The spring ligament has paramount role in supporting the arches and its fail causes the collapse of the medial longitudinal arc, inducing adult acquired flatfoot deformity. Our aim was to analyze the clinical and radiological outcomes of spring ligament repair and titanium wedges integration used in surgical osteotomies.
Material and methodsWe performed a retrospective study of 23 cases with middle ages of 63, diagnosed with adult acquired flatfoot deformity stage IIB in RAM classification after ortho-prosthetic treatment failure, assessing the functional outcomes using the American Orthopedic Foot and Ankle Society scale and the radiological outcomes studying angles variation (talonavicular uncoverage, talo-first metatarsal angle and Meary axis).
ResultsThe mean preoperative American Orthopedic Foot and Ankle Society score of the sample was 52±10 and the postoperative 88±6 (p<0.05). The radiological outcomes showed a statistically significant improvement.
ConclusionSpring ligament repair associated to bone reconstruction offers large functional and radiological outcomes to adult acquired flatfoot deformity stage IIB treatment. Titanium wedges present an excellent bone integration.
En el desarrollo del pie plano valgo adquirido del adulto ha cobrado gran importancia el fallo de la columna medial, y no tanto la rotura del tibial posterior, siendo principalmente la lesión del ligamento en hamaca calcaneonavicular (spring ligament) el determinante del desarrollo de esta deformidad. Nuestro objetivo es analizar los resultados clínico-radiológicos de la reparación del ligamento en hamaca, y valorar la utilidad e integración de las cuñas de titanio poroso en las osteotomías a las que se asocia la reparación ligamentosa.
Material y métodosRealizamos un estudio retrospectivo de 23 casos con una edad media de 63 años, diagnosticados de pie plano valgo adquirido del adulto estadio IIB de la clasificación RAM tras fallo de tratamiento ortoprotésico, valorando los resultados clínicos mediante la escala de la American Orthopaedic Foot and Ankle Society y los resultados radiológicos pre y postoperatorios basándose en la variación de los ángulos estudiados (cobertura talonavicular y ángulo talar-1.er metatarsiano en la proyección dorsoplantar y línea de Meary en la proyección lateral).
ResultadosLa puntuación media en escala de la American Orthopaedic Foot and Ankle Society pasó de 52±10 preoperatorio a 88±6 (p<0,05). En cuanto a los resultados radiológicos se demostró una mejoría estadísticamente significativa (p<0,05) en la variación de los ángulos en el postoperatorio.
ConclusionesLa reparación de los estabilizadores mediales, asociada a técnicas óseas, ofrece excelentes resultados clínico-radiológicos en el tratamiento del pie plano valgo adquirido del adulto estadio IIB. Además, las cuñas de titanio poroso presentan una adecuada integración, evitando los problemas de pinzamiento de los peroneos, asociados al uso de placas y la necesidad posterior de retirada.
Adult acquired flatfoot (AAF) is a progressive painful deformity characterised by hindfoot valgus, medial arch collapse, associated with secondary supination and abduction of the forefoot.
In addition to the tibialis posterior that is the dynamic stabiliser of the medial longitudinal arch, the foot deformity results from a failure of the static ligamentous stabilisers, especially involving the spring ligament complex, formed by two fascicles, the superomedial calcaneonavicular ligament (with direct attachment to the tibialis posterior and the superficial deltoid ligament) and the inferior calcaneonavicular ligament, the former being stronger and wider than the latter. This ligamentous complex provides direct support to the medial/plantar aspect of the talar head, and its reconstruction may therefore be the basis for treatment in association with bone techniques.1
Among the multiple classifications of AAF, the RAM2 classification determines that it is not a linear process, as it can affect different areas (hindfoot, ankle and midfoot) in varying forms and degrees in each individual patient.
Subsequently, Pasapula3 introduced a new concept to the classification, from a biomechanical point of view, based on the medial column, with the initial failure of the calcaneonavicular spring ligament being the determining factor in the development of this pathology, adding a subclinical stage 0, and the failure of the tarsometatarsal plantar ligament, inducing dorsiflexion of the first metatarsal and favouring valgus deformity of the hindfoot.
Because it is this midfoot instability which leads to valgus deformity, in 2020 Myerson et al.4 proposed a new nomenclature for this pathology, “progressive collapsing foot deformity”, categorising the deformities into flexible (stage 1) or rigid (stage 2), and into five patterns of deformity based on location and clinical and radiological features.
The aim of the study was to analyse the clinical and radiological results of spring ligament repair with augmentation and transfer of the flexor digitorum longus, together with lateral column lengthening osteotomy and Cotton's osteotomy, associated or not with medial sliding osteotomy of the calcaneus, in patients diagnosed with acquired flatfoot deformity stage IIB according to the RAM classification.
The secondary objective was to evaluate the usefulness and integration of porous titanium wedges used in osteotomies.
Material and methodsPatient recruitmentWe conducted a retrospective study between 2017 and 2019, with a mean follow-up of 21.5 months (18–38 months).
Twenty-three cases were studied in 20 patients with a mean age of 63 years (46–73 years), with the female sex predominating at 73.9% (17 cases).
With regards to inclusion criteria, patients had been diagnosed with AAF deformity grade IIB according to the RAM classification, had had no previous surgery and conservative osteoprosthetic treatment with medial support insoles and supinator gradient had failed.
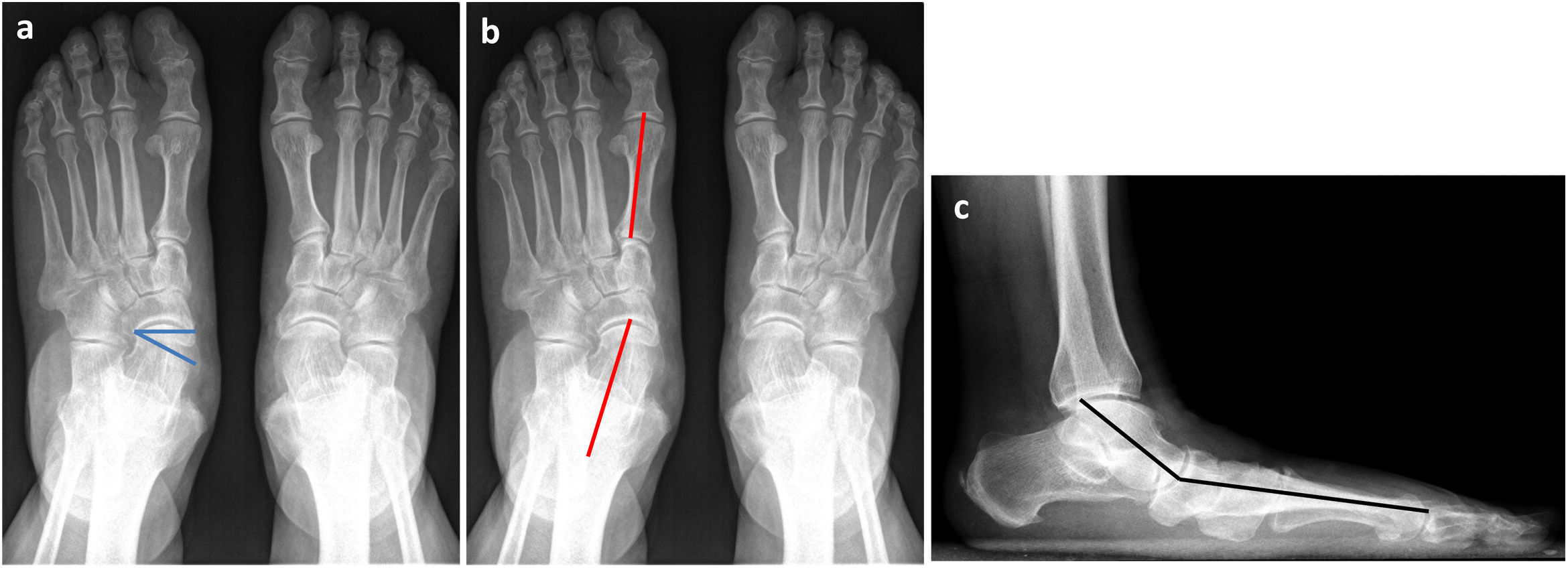
Study variablesA clinical–radiological study was performed, based on the American Orthopaedic Foot and Ankle Society Scale,5 and on pre- and post-surgical loading radiographs. The radiological results were based on the variation of the talonavicular coverage angles (TNC), the talar first metatarsal angle in the dorsoplantar projection in loading (TFMA) and the Meary line in the lateral projection in loading (Fig. 1).
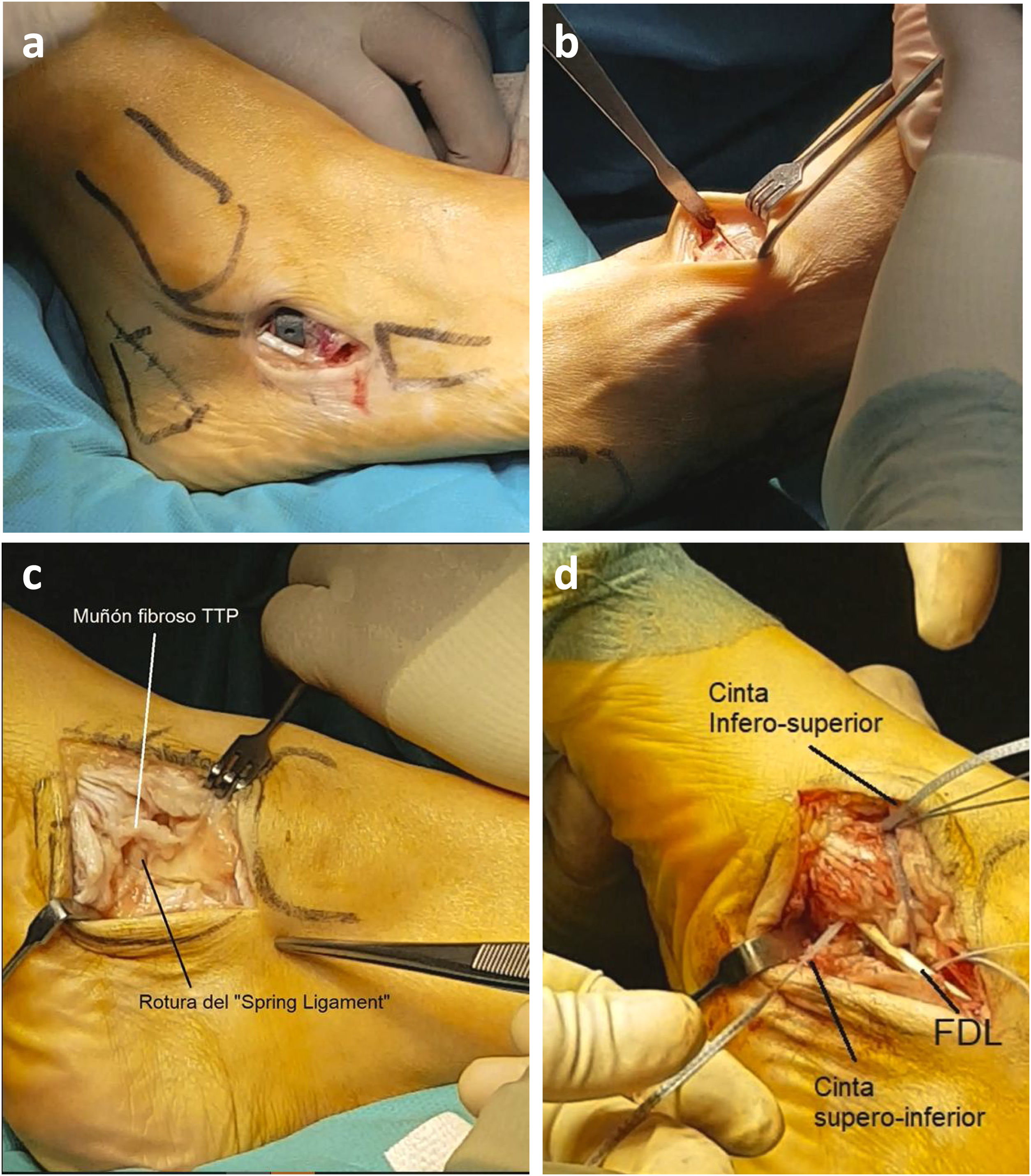
All patients underwent the same treatment sequence. Firstly, the achilles-calcaneal-plantar system was assessed to determine the need for surgical action at the level of the medial gastrocnemius muscle or Achilles tendon. Subsequently, Evans-type lateral column lengthening with porous titanium wedges up to 8mm thick (Wright Medical®, Memphis, TN), associated in 9 cases with MSCO, fixed with two 6.5mm headless HCS cannulated screws (DePuy Synthes Johnson & Johnson®, New Brunswick, NJ). All patients underwent repair with spring ligament augmentation and transfer of the flexor digitorum longus to the navicular tubercle with 5.5mm Swivelock biodegradable screws (Arthrex®, Naples, FL) and Cotton osteotomy with porous titanium wedges6 about 6mm thick (Wright Medical®, Memphis, TN) (Fig. 2).
Statistical analysisFor the statistical study the SPSS 23.0 programme was used (IBM Corp.®, Chicago, IL, U.S.A.).
ResultsFunctional clinical results were assessed according to the AOFAS scale, with the preoperative result being 52±10 and the postoperative result being 88±6, and with this difference being statistically significant (p<.05).
Regarding radiological findings, the preoperative talonavicular coverage angle (TNC) was 21.3±5.4 and 7.3±3.4 postoperatively (p<.05), the TFMA was 18.3±5.1 preoperatively and 3.9±2.4 postoperatively (p<.05) and Meary's line went from 15.7±3.4 preoperatively to 3.1±2.2 postoperatively (p<.05) (Table 1).
All the studied parameters show a statistically significant improvement (Fig. 3).
In reference to the degree of integration of the porous titanium wedges,7 the appearance of osteolysis and radiolucency was taken into account, as well as mobilisation of the material in serial radiographs, which were not observed in any of the cases studied.
With regard to complications, one case of progression of the deformity requiring double medial arthrodesis and one case of dehiscence of the surgical wound, which was resolved with local dressings, should be highlighted.
DiscussionBased on the role of the calcaneonavicular spring ligament as a stabiliser of the medial spine, and how its primary involvement favours the progressive development of the AAF, it is to be expected that surgical action at this level, associated with other surgical gestures, will have good results in treating this pathology in still flexible stages.8
Ligament repair must be accompanied by surgical intervention at bone level. Traditionally, medial calcaneal osteotomy (Koutsogiannis technique9) has been used to restore the point of traction of the Achilles tendon, helping to correct the valgus deformity of the hindfoot.10 However, this technique does not complete the correction of forefoot abduction or the lack of coverage of the talar head at the talonavicular joint.
Therefore, depending on the predominant type of deformity, it is necessary to perform other surgical techniques, such as lateral column lengthening osteotomy (Evans technique11) to correct forefoot abduction, present in stage IIB, thus favouring navicular rather than talar head coverage, reducing calcaneotalar divergence.12,13 Other techniques necessary to correct residual forefoot supination deformity include plantar flexion osteotomy of the medial cuneiform (Cotton technique14) or tarsometatarsal fusion (Lapidus technique15).
At present, there are various techniques for ligamentous intervention, either direct suturing in the case of tears or anatomical reconstruction of the ligament, creating an augmentation with a FiberTape® type suture with a vertical tunnel at the level of the navicular, anchoring it to another tunnel in the sustentaculum tali.16–18
With regard to osteotomies, a possible associated complication is the non-union of the graft traditionally used. According to the literature, the percentage of non-union is around 1.4%.19 In the total sample studied, no radiological signs indicating consolidation failure were detected, and adequate osteotomy integration was observed in all cases.
In addition, with the use of titanium wedges, replacing the traditionally used plates, we have observed a decrease in the rate of complications related to them.
The first limitation of our study is that it is a retrospective study. In addition, for the radiographic measurement of the angles studied, there is great inter- and intra-observer variability, after using measurement programmes available in our hospital.
Despite the limitations listed above, the sample was homogeneous in terms of patient selection, with an adequate number of patients for the study. In addition, all patients underwent the same protocolised treatment, performed in all cases by the same surgical team.
There are no comparative studies in the literature on the degree of integration between porous titanium wedges and previously used grafts, nor studies on the function and degree of correction of the wedges, so prospective studies are needed to determine the long-term clinical and functional repercussions of using porous titanium wedges in the treatment of AAF deformity in flexible stages.
ConclusionsThe repair of medial stabilisers associated with bone techniques offers excellent clinical and radiological results in the treatment of stage IIB AAF.
In addition, porous titanium wedges are well integrated, avoiding problems of peroneal impingement and the need for plate removal.
FundingThis research did not receive any specific grants from public or commercial sector agencies or from any not-for-profit entities.
Level of evidenceLevel of evidence IV.
Conflict of interestsThe authors have no conflict of interests to declare.
Right to privacy and informed consentThe authors have obtained informed consent from the patients and/or subjects referred to in the article. This document is held by the corresponding author.
Ethics committee approvalApproved by the Ethics Committee of Hospital Vozandes Quito.