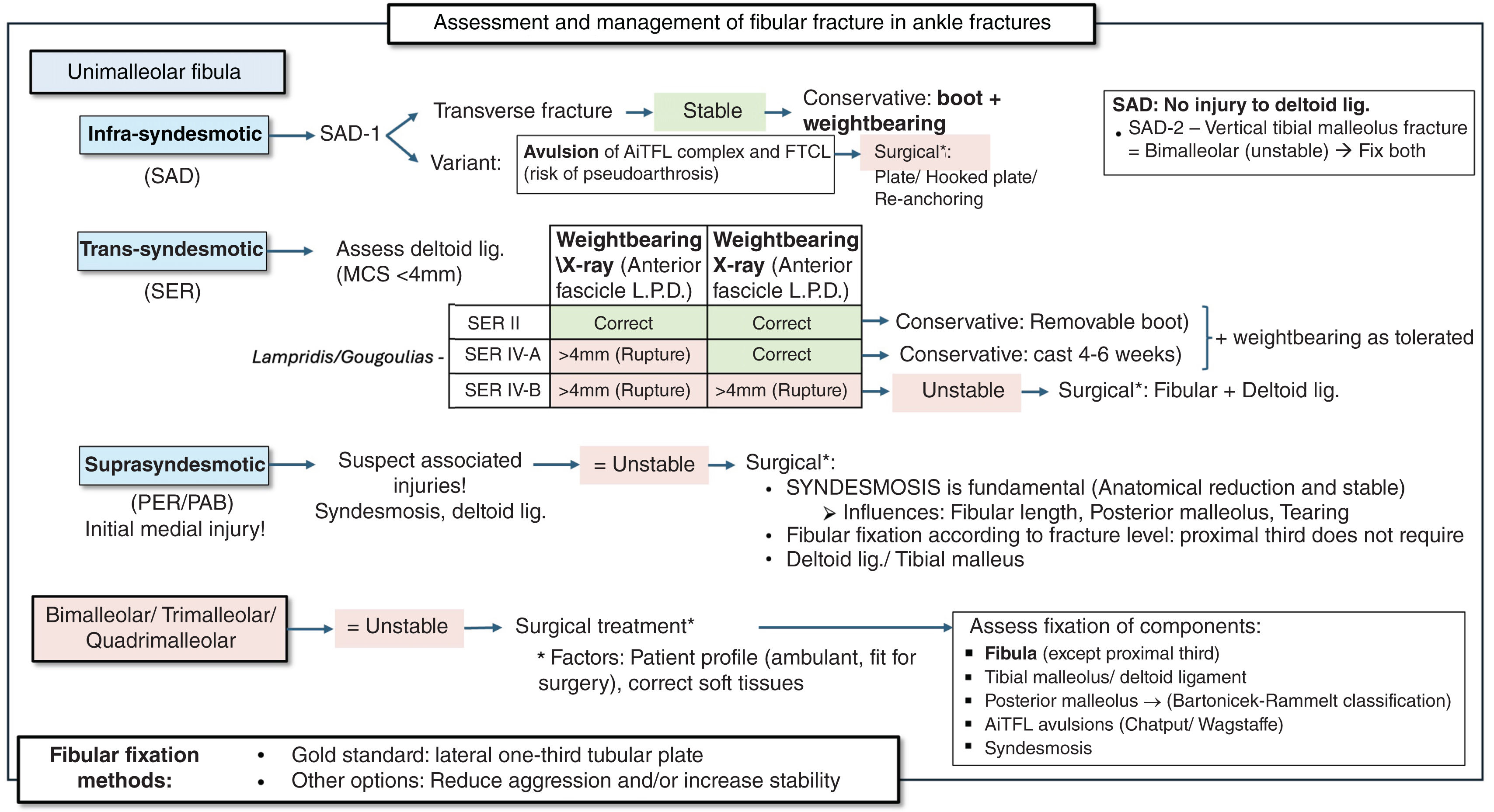
The aim of this paper is to present an update on the management of peroneal malleolus injury in the context of ankle fractures. We also propose a decision-making algorithm (Fig. 1) and review different options for fixation of the fibula.
ClassificationsSeveral classifications have been used to describe these fractures.5 The Danis–Weber classification is the most widely used for fractures of the peroneal malleolus due to its simplicity. It divides fractures according to the level of injury of the fibula in relation to the syndesmosis: below the syndesmosis (Weber A), at the level of the syndesmosis (Weber B), and above the level of the syndesmosis (Weber C). However, this classification does not assess stability because it does not consider the medial component. The AO/OTAclassification14 details different groups within each type. This classification has become the most widely used academically, due its simplicity and inter-observer reliability.15
- •
Type A: Includes infrasyndesmotic fractures. The tibioperoneal joint remains intact. They are subdivided into A1 (isolated fractures of the lateral malleolus), A2 (associated fractures of the medial malleolus), and A3 (trimalleolar fractures).
- •
Type B: Trans-syndesmotic fractures. The tibioperoneal joint may be involved. They are subdivided into B1 (isolated fractures of the lateral malleolus), B2 (associated medial injury), and B3 (associated medial and posterolateral injury).
- •
Type C: Suprasyndesmotic fractures. The injury may significantly compromise the stability of the ankle. They are subdivided into C1 (single fibula fracture), C2 (multifragmentary fracture), and C3 (proximal fibula fractures). All of these are associated with medial injuries (bony or ligamentous) and/or injuries to the posterior malleolus.
Of all these fractures, the most frequently observed in epidemiological studies are type B1.2
The Lauge–Hansen classification16,17 is based on the mechanism of injury (position of the foot and the direction of the force applied). It is divided into 4 fundamental groups, each type having several stages, with the anatomical lesions progressing in a predictable sequence. In order of frequency, they are:
- •
Supination-external rotation (SER):
- ∘
Trans-syndesmotic fibula fracture (SER-2).
- ∘
May progress to posterior injury (SER-3) and eventually medial injury (SER-4).
- ∘
- •
Pronation-abduction (PA):
- ∘
Initial medial injury (medial malleolus fracture or deltoid ligament injury).
- ∘
May progress to supraspinatus comminuted fracture of fibula.
- ∘
- •
Pronation external rotation (PER):
- ∘
Initial medial injury.
- ∘
May progress to simple suprasyndesmotic fibula fracture.
- ∘
- •
Supination-adduction (SAD):
- ∘
Lateral ligamentous injury or transverse infrasyndesmotic fracture of fibula (SAD-1).
- ∘
May progress to vertical line fracture of internal malleolus with or without medial tibial marginal impaction (SAD-2).
- ∘
For this article, focusing on fractures of the peroneal malleolus, we will follow the scheme based on the level of the fracture according to the Danis–Weber and AO/OTA classifications.
Infrasyndesmotic fracturesInfrasyndesmotic fractures of the fibula are usually stable fractures that do not affect the syndesmosis, although occasionally they may be associated with lateral and medial ligamentous injuries.4,18
Under the AO/OTA classification, the most frequent infrasyndesmotic fractures are A1 (isolated) at 68.9%, followed by A2 (bimalleolar) at 24.8%, and finally A3 (trimalleolar) at 6.3%.2
With regard to the Lauge–Hansen classification, infrasyndesmotic fractures correspond to the SAD type, with an incidence between 10% and 20%. In turn, these can be divided into SAD-1 (transverse fibula fracture or fracture-avulsion) or SAD-2 (vertical associated fracture of the internal malleolus).
The deforming force begins when the foot is progressively adducted while supinated, initially producing lateral column failure when exceeding 30–45°, developing a rupture of the anterior inferior tibiofibular ligament (AiTFL) and calcaneofibular ligament and/or a transverse line of the distal fibula (SAD-1). If the injury progresses, external rotation, and varus of the talus occurs, forming a shearing force that may result in impaction and collapse of the medial articular surface of the tibia, ultimately resulting in a vertical fracture of the internal malleolus (SAD-2), with no rupture of the deltoid ligament.19
Transverse infrasyndesmotic fractures (SAD-1) can be considered stable (integrity of the syndesmosis and medial complex) if they present a displacement of less than 2mm.20 Conservative treatment with early weightbearing as tolerated with the aid of a stabilising orthosis, semi-rigid ankle brace, or CAM walker boot is currently recommended.21
A relevant variant of SAD-1 is avulsion of the AiTFL and fibulotalocalcaneal complex, these ligaments being connected by arciform fibres.22
When there is a forced inversion movement, these ligaments tear from the fibula with subsequent instability of the talus within the ankle mortise. This avulsed fragment, with the inserted ligaments, has hypermobility that ultimately increases the space between the fibula and the fragment, increasing the risk of pseudoarthrosis and chronicity of this injury. Haraguchi et al.23 found 35% pseudarthrosis in patients with avulsions treated conservatively. They observed a large retraction of the fragment due to the traction exerted by the ligaments, which resulted in further separation of the fragment from the fibula.23 Therefore, surgery is a viable, reproducible option with good postoperative results. Available procedures include removal of the bone fragment and re-anchoring of the ligaments, synthesis of the fragment with compression plates and/or screws, or anatomical reconstruction plasties in cases of chronic instability18,23 (Fig. 2).
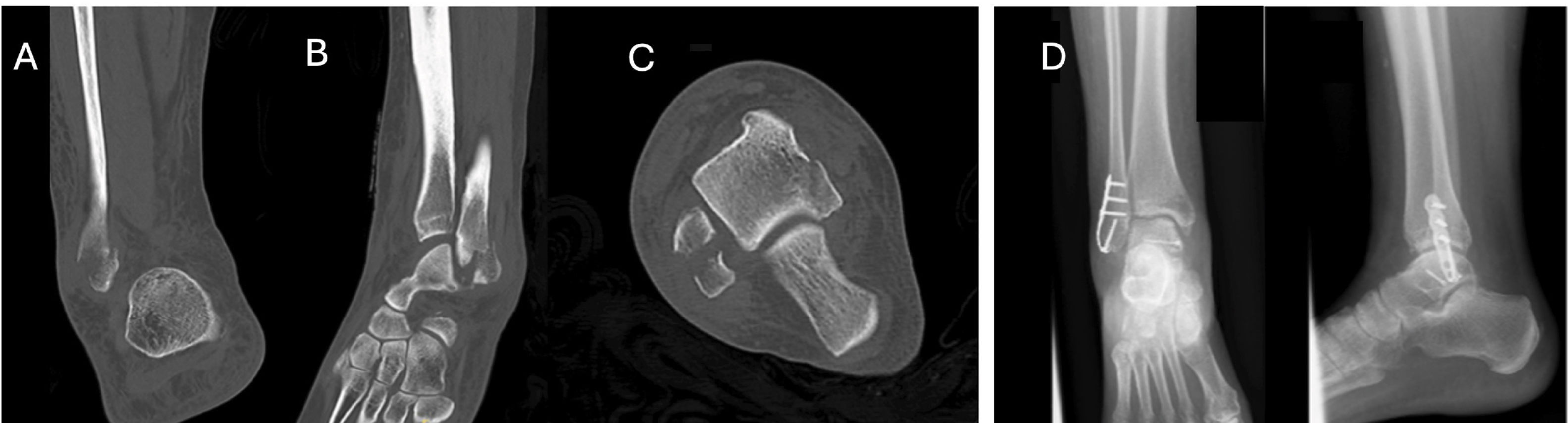
In SAD-2, where there is an associated vertical fracture of the medial malleolus, a CT scan is recommended to rule out joint impaction of the internal column, which can occur in 61–73% of cases.18,24 In this type of fracture, surgical treatment of both malleoli is required. For fixation of the medial column, it is recommended to follow the same principles as for treatment of a tibial pilon, using a medial plate to improve biomechanical support, and to restore joint collapse18,25 (Fig. 3).
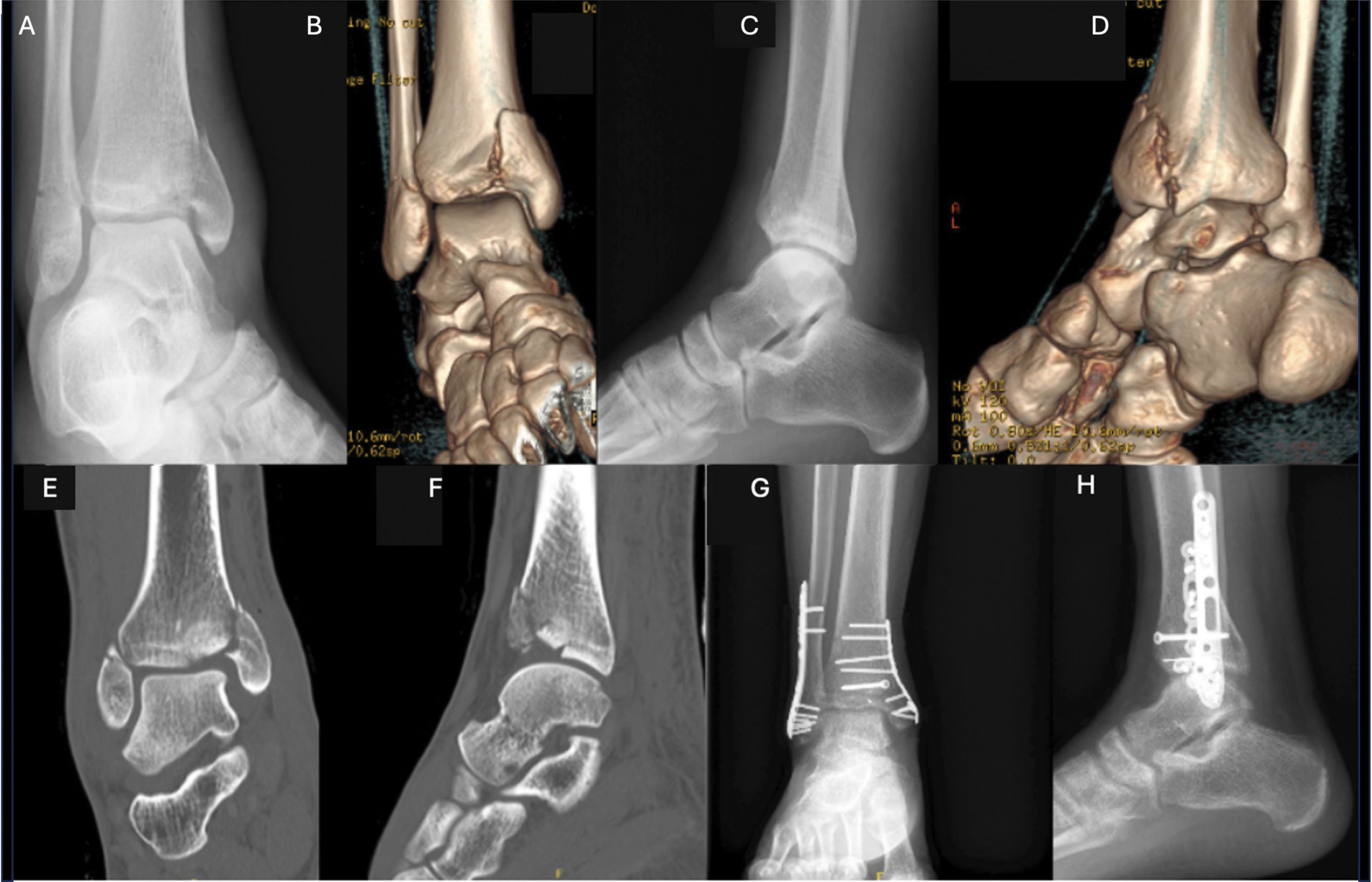
(A–D) Example of transverse fracture of the infrasyndesmotic fibula SAD-2 with vertical line in the internal column. (E and F) CT image showing medial impaction and articular cartilage collapse. (G and H) Postoperative X-rays showing osteosynthesis using anatomical fibula plate, anti-glide plate in internal column, K-wire, and lag screw to restore the articular surface.
These are produced by a rotational mechanism, when an external rotational force is applied to the supinated foot (SER).5,17
According to the AO/OTA classification,5 44-B1 would be the most frequent (51.8%), followed by 44-B2 (25.3%), and finally 44-B3 (22.9%).2
The injury begins in the external column, at the level of the anterior tibioperoneal ligament, extends externally, affecting the lateral column, and progresses sequentially in a posterior direction, to eventually produce a medial injury.1
Traditionally, greater importance was given to the injury to the lateral column to decide the management of these fractures.27,28 However it is now known that ankle stability depends primarily on the integrity of the medial column (deltoid ligament and medial malleolus).27–29
For the correct management of SER fractures, it is essential to understand the anatomy of the deltoid ligament. This ligament is composed of 2 fascicles, one superficial and one deep.30 The superficial fascicle resists plantar flexion and valgus of the talus in relation to the tibia. The deep fascicle is the main stabiliser of the deltoid, mainly resisting external rotation as well as lateral and posterior translation of the talus. It is composed of 2 parts: the deep anterior tibiotalar ligament (dATTL) and the deep posterior tibiotalar ligament (dPTTL). The dPTTL is the stability player, it tightens in plantigrade position, as occurs during weightbearing, and relaxes in plantar flexion.30,31
SER-type injuries are divided into 4 main groups:
- •
SER 1: Injury to the AiTFL without bone injury.
- •
SER 2: Short oblique fracture of the distal fibula without injury to the inner ankle.
- •
SER 3: Associated injury to the posterior malleolus or the posterior inferior tibiofibular ligament (PITFL) due to progressive rotational force.
- •
SER 4: Associated transverse fracture of the internal malleolus or injury to the deltoid ligament.
In 2017, Gougoulias and Sakellariou, and Lampridis et al.4,5 described a new subclassification of ligamentous SER 4 fractures, according to the degree of involvement of the deep deltoid ligament.
- •
SER 4a: There is injury to the superficial fascicle and dATTL, while the dPTTL is intact, being stable injuries (potentially unstable if not treated correctly).
- •
SER 4b: There is a complete rupture of the deltoid ligament (superficial fascicle, dATTL and dPTTL), resulting in an unstable injury.
This new subclassification provides guidance for the management of SER 4 type injuries, giving the greatest importance to the integrity of the dPTTL in deciding the most appropriate treatment in these subtypes.
In SER fractures, signs of swelling, haematoma, and pain in the medial region of the ankle are unreliable predictors of deltoid ligament injury.26 Plain X-ray is essential in the case of suspicion of medial associated injuries for measuring the medial clear space (MCS) from the internal malleolus to the medial border of the talus. If the MCS is >4mm, or 1mm greater than the superior tibiotalar space, it implies an injury to the deltoid ligament. This assessment will differentiate between SER 2 (deltoid ligament integrity) and SER 4 (deep deltoid ligament injury) fractures. Non-weightbearing X-rays with plantar flexion really assess the dATTL injury. However, information on the integrity of the dPTTL requires a weightbearing X-ray (at 90° of dorsiflexion). If there is no increase in the MCS on weightbearing X-rays, it is considered a SER 4a fracture and is classified as stable. Conversely, if the MCS remains increased, it implies injury to the dPTTL and is classified as unstable (SER 4b)4,5 (Fig. 1). These weightbearing X-rays can be performed in the emergency department, or in consultations (at one week), depending on pain tolerance.32 However, the gravity test overestimates the injury to the medial column, which is why it is no longer used.33 In relation to syndesmosis injury, obliquity of the fibula fracture line (longer lines) and widening of the MCS have been identified as possible predictors.34 CT scanning is recommended to assess joint steps, associated posterior malleolus fractures and evaluation of the syndesmosis.35
SER 1 and 2 injuries can be treated conservatively. Specifically, SER 2 injuries can be treated with a removable boot and immediate weightbearing, as immobilisation is prescribed primarily for pain control, not because these fractures displace with weightbearing.36
In SER 3 fractures, we must assess the type of posterior malleolus fracture. It has been known for several years that size is not a determining factor in the treatment of these posterior injuries, and that other factors must be considered, such as syndesmotic instability, a joint step greater than 1–2mm, impaction of the tibial articular surface, and the presence of intercalary fragments.37 The Bartonicek–Rammelt classification may be useful for decision-making in these posterior malleolus fractures.34
SER 4 fractures with medial bone injury (bimalleolar or trimalleolar) are considered unstable injuries and surgical treatment is recommended. However, in the case of SER 4 fractures with medial ligamentous injury, we divide them, depending on whether or not the posterior fascicle of the deep deltoid ligament (dPTTL) is injured, into stable (SER 4a) and unstable (SER 4b).4,5SER 4a fractures can be treated conservatively, using a 90° weight-bearing cast4,38 (Fig. 4). It is important to note that this weightbearing cast should not be removed or replaced by a removable boot, as dorsal flexion at 90° helps the anterior fascicle of the deep deltoid ligament to heal in an appropriate position. If a removable boot were used, this ligament could heal in an incorrect position, which could lead to ligamentous laxity and instability of the ankle in plantar flexion. Thus, SER 4a fractures are potentially unstable if treated incorrectly. However, SER 4b fractures are considered unstable from the outset and require surgical treatment of the fibula and deltoid ligament (Fig. 4). This is because the posterior fascicle of the deep deltoid ligament cannot heal on its own and needs repair.36
Example of SER 2 fracture. (A) Non-weightbearing X-ray showing bilateral trans-syndesmotic fibular fracture. (B) Weightbearing X-ray MCS maintained (<4mm). It was treated by immediate weightbearing without immobilisation. (C) Weightbearing X-ray at 6 months showing correct fracture healing. Example of a SER 4a fracture. (D) Non-weightbearing X-ray with increased MCS (>4mm). (E) Weightbearing X-ray showing reduction of the medial clear space with loading at 90°. The fracture was managed conservatively with a weightbearing cast. Example of SER 4b ankle fracture. (F) Weightbearing X-ray showing opening of the MCS and asymmetry of the mortise (unstable lesion). (G) Surgery is indicated with open reduction and internal fixation with plate and screws in the fibula and fixation of the syndesmosis by means of a dynamic system.
These are fractures of the fibula occurring above the syndesmosis. We must always suspect and rule out an associated injury to the medial column and syndesmosis, which will imply an unstable injury.
They correspond to Weber classification type C and, following the AO/OTA classification, type 44C1 would be the most frequent (5.3%), followed by C2 and C3 (3.2% and 3.4% respectively).2
According to the Lauge–Hansen classification, they usually appear in pronation external rotation type fractures and in PAB fractures.5
The deforming force begins when external rotation or abduction is applied to the pronated foot. The medial column is injured first, either at the bony or ligamentous level. If the injury progresses, the force continues to the lateral side and ends up causing injury to both the ligaments of the syndesmosis and the fibula itself, resulting in a suprasyndesmotic fracture.9 In pronation external rotation type injuries, the fibula fracture is usually simple and in PAB it is usually comminuted.
The fundamental injury in this type of fracture is syndesmotic involvement. The syndesmosis comprises 3 main ligaments: the AiTFL, the interosseous tibiofibular ligament, which is the lower part of the interosseous membrane, and the PiTFL.9 These provide a 3-point anchorage between the tibia and fibula that is essential for the stability of the bony ankle mortise.9,39 During assessment of a syndesmosis injury on plain X-ray, the following parameters may be affected40:
- -
Decreased tibiofibular overlap: measured at the point of maximum overlap. Suggestive of injury if less than 6mm on anteroposterior X-ray or 1mm on mortise X-ray.
- -
Increased tibiofibular clear space: the distance between tibia and fibula is measured at 1cm from the joint. Suggestive of injury if greater than 6mm on both the anteroposterior and mortise views.
- -
Increased MCS: the distance between the talus and the outer part of the medial malleolus is measured. Suggestive of injury if greater than 4mm.
When an external rotation mechanism fracture occurs, there is sequential tearing of these ligaments starting anteriorly and progressing posteriorly. Isolated injury to the AiTFL confers anteroposterior instability. If associated with injury to the interosseous tibiofibular ligament rotational instability is added. Finally, rupture of the PiTFL causes multidirectional instability that allows frank diastasis.9,40 It should be noted that these ligamentous lesions may present as bony tears of Chaput's tubercle (tibial insertion of AiTFL), Wagstaffe's fragment (fibular insertion of AiTFL), or Volkmann's fragment (tibial insertion of PiTFL).9
An X-ray of the entire tibia should be included for the correct study of these injuries, especially if there is suspicion of a Maissonneuve fracture. Maissonneuve fracture is defined as a fracture of the proximal third of the fibula combined with at least a rupture of the anterior tibioperoneal ligament and the tibioperoneal interosseous ligament.10 To rule out other associated injuries, such as injury to the deltoid ligament, fracture-avulsions, or posterior malleolus fractures, weightbearing X-rays, CT scan, and even diagnostic-therapeutic arthroscopy are recommended if syndesmosis injuries are suspected that are unclear on X-ray.10
Given the inherent instability of these fractures, surgical treatment is recommended. The primary goal will be to achieve a stable syndesmosis with an anatomical reduction of the fibula at the fibular incisura. Restoration of length (shortening≥2mm), correction of external rotation, and sagittal angulation are essential in fibular osteosynthesis.10 However, when these fractures are located in the proximal third, fixation is not recommended due to the risk of injury to the common peroneal nerve.10 To assess the stability of the syndesmosis, the most commonly used manoeuvres are the external rotation test and the bone hook test, although neither has been shown to be completely reliable.8,41 For this reason, assessment of the stability and anatomical reduction of the syndesmosis may require direct visualisation, either by arthroscopy or using a direct anterior approach.5,42 Recent studies evaluating the syndesmosis by postoperative CT scan describe malreductions in up to 40%.8,43 The syndesmosis can be stabilised by trans-syndesmotic screws (2mm×3.5mm tri- or quadricortical screws) or by flexible fixation (suture-button systems).10
Finally, with regard to associated posterior malleolus fractures, it is worth highlighting their role in the stability of the syndesmosis due to their insertion of the PiTFL. Its osteosynthesis may have an even greater stabilising role than trans-syndesmotic fixation itself.44 For this reason, in supraspinous fractures with associated fractures of the posterior malleolus, direct osteosynthesis of the posterior malleolus is recommended as a first step in surgical treatment, as it will greatly assist in achieving an anatomical reduction of the syndesmosis.42
Fixation options for fibular fracturesThe standard or gold standard treatment for these fractures remains the lateral one-third tubular plate.45–47 Other fixation options are aimed at increasing stability and/or reducing soft tissue damage.48,49 The therapeutic decision will depend on the type of fracture, soft tissue status, bone quality, and patient type.6,20
Lateral plates (one-third tubular versus locking plates)Lateral plate fixation can have a complication rate of up to 30%, the most frequently reported being dehiscence.11 This is due to soft tissue damage caused by trauma in an area with already limited soft tissue coverage. The risk increases in elderly patients, smokers, and in patients with comorbidities such as peripheral vascular disease or diabetes.11–13 To reduce these complications, these plates can be implanted using minimally invasive techniques.48
Several studies comparing standard one-third tubular locking plates with anatomical locking plates show no significant differences in clinical or radiological outcomes,48,50–52 except for the increased costs associated with the latter.45 Therefore, many authors suggest individualising each case, reserving the use of locking plates for cases with severe osteoporosis, comminuted fractures, or very distal fragments. The main advantage of the new anatomical plates is that they allow a greater option of fixation at the distal level, especially in cases where the conventional plate does not allow at least two screws to be implanted in the distal fragment.50,52
Combining lateral plates with other techniques may also be a useful strategy to increase stability. The use of one-third tubular plates (locking or conventional) or anatomical locking plates can be combined with pins or intramedullary screws. In addition, lateral plate screws can be augmented with cement in patients with severe osteoporosis.6
Antiglide posterior platePosterior plates may provide a biomechanical advantage for oblique distal fibula fractures. This posterior placement counteracts the displacement of the distal fragment proximally and posteriorly, acting as an antiglide mechanism. In addition, this position facilitates the insertion of a lag screw through the plate and allows the placement of bicortical screws in the distal region, without the risk of penetrating the joint.49,53
Compared to the lateral plate, the posterior plate decreases pain due to the prominence of the osteosynthesis material. However, a higher incidence of peroneal tendon irritation and the need to remove the osteosynthesis material has been observed.54 Therefore, it is recommended to avoid extending the endplate beyond the beginning of the osteosynovial peroneal groove.54 Furthermore, Kilian et al.55 suggest avoiding placing the screw further distal to the plate to prevent peroneal tendinopathy. However, if placement of the latter distal screw is necessary, it is recommended not to use an oblique direction to avoid a protruding screw head.54
For the placement of these plates, 2 types of approaches can be used: lateral or posterolateral. The posterolateral approach offers the additional advantage of also allowing osteosynthesis of the posterior malleolus through a single surgical access.55
Double platingThe double plating system, combining lateral and posterior plates, may be indicated for cases of fibular fractures with severe comminution or severe osteoporosis, offering greater intrinsic stability.56 Kwaadu57 uses 2 low-profile locking plates, observing excellent functional results and a lower incidence of problems with posterior plate intolerance. However, Vance58 deploys the double plating technique using one-third tubular plate in comminuted fractures, achieving satisfactory results, and propose this method as an economical and stable option for this type of injury.
Tibia pro-fibulaThe “tibia pro-fibula” technique consists of the placement of 2–4 trans-syndesmotic screws through the lateral fibula plate, irrespective of whether there is injury to the syndesmosis. This technique aims to increase stability by taking advantage of the tibia as a support point, allowing the screws to be fixed in 4 cortices. This option is especially beneficial in patients with severe osteoporosis or diabetic neuropathy, and even offers sufficient strength to allow immediate weightbearing.3,6
Hooked locking platesThe use of hooked locking plates can be of great benefit in distal fracture-avulsions or for comminuted infrasyndesmotic fractures. A recent study, focusing on tibial pilon fractures with associated comminuted fibular fractures, compares these hooked plates with non-locking plates. The results show significant functional improvement with hooked plates, shorter fracture healing time, and a lower incidence of complications.59
Intramedullary fibular screwsIntramedullary screws allow for less soft-tissue injury and provide sufficient stability in non-comminuted fibular fractures.60,61 They offer additional advantages, such as preventing discomfort caused by protruding material, avoiding injury to the peroneal tendons, and preventing intra-articular penetration of screws.60
In a biomechanical comparison of plate and lag screw fixation versus intramedullary nail for single line fractures, no differences in torsional strength were found.62 Giordano, using intramedullary techniques (screws or nails), obtained excellent results with very low complication rates, proposing this technique as safe and effective for almost any distal fibular fracture pattern.63
In a systematic review, Loukachov et al. conclude that the intramedullary screw is a safe technique, with low rates of soft tissue complications, and without the high costs associated with nails.60 However, the disadvantage of the intramedullary screw lies in the difficulty of controlling the length of the fibula in comminuted fractures, unlike the new intramedullary nails.62
Screws with a diameter of 3.5, 4.2, or 4.5mm are the most commonly used for this intramedullary technique.60 Reduction techniques can be performed with percutaneous forceps under fluoroscopic control, prior to screw insertion. Ideally, 3.5mm long cortical screws are preferred, as they have great flexibility and ability to adapt to the medullary canal.61 The 3.5mm screw also allows sufficient space to combine fixation with a percutaneous trans-syndesmotic screw60 (Fig. 5).
Intramedullary fibular nailThe main advantages of this technique are similar to those of the intramedullary screw: less aggression to soft tissue, less discomfort from protruding material, greater respect for bone biology, and lower complication rate.64–66
Early nail designs had complications such as implant migration and shortening of the fibula, and not allowing proximal fixation. However, the new nails allow proximal and distal locking, and indications can even extend to comminuted fractures, maintaining the length of the fibula.65,66 These new nails also allow stabilisation of associated lesions of the syndesmosis, with the possibility of placing screws or dynamic systems through the nail64,65 (Fig. 6).
Example of a fibular fracture treated with a second-generation intramedullary nail due to soft tissue involvement. (A) Clinical image showing severe soft tissue injury (open fracture wound). (B) Preoperative X-rays showing bifocal fibula fracture. (C) Postoperative X-rays showing second generation nail fixation and trans-syndesmotic fixation with 2 screws through the nail.
Biomechanical cadaveric studies comparing locking plates with intramedullary nails show similar results in terms of load resistance and implant fatigue.67 Other studies describe superior results in torsional resistance in favour of nailing compared to one-third tubular plate and lag screw.62
Clinical studies comparing plates versus first generation intramedullary nails find no differences in clinical or functional results.65 However, more recent studies comparing second generation nails with plates report superior results in favour of nails, with better functional results, lower infection rate, and lower overall cost.65,68,69 Some authors consider the intramedullary nail the treatment of choice in patients at risk or with severe soft tissue injury.66
ConclusionsIn the assessment and management of fibular fractures, it is essential to consider the stability of the ankle ring, considered stable if only one point is affected, and unstable if there are 2 or more. The surgical approach, adapted to each type of fracture, focuses on restoring the length of the fibula, joint reconstruction, and stability of the syndesmosis, as well as providing stable fixation with minimal soft tissue damage to allow early weightbearing. It is also essential to rule out all associated injuries that may influence treatment. This article presents a comprehensive review of the management of peroneal malleolus fractures and a decision algorithm, and discusses various options for fibular fixation, with the aim of facilitating decision-making in this increasingly common condition.
Level of evidenceLevel of evidence ii.
Conflict of interestsThe authors have no conflict of interests to declare.