The tarsal coalition can be a cause of mid-hindfoot pain in older children. The objective is to analyse the types of coalition treated in our hospital from 2010 to 2019 as well as the treatment carried out.
Material and methodObservational, descriptive and retrospective study of 18 patients with tarsal coalition, 8 women and 10 men, aged 11.9±2.6 years. Epidemiological data, clinical findings and imaging tests, and treatment performed were collected.
ResultsTwenty-five feet (38.8% bilateral) were reviewed. The main symptom was pain. Sixty-four percent were associated with flat-valgus foot. Fifty-two percent were located in the calcaneal-scaphoid joint, and 40% in the calcaneal-talar joint. Treatment was conservative in 44.4% of cases and surgical in 56% (coalition resection). There was only one case of recurrence. The results were mostly excellent or good (88%) after a mean follow-up period of 4 years.
ConclusionsThe most frequently diagnosed type of tarsal coalition was that located in the calcaneal-scaphoid joint followed by the calcaneal-talar joint, but they can appear in any joint of the foot. Almost half responded well to conservative treatment with mostly good results, but the rest required surgical treatment due to persistence of the symptoms, the results of which were excellent in all cases except one who suffered a recurrence. In cases of calcaneal-talar coalitions associated with severe hindfoot valgus, correction of this deformity, associated or not with resection of the coalition, is recommended.
La coalición tarsiana puede ser causa de dolor de medio-retropié en niños mayores. El objetivo es analizar los tipos de coalición tratados en nuestro centro hospitalario de 2010 a 2019 así como el tratamiento realizado.
Material y métodoEstudio observacional, descriptivo y retrospectivo de 18 pacientes con coalición tarsiana, ocho mujeres y 10 hombres, de 11,9 ± 2,6 años de edad. Se recogieron datos epidemiológicos, hallazgos clínicos y de pruebas de imagen y tratamiento realizado.
ResultadosSe revisaron 25 pies (38,8% bilaterales). El principal síntoma fue el dolor; 64% se asociaba a pie plano-valgo, 52% se localizaba en la articulación calcáneo-escafoidea, y 40% en la calcáneo-astragalina. El tratamiento fue conservador en un 44,4% de los casos y quirúrgico en 56% (resección de la coalición). Se produjo un solo caso de recidiva. Los resultados fueron mayoritariamente excelentes o buenos (88%) tras un periodo medio de seguimiento de cuatro años.
ConclusionesEl tipo de coalición tarsiana diagnosticada con mayor frecuencia fue la localizada en la articulación calcáneo-escafoidea seguida de la calcáneo-astragalina, pero puede aparecer en cualquier articulación del pie. Casi la mitad respondieron bien al tratamiento conservador con resultados mayoritariamente buenos, pero el resto requirieron tratamiento quirúrgico por persistencia de la clínica, cuyos resultados fueron excelentes en todos los casos excepto en uno que sufrió una recidiva. En los casos de coaliciones calcáneo-astragalinas asociadas a valgo severo de retropié, la corrección de esta deformidad, asociada o no a la resección de la coalición, es recomendable.
One possible cause of foot pain, repeated ankle sprain or insidious onset of painful flatfoot with rigid valgus deformity of the hindfoot in older children and teenagers is tarsal coalition.1 This is the absence of segmentation between 2 or more bones in the foot due to the failure of development of the joint cleft in the embryonic period. Clinical series estimate a rate of 1%–6% but as they are often asymptomatic or undiagnosed, actual incidence may be higher.1 The most common coalitions are calcaneal-navicular and talo-calcaneal, accounting for almost 90% of all cases, but any adjacent bone in the foot may be fused.2
Advances in imaging methods have increased diagnostic possibilities and have favoured an evolution of treatment from conservative to surgical. The latter is generally recommended in the event of failure of conservative treatment and usually consists of resection of the coalition and interposition of soft tissue to prevent recurrence.3
The aim of this study is to analyse the types of tarsal coalition, depending on the joint of the foot affected, diagnosed in our hospital during the period from 2010 to 2019, as well as the type of treatment performed, both conservative and surgical, and the results obtained after treatment.
Material and methodAn observational, descriptive and retrospective study was conducted in 18 patients (25 feet in total) diagnosed with tarsal coalition in our hospital between 2010 and 2019.
The study included all patients under 18 years of age who consulted for clinical manifestations located in the foot or ankle and were finally diagnosed with tarsal coalition.
To obtain the data for the study, a review of the digitalised medical records of these patients in the Orion Clinic programme, as well as their imaging tests, was carried out.
As study variables, epidemiological data were collected (sex, age at diagnosis, personal history); clinical data from the anamnesis and physical examination (analysis of the plantar footprint by podoscope according to Viladot's classification4 and of the alignment of the hindfoot with the tibia); data from the imaging tests (type of tarsal coalition and its location, laterality or bilaterality); and the type of treatment performed (complications and results).
For evaluation of findings the following functional scale was used5: grade I (excellent: patient without pain, deambulation and practice of sport to the same level as before the appearance of symptoms); grade II (good: cyclical pain and/or deambulation and lowered practice of sport); grade III (fair: frequent pain and/or major sport restriction or change to a less active sport); grade IV (bad: constant pain, no practice of sport or patient reoperated on).
In all cases anteroposterior and lateral loading and oblique radiographs were taken. In patients in whom the diagnosis of coalition was not clear on radiographs but there was a high degree of suspicion and in those in whom surgical treatment was considered, the diagnosis was complemented with CT and/or MRI. In cases where the younger age of the patient and the X-ray and/or CT findings led to the suspicion that the coalition was in the early stages of development and therefore could be a fibrous or cartilaginous bridge not visible on CT, MRI was chosen.
All the above data were collected onto a Microsoft Office 2011 Excel database (version 14.4.5) and then processed using IBM SPSS Statistics (version 22.0.0.0) to obtain descriptive statistics. Quantitative variables were expressed as mean, minimum and maximum values and standard deviation. Qualitative variables were presented as relative and absolute frequencies.
This study has been carried out in accordance with the official standards in force and in agreement with the World Medical Association and in line with the WHO code of ethics (Declaration of Helsinki). Furthermore, the anonymity of the patients included in the study and the confidentiality of the data have been respected. The study was accepted by the Research Ethics Committee of our hospital.
ResultsThe study comprised 18 patients, 8 women (44.4%) and 10 men (55.5%). Mean age at diagnosis of tarsal coalition was 11.9±2.6 years [4–16]. A total of 25 feet were reviewed since in 7 patients (38.8%) synotosis was bilateral. In the unilateral cases, 6 patients were diagnosed in the left foot (33.3%) and 5 in the right foot (27.7%).
In 11.1% (2 cases) of the tarsal coalitions symptoms were present: one patient aged 12 years with a bilateral calcaneal-scaphoid coalition was diagnosed with a brachio-oto-renal polymalformative syndrome and a 4-year-old patient with peroneal haemimelia type IA (Achterman and Kalamchi classification), who presented with an equino-varo-adductus left foot deformity with an agenesis of the fifth radius and fusion of the calcaneus with the talus.
In terms of signs, symptoms and clinical findings the following were detected: asymptomatic cases (1/18; 5.5%); recurrent sprains (1/18; 5.5%); pain when walking (12/18; 66.6%); pain only when running or doing sports (4/18; 22.2%); walking with the foot in external rotation and foot abduction (5/18; 27.7%).
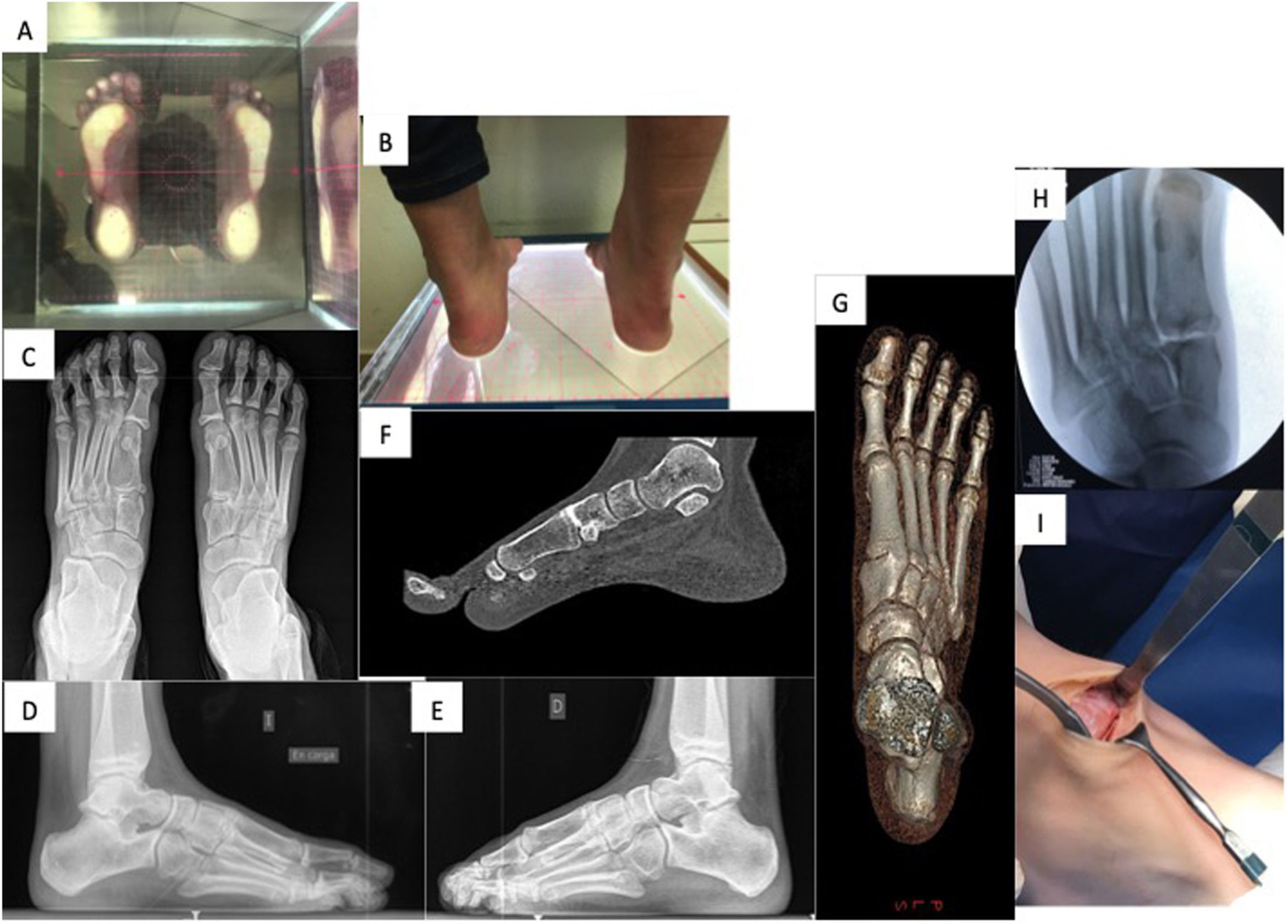
Regarding the footprint impression on the podoscope, 16 (64%) feet had a flat footprint of different grades according to the Viladot classification4: 4/16 (25%) grade I, 8/16 (50%) grade II, 3/16 (18.7%) grade III and 1/16 (6.2%) grade IV. One patient (2/25; 8%) had cavus feet in relation to a partial bony coalition between the first wedge and the base of the first metatarsal in both feet (Fig. 1A–G). The patient with peroneal haemimelia had an equino-varo-adductus foot morphology. Six feet (24%) had a normal footprint. In terms of hindfoot morphology, 17 feet (68%) had a valgus deformity, rigid in 11 cases (64.7%) and reducible in 6 cases (35.2%).
Bilateral partial bony coalition at the level of the joint between the base of the first metatarsal and the first wedge. (A) Plantar footprint on podoscope. (B) Clinical image of the hindfoot. (C) Dorsal-plantar loading X-ray prior to surgery showing the bilateral coalition. (D) Profile projection radiograph of the Left foot under load. (E) X-ray of the loaded profile projection of the right foot. (F) CT image (sagittal section). (G) Three-dimensional reconstruction CT image. (H) Fluoroscopy image after resection of the coalition during surgery. (I) Image of the resection area during surgery.
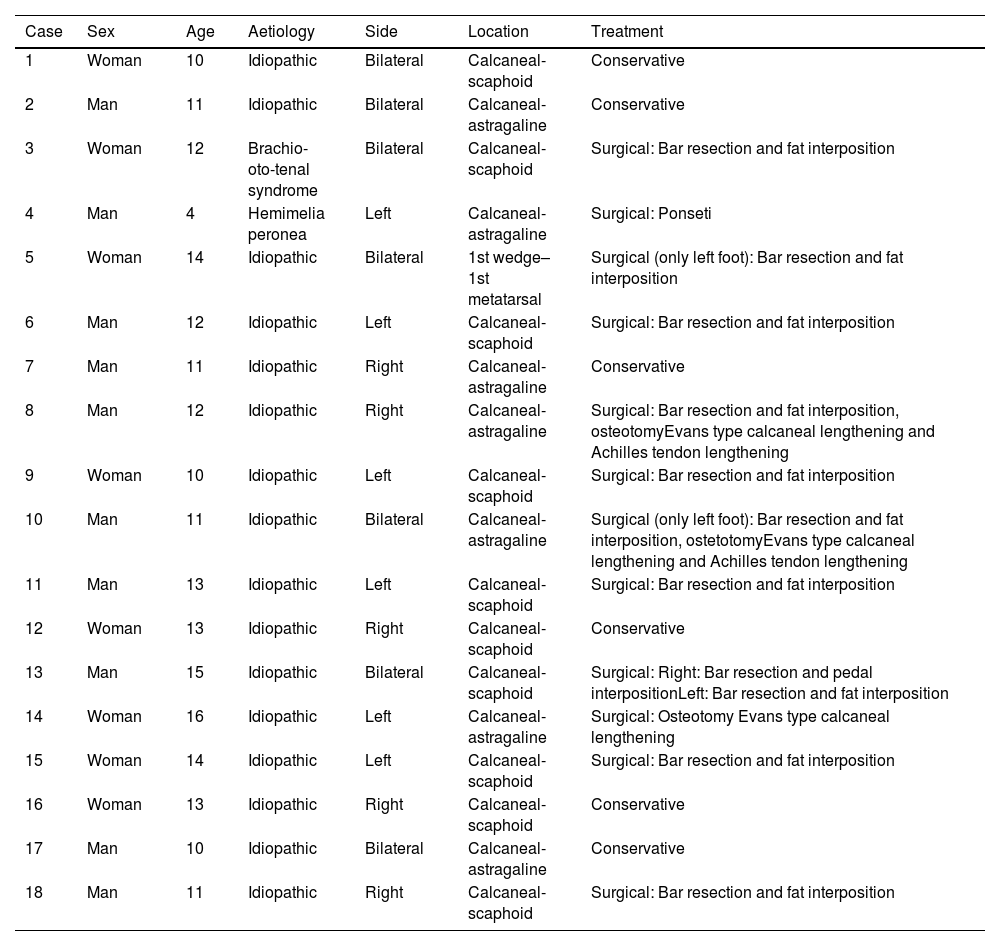
Table 1 contains data relating to sex, age, aetiology, laterality, location of coalition and treatment applied for each case.
Characteristics of the patients with tarsal coalition and the treatment applied.
| Case | Sex | Age | Aetiology | Side | Location | Treatment |
|---|---|---|---|---|---|---|
| 1 | Woman | 10 | Idiopathic | Bilateral | Calcaneal-scaphoid | Conservative |
| 2 | Man | 11 | Idiopathic | Bilateral | Calcaneal-astragaline | Conservative |
| 3 | Woman | 12 | Brachio-oto-tenal syndrome | Bilateral | Calcaneal-scaphoid | Surgical: Bar resection and fat interposition |
| 4 | Man | 4 | Hemimelia peronea | Left | Calcaneal-astragaline | Surgical: Ponseti |
| 5 | Woman | 14 | Idiopathic | Bilateral | 1st wedge–1st metatarsal | Surgical (only left foot): Bar resection and fat interposition |
| 6 | Man | 12 | Idiopathic | Left | Calcaneal-scaphoid | Surgical: Bar resection and fat interposition |
| 7 | Man | 11 | Idiopathic | Right | Calcaneal-astragaline | Conservative |
| 8 | Man | 12 | Idiopathic | Right | Calcaneal-astragaline | Surgical: Bar resection and fat interposition, osteotomyEvans type calcaneal lengthening and Achilles tendon lengthening |
| 9 | Woman | 10 | Idiopathic | Left | Calcaneal-scaphoid | Surgical: Bar resection and fat interposition |
| 10 | Man | 11 | Idiopathic | Bilateral | Calcaneal-astragaline | Surgical (only left foot): Bar resection and fat interposition, ostetotomyEvans type calcaneal lengthening and Achilles tendon lengthening |
| 11 | Man | 13 | Idiopathic | Left | Calcaneal-scaphoid | Surgical: Bar resection and fat interposition |
| 12 | Woman | 13 | Idiopathic | Right | Calcaneal-scaphoid | Conservative |
| 13 | Man | 15 | Idiopathic | Bilateral | Calcaneal-scaphoid | Surgical: Right: Bar resection and pedal interpositionLeft: Bar resection and fat interposition |
| 14 | Woman | 16 | Idiopathic | Left | Calcaneal-astragaline | Surgical: Osteotomy Evans type calcaneal lengthening |
| 15 | Woman | 14 | Idiopathic | Left | Calcaneal-scaphoid | Surgical: Bar resection and fat interposition |
| 16 | Woman | 13 | Idiopathic | Right | Calcaneal-scaphoid | Conservative |
| 17 | Man | 10 | Idiopathic | Bilateral | Calcaneal-astragaline | Conservative |
| 18 | Man | 11 | Idiopathic | Right | Calcaneal-scaphoid | Surgical: Bar resection and fat interposition |
In all cases, plain X-rays were performed as an initial complementary test. In 9 cases (50%) the diagnosis was complemented with MRI, in 5 patients (27.7%) with CT, and in 4 cases (22.2%) with both imaging tests.
The most frequent location of tarsal coalition (13 cases, 52%) was at the level of the calcaneal-scaphoid joint, followed by the calcaneal-astragaline joint (10 cases, 40%). Two cases (8%) were detected in a rare location between the base of the first metatarsal and the first cuneiform. Fifty-two per cent (13 feet) consisted of fibrous coalitions, 36% (9 feet) were cartilaginous coalitions according to the MRI report, and 12% (3 cases) were bony.
As may be appreciated in Table 1, in 11 feet (44.4%) conservative treatment was successfully applied and in 14 (56%) it was necessary to use surgical treatment due to non-improvement of symptoms with conservative measures. Conservative treatment consisted in using orthopaedic insoles and modifying sports activity.
Surgical treatment of calcaneal-scaphoid coalitions involved open resection via an Ollier approach over the tarsal sinus, together with interposition of bone wax and autologous fatty tissue from the inner and proximal thigh. Only one patient underwent interposition via the pedicle muscle. The case associated with peroneal haemimelia was treated by serial manipulations according to Ponseti's method and the Achilles tendon was subsequently lengthened, without acting on the coalition. In the case of bilateral first metatarsal-first wedge coalition, only one of the feet, the left foot, was treated by resecting the bar and interposing fat (Fig. 1H and I).
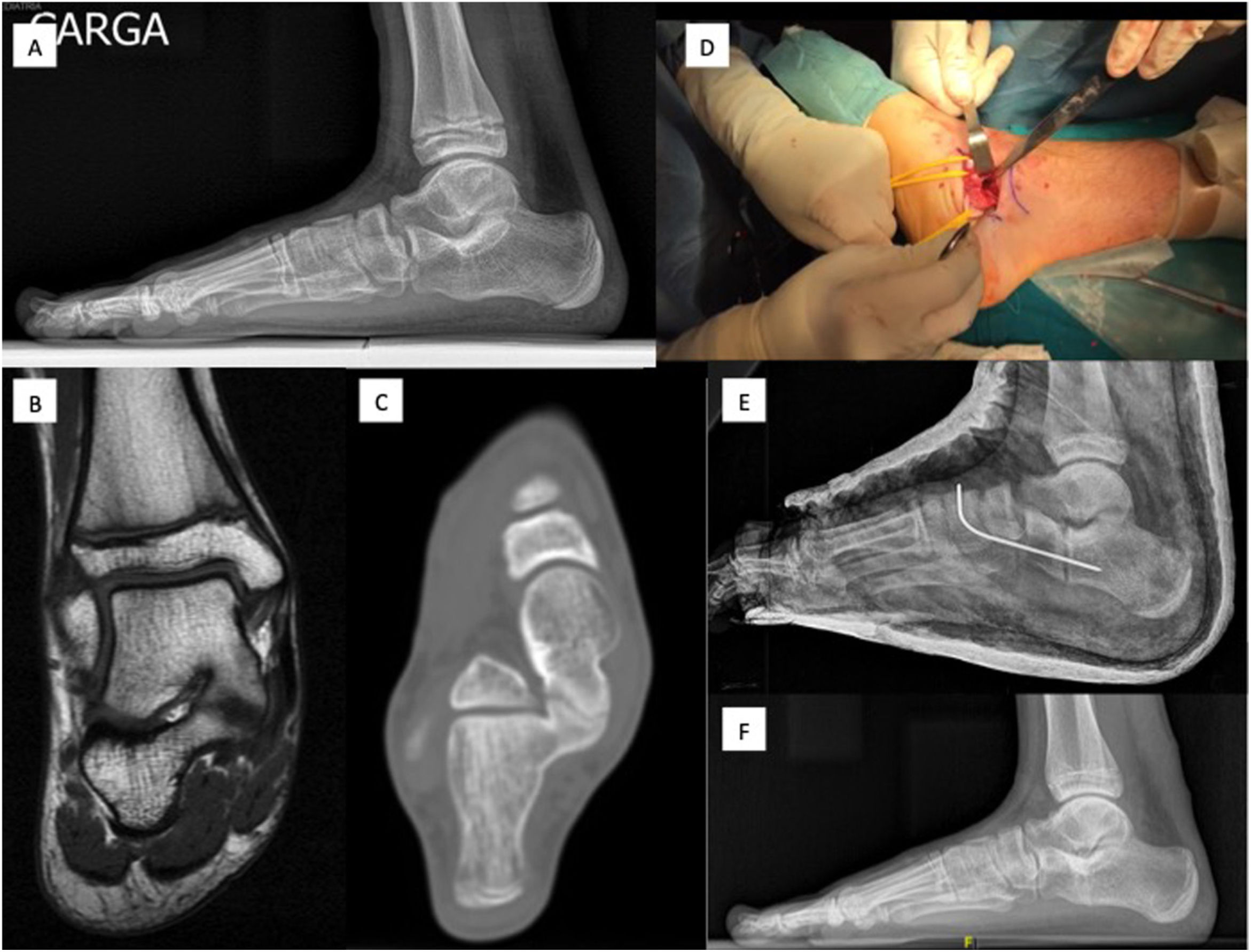
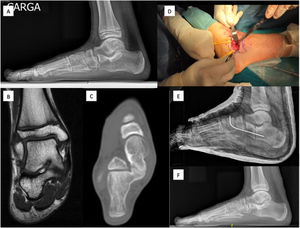
In the case of calcaneal-talar coalitions, in 2 patients with a coalition of less than 50% of the articular surface, an open resection of the bar was performed through a medial approach with interposition of autologous fatty tissue (Fig. 2). In these 2 cases, a calcaneal lengthening osteotomy with autologous iliac crest graft was also associated with the Evans technique, and a percutaneous lengthening of the Achilles tendon at 3 levels. In the third patient, only the calcaneal lengthening osteotomy was performed, without resecting the rod, because the rod was greater than 50% and was considered unresectable, achieving an improvement in hindfoot valgus. The calcaneal osteotomies were fixed with a Kirshner wire, except in one patient where a Synthes X-plate with 4 screws was used to provide greater stability.
Calcaneal-astragaline coalition with less than 50% extension. (A) Pre-surgical foot loading profile radiograph. (B) MR image (coronal slice). (C) CT image (coronal section). (D) Image of the resection site during surgery. (E) Postoperative X-ray after resection and calcaneal lengthening osteotomy fixed with K-wire. (F) Loading X-ray in profile projection after consolidation of the osteotomy.
After surgery all cases were immobilised with a suropedic splint which was removed at 3 weeks in patients in whom calcaneal osteotomy was not performed or at 6 weeks in those in whom it was performed, and partial weight bearing was then progressively initiated. No immediate postoperative complications such as infections, haematomas or neuromas were detected.
Of the 11 idiopathic cases that underwent surgery, 9 feet were pain-free and started practising sports on average 3.6 [1.5–6] months after surgery. There was only one case of recurrence of the calcaneal-scaphoid coalition confirmed by CT scan 8 months after surgery with persistence of pain symptoms, which required a new surgical intervention by resection of the bar and interposition of fatty tissue, leaving the patient asymptomatic.
The mean follow-up time of the patients was 4 years [2–8]. According to the functional scale applied after treatment, overall, in 13 (52%) feet the results were excellent (grade I), in 9 (36%) good (grade II), in 2 (8%) fair (grade III) and in one case (4%) poor (grade IV). Among the 9 cases of idiopathic calcaneal-astragaline coalition, of the 6 feet treated conservatively, one case (16.6%) had an excellent result (grade I) and 5 cases (83.3%) good (grade II). The 3 cases treated surgically had an excellent result (grade I). Among the 13 cases of calcaneal-scaphoid coalitions, of the 6 feet treated conservatively, 3 had an excellent result (grade I) and 3 had a good result (grade II). All the cases operated on (6 feet) had an excellent result (grade I) except for one case (grade IV) due to recurrence. The outcome of the 2 feet with first wedge-first metatarsal base coalition was fair (grade III).
DiscussionCalcaneal-navicular coalition is the most frequent type described in the literature (53%–73%) followed by talocalcaneal (37%), results that coincide with those obtained in this series.1 There are few described cases of coalitions in rare locations6–8 and it is generally recommended that if the coalition is resectable and joint mobility can be recovered, in these cases exercises is a better option than arthrodesis in young patients. This is what was done in the case of the patient with a rare coalition between the base of the first metatarsal and the first wedge. Seo et al.9 suggest that patients with midfoot sprains that do not improve with conservative treatment or with persistent pain after minor trauma should be evaluated by CT scanning to rule out such coalitions in unusual locations.
There is a similar distribution by gender of this pathology,1 as observed in this study, although some predilection by the male sex has been detected. Fifty to sixty-eight percent are bilateral10 and both feet should therefore be examined. In our study this was observed to a lesser extent (38.8%). Tarsal coalitions generally manifest late due to the process of ossification of the coalition, which limits the mobility of the affected joint,3 as seen in our study, where the mean age of onset of symptoms was around 12 years. The most frequently observed symptomatology was pain in the foot, especially when walking or performing sports activities such as running, coinciding with what has been published in the literature.3
Most coalitions were cogenital/idiopathic but they can also appear in association with other malformations such as peroneal haemimelia, symphalangism, Apert syndrome, Nievergelt-Pearlman syndrome or proximal femoral deficiency.11,12 In our series, 2 syndromic cases were detected, peroneal haemimelia and brachy-oto-renal syndrome associated with other malformations such as peroneal hemimelia.
CT is very useful in assessing the extent of synostosis as well as in detecting recurrences and MRI allows early diagnosis of non-ossified coalitions in young patients with skeletal immaturity.2,3 In this review, MRI was used more frequently, probably because in most patients the coalitions were fibrous or cartilaginous. In the only case of recurrence in the series, CT scanning was essential to confirm coalition reossification in the face of persistent symptoms.
According to the literature, symptomatic conservative treatment should always be attempted based on the form of support or immobilisation of the affected foot, change in activities and non-steroidal anti-inflammatory drugs, reserving surgical treatment for those patients in whom conservative treatment fails.3 In a significant percentage of the patients presented (44.4%) conservative treatment, consisting of orthopaedic insoles and modification of sporting activity, was satisfactory. In the rest, the persistence of symptoms made it necessary to resort to surgical treatment, which generally consists of resection of the tarsal bar and the interposition of some type of material to prevent recurrence, such as the short extensor tendon of the fingers, autologous fat extracted 2cm from the gluteal fold or bone wax, haemostatic agents or silicone sheets.2 In our series only one patient had the extensor digitorum brevis muscle interposed. In all other cases autologous fat and bone wax were used.
In the case of the talo-calcaneal coalitions, Mosca et al.13 state that treatment of hindfoot valgus deformity by calcaneal lengthening osteotomy together with lengthening of the gastrocnemius or Achilles tendon is as important as that of the coalition, if the coalition is resectable due to its extent, in relieving pain. In our study, 3 patients with heel-calcaneal coalition associated with hindfoot valgus were treated by calcaneal lengthening osteotomy. In 2 cases, as the coalition had an extension of less than 50%, coalition resection was also performed, and in the third case only calcaneal osteotomy was performed, as the coalition was too extensive to be resected. The results in all 3 cases were excellent. Khosbin et al.14 also demonstrated good results with resection of the coalition and correction of the hindfoot valgus deformity in patients with heel-calcaneal coalitions of more than 50% and more than 16% valgus.
The main complications of resection of coalition are infection of the wound, sural neuropathy, incomplete resection or recurrent ossification, talonavicular subluxation and progressive degeneration.9 In this study only one case of recurrent ossification was detected which required further resection. According to Khoshbin et al.15, the incidence of reoperation after primary resection of a tarsal coaliation is low.
The results of resection are generally good irrespective of age, provided there is no joint degeneration.2 Saxena and Erickson16 conclude that patients have a higher level of activity and return to sporting activity 3 years after coalition resection compared to non-operative treatment. This is also demonstrated in the present study since, although the outcome was satisfactory in all cases treated conservatively, the percentage of cases with excellent function was higher in those who underwent surgery compared to those who did not (100% versus 16.6% respectively, in calcaneal-astragaline coalitions; 85% versus 50% respectively, in calcaneal-scaphoids). In the study by Mahan et al.,17 70% of patients had no activity limitation due to foot pain 2 years after coalition resection. Wilde et al.18 also reported good to excellent results in cases with a calcaneal-astragaline coalition if the CT surface of the coalition was less than 50% and the hindfoot valgus was less than 16°.
The main limitation of this study is that it is a small sample size, retrospective and case series type, so in the absence of a control group it is not possible to evaluate a statistical association. In addition, the follow-up period could be considered short in some cases and it would be advisable to conduct a study with a larger number of cases, in the longer term, in order to assess possible future problems.
As conclusions, tarsal coalitions should be kept in mind as a possible cause of foot pain in older children, although they are most frequently located between the scaphoid-calcaneus and talo-calcaneus, they can appear in any joint of the foot. Almost half of the cases can be treated conservatively with good results (cyclical but tolerated pain) but it seems that surgical treatment provides better results and allows the child to return to his or her functional state prior to the onset of the coalition. The risk of recurrence after resection is low but does exist and should be suspected if symptoms persist. In cases of calcaneal-talar coalitions associated with a valgus hindfoot, correction of this deformity as well, whether or not associated with resection depending on its extent, allows excellent results to be obtained.
Level of evidenceLevel of evidence IV.
FundingThis research did not receive any specific funding from public sector agencies, the commercial sector or not-for-profit entities.
Conflict of interestsNone.
FundingThe authors declare that they have received no funding for the conduct of the present research, the preparation of the article, or its publication.