A meta-analysis was carried out to evaluate the clinical–functional results of anterior cruciate ligament surgery in military population, as well as the complications associated with it.
Material and methodThree major database sources up to December 2022 (PubMed, Google Scholar, and ScienceDirect) were searched for outcomes after anterior cruciate ligament surgery in military personnel. The systematic review was carried out following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses –PRISMA– standards, and the inclusion criteria following the PICO strategy. Data from included studies were analysed using Review Manager 5.4 software.
ResultsA total of seven retrospective studies were selected. The general rate of return to full duty in military personnel was 62.3% (61.5% for the non-officer group versus 68.3% for the officer group) without this difference being significant (p=0.92). The general rate of meniscal injury in the military was 58.8%, without this difference being significant (p=0.88). The homogeneity in both cases was good (I2=0%, p=0.99).
ConclusionReturn to full military duty can be used in the military population as a marker of success after anterior cruciate ligament reconstruction. It should be noted that a large number of military personnel experience permanent activity limitations that prevent full return to service.
Se realizó un metaanálisis para evaluar los resultados clínico-funcionales de la cirugía de ligamento cruzado anterior en militares, así como las complicaciones asociadas a la misma.
Material y métodosSe realizó una búsqueda en las 3 principales fuentes de bases de datos hasta diciembre de 2022 (PubMed, Google Scholar y ScienceDirect) en cuanto a los resultados tras la cirugía del ligamento cruzado anterior en personal militar. La revisión sistemática se realizó siguiendo las normas Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA), y los criterios de inclusión siguieron la estrategia PICO. Los datos de los estudios incluidos se analizaron mediante el software Review Manager 5.4.
ResultadosSe seleccionaron un total de 7 estudios retrospectivos. La tasa general de retorno a la actividad completa en el personal militar fue del 62,3% (61,5% para el grupo de no oficiales frente al 68,3% para el grupo de oficiales), sin ser esta diferencia significativa (p=0,92). La tasa general de lesión meniscal en los militares fue del 58,8%, sin ser esta diferencia significativa (p=0,88). La homogeneidad en ambos casos fue buena (I2=0%; p=0,99).
ConclusiónEl regreso a la actividad militar completa puede usarse en la población militar como un marcador de éxito después de una reconstrucción del ligamento cruzado anterior. Hay que destacar que una gran cantidad de militares experimentan limitaciones permanentes en la actividad, que impiden el regreso completo al servicio.
The demands of training and exercise performed in the armed forces, as well as during combat manoeuvres or military service, may be an added risk factor, among many others, for anterior cruciate ligament (ACL) rupture that may predispose to poorer outcomes and a higher incidence of associated complications, such as joint degeneration and/or meniscal injury.1
Approximately 22% of all musculoskeletal injuries indicative of surgical treatment occurring in military personnel are located in the knee.2 Several studies have determined that the incidence of ACL injuries among the general population is .3 to .68 cases per 1000 persons-year.3 When compared to the military population, other authors report an incidence 10 times higher, i.e., between 2.96 and 3.65 cases per 1000 persons-years.4
Consequently, multiple joint injury prevention training programmes have been developed to improve the biomechanics of the lower extremities of military personnel with the aim of decreasing the incidence of injuries.5 Furthermore, although the short-term results of ACL surgery are good, there is particular concern among the military population that the post-traumatic effects of cartilage at the time of ACL injury will lead to a high degree of post-traumatic osteoarthritis requiring eventual treatment.6 it is of note that soldiers, and specifically those who serve in combat arms and who are not high commanders like officers, must perform aggressive impacts, run daily distances and carry heavy weights every day. The risk of knee injuries is high among servicemen and lower in officers, who do not perform these physical practices on a daily basis, so it is of scientific interest to investigate whether there are differences in the return to full duty (RTFD) after ACL reconstruction. Therefore, and given that there is no meta-analysis in the literature at present, it is of scientific interest to find out whether there are differences in the RTFD between the two groups, whose physical demands and military performance are different prior to the injury, and may be more compromised in the case of non-officer military personnel.7
For this reason, a systematic review and meta-analysis was performed to evaluate the clinical–functional results in terms of the RTFD of ACL surgery in military personnel.
Material and methodsEligibility criterionA systematic review of the literature was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses –PRISMA–8 guidelines. Inclusion criteria followed the PICO9 strategy. Inclusion criteria were applied to all studies (prospective and retrospective) in which the clinical–functional outcomes of primary ACL surgery in military personnel were quantitatively assessed in at least one questionnaire, providing reliable information on the RTFD. We therefore excluded studies that only analysed the incidence of this injury, those evaluating risk factors associated with ACL rupture, studies of conservatively treated ACL ruptures, survival analysis of the plasty used or studies of ACL revision surgery. Studies that were not of the type of research described, i.e., systematic reviews, meta-analyses, book chapters, narrative reviews, review articles, description of techniques, letters to the editors, expert opinion, animal research or in vitro studies were excluded. Articles in a language other than English or Spanish were not evaluated. Related articles involving the same patients were not considered.
Search strategyThe three main online database sources were used: PubMed/MEDLINE, Google Scholar and ScienceDirect. The databases were searched for outcomes after ACL surgery in military personnel up to December 2022. Data were extracted uniformly and compiled in Microsoft Excel 2019, version 16.54.
The search equation used in PubMed was: ((anterior cruciate ligament) OR (ACL)) AND (military); for Google Scholar: (anterior cruciate ligament) AND (military); and for ScienceDirect: (military) AND (anterior cruciate ligament OR ACL) treatment.
Articles were included in both English and Spanish, excluding those in another language. We did not limit by year of publication or level of evidence. The bibliographic references of the selected articles were also analysed in order to rescue other studies that could potentially be included in the review. These studies were located through PubMed and Google Scholar.
Data extractionThe data collected included the type of study involved (retrospective/prospective, case series, cohort), sex, mean age, number of patients included in each study, mean follow-up in years, ACL reconstruction surgical technique used (bone-patellar tendon-bone (BTB), hamstring, iliotibial band tenodesis, allograft), military grade (officer/non-officer), which significantly differentiates the degree of military physical activity and demand, the country of origin of the military corps, the mechanism of action of the ligament rupture (sports accident, traffic accident, combat accident, other), the percentage of the military with RTFD without any restriction, the rate of associated meniscal injury and the rate of chondropathy or chondral damage associated with ACL rupture.
Risk of bias assessmentThe assessment of the methodological quality of the included studies was based on the criteria of the methodological index for non-randomized studies –MINORS–10 for risk of bias in retrospective studies. It involves 8 items for non-comparative studies and 12 items for comparative studies. The 12 domains used to assess bias in each study included: clearly stated objective, inclusion of consecutive patients, prospective data collection, conclusions appropriate to the study objective, unbiased assessment of the study, adequate follow-up period, loss to follow-up less than 5%, prospective study size calculation, adequate control group, contemporaneous groups, groups with equivalent objectives in terms of outcomes, and adequate statistical analyses (the latter 4 only present in comparative studies). Items were classified as not present in the study (0), existing but inadequate1 or clearly existing in the study.2 If the maximum item score was 2, the ideal overall score would be 16 for non-comparative studies and 24 for comparative studies. The included studies were assessed independently by two investigators and differences of opinion between them were resolved by discussion and consultation with a third author.
Statistical analysis of the dataData from included studies were analysed using Review Manager 5.4 software (RevMan Cochrane® 2023). Dichotomous variables were expressed as risk ratio and 95% confidence interval. Q-tests and I2 tests were used to estimate between-study heterogeneity. When I2<50% or p>.1, a fixed-effects model was applied for meta-analysis; and when I2>50% or p<.1, a random-effects model was used. For all outcome measures, forest plot and funnel plot were used to present the results of individual studies.
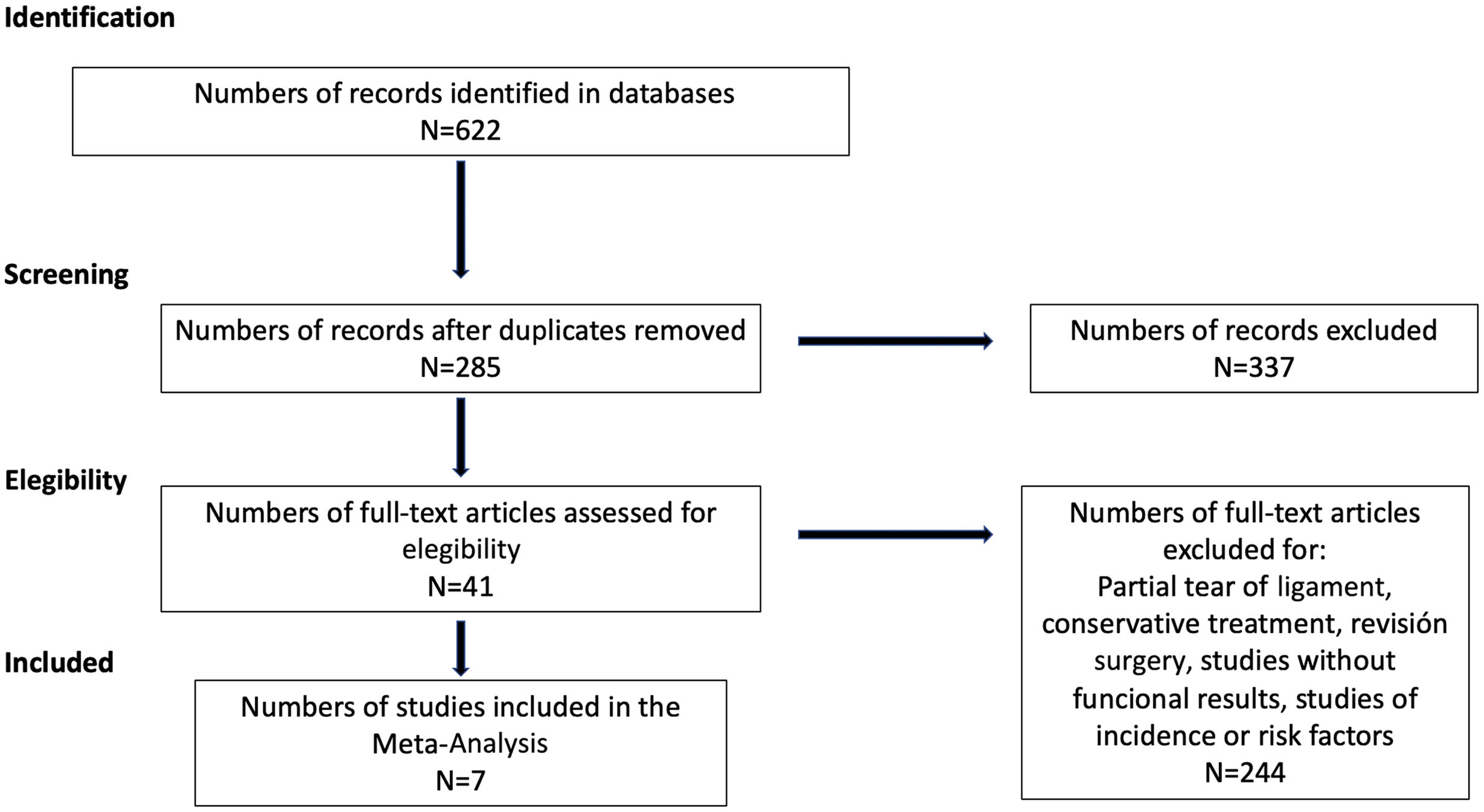
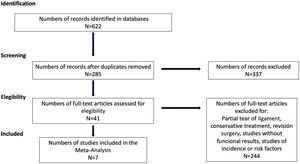
ResultsSearch findingsA literature search was conducted and 622 published articles were located; after excluding duplicate articles, 285 articles were collected. After reviewing titles and abstracts, we were left with 41 studies that met our inclusion criteria, excluding 244 articles as they were studies corresponding to literature reviews, prevalence studies, studies on associated risk factors or studies in which clinical outcomes were not included. After a thorough and detailed review of the remaining studies, in order to decide whether or not the information they contained was related to our objective, 34 studies were excluded as they were partial ruptures, studies on conservative treatment or studies on ACL revisions. In the end, a total of seven studies were selected for this systematic review and meta-analysis. The process of article selection is shown in Fig. 1.
Study characteristicsWe considered as outcomes the return to full or unrestricted return to military duty (RTFD), and the rate of meniscal lesions and chondropathy associated with ligament rupture. Surgical repair was performed arthroscopically in all included studies, using BTB plasty in four studies,7,11–13 hamstring plasty in four studies,7,13–15 extra-articular plasty with iliotibial web tenodesis in one study11 and allograft in another study.7 In one study16 the surgical technique performed on patients was not detailed.
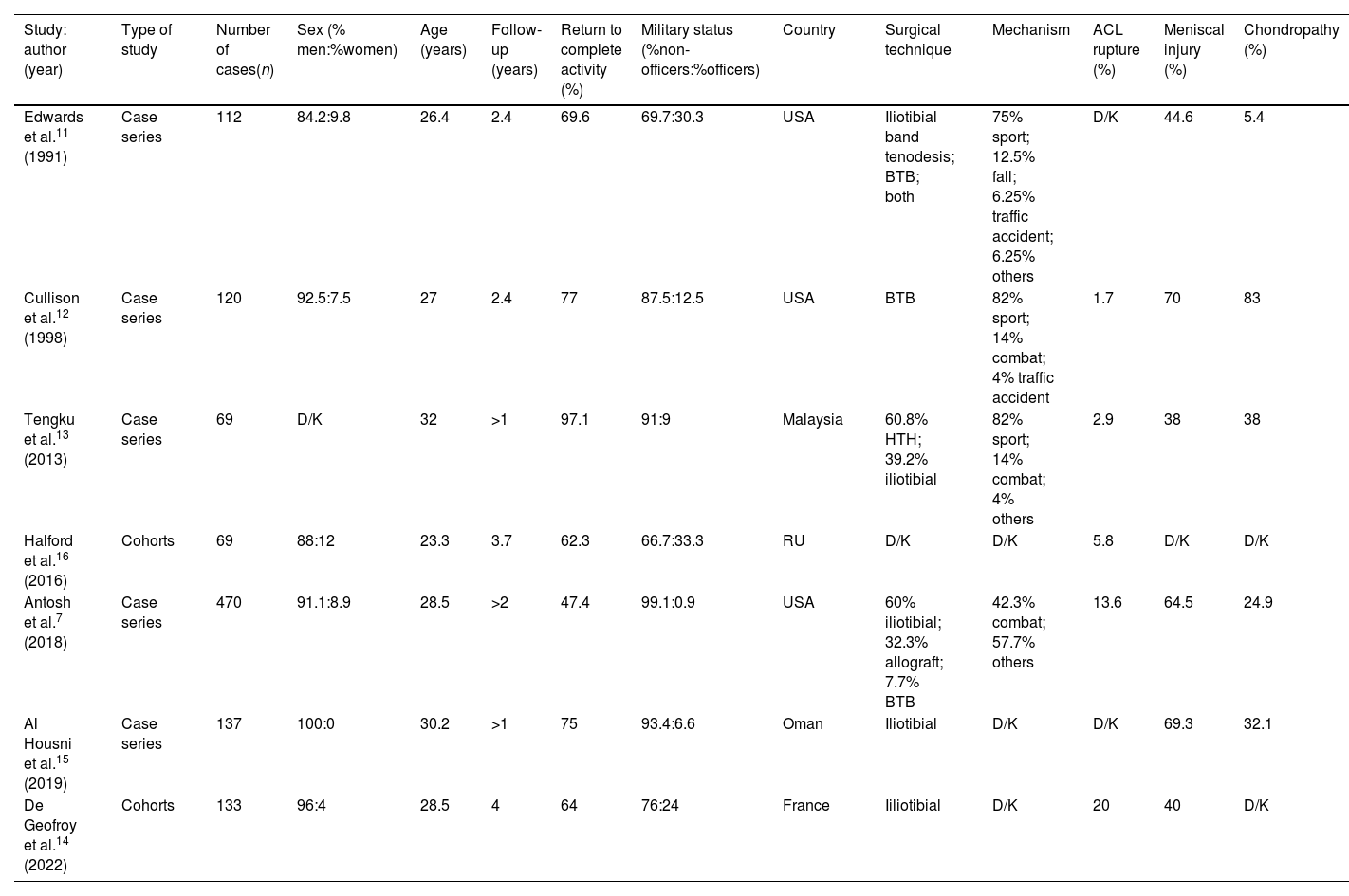
All included studies were published between 1991 and 2023 and included 1110 patients (987 non-officers and 123 officers). All studies used MRI as a complementary test for diagnosis, associated with a physical examination indicative of rupture. The main characteristics of the included studies are summarised in Table 1.
Characteristics of the studies included.
| Study: author (year) | Type of study | Number of cases(n) | Sex (% men:%women) | Age (years) | Follow-up (years) | Return to complete activity (%) | Military status (%non-officers:%officers) | Country | Surgical technique | Mechanism | ACL rupture (%) | Meniscal injury (%) | Chondropathy (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Edwards et al.11 (1991) | Case series | 112 | 84.2:9.8 | 26.4 | 2.4 | 69.6 | 69.7:30.3 | USA | Iliotibial band tenodesis; BTB; both | 75% sport; 12.5% fall; 6.25% traffic accident; 6.25% others | D/K | 44.6 | 5.4 |
| Cullison et al.12 (1998) | Case series | 120 | 92.5:7.5 | 27 | 2.4 | 77 | 87.5:12.5 | USA | BTB | 82% sport; 14% combat; 4% traffic accident | 1.7 | 70 | 83 |
| Tengku et al.13 (2013) | Case series | 69 | D/K | 32 | >1 | 97.1 | 91:9 | Malaysia | 60.8% HTH; 39.2% iliotibial | 82% sport; 14% combat; 4% others | 2.9 | 38 | 38 |
| Halford et al.16 (2016) | Cohorts | 69 | 88:12 | 23.3 | 3.7 | 62.3 | 66.7:33.3 | RU | D/K | D/K | 5.8 | D/K | D/K |
| Antosh et al.7 (2018) | Case series | 470 | 91.1:8.9 | 28.5 | >2 | 47.4 | 99.1:0.9 | USA | 60% iliotibial; 32.3% allograft; 7.7% BTB | 42.3% combat; 57.7% others | 13.6 | 64.5 | 24.9 |
| Al Housni et al.15 (2019) | Case series | 137 | 100:0 | 30.2 | >1 | 75 | 93.4:6.6 | Oman | Iliotibial | D/K | D/K | 69.3 | 32.1 |
| De Geofroy et al.14 (2022) | Cohorts | 133 | 96:4 | 28.5 | 4 | 64 | 76:24 | France | Iiliotibial | D/K | 20 | 40 | D/K |
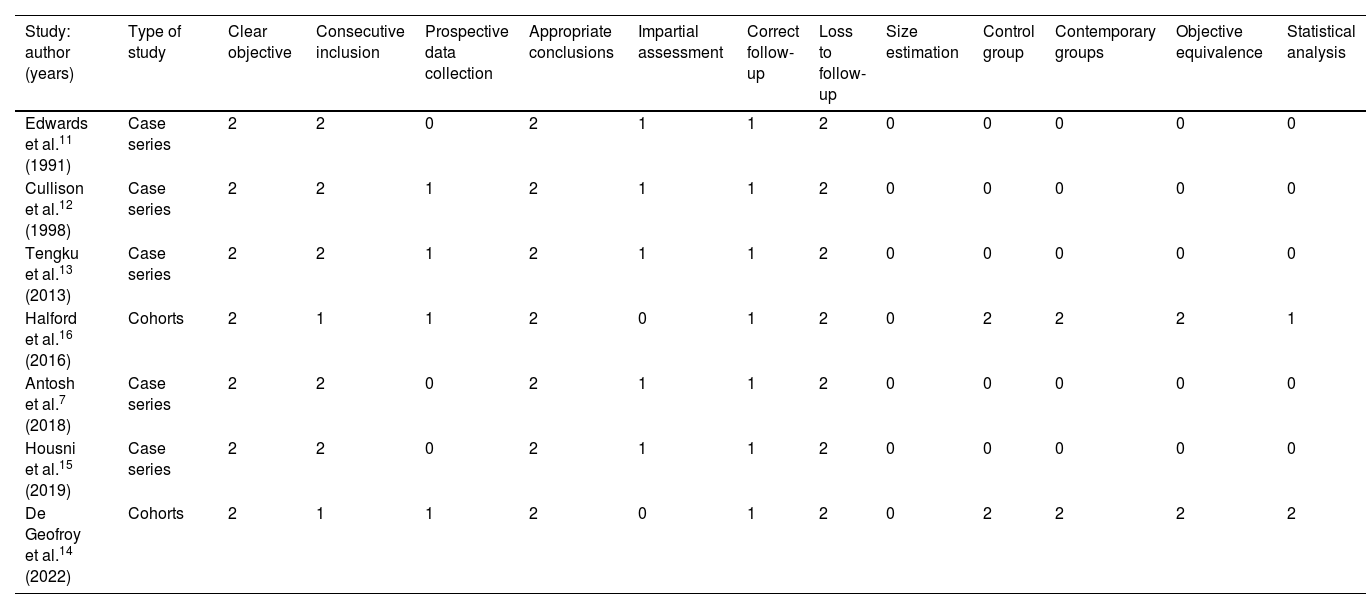
The assessment of the methodological quality of the included studies was based on the MINORS criteria described above. The risk of bias in each study is illustrated in Table 2.
Risk of bias table: reviewers’ judgments on each risk of bias item presented as scores in all included studies.
| Study: author (years) | Type of study | Clear objective | Consecutive inclusion | Prospective data collection | Appropriate conclusions | Impartial assessment | Correct follow-up | Loss to follow-up | Size estimation | Control group | Contemporary groups | Objective equivalence | Statistical analysis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Edwards et al.11 (1991) | Case series | 2 | 2 | 0 | 2 | 1 | 1 | 2 | 0 | 0 | 0 | 0 | 0 |
| Cullison et al.12 (1998) | Case series | 2 | 2 | 1 | 2 | 1 | 1 | 2 | 0 | 0 | 0 | 0 | 0 |
| Tengku et al.13 (2013) | Case series | 2 | 2 | 1 | 2 | 1 | 1 | 2 | 0 | 0 | 0 | 0 | 0 |
| Halford et al.16 (2016) | Cohorts | 2 | 1 | 1 | 2 | 0 | 1 | 2 | 0 | 2 | 2 | 2 | 1 |
| Antosh et al.7 (2018) | Case series | 2 | 2 | 0 | 2 | 1 | 1 | 2 | 0 | 0 | 0 | 0 | 0 |
| Housni et al.15 (2019) | Case series | 2 | 2 | 0 | 2 | 1 | 1 | 2 | 0 | 0 | 0 | 0 | 0 |
| De Geofroy et al.14 (2022) | Cohorts | 2 | 1 | 1 | 2 | 0 | 1 | 2 | 0 | 2 | 2 | 2 | 2 |
Of the five non-comparative retrospective case series studies, we scored 10 points for all studies, as sample size calculation was missing and follow-up was inadequate in all series. For the two comparative studies, we scored 16 and 17 points, respectively.
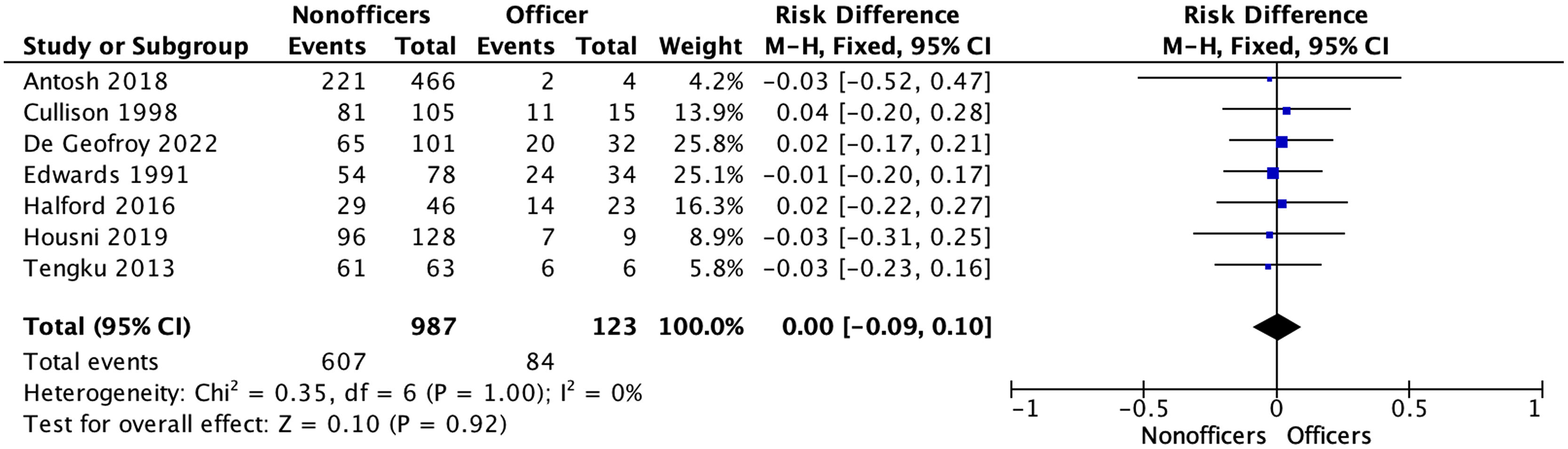
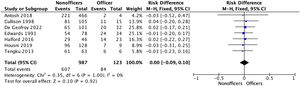
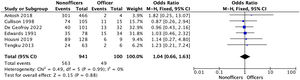
Clinical results and associatedThe RTFD rate was reported in all studies. Homogeneity between studies was good (I2=0%, p=1.00). The overall rate of RTFD in military personnel was 62.3% (61.5% for the non-officer group versus 68.3% for the officer group), with no significant difference (p=.92).
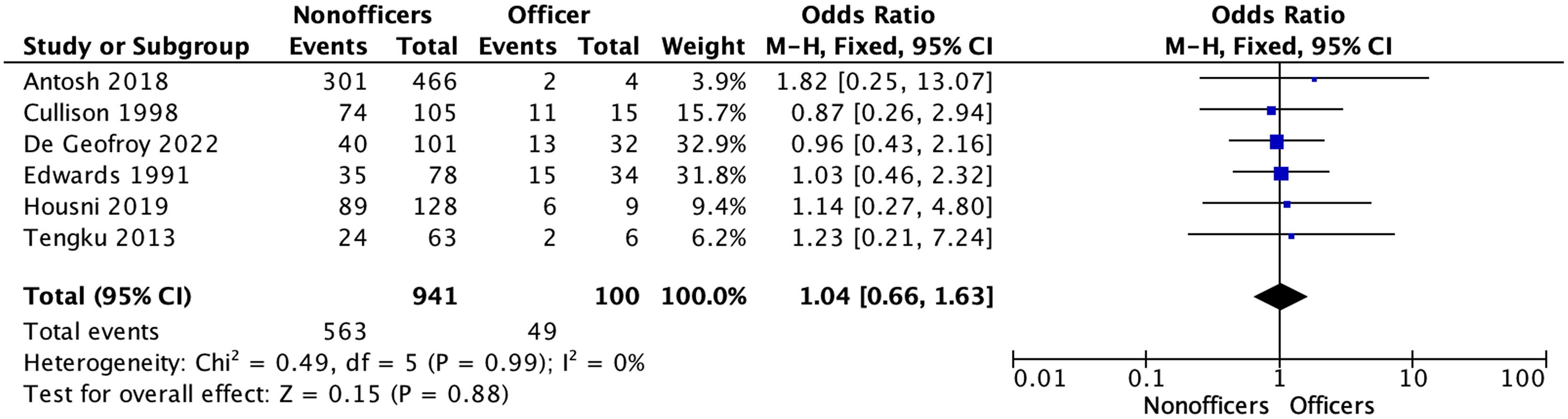
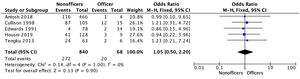
The overall rate of meniscal injuries associated with ACL rupture was reported in six studies. Homogeneity was good (I2=0%, p=.99). The overall rate of meniscal injury in the military was 58.8% (59.8% for the non-officer group versus 49% for the officer group), with no significant difference (p=.88).
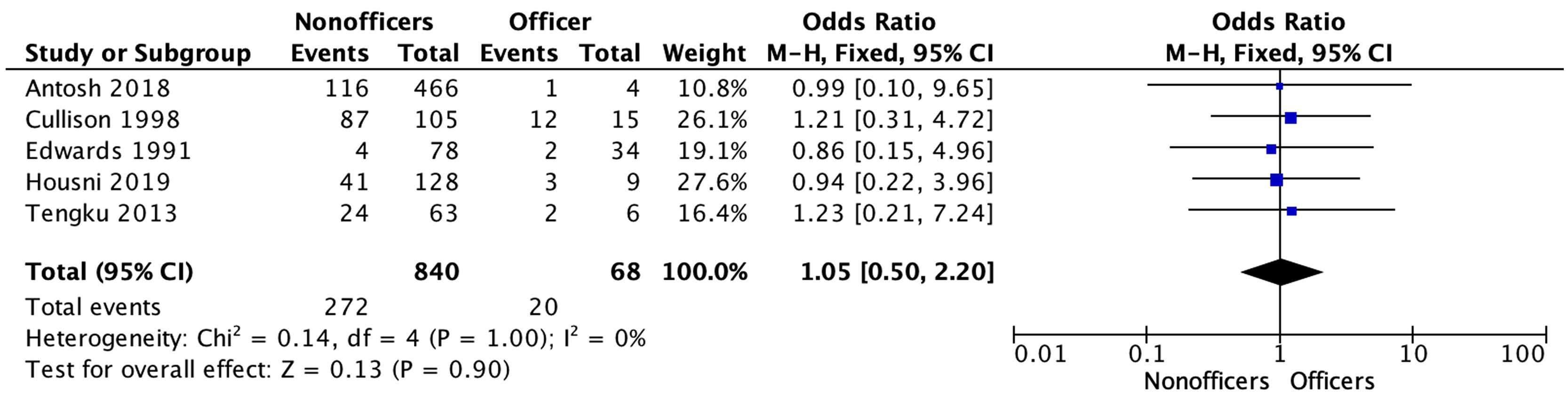
The overall rate of chondropathy associated with ACL rupture was reported in five studies. Homogeneity was good (I2=0%, p=1.00). The overall meniscal injury rate in the military was 32.2% (32.4% for the non-officer group versus 29.4% for the officer group), with no significant difference (p=.9). The results of the RTFD forest plot and associated injuries are shown in Figs. 2–4.
This meta-analysis provides details of the functional results of soldiers operated on for ACL and the incidence of associated meniscal lesions and chondropathy in these patients. It should be noted that the risk of ACL rupture is particularly high in this population group due to the fact that their regular activity requires high physical demands after ligament reconstruction, resulting in a high number of these soldiers not regaining the level of regular military activity they had prior to the ACL injury.15
The ACL is a frequently injured ligament of the knee and is known to occur in people who participate in sporting activities. As sports become an increasingly important part of daily life, the number of ACL injuries has also steadily increased. ACL injuries are a major concern for military and civilian health systems, with estimates of growth of 4–6% per year, particularly among young people (15–25 years).17 However, most of the literature on ACL injuries has focused on the civilian population.13 Previous studies have shown that this injury is not uncommon among military personnel, resulting in knee instability and affecting performance in military duties, loss of duty time and military readiness.4
Service in the armed forces involves intensive and physically arduous work in environmentally challenging locations, far from medical support. There is evidence that successful ACL reconstruction does not provide excellent results in this population.7,16 In this regard, all the studies reviewed found a higher prevalence of these injuries in lower-ranking military personnel, probably associated with greater physical demands in their usual military activity and, therefore, a lower prevalence of these injuries in military officers. As evidenced by this study, although the total number of ACL injuries is higher among non-commissioned military personnel due to physical military practice in their regular work, as opposed to commissioned military personnel, who are less exposed to a possible ACL injury due to their command and less combat activities, the differences are not significant between the two groups in terms of the rate of RTFD (61.5% in non-officer personnel compared to 68.3% in officer personnel). The same is true for associated injuries, such as meniscal injury (59.8% in non-officers versus 49% in officers, with no significant difference) and associated chondropathy (32.4% in non-officers versus 29.4% in officers, with no significant difference).
Regarding the selection of the best ACL reconstruction plasty, this remains a controversial issue for the military. In a recent survey of military orthopaedic surgeons regarding ACL plasty, more than 50% of surgeons preferred BTB plasty; 26.25% preferred hamstring; 3.75% preferred quadriceps tendon; 2.5% preferred allograft; and the remaining 16.25% deferred the decision to patient preference in males under 25 years of age.18 Several meta-analyses have reported no superiority of one technique over another; however, these studies are heterogeneous and include a wide range of patient ages and many do not specify patient activity level.
According to Tennent and Posner,3 patellar tendon autograft has become the gold standard for ACL reconstruction by military orthopaedic surgeons, as it has repeatedly been shown to offer the safest fixation with low failure rates and high patient-reported outcomes.3 However, in the studies collected, four had used BTB as an autograft (in three together with other techniques and in one solely) and four had used hamstring (in three together with other techniques and in one solely), so we can see that there is no clear predominance over the BTB technique as found in this meta-analysis.
In terms of clinical–functional outcomes regarding return to military activity after ACL surgery, we found an RTFD rate of between 47.4% and 97.1% according to the studies reviewed, regardless of the surgical ligamentoplasty technique used, so that a considerable number of servicemen who underwent ACL plasty continue to have some degree of activity limitation after ligament reconstruction.
Return to sport is a particularly important criterion following an ACL tear and has been extensively studied in the literature in sporting populations that may have physical demands comparable to those of the military study population.14 Furthermore, the harsh military work environment is an additional factor that could decrease the rate of return to pre-injury activity level.15
Predictors of poorer outcomes in this population include subsequent surgeries, severe chondromalacia at the time of surgery, need for revision surgery and a combined multi-ligamentous injury.3 It is of note that chondropathy rates were significantly higher in military populations than in the general population,19,20 and a large-scale study of knee joint degeneration in an active military population showed that incidence rates of both primary and secondary osteoarthritis increased significantly between 2005 and 2014.21 In terms of associated meniscal damage, the incidence rate of meniscal injury ranges from 38% to 70% according to the studies reviewed.
The literature showed that ACL injury can be associated with meniscal injury in 42–77% of cases and cartilage injury in 20–23% of cases. These associated injuries were associated with a lower rate of return to play in elite athletes.22
Regarding the limitations of this review, we can highlight that all of the studies were retrospective, either comparative cohorts or case series, i.e., studies with a III–IV evidence level, so the results must be considered with caution, since the possibility of finding selection and detection biases was very high due to the study designs. No prior systematic review protocol has been carried out in this study. The prevailing fact is that the topic of the study deals with a common ailment associated with a population not widely studied in the literature, so the number of studies selected is small, thereby limiting the number of comparisons. In addition, we should add the variability of the origin of the sample collected by the studies, which makes the comparison process even more difficult. Follow-up according to the outcomes differed between the studies, which compromised the greater number of comparisons and variables included in this meta-analysis. The studies did not include risk factors or comorbidities of the included patients, resulting in these aspects not being assessed in the outcomes. Further exploration of statistical non-uniformity with subgroup analyses has not been attempted due to the limited number of articles, which limits confidence in the validity of the study results. Variables with greater follow-up, complications and functional outcomes were missing. Furthermore, the wide variability in the type of complications, techniques and origin of the sample in each study obfuscates a better statistical comparison between them. Notwithstanding, the groups analysed in this meta-analysis are homogeneous for the variables analysed (I2<30%). Notwithstanding, the type of plasty, BTB or hamstrings, as well as other factors related to the sample (American, European, Asian) and associated comorbidities that may predispose to better or worse results, have not been analysed. Finally, the population is highly specific and difficult to extrapolate to the general population although it may be comparable to populations of elite athletes.
To date, and according to that published in the literature, this is the first meta-analysis on this topic, so comparisons with similar studies could not be established. Further prospective studies that provide greater evidence than our findings and that may lead to possible changes in military training programmes in order to avoid this type of injuries are required.
ConclusionsReturn to full military activity can be used in the military population as a marker of success after ACL reconstruction. Although high success rates are generally reported following this intervention, our study revealed that a large number of military personnel experience permanent activity limitations that prevent full return to duty, with no differences existing between officers and non-officers.
Level of evidenceLevel of evidence iv.
Conflict of interestsThe authors have no conflict of interests to declare.