Open reduction is rarely performed in pediatric supracondylar humerus fractures. However, clear evidence is lacking regarding the optimal open approach to achieve satisfactory results. The anterior approach provides direct visualization of the fracture and excellent exposure to neurovascular structures, although its utilization is less common. The objective of this study was to review the indications, outcomes, and complications associated with the anterior approach for open reduction of these fractures.
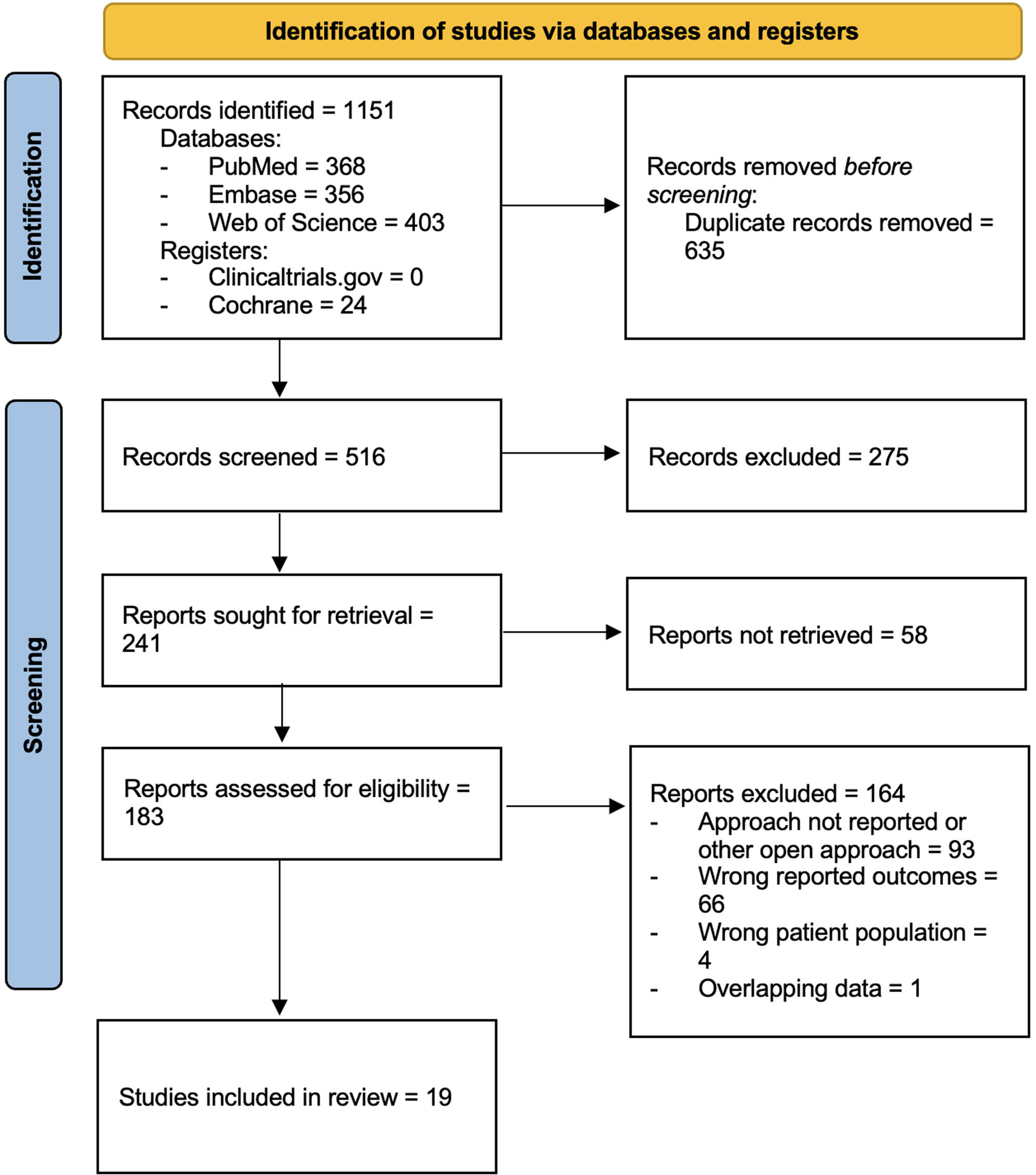
MethodsOur protocol was registered at PROSPERO: CRD42023446923. MEDLINE/PubMed, Embase, Web of Science, Clinicaltrials.gov, and Cochrane Library were searched from database inception to search date (December 2023) and screened in duplicate for relevant studies. Data were collected regarding patient demographics, indications for open reduction, Flynn's functional and cosmetic outcomes, and complications. Study quality was assessed using the Methodological Index for Non-Randomized Studies Criteria.
ResultsA total of 19 studies involving 483 patients were included. One study was classified as Level 2 evidence, ten as Level 3, and eight as Level 4. The mean MINORS score was 13.05±3.47. The primary indication for open reduction was failed closed reduction, observed in 46% of patients. 97.7% and 98.6% of patients achieved Flynn's functional and cosmetic satisfactory results, respectively. The postsurgical neurovascular injury rate was 1.4%. One patient required reintervention.
ConclusionThe anterior approach is safe and effective for managing pediatric supracondylar humerus fractures requiring open reduction.
Level of evidenceSystematic review of Level 2–4 evidence studies.
La reducción abierta rara vez es necesaria en las fracturas supracondíleas de húmero pediátrica. Sin embargo, falta evidencia sobre cuál es el abordaje óptimo para obtener resultados satisfactorios. El abordaje anterior facilita una visión directa de la fractura y una excelente exposición de las estructuras neurovasculares, aunque su uso es poco común. El objetivo de este estudio fue revisar las indicaciones, resultados y complicaciones asociadas con el abordaje anterior para la reducción abierta de estas fracturas.
MétodosNuestro protocolo se registró en PROSPERO: CRD42023446923. La búsqueda se realizó en MEDLINE/PubMed, Embase, Web of Science, Clinicaltrials.gov y Cochrane Library, desde inicios hasta diciembre de 2023. Se realizó screening por duplicado. Se recogieron datos demográficos, indicaciones para el abordaje abierto, puntuación de Flynn funcional y estética y complicaciones. La calidad de los estudios se evaluó con Methodological Index for Non-Randomized Studies Criteria (MINORS).
ResultadosSe incluyeron 19 estudios que agrupaban a 483 pacientes. Un estudio se clasificó con nivel de evidencia 2, 10 con nivel 3, y 8 con nivel 4. La puntuación media MINORS fue 13,05±3,47. La indicación principal para el abordaje abierto fue el fracaso de la reducción cerrada, reportada en 46% de pacientes. El 97,7% y 98,6% de los pacientes lograron un Flynn funcional y cosmético satisfactorio, respectivamente. La tasa de lesiones neurovasculares postquirúrgicas fue 1,4%. Un paciente fue reintervenido.
ConclusionesEl abordaje anterior es seguro y efectivo en el maneco de fracturas supracondíleas de húmero pediátricas cuando se requiera un abordaje abierto.
Nivel de evidenciaRevisión sistemática de estudios con nivel de evidencia 2-4.
Supracondylar humerus fractures (SHFs) are the most frequent traumatic fractures around the elbow in children.1 While non-displaced or minimally displaced fractures are typically managed conservatively,2 for displaced fractures the gold standard approach entails closed reduction percutaneous pinning (CRPP) followed by immobilization with a posterior plaster cast for 3–4 weeks.3 However, almost 13% of SHFs require open reduction when closed reduction proves ineffective4,5 or in the presence of factors such as an open fracture, neurovascular injury, compartment syndrome, skin puckering, other soft tissue complications or delayed presentation.6,7
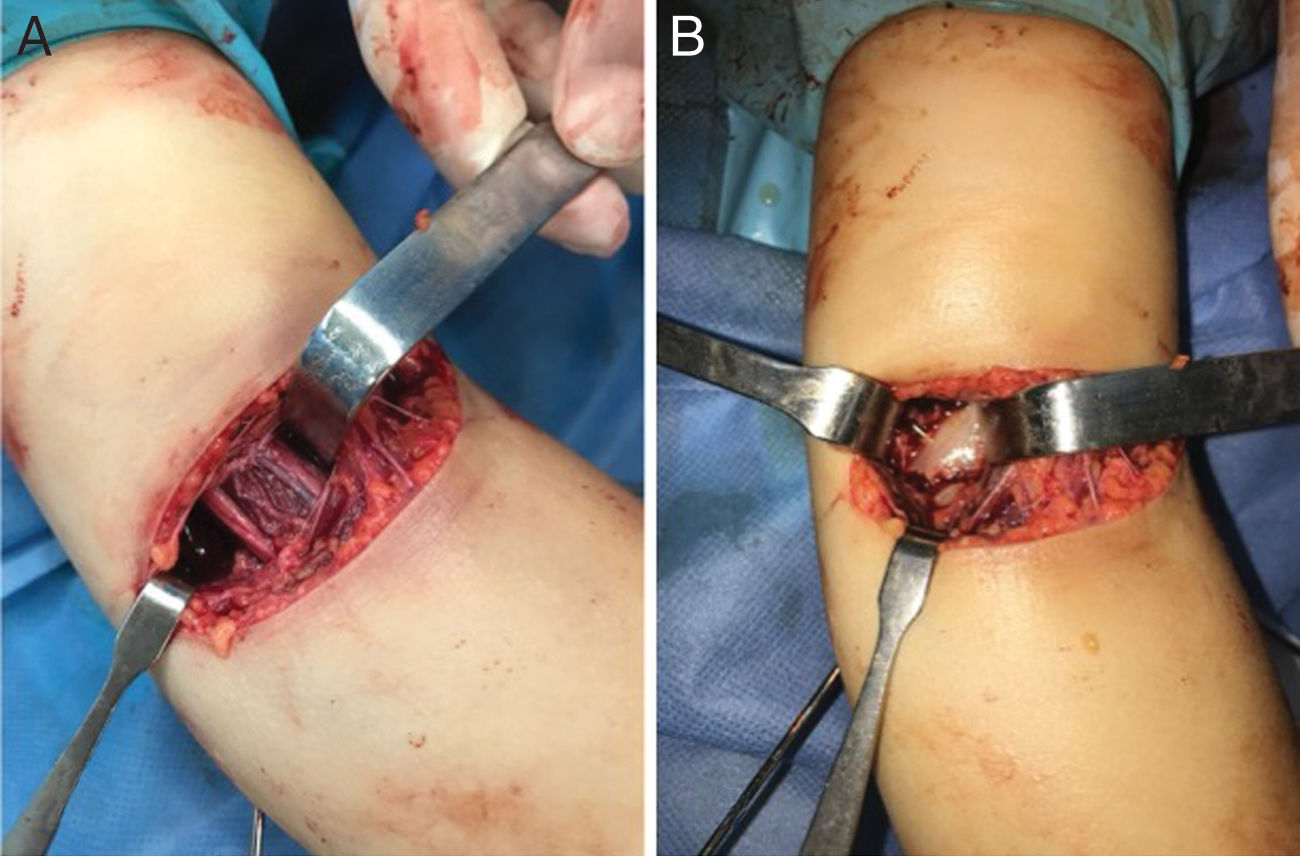
Various approaches exist for open reduction, with the posterior, medial, lateral, and anterior methods being the most utilized. Surgeons can favor one approach over the others based on fracture displacement, concomitant injuries, or their own experience and preference. However, the optimal open approach to achieve favorable functional and cosmetic outcomes remains undetermined. The lateral, medial, and posterior approaches necessitate less intricate identification of neurovascular structures and are favored for their simplicity. In contrast, despite it could be considered more technically demanding, the anterior approach affords superior exposure to neurovascular structures, does not violate posterior periosteum, and enables improved access for evaluating the potential interposition of the brachialis muscle or other structures at the fracture site.8,9
Numerous case series and some comparative studies delineating the utilization of an anterior approach for open reduction of SHF in pediatric patients have been documented. However, to the best of our knowledge, no systematic review in the literature has been conducted to assess the indications, outcomes and potential complications of this approach.10,11 Thus, we conducted a systematic review to provide comprehensive insights into the functional and cosmetic outcomes and complications associated with the anterior approach for open reduction of SHF. We hypothesized that the anterior approach would lead to satisfactory outcomes and a low complication rate.
Material and methodsThis review was conducted according to the Cochrane Handbook for Systematic Reviews of Interventions, and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guided this systematic review. The protocol was registered on the PROSPERO International Prospective Register of Systematic Reviews (Registration number CRD42023446923).
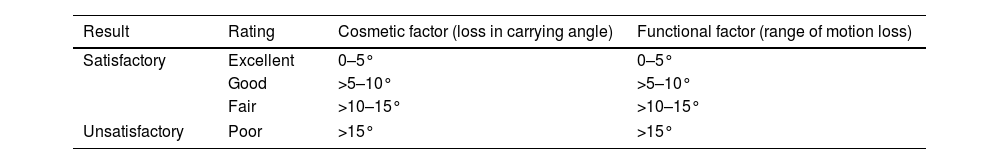
Eligibility criteriaThe inclusion criteria were established using the PICO concept (patient, intervention, comparison, outcome). This included skeletally immature patients operated on for supracondylar humeral fractures through an anterior approach. The primary outcome was results according to Flynn's score (Table 1), which stands out as the dominant system in the literature for assessing outcomes in treating SHFs in children.12 The secondary outcomes were postoperative complications. The exclusion criteria encompassed patients above 12 years of age, mini-open approaches, delayed presentation of more than 7 days, and studies lacking full-text availability. We excluded patients older than 12 years due to concerns related to bone maturity, which can impact the ability to manipulate and reduce the fracture and consequently, the indication for an open approach.
We reviewed studies of evidence levels I–IV (case reports, case series, cohort, case–control studies, and RCTs) that reported on the anterior approach for ORIF of pediatric SHF. Studies from across the world in any operative setting were accepted. We excluded systematic reviews, meta-analyses, literature reviews, technical reports, book chapters, meeting and conference abstracts, and non-human studies. Studies with overlapping data were managed by selecting only one of the studies, prioritizing the one with a higher level of evidence and a lower risk of bias.
Search strategyThe search, conducted in December 2023, covered MEDLINE/PubMed, Embase, Web of Science, Clinicaltrials.gov, and Cochrane Library databases. The strategy involved the terms: “Supracondylar humer*”, “Gartland”, “Children”, “Pediatric”, “open reduction”, “approach”. No publication date restrictions were applied. Eligibility was limited to articles written in the Latin alphabet. The search strategy details can be found here: https://www.crd.york.ac.uk/PROSPEROFILES/446923_STRATEGY_20230719.pdf.
Study selectionThe systematic review software Covidence® (Veritas Health Innovation, Melbourne, Australia) facilitated reference import and duplicate removal. Two independent reviewers (DGM and FBC) screened the references by title, abstract and full-text. Articles not meeting inclusion criteria or lacking accessible abstracts/full-texts were excluded following manual searches across databases, journals, and Google Scholar. Discrepancies were resolved by a senior third reviewer (FS).
Data collectionTwo independent reviewers (UJA and JMMP) collected data including author and publication year, country, study design, patient or mean age, Gartland classification, indication for open reduction, follow-up duration, Flynn's cosmetic and functional score (satisfactory or unsatisfactory), and complications including iatrogenic neurovascular injury, reoperation rate, scar quality, infection, cubitus varus, loss of range of motion. Unsatisfactory results based on Flynn's criteria were considered complications. Loss of range of motion, not reported as Flynn's score, was converted to Flynn's score, considering the 15° threshold for defining satisfactory or unsatisfactory outcomes. Cubitus varus was considered an unsatisfactory Flynn's cosmetic score. Discrepancies were resolved by a senior third reviewer (FS).
Risk of bias analysisWe employed the “Methodological Index for Non-Randomized Studies (MINORS)”. This assessment involved two independent reviewers (DGM and FBC), with disagreements resolved by a third reviewer (FS).
Outcomes measures and statistical analysisCategorical variables were summarized using counts and percentages, and continuous variables with means and standard deviations or medians and ranges, as appropriate. IBM SPSS Statistics, Version 25.0 facilitated statistical analysis. No meta-analysis was performed due to low study quality and heterogeneous outcomes.
ResultsStudy selectionThe initial search found 1151 studies. 635 studies duplicates were removed and 19 met inclusion/exclusion criteria (Fig. 1).1,8,9,13–28 One study was excluded due to overlapping data.29 Excluded studies from eligibility assessment are shown in Appendix 1.
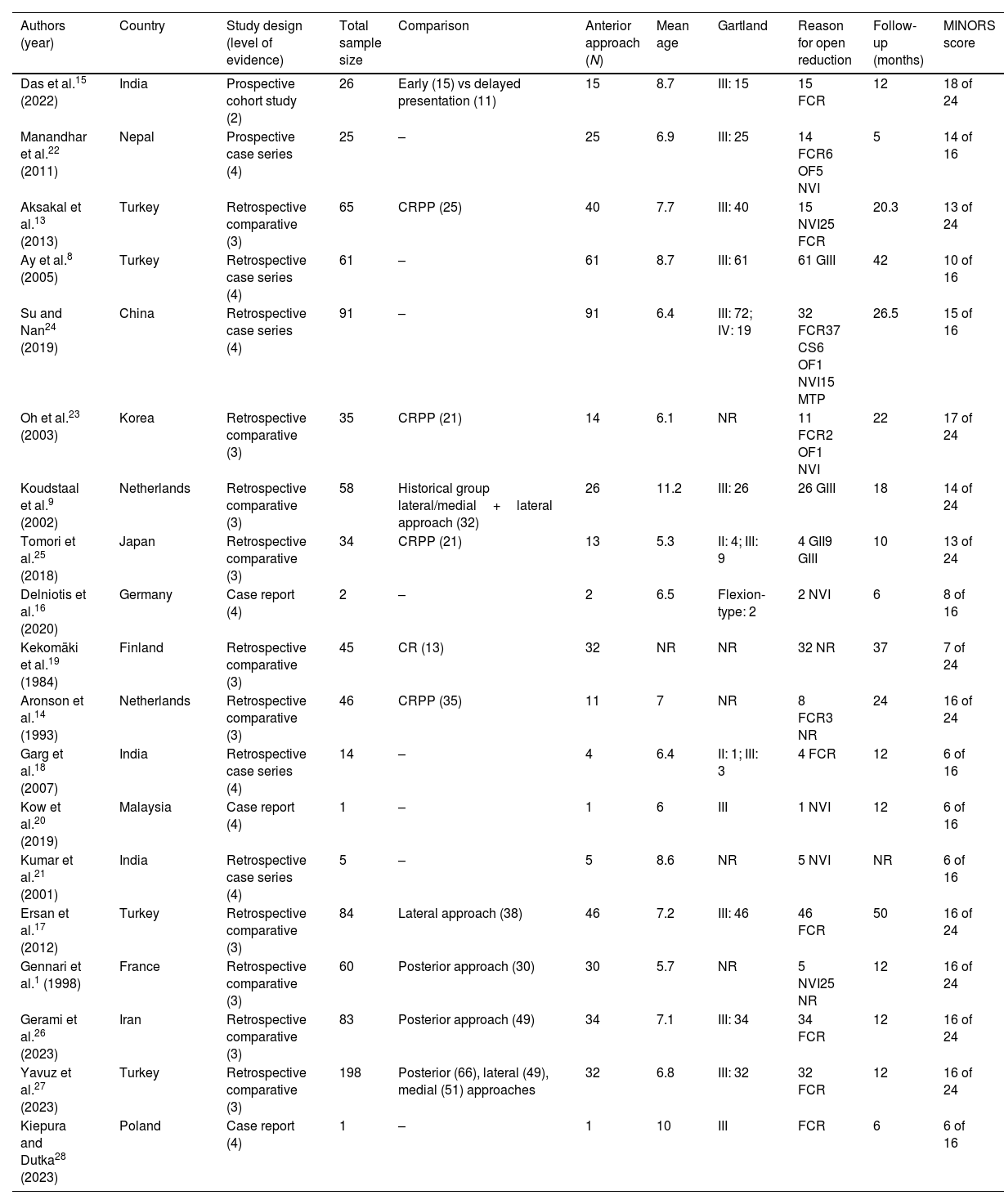
Study qualityOne study was of Level 2 evidence, 10 were of Level 3, and 8 were of Level 4. The mean MINORS score was 13.05±3.47 (6–19), which indicated a relatively poor quality of evidence (Table 2 and Appendix 2).
Study demographics and characteristics.
| Authors (year) | Country | Study design (level of evidence) | Total sample size | Comparison | Anterior approach (N) | Mean age | Gartland | Reason for open reduction | Follow-up (months) | MINORS score |
|---|---|---|---|---|---|---|---|---|---|---|
| Das et al.15 (2022) | India | Prospective cohort study (2) | 26 | Early (15) vs delayed presentation (11) | 15 | 8.7 | III: 15 | 15 FCR | 12 | 18 of 24 |
| Manandhar et al.22 (2011) | Nepal | Prospective case series (4) | 25 | – | 25 | 6.9 | III: 25 | 14 FCR6 OF5 NVI | 5 | 14 of 16 |
| Aksakal et al.13 (2013) | Turkey | Retrospective comparative (3) | 65 | CRPP (25) | 40 | 7.7 | III: 40 | 15 NVI25 FCR | 20.3 | 13 of 24 |
| Ay et al.8 (2005) | Turkey | Retrospective case series (4) | 61 | – | 61 | 8.7 | III: 61 | 61 GIII | 42 | 10 of 16 |
| Su and Nan24 (2019) | China | Retrospective case series (4) | 91 | – | 91 | 6.4 | III: 72; IV: 19 | 32 FCR37 CS6 OF1 NVI15 MTP | 26.5 | 15 of 16 |
| Oh et al.23 (2003) | Korea | Retrospective comparative (3) | 35 | CRPP (21) | 14 | 6.1 | NR | 11 FCR2 OF1 NVI | 22 | 17 of 24 |
| Koudstaal et al.9 (2002) | Netherlands | Retrospective comparative (3) | 58 | Historical group lateral/medial+lateral approach (32) | 26 | 11.2 | III: 26 | 26 GIII | 18 | 14 of 24 |
| Tomori et al.25 (2018) | Japan | Retrospective comparative (3) | 34 | CRPP (21) | 13 | 5.3 | II: 4; III: 9 | 4 GII9 GIII | 10 | 13 of 24 |
| Delniotis et al.16 (2020) | Germany | Case report (4) | 2 | – | 2 | 6.5 | Flexion-type: 2 | 2 NVI | 6 | 8 of 16 |
| Kekomäki et al.19 (1984) | Finland | Retrospective comparative (3) | 45 | CR (13) | 32 | NR | NR | 32 NR | 37 | 7 of 24 |
| Aronson et al.14 (1993) | Netherlands | Retrospective comparative (3) | 46 | CRPP (35) | 11 | 7 | NR | 8 FCR3 NR | 24 | 16 of 24 |
| Garg et al.18 (2007) | India | Retrospective case series (4) | 14 | – | 4 | 6.4 | II: 1; III: 3 | 4 FCR | 12 | 6 of 16 |
| Kow et al.20 (2019) | Malaysia | Case report (4) | 1 | – | 1 | 6 | III | 1 NVI | 12 | 6 of 16 |
| Kumar et al.21 (2001) | India | Retrospective case series (4) | 5 | – | 5 | 8.6 | NR | 5 NVI | NR | 6 of 16 |
| Ersan et al.17 (2012) | Turkey | Retrospective comparative (3) | 84 | Lateral approach (38) | 46 | 7.2 | III: 46 | 46 FCR | 50 | 16 of 24 |
| Gennari et al.1 (1998) | France | Retrospective comparative (3) | 60 | Posterior approach (30) | 30 | 5.7 | NR | 5 NVI25 NR | 12 | 16 of 24 |
| Gerami et al.26 (2023) | Iran | Retrospective comparative (3) | 83 | Posterior approach (49) | 34 | 7.1 | III: 34 | 34 FCR | 12 | 16 of 24 |
| Yavuz et al.27 (2023) | Turkey | Retrospective comparative (3) | 198 | Posterior (66), lateral (49), medial (51) approaches | 32 | 6.8 | III: 32 | 32 FCR | 12 | 16 of 24 |
| Kiepura and Dutka28 (2023) | Poland | Case report (4) | 1 | – | 1 | 10 | III | FCR | 6 | 6 of 16 |
MINORS: Methodological Index for Non-Randomized Studies; CR: close reduction; CRPP: close reduction and percutaneous pinning; NR: not reported; FCR: failed closed reduction; DP: delayed presentation; OF: open fracture; NVI: neurovascular injury; G: Gartland; CS: compartmental syndrome; MTP: multiple trauma patients.
The included studies were conducted between 1984 and 2023 in 14 different countries (Table 2).
Overall, 483 patients underwent an anterior approach for ORIF of SHF across the included studies. The patient's median age of included studies was 7 (5.3–11.2). Fractures were classified according to Gartland classification in 16 studies: 5 fractures were (1%) Gartland II fracture, 365 (75.6%) Gartland III, 19 (3.9%) Gartland IV and 2 (0.4%) flexion-type SHF and 92 (19%) unknowns (Table 2).
A failed closed reduction was the reason for open reduction in 222 (46%) patients.13,17,18,22–24,26–29 Open fracture specifically indicated an open approach in 14 (2.9%) patients.23,24 Neurovascular injuries prompted an anterior approach in 35 (7.2%) patients.1,13,16,20–22,24 Compartment syndrome was cited as a cause for open reduction in 37 (7.7%) patients.24 One article mentioned “multiple trauma” as the reason for open reduction in a series of 15 patients (3.1%).24 Three studies found the fracture pattern (Gartland II and III) motivated open reduction in 100 patients (20.7%).8,9,25 In three studies,1,14,19 the motivating reason for open reduction was incompletely reported for 60 (12.4%) patients. The mean patient follow-up was 18.5±8.2 months. Baseline characteristics and demographics are shown in Table 2.
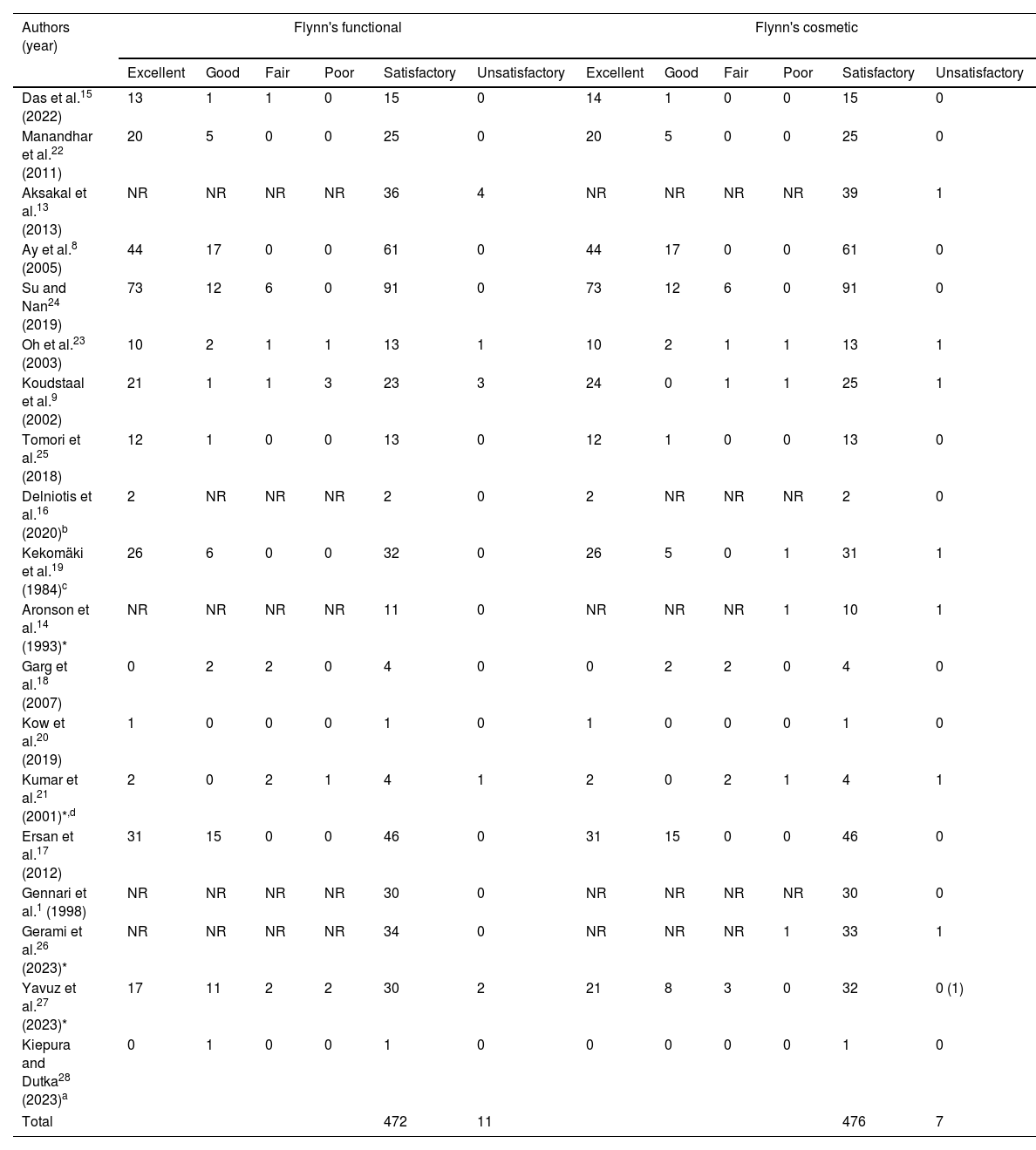
Functional and cosmetic resultsUsing Flynn's functional criteria, 472/483 (97.7%) patients achieved a satisfactory result, while 11/483 (2.3%) did not. For cosmetic criteria, 476/483 (98.6%) were satisfied, and 10/483 (1.4%) were not. Refer to Table 3.
Functional and cosmetic results according to Flynn's criteria.
| Authors (year) | Flynn's functional | Flynn's cosmetic | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Excellent | Good | Fair | Poor | Satisfactory | Unsatisfactory | Excellent | Good | Fair | Poor | Satisfactory | Unsatisfactory | |
| Das et al.15 (2022) | 13 | 1 | 1 | 0 | 15 | 0 | 14 | 1 | 0 | 0 | 15 | 0 |
| Manandhar et al.22 (2011) | 20 | 5 | 0 | 0 | 25 | 0 | 20 | 5 | 0 | 0 | 25 | 0 |
| Aksakal et al.13 (2013) | NR | NR | NR | NR | 36 | 4 | NR | NR | NR | NR | 39 | 1 |
| Ay et al.8 (2005) | 44 | 17 | 0 | 0 | 61 | 0 | 44 | 17 | 0 | 0 | 61 | 0 |
| Su and Nan24 (2019) | 73 | 12 | 6 | 0 | 91 | 0 | 73 | 12 | 6 | 0 | 91 | 0 |
| Oh et al.23 (2003) | 10 | 2 | 1 | 1 | 13 | 1 | 10 | 2 | 1 | 1 | 13 | 1 |
| Koudstaal et al.9 (2002) | 21 | 1 | 1 | 3 | 23 | 3 | 24 | 0 | 1 | 1 | 25 | 1 |
| Tomori et al.25 (2018) | 12 | 1 | 0 | 0 | 13 | 0 | 12 | 1 | 0 | 0 | 13 | 0 |
| Delniotis et al.16 (2020)b | 2 | NR | NR | NR | 2 | 0 | 2 | NR | NR | NR | 2 | 0 |
| Kekomäki et al.19 (1984)c | 26 | 6 | 0 | 0 | 32 | 0 | 26 | 5 | 0 | 1 | 31 | 1 |
| Aronson et al.14 (1993)* | NR | NR | NR | NR | 11 | 0 | NR | NR | NR | 1 | 10 | 1 |
| Garg et al.18 (2007) | 0 | 2 | 2 | 0 | 4 | 0 | 0 | 2 | 2 | 0 | 4 | 0 |
| Kow et al.20 (2019) | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 |
| Kumar et al.21 (2001)*,d | 2 | 0 | 2 | 1 | 4 | 1 | 2 | 0 | 2 | 1 | 4 | 1 |
| Ersan et al.17 (2012) | 31 | 15 | 0 | 0 | 46 | 0 | 31 | 15 | 0 | 0 | 46 | 0 |
| Gennari et al.1 (1998) | NR | NR | NR | NR | 30 | 0 | NR | NR | NR | NR | 30 | 0 |
| Gerami et al.26 (2023)* | NR | NR | NR | NR | 34 | 0 | NR | NR | NR | 1 | 33 | 1 |
| Yavuz et al.27 (2023)* | 17 | 11 | 2 | 2 | 30 | 2 | 21 | 8 | 3 | 0 | 32 | 0 (1) |
| Kiepura and Dutka28 (2023)a | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| Total | 472 | 11 | 476 | 7 | ||||||||
A total of 46 complications (9.5%) were reported. Eleven presented a restriction in the ROM (2.3%). Cubitus varus was reported in 8 patients (1.7%). Seven patients (1.4%) experienced postsurgical neurovascular injuries: 4 (0.8%) ulnar nerve, 2 (0.4%) anterior interosseous nerve, and 1 cephalic vein injury. Fifteen (2.9%) reported pin tract and wound infections, all treated with antibiotics and pin removal. Three patients (0.6%) had a hypertrophic scar and two patients presented cubitus valgus (0.4%). One patient required reoperation: fracture displacement with dorsal tilting of distal humerus fragment. Further details are available in an Appendix 3.
DiscussionThis investigation was conducted to provide a comprehensive overview and analysis of the postoperative outcomes and complications of the anterior approach for the treatment of SHF in children. The strengths of this study include its rigorous methodology and broad search, which resulted in the inclusion of 19 articles encompassing 483 patients. The most significant finding of the study was that 97.7% and 98.6% of patients achieved a satisfactory functional and cosmetic result according to Flynn's criteria, respectively; with a reoperation rate of less than 1%.
Previous studies have demonstrated that Gartland III fractures and delayed presentations are associated with failed closed reductions, necessitating open reduction.7,30 Delayed presentation of more than 7 days has been associated with the inability to achieve a satisfactory closed reduction, even in Gartland II fractures.31 1iculty is likely due to callus formation and advanced healing tissue, potentially leading to poorer outcomes and complications. Consequently, studies including fractures treated beyond this timeframe were excluded.15,32 Remarkably, the rationale for open reduction has not been documented in previous systematic reviews on pediatric SHF.10,11 In the systematic review by Pretell Mazzini et al.,11 although they noted the absence of statistically significant differences in the incidence of neurovascular injuries across various surgical approaches, they did not provide insight into the specific motivations for opting for an open approach. In our review, neurovascular injuries were the driving factor behind 6.7% of cases involving the anterior open approach, similar to the 5–20% rate reported in the literature.33,34 An important observation from our systematic review is that the rationale for adopting the open approach was compartment syndrome in 7% of patients, a considerably higher rate than the 0.1–0.3% reported incidence of compartment syndrome in SHF.35 We believe that this is related to the proper exposure of arteries and nerves that the approach offers and its versatility in extending it for the effective treatment of compartment syndrome, addressing one of the most significant complications associated with these fractures.36
SHFs surgically treated by CRPP have demonstrated excellent outcomes.37–39 While this method is preferred over open reduction, a recent systematic review and meta-analysis has shown that, when open reduction is necessary, both CRPP and open reduction have comparable functional and cosmetic results in the treatment of SHF.4 A systematic review and meta-analysis by Irianto et al.,10 comparing lateral and posterior approaches outcomes demonstrated a functional satisfaction rate of 98% for the lateral approach and 94% for the posterior approach, along with a 99% cosmetic satisfaction rate for both. To our knowledge, no meta-analysis and only one systematic review have reported the use of the anterior approach to treat SHF. The systematic review conducted by Pretell Mazzini et al.11 assessed all approaches, including the anterior, for treating SHF. Although the anterior approach yielded good results, the limited number of articles included was a significant limitation in interpreting these findings.8,21 Our review revealed a high satisfaction rate in both functional and cosmetic outcomes using the anterior approach, with an overall functional satisfaction rate of 98% and a cosmetic satisfaction rate of 99% according to the widely used Flynn's score.10,40
The most common complications following SHF are infection, cubitus varus and neurovascular injuries.41 We found an overall complication rate of 9.5%. It is worth noting that we included an unsatisfactory Flynn score as a complication, which might have contributed to the elevated rate. In the literature, pin site infection rates range between 2 and 10%, aligning with the 2.9% rate found in our review. Most cases are effectively managed with oral antibiotics and local wound care.42 Similar rates were reported for other approaches in the systematic review by Pretell Mazzini et al.11 Interestingly, a 9.5% rate of pin tract infection was observed in the open medial approach, compared to only 2% for the lateral approach. The reason for this discrepancy remains unclear. Only 0.6% of patients developed hypertrophic scars. While no systematic reviews directly compared the rates of this cosmetic complication across approaches, the incidence for the anterior approach is likely significantly lower than for the posterior or lateral approaches.43
Nerve injury is one of the primary concerns when surgically addressing SHF.44–46 Neurovascular injuries were infrequent, with only seven cases of postsurgical nerve injuries reported and no instances of arterial injuries. However neural injuries might not be solely attributed to the approach itself but could also be linked to preoperative conditions or the pinning process. A systematic review on the preferred pinning methods showed that the probability of iatrogenic nerve injury and ulnar nerve injury was 1.84 and 5.04 times higher, respectively, with medial/lateral entry pins than with isolated lateral entry pins.38 The iatrogenic nerve injury rate of less than 1% achieved with lateral entry CRPP presented in that systematic review is comparable to what is presented in our work. Consistent with our findings, Pretell Mazzini et al.11 found higher rates of iatrogenic nerve injuries in the lateral and posterior approaches compared to the anterior approach. This highlights the importance of directly identifying neurovascular structures to reduce the risk of iatrogenic neurovascular injuries when performing an open approach for the treatment of SHF.
Despite its rigorous methodology, broad search, and high number of patients included this review is subject to several limitations. First, the studies encompassed in this systematic review were predominantly characterized by low-level evidence, wherein 94% of the included studies were classified as Level 3 and 4 evidence. Second, there exists the potential for language and publication bias given that only publications in the Latin alphabet were included. Third, performing a more extensive statistical analysis involving variables such as Gartland-type or the indication for open reduction, which could have enhanced the study's quality, was not feasible due to the absence of individual data in the analyzed articles. Fourthly, the heterogeneity in the indications and the reports of outcomes among the studies could have influenced the results. Furthermore, the variability in follow-up duration introduces heterogeneity to the results. Three studies with follow-up periods of less than a year may have underestimated complication and reoperation rates. Fifthly, the absence of comparative studies rendered the conduct of a meta-analysis unfeasible. Lastly, more than half of the studies were published in Asia, encompassing developing countries, which is unusual in the orthopedic literature.47 This factor can influence the results, as the hospital setting might have lacked fluoroscopy or C-arm for assessing the quality of reduction, consequently compromising the reduction quality. Additionally, most studies conducted in Europe were reported more than 20 years ago, contributing to heterogeneity. However, we believe that this adds value to the present study, as it enables the results to have global reach and applicability, irrespective of hospital or health system resources.
To the best of our knowledge, this was the first systematic review on the anterior approach for SHFs. This study provided nuance on the indications, clinical outcomes, and complications associated with this approach. If an open approach is required, we recommend utilizing the anterior approach due to its ability to directly visualize the fracture site, facilitating precise reduction and fixation. Furthermore, this approach allows for visualization of the anterior neurovascular bundle, enabling its identification and protection from potential damage or repair when injured (Fig. 2). Future prospective multicenter comparative studies comparing the anterior and other approaches are essential to determine the best open approach. A meta-analysis or network meta-analysis comparing all approaches would provide even deeper insights. Given the prevalence of this fracture and the relative infrequency of ORIF, national registries dedicated to SHFs can offer valuable data for future research.
In conclusion, our systematic review shows that the anterior approach for managing pediatric SHF requiring open reduction offers high rates of both satisfactory functional and cosmetic outcomes, with minimal risk of neurovascular injuries and low reintervention rates.
Level of evidenceLevel of evidence IV.
Ethical approvalThe authors declare that no ethical considerations are applicable in this article. The authors declare that no ethical conflicts exist in regards to the production of this study.
Author's contributionsAll authors contributed to the study's conception and design. Search strategy and statistical analysis were performed by SE. Study selection and bias analysis were performed by DGM, FBC. Data collection was performed by JMMP, UJA, YLT. Discrepancies and conflicts and methodology confection were performed by FS, MP. The first draft of the manuscript was written by DGM. Supervision and guidance were performed by EGF. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Conflict of interestThe authors declare that they have no relevant financial or non-financial interests to report.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of generative AI and AI-assisted technologies in the writing processWe declare that no generative AI or AI-assisted technologies have been used during the writing process.